Abstract
Prenatal exposures may be critical for immune system development, with consequences for allergic disease susceptibility. We examined associations of prenatal exposures (nutrient intakes and air pollutants) with allergic disease biomarkers in adolescence. We used data from 857 mother-child pairs in Project Viva, a Massachusetts-based pre-birth cohort. Outcomes of interest at follow-up (median age 12.9 years) were fractional exhaled nitric oxide (FeNO) and total serum IgE. We applied Bayesian Kernel Machine Regression analyses to estimate multivariate exposure-response functions, allowing for exposure interactions. Exposures were expressed as z-scores of log-transformed data and we report effects in % change in FeNO or IgE z-score per increase in exposure from the 25th to 75th percentile. FeNO levels were lower with higher intakes of prenatal vitamin D (−16.15%, 95% CI: −20.38 to −2.88%), folate from foods (−3.86%, 95% CI: −8.33 to 0.83%) and n-3 PUFAs (−9.21%, 95% CI −16.81 to −0.92%). Prenatal air pollutants were associated with higher FeNO and IgE, with the strongest associations detected for PM2.5 with IgE (25.6% increase, 95% CI 9.34% to 44.29%). We identified a potential synergistic interaction (p = 0.02) between vitamin E (food + supplements) and PM2.5; this exposure combination was associated with further increases in FeNO levels.
Similar content being viewed by others
Introduction
Allergic diseases represent a large proportion of childhood chronic disease, and constitute a major public health burden. Susceptibility to childhood allergic disease likely begins in fetal life. Fetal immune cell precursors are detectable at 3–4 weeks gestation, and begin seeding fetal tissues soon after1. Myeloid and lymphoid cell populations continue to expand until birth, and allergic sensitization and airway inflammation in response to foreign antigen exposures evolves throughout early and later childhood, further widening the potential window of susceptibility2.
Exposures encountered during prenatal life have been shown to have either adverse or, in some cases, protective associations with asthma and allergic disease in later childhood3,4. For example, a number of studies have shown early life air pollution exposures to be risk factors for later wheeze, asthma, and reduced lung function5,6,7. Other studies have found protective associations of maternal antenatal vitamin D or antioxidant nutrient intake with later allergic or respiratory outcomes8,9,10,11,12, though their findings have not always been reproducible13,14,15,16. In the antenatal and early-life periods, exposures do not occur one at a time, but as mixtures, with possible interactions amongst the exposures within those mixtures. Between-study variation in associations of individual exposures with allergy, asthma symptoms and lung function may occur in part because their effects in the context of other exposures were not explored. In addition, between-study variation in associations of exposures with allergy or asthma outcomes may reflect variation in subject sensitivity to those exposures and their mixtures. Recent studies have suggested sexual dimorphism in allergy and asthma that may lead to differential responses to pollutants17.
IgE and fractional exhaled nitric oxide (FeNO) are important intermediate biomarkers of allergic disease and allergic airway inflammation. IgE mediates the type I hypersensitivity reactions involved in pathogenesis of asthma and allergic rhinitis18. FeNO is a known biomarker of eosinophilic airway inflammation, and is elevated in subjects with atopy19. In adolescent children followed since the prenatal period, we examined multiple components from two prenatal exposure types, air pollution and maternal nutrient intakes, to determine their associations with IgE and FeNO measured in adolescence. We hypothesized that intake of prenatal antioxidant nutrients would mitigate the detrimental effects of prenatal air pollutants on allergic disease biomarkers measured in adolescence. We considered nutrient intakes from diet alone (as bioavailability and potential protective effects may be greatest when nutrients are absorbed from food), and then also conducted analyses using combined nutrient intakes from foods plus supplements. We also examined the potential for sexual dimorphism in the effects of mixtures of exposures on outcomes in adolescence, when the influences of sex on allergy and allergic airway inflammatory responses may be in transition.
To investigate these hypotheses, we applied Bayesian Kernel Machine Regression (BKMR)20, a recently developed approach for estimating the health effects of multi-exposure mixtures. Although there are other types of exposure-mixture modeling approaches, many of these have significant limitations. For example, clustering methods are often too reductionist (categorizing continuous exposures), variable selection methods (i.e. Lasso regression) typically rely on simple linear and additive models that may not adequately capture complex exposure-response relationships, and traditional hierarchical modeling techniques, while accounting for correlation amongst exposure mixture components, are typically also based on a parametric model that assumes (often unrealistic) linear and additive associations. BKMR offers distinct advantages over these other approaches, including the ability to allow for potential non-linear exposure-response relationships, to identify interactions between exposures, and to simultaneously rank the importance of hierarchical exposure groups in association with the outcome of interest. We applied BKMR methodology to data from Project Viva, a longitudinal pre-birth cohort study of prenatal exposures and chronic disease outcomes, with follow-up through adolescence.
Results
Sociodemographic and perinatal characteristics of the mothers and children enrolled in the study are shown in Table 1. Mean maternal pre-pregnancy BMI was 24.7 kg/m2. Sixty six percent of the children in the study were white, 15% were black, 4% were Hispanic and 16% were other race/ethnicities. Nine percent of women reported smoking in pregnancy. Characteristics of the mother-infant pairs at enrollment were very similar to the characteristics of those with FeNO and total IgE outcome data at the early teen visit age 12 (Supplemental Table 1). Distributions of the prenatal nutrient and air pollutant exposures (25th percentile, median, 75th percentile) are shown in Table 2.
Geometric mean (+/− stddev) FeNO concentrations were 19 ppb (+/− 2 ppb), and IgE was 63.2 IU/ml (+/− 4.14). Associations between socioeconomic and demographic covariates and our outcomes of interest are shown in Table 1. Males had higher FeNO as compared to females, but sex was not a predictor of total serum IgE levels. Children of other race/ethnicity tended to have higher FeNO and IgE, and there was a suggestion of an effect for higher IgE in black children. Differences between racial groups overall were marginally statistically significant (ANOVA p values = 0.1 for group comparisons). Participants born in winter or spring tended to have higher FeNO, but season of birth was not associated with total IgE levels. Maternal history of hay fever was related to a higher offspring total serum IgE concentration in adolescence (p = 0.006). There was no evidence for associations between report of smoking in pregnancy or maternal BMI and either FeNO or total serum IgE in adolescence.
For BKMR analyses, posterior inclusion probabilities were calculated for exposure groups in models for each outcome. In models for FeNO, the largest group of nutrients (Vitamin D, Vitamin C, Folate, n−3 and n−6 polyunsaturated fatty acids (PUFAs)) was consistently ranked higher than air pollutant exposures, with the second nutrient grouping (Vitamin E and β-carotene) ranked last. (Supplemental Table 2) In models for IgE, air pollutant exposures had much higher posterior inclusion probabilities than either of the individual nutrient groups, which showed similar posterior inclusion probabilities to one another. (Supplemental Table 3).
For models of FeNO, estimated dose response curves for individual exposures are shown in Fig. 1, and point estimates for percent increase in FeNO z score, with an increase in exposure from the 25th to 75th percentile, (with all other exposures are fixed at the median) are shown in Table 3. Maternal prenatal n−3 polyunsaturated fatty acids and folate from food sources were associated with reduced early teen FeNO levels (−9.21% (95% CI −16.81% to −0.92%) for n-3s and −3.86%, (95% CI −8.33% to 0.83%) for folate. In models with IgE as the outcome, point estimates for these two nutrients and were similar in magnitude and direction (Table 3). Prenatal vitamin D intake from foods showed a trend toward decreased FeNO measures in adolescence (Table 3). Overall, the strongest association observed was for black carbon (BC) exposure and total IgE level (15.25% increase in total IgE was associated with an interquartile range increase in log BC exposure). In models for the FeNO outcome, the point estimate for BC was 7.39% (95% CI −1.35 to 16.91%).
Estimated exposure response functions (h(z)) for prenatal nutrient intake (foods only), prenatal air pollution (Black carbon) and allergic disease outcomes in adolescence. Plots show the estimated relationship between log-transformed z scores of exposures (z) and outcomes; shaded areas indicate 95% credible intervals. Plots are shown for outcomes FeNO (A) and Total Serum IgE (B).
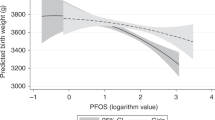
We also considered nutrient exposures as combined intakes from food and supplements, if supplement intakes for a given nutrient were available in our data (Table 4). Vitamin D intake (food plus supplements) showed a strong inverse association with FeNO (−16.15%, 95% CI: −20.38 to −2.88%). The shape of the estimated dose-response curve was not linear (Fig. 2), with a relatively flat dose-response at lower vitamin D levels, and a decreasing linear slope from moderate to high Vitamin D levels. In contrast, there was no clear relationship between Vitamin D intake from foods plus supplements and total IgE level (Table 4, Fig. 3). The point estimate for prenatal vitamin E intake from food and supplements combined was 6.94% (95% CI −2.36 to 12.24%) for the FeNO outcome (Table 4), which was much larger than the vitamin E estimate from diet alone (Table 3). No association was observed for Vitamin E and total IgE levels.
Estimated exposure response functions (h(z)) for prenatal nutrient intake from foods alone (choline, n-6 PUFAs, n-3 PUFAs, Beta-carotene) and foods + supplements (Vitamin C, Vitamin E, Vitamin D, Folate), prenatal air pollution (PM2.5) and allergic disease outcomes in adolescence. Plots show the estimated relationship between log-transformed z scores of exposures (z) and outcomes; shaded areas indicate 95% credible intervals. Plots are shown for outcomes FeNO (A) and Total Serum IgE (B).
In addition to modeling exposure to BC as an air pollutant, we also considered exposure to PM2.5 (Table 4, Fig. 2). PM2.5 was associated with a 10.51% increase in FeNO (95% CI −0.78 to 16.63%) and a 25.6% increase in serum total IgE (95% CI 9.34 to 44.29%). Plots of BKMR results for the effects of one exposure at various levels of another exposure showed an interaction between PM2.5 and Vitamin E intake from foods plus supplements. As shown in Fig. 3, Vitamin E is associated with larger increases in FeNO when PM2.5 exposure is higher. This interaction was confirmed in a standard linear regression model (p = 0.02 for interaction term). For participants in the highest quartile of PM2.5 exposure, Vitamin E (food plus supplements) was associated with 8.42% increase in FeNO (95% CI −1.18 to 13.87%). For participants in the highest quartile of Vitamin E (food plus supplements) exposure, PM2.5 was associated with a 14.29% increase in FeNO levels (95% CI 0.49 to 20.94%). In contrast, no interaction between black carbon and vitamin E was observed in BKMR models for the FeNO outcome, and a test of the interaction term in linear regression models was not statistically significant (p = 0.75).
In addition to examining interactions amongst the exposures themselves, we examined potential sex interactions by conducting sex-stratified BKMR analyses and comparing sex-specific prenatal exposure-response curves (Fig. 4). Air pollutant exposure response associations were strongest for male participants. In stratified analyses, prenatal PM2.5 exposure was associated with FeNO in males (20.47% increase, 95% CI 2.52 to 41.56%) but not in females (−1.52% decrease, 95% CI −15.50 to 14.79%).The interaction between sex and PM2.5 exposure was reproduced in a linear model (p < 0.05 for interaction term). We did not detect any differences in exposure response curves by sex for the total serum IgE outcome.
We also examined other exposure combinations in two additional sets of models (models for PM2.5 exposure and food-based nutrient intakes (Supplemental Table 4) and models for black carbon exposure and Nutrients (Food + supplements) (Supplemental Table 5)). For brevity, and since main effects of exposures showed similar trends across all models, we present only the models in Table 3 (food-based nutrients and black carbon exposure) and Table 4 (nutrients from food plus supplements and PM2.5 exposure) in the main text.
Discussion
In this work, we used a state of the art, non-parametric statistical methodology, BKMR, to identify potential relationships between exposures mixtures encountered in prenatal life and biomarkers of allergic disease in adolescence. While interactions between prenatal nutrient and air pollutant exposures have been studied in the context of birth defects and childhood cognitive outcomes21,22, this is the first study, to our knowledge, that considers how these types of prenatal exposure mixtures may relate to childhood allergic disease. We hypothesized that exposure to prenatal nutrients, particularly antioxidants, would have protective effects, and that these protective nutrients would interact with prenatal air pollutant exposures to diminish their adverse effects on childhood allergic disease. In keeping with our hypothesis, we observed that higher prenatal intakes of n-3 polyunsaturated fatty acids (a potential immunomodulatory agent), vitamin D (an antioxidant and immunomodulatory agent) and folate were associated with lower levels of allergic disease biomarkers. In contrast with other nutrients, total vitamin E intake in pregnancy appeared to amplify the adverse effect of prenatal exposure to PM2.5 on FeNO measured in adolescence, suggesting a synergy between these two exposures. The effects of protective nutrients were consistent across all levels of background air pollution exposure, which suggests that there was no statistical interaction between these two exposure types. However, when considering additive effects, it is clear that protective nutrients may help reduce the overall impact of adverse exposures.
In our study, average folate intake over the 1st and 2nd trimesters (specifically from foods) showed a borderline association with lower concentrations of FeNO in adolescence, but showed no association with total serum IgE levels. Prenatal folate intake and allergic disease risk has been examined in multiple previous reports, with inconsistent results. Some reports show no association with folate23,24, but others demonstrate associations between prenatal folate and increased risk of atopy, early childhood asthma or eczema25,26,27,28,29. Differences across studies may stem from variation in prenatal exposure window (early vs. late pregnancy), underlying genetic susceptibility (maternal history of allergic disease and/or MTHFR genotype), and dose of folate. We observed a potential protective association for higher dietary prenatal folate and lower adolescent FeNO within a fairly low exposure range (150 to 1200 μg/day), which is well below the levels of supplemental folate that have been linked to increased allergic disease risk. Although the potential mechanism of action for folate on asthma/allergy phenotypes has yet to be elucidated, its role as a methyl donor suggests that effects of prenatal folate could be mediated via epigenetic modifications. However, our observation of suggestive protective associations with intake from diet alone, suggests that folate (found naturally in green leafy vegetables and other food), but not folic acid (the form found in supplements), may be responsible for the observed protective associations.
Two other prenatal nutrients with immunomodulatory potential, n-3 polyunsaturated fatty acids and vitamin D, were also associated with lower FeNO levels in our study. n-3 polyunsaturated fatty acids also showed protective effects with similar (although not statistically significant) effect sizes for total serum IgE. In Project Viva, we have previously reported a lower risk of mid childhood atopy and allergic rhinitis with more vitamin D intake in pregnancy30. The results of the current study extend these findings by examining a biomarker of allergic disease (FeNO) at a later time point. In addition to our Project Viva findings, results from clinical trials also show reduced childhood allergic disease risk with higher intakes of these prenatal nutrients. A recent randomized controlled trial published in the New England Journal of Medicine showed lower rates of persistent wheeze or asthma in children whose mothers were supplemented with 2.4 g n−3 polyunsaturated fatty acids (in fish oil) vs. olive oil starting at 24 weeks gestation31. Secondary analyses of the VDAART randomized trial demonstrate lower odds of early childhood asthma (OR = 0.42, 95% CI 0.19 to 0.91) when prenatal supplementation of 4400 IU/day Vitamin D is administered to women with baseline Vitamin D serum levels of 30 ng/ml or above32. Mechanistic evidence exists for how both n-3 polyunsaturated fatty acids and Vitamin D may alter immune phenotypes in utero that complements epidemiological findings. n−3 supplementation in pregnancy has been linked to increased cord blood DNA methylation of genes encoding Th1 and Th2 cytokine production33. Vitamin D inhibits Th1-cytokine synthesis and suppresses allergen-specific IgE in in vitro studies34, and is associated with expression of innate immune receptors (TLR9 and TLR2) in cord blood35. Vitamin D may also increase production of IL-10 in neonatal bronchial epithelium36. Thus, our findings for nutrients with immunomodulatory potential (Vitamin D and n−3 polyunsaturated fatty acids) and their influence on allergic disease biomarkers in adolescence are supported mechanistically by experimental data, and demonstrate protective associations that extend beyond those observed in clinical trials (which are focused upon early childhood allergic disease outcomes).
In contrast to the other nutrients studied, total prenatal intake of Vitamin E (foods plus supplements) appeared to be associated with higher FeNO in adolescence, particularly in the context of higher PM2.5 levels. Prenatal exposure to PM2.5 has been associated with greater risk of childhood asthma and reduced lung function in a number of studies37; mechanisms of action are hypothesized to include oxidative stress and enhancement of pro-inflammatory cytokine production37,38. At high doses, Vitamin E is known to have pro-oxidant effects, which may be induced by the production of α-tocopheroxyl radicals. The pro-oxidant influences of high levels of Vitamin E and PM2.5 combined might explain the potential synergy between the two exposures detected in our analysis of FeNO. Interestingly, we did not observe a similar interaction for the total serum IgE outcome in adolescence. Although there is significant overlap between both of the allergic disease biomarkers considered in our study, we may have had more power to detect an association with FeNO. FeNO is more representative of lung-specific Th2 inflammation, while circulating IgE levels are instead a systemic, rather than compartment specific, biomarker. Even though there was no interaction with Vitamin E, PM2.5 exposure was as an independent predictor of relatively large increases (~25%) in total serum IgE measured in adolescence.
We also uncovered an interaction with sex. In male participants, we observed a strong association between prenatal PM2.5 levels and increased FeNO in adolescence, but exposure response curves for this association were essentially flat in female participants (Fig. 4). Others have reported important sex interactions for PM2.5 exposure. Hsu and colleagues showed that prenatal PM2.5 exposure is related to increased asthma incidence in males, but not females17. Underlying sex differences in prenatal lung development may in part explain the unique susceptibility of males to PM2.5.
In this work, we chose to focus on 3rd trimester air pollutants because the third trimester is an active period of lung development, with potential import for airway inflammatory outcomes in childhood and adolescence, and because exposure assessments for this trimester were most complete for PM2.5. We also tested 1st and 2nd trimester black carbon exposures in our models for FeNO and IgE (data not shown), but found the strongest associations for 3rd trimester exposures.
There were some limitations to our study. For maternal dietary assessment, we used intakes based on food frequency questionnaires from the 1st and 2nd trimester, rather than direct serum measurements. However, the food frequency questionnaire used to capture nutrient intakes has been validated for use in pregnancy, and the assessment of nutrient intakes at two time points strengthens the reliability of our exposure assessments. Prenatal exposure to 3rd trimester air pollutants did not directly overlap with our nutrient assessments from the 1st and 2nd trimesters. It is possible that we would have observed more interaction effects if we had data on 3rd trimester nutrient intakes that were concurrent with air pollutant exposures; however the 1st and 2nd trimester nutrient intakes are likely to be reasonable approximations of dietary intakes in the 3rd trimester. We assessed air pollution exposure by PM2.5, and black carbon (a component of PM2.5), but did not interrogate additional PM components, many of which may have import for health effects. Lastly, we considered only prenatal exposures. Cumulative exposures to nutrients and air pollutants from the prenatal period through early adolescence are likely important, but were beyond the scope of this analysis.
Our study also had several strengths. Use of the BKMR methodology to model our exposures of interest enabled us to detect interactions between exposure components, as well as possible non-linear dose response effects, such as those observed for Vitamin D. To our knowledge, this is the first study to examine interactions of prenatal exposures on allergic disease outcomes in this way. Our findings show that relationships between prenatal exposures and allergic disease may extend beyond early childhood and into adolescence. For many of the nutrients examined, we were able to study the effect of the nutrients from foods alone, as well as the effects of nutrients from foods and supplements combined. Direct measurement of these disease biomarkers is advantageous, as they may better capture underlying disease processes as compared to parental report of diagnoses and symptoms. Prenatal exposure mixture studies like the one presented here may ultimately be extended to incorporate effect modification by polymorphisms in relevant genes (i.e. MTHFR for folate and VDR for Vitamin D response) and/or mediation of exposure effects through intermediary “–omics” biomarker profiles (such as epigenetic, gene expression or metabolomics assessments).
In summary, we found that greater maternal intakes of vitamin D, folate, and n-3 fatty acids were associated with less airway inflammation in adolescence, while other nutrients (vitamin E), and air pollutants were associated with higher inflammation. Prenatal exposure interactions may play an important role, as evidenced by the potential synergy between vitamin E and PM2.5. We also observed potential protective effects of prenatal nutrients (n-3 PUFAs) and adverse associations with prenatal air pollution exposure for a second allergic disease biomarker (total IgE) in adolescence. Whenever possible, exposure interactions in prenatal life should be examined in studies of chronic disease outcomes in childhood. Understanding how prenatal exposures, particularly in the context of mixtures, influence allergic disease in childhood may ultimately inform the design of prenatal intervention trials to reduce the incidence of these disorders.
Methods
This study involved women and their children enrolled in Project Viva, an ongoing longitudinal pre-birth cohort study. The design of this cohort study has been described in detail elsewhere39. The study was approved by the Brigham and Women’s Hospital Institutional Review Board and the Harvard Pilgrim Health Care Institute Institutional Review Board. All methods were performed in accordance with the guidelines and regulations of these institutional review boards. Mothers provided informed consent at enrollment and for their child during follow-up visits, and children gave verbal assent. Participants were recruited into Project Viva at 8 offices of Atrius Harvard Vanguard Medical Associates in Eastern Massachusetts between 1999 and 2002. Exclusion criteria were multiple gestation, inability to answer questions in English, plans to move out of the study area before delivery of the infant, and gestational age ≥ 22 weeks at the time of presentation for prenatal care. We saw mothers during the first and second trimesters of pregnancy, and both mothers and children at delivery and periodic postnatal research visits, most recently when children reached adolescence (the “Early Teen” visit at median 12.9 years, range 11.9 to 16.6 years). At this visit, we measured respiratory function and collected blood.
Of the 2,128 women who delivered a live infant, we excluded 270 who were missing all prenatal exposure data (nutrient intakes and air pollution exposure estimates), and 22 who were missing relevant covariates. Of the 1,836 mother-infant pairs with available exposures and covariate measures, 857 (47%) had child’s FeNO and 590 (32%) had child’s total IgE measured at the Early Teen visit. Comparison of the 2,128 participants to the 1,836 mother-infant pairs with measured exposures and covariates showed some differences. For example, maternal pre-pregnancy body mass index (BMI) was lower for participants with exposure measures (mean 24.6 vs. 26.5 kg/m2, t-test p value = 0.0001). A larger percentage of participants with prenatal exposures measures were white (67 vs. 39%), and highly educated (68% with a college degree vs 36%), but the two groups did not differ on maternal history of hay fever. Comparisons between the 1,836 participants with exposure and covariate data and those with FeNO and total IgE outcome data in adolescence are shown in Supplemental Table 1.
Prenatal Dietary Nutrients and Supplement Intakes
During both the first and second trimesters, data on prenatal nutrient intakes were gathered using semi-quantitative food frequency questionnaires (FFQs) validated specifically for use in pregnancy40.We used the average of 1st and 2nd trimester FFQ derived nutrient intakes for our analyses. Use of these questionnaires in the Project Viva cohort have been described previously41,42. For first trimester data, the time referent was “during this pregnancy” (i.e. from the date of the last menstrual period until the assessment at a median of 9.9 weeks gestation at enrollment). The time referent for second trimester intakes collected by FFQ at the second visit (at 26–28 weeks gestation) was “during the past 3 months”. We did not administer a full FFQ that covered diet during late pregnancy, but we have found that diet was fairly stable across the first and second trimesters43. In addition to the FFQ, we also gathered data on vitamin and supplement intakes, including information on dose, duration of use, brand or type of multivitamin, prescribed prenatal vitamins and supplement use by the mother during both the first and second trimesters. We estimated individual nutrient intakes using the Harvard nutrient-composition database, which contains food composition values from the US Department of Agriculture, supplemented by other data sources44. We used mean nutrient intakes from the first and second trimesters as the exposures in the analyses, adjusted for total energy intake by the nutrient residual method45. If a participant completed only one FFQ, we used that value for the exposure variable.
Prenatal Air Pollutant Exposures
We estimated third trimester air pollutant exposures of interest, residence-specific 3rd trimester black carbon (BC) and PM2.5, using validated spatio-temporal regression models. Methodology for generating daily estimates of these exposures has been published elsewhere46,47. Briefly, daily residence-specific BC estimates were generated from a spatiotemporal regression model that contained land-use predictors (e.g., cumulative traffic-density within 100 m of a given location), meterological terms, and a smooth term of longitude and latitude. This model was applied separately for predictions in the warm (May-October) and cold (November-April) seasons. For BC estimates obtained using this spatiotemporal land-use regression model, the mean “out-of-sample” R2 was 0.73. For PM2.5 exposure estimates, we used a spatiotemporal prediction model that uses 10 × 10 km resolution daily satellite remote sensing data on aerosol optical depth (AOD) from the NASA MODIS satellite, land use terms, and meterological factors. The models first calibrate the remote sensing AOD data to observed PM2.5 ground monitoring data while accounting for land use and meterological factors. A second stage uses generalized additive models to fill in missing AOD data, due to cloud cover, snow, or other factors, using regional measured PM2.5, AOD values in neighboring cells, and land use terms. A final third stage uses fine-scale spatial information at 100 m resolution to account for very local traffic particle emissions. Daily PM2.5 exposure estimates at each residence yielded mean “out-of-sample” R2 of 0.83 for days having AOD remote sensing data and 0.81 for days without48. Participants reported their residential address at enrollment and updated it at the end of the second trimester and shortly after birth. All air pollution exposure estimates account for any moves during pregnancy. Third trimester exposure estimates were calculated by averaging daily exposures from the 188th day after LMP (last menstrual period) to the day before birth. We chose to model 3rd trimester air pollutant exposures, as 1) the third trimester is a very active period of lung development49 and therefore a biologically plausible window of vulnerability for airway inflammatory outcomes in childhood (i.e. FeNO) and 2) satellite model data for PM2.5 was available starting in the year 2000 (and therefore the 3rd trimester exposure data were most complete for mothers who enrolled at the beginning of the study, which began in 1999).
Fractional Exhaled Nitric Oxide (FeNO) Measurement
Nitric oxide (NO) is a mediator involved in chronic inflammatory diseases and Th2-mediated immune responses50. Measurement NO in exhaled air, as fractional exhaled nitric oxide (FeNO), is a non-invasive biomarker of airway inflammation that correlates with airway eosinophilia51. We measured FeNO levels with a portable electrochemical device (NIOX MINO; Aerocrine AB, Stockholm, Sweden), which is in agreement with published procedures for FeNO measurement52. Before FeNO measurement, participants breathed in through a nitric oxide scrubbing filter and exhaled out into the room air twice before inhaling a third time through the filter and exhaling into the FeNO analyzer. Exhaled FeNO measurements were conducted without a nose clip at a flow rate of 50 mL/s. (The last 3 seconds of the exhalation was used for FeNO measurement to ensure quantification of lower rather than upper airway FeNO). In accordance with American Thoracic Society guidelines, we did not use nose clips because blocking the nasal passages can cause exhaled nitric oxide to accumulate in the nose and potentially leak into the exhaled air stream through the posterior nasopharynx52. This procedure was performed twice, so that each subject had two FeNO measurements. The mean of these two measurements was used in data analysis.
Total IgE Measurement
Of the 1,836 children with prenatal exposure assessment for air pollutants and nutrients, 706 had blood drawn at school age for additional studies, of whom 590 had sufficient sample to measure serum total IgE by using ImmunoCAP (Phadia, Uppsala, Sweden).
Covariates
At enrollment mothers completed questionnaires reporting their education, history of atopy, smoking habits, and pre-pregnancy height and weight, from which we calculated BMI. On postpartum questionnaires, mothers reported child race/ethnicity. We obtained child sex and date of birth from hospital birth records.
Statistical Analysis
We applied Bayesian Kernel Machine Regression (BKMR)20, which estimates the multivariable exposure-response function of the prenatal nutrients and air pollutant exposures with each of our two outcomes (FeNO and IgE levels). BKMR is a flexible modeling approach that allows for a non-linear and non-additive (e.g., interactive) exposure-response relationships, and which simultaneously provides measures of variable importance (posterior inclusion probabilities). Using BKMR, it is possible to estimate a flexible exposure-response function (denoted h(z)). For each BKMR model, we performed 10,000 iterations. We applied the hierarchical variable approach in order to rank the importance of exposure groups in association with FeNO and total serum IgE level measured at the early teen visit. Prenatal maternal exposures of interest were residence-specific air pollutants (3rd trimester BC or PM2.5,) and nutrient intakes (1st and 2nd trimester averaged energy-adjusted dietary intakes of vitamins D, C, and E, β-carotene, folate, choline, and n-3 and n-6 polyunsaturated fatty acids). We conducted secondary analyses with nutrient intakes derived from supplements and food combined. We modelled all nutrients in the same exposure group except vitamin E and β-Carotene, which demonstrated associations with FeNO in the direction opposite to that observed for other nutrients. In our BKMR model specification, we grouped the exposures into 3 different groups, vitamin E and β-Carotene (group 1), all of the other nutrients (group 2), and the air pollutant (either PM2.5 or BC) exposure (group 3) and conducted hierarchical variable selection on these groups of exposures. In particular, under the hierarchical variable selection formulation, BKMR simultaneously identifies (1) whether there are particular groups of exposures that are associated with the outcome, and (2) which exposures within the group may be driving the association between that group of the pollutants with the outcome by calculating group-specific importance measures, which are referred to as ‘posterior inclusion probabilities’. We used posterior inclusion probabilities from the BKMR model, which is an importance score, to rank the strength of association between each exposure group and the outcome. Models were adjusted for maternal education, hay fever, pre-pregnancy BMI, and smoking in pregnancy, and child sex, race/ethnicity, season of birth, and sine and cosine of time of outcome measure to adjust for confounding by seasonal trends in both the outcome and the exposure. Exposure covariates were expressed as z-scores of log-transformed exposures and we report effects in % change in FeNO or IgE z-per interquartile range (25th to 75th percentile) increase in exposure. Since BC is a component of PM2.5, we modeled the two air pollutant exposures separately. In all, four combinations of variable types were run in BKMR analyses: Model 1: Nutrients (foods only) + BC air pollutant; Model 2. Nutrients (foods only) + PM2.5 air pollution; Model 3: Nutrients (foods + supplements) + BC, Model 4: Nutrients (foods + supplements) + PM2.5 air pollution. Models 1 and 4 are presented in the main text for the outcomes FeNO and serum total IgE. Results of models 2 and 3 are shown in the supplement. We confirmed the main effects and interactions estimated in the BKMR analyses with standard parametric regression models with interaction terms. We refer to associations as statistically significant if 95% posterior credible intervals exclude the null.
References
Holt, P. G. & Jones, C. A. The development of the immune system during pregnancy and early life. Allergy 55, 688–697 (2000).
Dietert, R. R. & Zelikoff, J. T. Early-life environment, developmental immunotoxicology, and the risk of pediatric allergic disease including asthma. Birth defects research. Part B, Developmental and reproductive toxicology 83, 547–560 (2008).
Grieger, J. A. et al. In utero Programming of Allergic Susceptibility. International archives of allergy and immunology 169, 80–92 (2016).
Khan, T., Palmer, D. & Prescott, S. In-utero exposures and the evolving epidemiology of paediatric allergy. Current Opinion in Allergy and Clinical Immunology 15, 402–408 (2015).
Jedrychowski, W. A. et al. Effect of prenatal exposure to fine particulate matter on ventilatory lung function of preschool children of non-smoking mothers. Paediatr. Perinat. Epidemiol. 24, 492–501 (2010).
Deng, Q., Lu, C., Li, Y., Sundell, J. & Dan, N. Exposure to outdoor air pollution during trimesters of pregnancy and childhood asthma, allergic rhinitis, and eczema. Environ. Res. 150, 119–127 (2016).
Chiu, Y. H. et al. Effects of prenatal community violence and ambient air pollution on childhood wheeze in an urban population. J. Allergy Clin. Immunol. 133, 22.e4 (2014).
West, C. E. et al. Associations between maternal antioxidant intakes in pregnancy and infant allergic outcomes. Nutrients 4, 1747–1758 (2012).
Maslova, E. et al. Vitamin D intake in mid-pregnancy and child allergic disease - a prospective study in 44,825 Danish mother-child pairs. BMC pregnancy and childbirth 13, 199 (2013).
Vereen, S. et al. The association of maternal prenatal vitamin D levels and child current wheeze. Ann Allergy Asthma Immunol. 120, 98–99 (2018).
McEvoy, C. T. et al. Vitamin C supplementation for pregnant smoking women and pulmonary function in their newborn infants: a randomized clinical trial. JAMA 311, 2074–2082 (2014).
Allan, K. M. et al. Maternal vitamin D and E intakes during pregnancy are associated with asthma in children. European Respiratory Journal 45, 1027–1036 (2015).
Greenough, A., Shaheen, S. O., Shennan, A., Seed, P. T. & Poston, L. Respiratory outcomes in early childhood following antenatal vitamin C and E supplementation. Thorax 65, 998–1003 (2010).
Martindale, S. et al. Antioxidant Intake in Pregnancy in Relation to Wheeze and Eczema in the First Two Years of Life. American Journal of Respiratory and Critical Care Medicine 171, 121–128 (2005).
Beckhaus, A.A. et al. Maternal nutrition during pregnancy and risk of asthma, wheeze, and atopic diseases during childhood: a systematic review and meta-analysis. Allergy 70, 1588–604 (2015).
Goldring, S. T. et al. Prenatal vitamin d supplementation and child respiratory health: a randomised controlled trial. PloS one 8, e66627 (2013).
Hsu, H. H. et al. Prenatal Particulate Air Pollution and Asthma Onset in Urban Children. Identifying Sensitive Windows and Sex Differences. Am. J. Respir. Crit. Care Med. 192, 1052–1059 (2015).
Wu, L. C. & Zarrin, A. A. The production and regulation of IgE by the immune system. Nature Reviews: Immunology 14, 247–259 (2014).
Kim, H., Eckel, S. P., Kim, J. H. & Gilliland, F. D. Exhaled NO: Determinants and Clinical Application in Children With Allergic Airway Disease. Allergy, Asthma & Immunology Research 8, 12–21 (2016).
Bobb, J. F. et al. Bayesian kernel machine regression for estimating the health effects of multi-pollutant mixtures. Biostatistics 16, 493–508 (2015).
Stigone, J.A. et al. Maternal exposure to nitrogen dioxide, intake of methyl nutrients and congenital heart defects in offspring. Am J Epidemiol. May 18 [epub ahead of print] (2017).
Guxens, M. et al. Prenatal exposure to residential air pollution and infant mental development: modulation by antioxidants and detoxification factors. Environ. Health Perspect. 120, 144–149 (2012).
Magdelijns, F. J., Mommers, M., Penders, J., Smits, L. & Thijs, C. Folic acid use in pregnancy and the development of atopy, asthma, and lung function in childhood. Pediatrics 128, 135 (2011).
Crider, K. S. et al. Prenatal folic acid and risk of asthma in children: a systematic review and meta-analysis. Am. J. Clin. Nutr. 98, 1272–1281 (2013).
Haberg, S. E. et al. Maternal folate levels in pregnancy and asthma in children at age 3 years. J. Allergy Clin. Immunol. 127(4), 264.e1 (2011).
Granell, R. et al. The association between mother and child MTHFR C677T polymorphisms, dietary folate intake and childhood atopy in a population-based, longitudinal birth cohort. Clin. Exp. Allergy 38, 320–328 (2008).
Whitrow, M. J., Moore, V. M., Rumbold, A. R. & Davies, M. J. Effect of supplemental folic acid in pregnancy on childhood asthma: a prospective birth cohort study. Am. J. Epidemiol. 170, 1486–1493 (2009).
Yang, L. et al. High dose of maternal folic acid supplementation is associated to infant asthma. Food Chem. Toxicol. 75, 88–93 (2014).
Parr, C. L. et al. Maternal Folate Intake during Pregnancy and Childhood Asthma in a Population-based Cohort. Am. J. Respir. Crit. Care Med. 195, 221–228 (2017).
Bunyavanich, S. et al. Prenatal, perinatal, and childhood vitamin D exposure and their association with childhood allergic rhinitis and allergic sensitization. J. Allergy Clin. Immunol. 137, 2 (2016).
Bisgaard, H. et al. Fish Oil-Derived Fatty Acids in Pregnancy and Wheeze and Asthma in Offspring. N. Engl. J. Med. 375, 2530–2539 (2016).
Wolsk, H. et al. Vitamin D supplementation in pregnancy, prenatal 25(OH)D levels, race, and subsequent asthma or recurrent wheeze in offspring: Secondary analyses from the Vitamin D Antenatal Asthma Reduction Trial. J Allergy Clin Immunol. 2017 Mar 9 [epub ahead of print].
Lee, H. S. et al. Modulation of DNA methylation states and infant immune system by dietary supplementation with omega-3 PUFA during pregnancy in an intervention study. Am. J. Clin. Nutr. 98, 480–487 (2013).
Comberiati, P. et al. Is vitamin D deficiency correlated with childhood wheezing and asthma? Front Biosci (Elite Ed). 6, 31–9 (2014).
Hornsby, E. et al. Vitamin D supplementation during pregnancy: Effect on the neonatal immune system in a randomized controlled trial. J Allergy clin Immunol. 141, 269–278 (2018).
Miller, D. R. et al. Maternal vitamin D and E intakes during early pregnancy are associated with airway epithelial cell responses in neonates. Clin. Exp. Allergy 45, 920–927 (2015).
Wright, R. J. & Brunst, K. J. Programming of respiratory health in childhood: influence of outdoor air pollution. Curr. Opin. Pediatr. 25, 232–239 (2013).
Xu, X. et al. Association of systemic inflammation with marked changes in particulate air pollution in Beijing in 2008. Toxicol. Lett. 212, 147–156 (2012).
Oken, E. et al. Cohort profile: project viva. Int. J. Epidemiol. 44, 37–48 (2015).
Fawzi, W. W., Rifas-Shiman, S. L., Rich-Edwards, J. W., Willett, W. C. & Gillman, M. W. Calibration of a semi-quantitative food frequency questionnaire in early pregnancy. Annals of Epidemiology 14, 754–762 (2004).
Oken, E., Kleinman, K. P., Olsen, S. F., Rich-Edwards, J. W. & Gillman, M. W. Associations of seafood and elongated n-3 fatty acid intake with fetal growth and length of gestation: results from a US pregnancy cohort. Am. J. Epidemiol. 160, 774–783 (2004).
Gillman, M. W., Rifas-Shiman, S. L., Kleinman, K. P., Rich-Edwards, J. W. & Lipshultz, S. E. Maternal calcium intake and offspring blood pressure. Circulation 110, 1990–1995 (2004).
Rifas‐Shiman, S. L. et al. Changes in dietary intake from the first to the second trimester of pregnancy. Paediatric and Perinatal Epidemiology 20, 35–42 (2006).
US Department of Agriculture ARS. USDA national nutrient database for standard reference, release 14. Washington, DC: US Department of Agriculture, (2001).
Willett, W. C. Implications of total energy intake for epidemiologic studies of breast and large-bowel cancer. Am. J. Clin. Nutr. 45, 354–360 (1987).
Zanobetti, A. et al. Associations between arrhythmia episodes and temporally and spatially resolved black carbon and particulate matter in elderly patients. Occup. Environ. Med. 71, 201–207 (2014).
Gyparis, A., Coull, B. & Schwartz, J. & Suh, h. Semiparametric latent variable regression models for spatio-teomporal modeling of mobile source particles in the greater Boston area. J Royal Stat Soc C (Appl Stat) 56, 183–209 (2007).
Kloog, I., Koutrakis, P., Coull, B. A., Lee, H. J. & Schwartz, J. Assessing temporally and spatially resolved PM 2.5 exposures for epidemiological studies using satellite aerosol optical depth measurements. Atmospheric Environment 45, 6267–6275 (2011).
Sharma, S. et al. The genomic origins of asthma. Thorax. 69, 481–7 (2014).
Pijnenburg, M. W. H. & De Jongste, J. C. Exhaled nitric oxide in childhood asthma: a review. Clinical & Experimental Allergy 38, 246–259 (2008).
Warke, T. J. et al. Exhaled nitric oxide correlates with airway eosinophils in childhood asthma. Thorax 57, 383–387 (2002).
Dweik, R. A. et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am. J. Respir. Crit. Care Med. 184, 602–615 (2011).
Author information
Authors and Affiliations
Contributions
J.E.S performed analyses, interpreted data and wrote manuscript. B.A.C. helped with air pollution exposure assessment, data interpretation, and also guided statistical analyses with BKMR methodology. J.B. guided statistical analyses with BKMR methodology. S.L.R. assisted with data management, data interpretation and manuscript editing. J.S. helped with data interpretation and manuscript editing. I.K. helped with air pollution exposure assessment, data interpretation and manuscript editing. H.G. helped with data management, data interpretation and manuscript editing. K.M.S. helped with data interpretation and manuscript editing. A.A.L. helped with data interpretation and manuscript editing. P.K. helped with air pollution exposure assessment, data interpretation and manuscript editing. D.R.G. conceived of the study design and assisted with data interpretation and manuscript writing. E.O. conceived of the study design and assisted with data interpretation and manuscript writing. All authors read, approved and commented on the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sordillo, J.E., Switkowski, K.M., Coull, B.A. et al. Relation of Prenatal Air Pollutant and Nutritional Exposures with Biomarkers of Allergic Disease in Adolescence. Sci Rep 8, 10578 (2018). https://doi.org/10.1038/s41598-018-28216-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-28216-0
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.