Abstract
This study aimed to examine the effectiveness of defibrinogen therapy on functional recovery and safety among 1332 consecutive ischemic stroke patients who had not received intravenous thrombolysis with recombinant tissue plasminogen activator. Stroke patients undergoing conservative and relatively individualized multiple-day dosing regimens of defibrinogen therapy between January 1, 2008 and May 30, 2016 were enrolled. Data were analyzed according to functional success (Barthel Index of 95 or 100, mRS of 0 or 1) and safety variables (intracranial hemorrhage, mortality and stroke recurrence). At 12 months, 18.62% (203/1087) of patients were lost to follow-up. The functional success rates were 39.84% (526/1320) and 42.23% (459/1087) as assessed by BI at 3 months and 12 months, respectively. Fifteen patients had asymptomatic intracranial hemorrhage within 24 hours after the initial defibrase administration. During the 14 days after hospitalization, 12 patients were diagnosed with symptomatic intracranial hemorrhage (sICH) and a total of 12 patients died from all causes. At 3 months, 56 patients were dead and 21 patients had recurrent stroke. The percentage of death and recurrence of stroke at 12 months were 6.81% and 3.22%, respectively. Results from the historical control showed no significant differences of functional success were detected between the patients treated with rt-PA within 6 hours of stroke onset in NINDS II and the patients treated with defibrase within 6 hours after stroke in the present study. The multiple-day dosing regimen of defibrinogen therapy using defibrase applied in the present study could achieve functional improvement among acute ischemic stroke patients, with low risks of mortality when compared with other similar studies. However, the efficacy and safety of such a defibrinogenating therapy is needed to be verified by RCTs with large sample size.
Similar content being viewed by others
Introduction
Stroke is a major cause of death and adult disability throughout the world1,2,3. Currently, at organized stroke units, intravenous thrombolysis with recombinant tissue plasminogen activator (IV rt-PA) administered within 3 to 4.5 hours after symptom onset and endovascular therapy with or without intravenous thrombolysis within 6 hours are proven to be beneficial in acute ischemic stroke4,5,6,7. However, the narrow therapeutic window and low recanalization rate in proximal vessel occlusions of intravenous thrombolysis and the limitation of application to acute stroke patients with posterior circulation occlusion restrict the utility of these specific interventions8,9,10. Thus, new effective therapeutic strategies must be explored.
Epidemiological studies have established that elevated fibrinogen levels are independently and highly associated with stroke and peripheral arterial disease11,12,13. Studies found strong correlations between high initial fibrinogen levels in acute ischemic stroke patients and poor prognosis for functional outcomes14,15. Fibrinogen-depleting agents lower blood plasma fibrinogen levels, reduce blood viscosity, increase local blood flow and hence inhibit further thrombus formation or extension16,17,18. This drug-induced hypofibrinogenemia also promotes release of plasminogen activator with concomitant reductions in plasmin inhibitor and plasminogen activator inhibitor19. Fibrinogen-depleting agents have been used as reperfusion therapy for treatment of deep vein thrombosis, central retina venous thrombosis and peripheral vascular disorders since the 1970s in Europe and Canada20,21,22. However, prior randomized controlled trials (RCTs) reported inconsistent conclusions in terms of influence of fibrinogen depleting agents on functional outcomes of acute stroke patients18,19,23,24,25,26,27,28,29. Some studies showed fibrinogen depleting agents delivered in acute ischemic stroke patients did not improve them outcome and revealed a tread to increase bleeding23,24,29, while other researchers demonstrated fibrinogen depleting agents had a favorable benefit-risk profile for patients with acute ischemic stroke18,19,25,26,27,28. In the latest meta-analysis of fibrinogen depleting agents for acute ischemic stroke30, results showed that fibrinogen depleting agents marginally reduced the proportion of patients who were deed or disabled at the end of follow-up (risk ratio (RR): 0.95; 95% confidence interval (CI): 0.90–0.99; P = 0.02) and decreased the stroke recurrences (RR: 0.67; 95% CI 0.49–0.92; P = 0.01)30. In the meta-analysis, although the risk of symptomatic intracranial hemorrhage (sICH) was higher in fibrinogen depleting agent treatment group compared with the control group30, the risk could reduce as long as fibrinogen levels and other coagulation values were carefully controlled18. Moreover, factors such as time to treatment, dosing regimen and patient selection may influence the results16,30.
Hence, in the present study, which aimed to investigate the effectiveness and safety of a conservative and relatively individualized multiple-day dosing regimen of defibrinogenating agents in patients with ischemic stroke within 72 hours of recognized symptom onset, plasma fibrinogen level and global coagulation tests such as activated partial thromboplastin time (APTT), prothrombin time (PT), thrombin time (TT) were monitored carefully during each use of defibrase to reduce bleeding events, such as sICH and to confirm the safety. What’s more, we applied defibrase as interventional fibrinogen depleting agent other than ancrod (another kind of fibrinogen depleting agent) to reduce the risk of sICH, which in accord with the subgroup analysis of meta-analysis showed defibrse tend to be associated with the lower risk of sICH (RR: 1,15; 95% CI: 0.60–2.20) than ancrod (RR: 3.56; 95% CI: 2.15–5.87)30.
Methods
Study participants
This study was performed in compliance with the Declaration of Helsinki and approved by the Independence Ethics Committee of the Shanghai Fifth People’s Hospital Affiliated to Fudan University (ethic approval number: 2017-ETRE-059).
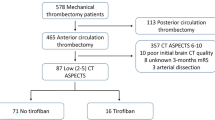
We conducted a retrospective review of a prospectively obtained dataset on all acute ischemic patients treated conservatively in our hospital from January 1, 2008 to May 30, 2016 who received defibrase (a defibrinogenating agent extracted from Agkistrodon acutus venom, 5 U/vial). Adults with an acute moderate or severe neurological deficit (pretreatment NIHSS 5–22) suggestive of ischemic origin were eligible for defibrinogen therapy. Defibrinogen therapy could be given within 72 hours after stroke symptom onset. Subjects with clinical or neuroimaging evidence of intracranial extravascular blood or obvious bleeding tendencies, or with pretreatment plasma fibrinogen levels below 1.5 g/L or persistent hypertension (systolic blood pressure >180 mmHg or diastolic blood pressure >110 mmHg), were excluded (Appendix 1). Patients had used or intended to use of thrombolytic agents including IV rt-PA were excluded. The patients who were not qualified to receive IV rt-PA, such as patients were missed the therapeutic window of IV rt-PA, patients or family members were unwilling to receive rt-PA and patients were over 80 years of age, were considered receiving the defibrinogen therapy.
Written informed consent documents were signed by the patients or their representatives before treatment.
Dosing regimen of defibrase
A conservative and relatively individualized multiple-day dosing regimen of defibrase was adopted. Theoretically, each eligible patient should receive intravenous infusions of defibrase three times, on the 1st, 3rd and 5th days (defining the day of the initial infusion as the first day). However, the number of times and time interval of infusion depended on the concrete specifics of the situation. Brain CT scanning was conducted within 24 hours after initial infusion of defibrase. If the results of the CT scan presented intracranial hemorrhage, the subsequent infusions were prohibited. If not, the second or third infusion was given based on the fibrinogen level measured on the 3rd day after the previous infusion. On the one hand, theoretically, each eligible patient should receive intravenous infusions of defibrase three times at the 1st, 3rd and 5th day (presumed that the day receiving the initial infusion as the first day). But the number of times and time interval of infusion depended on fibrinogen level. Fibrinogen level was measured before every defibrase infusion, when fibrinogen level was less 1.5 g/L, defibrase infusion was prohibited absolutely (lower than 1.5 g/L for three consecutive days, measured once a day) or delay until next measurement of fibrinogen level was more than 1.5 g/L (lower than 1.5 g/L for once or twice, measured once a day). Hence, patients may receive the defibrase infusion once, twice or three times, and patients received the defibrase infusion in the first day for the initial infusion, the 3th, or 4th or 5th day for the second infusion (Fig. 1). On the anther hand, when fibrinogen level was between 1.5 g/L and 2.0 g/L, the dose was 5 U; when fibrinogen level was over 2.0 g/L, the dose was 10 U (Fig. 1). Defibrase (10 U or 5 U) was diluted into 250 mL saline and administered at the same infusion rate (30 drops per min). Eligible patients were not allowed to receive thrombolytic agents, antiplatelet drugs, anticoagulants, heparin, or other agents that might influence the fibrinolytic system. After completion of defibrinogen therapy, patients were permitted to receive prophylactic measures (such as antiplatelet or anticoagulant drugs) as required.
Data collection and outcome measures
All pretreatment and posttreatment data were collected from the hospital’s electronic medical system and recorded in a review-board-approved electronic database. The data parameters collected from pretreatment included age, gender, smoking status, blood pressure, time to treatment, National Institute of Health Stroke Scale (NIHSS) score, and history of hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, transient ischemic attack (TIA) and stroke. Hematology parameters and global coagulation tests such as APTT, PT, and TT were measured before treatment and on the 14th day after admission. Plasma fibrinogen level was measured before pretreatment (Fib-i), on the 3rd day after each infusion of defibrase (Fib-1st, Fib-2nd, Fib-3rd) and on the 14th day after admission (Fib-14d).
The efficacy end points of efficacy included the Barthel Index (BI) and the modified Rankin scale (mRS) at 3 months and 12 months after defibrinogen therapy. A BI score of 95 or 100 and an mRS score of 0 or 1 at 3 months and 12 months were defined as functional success. The safety end points consisted of asymptomatic intracranial hemorrhage within 24 hours after the initial defibrase treatment (detected by a repeat CT scan); symptomatic intracranial hemorrhage (sICH); bleeding at other sites; coagulation tests and special hematology profiles during the first 14 days after admission; mortality at the 14th days after admission, 3 months and 12 months; and recurrence of stroke at 3 months and 12 months.
Statistical analyses
The normality of the data distribution was evaluated by the Shapiro-Wilk test. Data were presented as the means, standard deviation, medians or ranges for continuous variables and percentages for categorical variables. Descriptive statistical analyses and paired-sample t-tests were performed for demographic data, hematology and coagulation function indicators. Distribution of the percentages of functional success in difference variables were analyzed by using the chi-squared statistic, Fisher’s exact test or the Cochran-Mantel-Haenszel chi-squared test. Collinearity diagnosis tests were performed to determine whether there was multicollinearity among variables (age, initial NIHSS score, smoking or not, initial fibrinogen level, time to treatment, number of times defibrase was given and dose of defibrase), which may influence the independent roles of variables or the degree of correlation between them in the multivariate regression model. Logistic regression analysis was used to estimate odds ratios for functional success at 12 months. Potential covariates, such as age, gender, smoking, high risk of factors, history of prior TIA or stroke, initial NIHSS score, initial fibrinogen level, time to treatment, the number of uses of defibrase and the total dose of defibrase, were first calculated in univariate analyses, and factors that showed significant in univariate analyses were furtherly introduced to the multivariable modeling. The statistical tests were 2-sided and at the 5% significance level. Analyses were conducted using IBM SPSS version 19.0 statistical software.
Results
Demographics and dosing characteristics
A total of 1332 patients who received defibrinogen therapy from January 1, 2008 to May 30, 2016 were enrolled in this study. The patients had an average age of 65.4 years, and 55.3% were men. The median pretreatment NIHSS score was 9 with a range of 6 to 22. The median time to treatment was 37 hours, with only 7.0% of patients receiving defibrase within 6 hours of symptom onset. The mean level of initial fibrinogen was 3.2 g/L, and the majority of patients had levels of over 2.0 g/L (91.4%). Nine hundred twenty-twp (69.1%) of the patients received defibrase three times. The most common dose of defibrase (32.9% of patients) was 20 U. The complete demographics and dosing characteristics are listed in Table 1.
Hematology and coagulation function
Compared with pretreatment, the mean value of plasma viscosity (1.7 to 1.3 mPa/s), PLT (224 to 210 × 109/L), hemoglobin (141 to 138 g/L), Hct value (46.4 to 42.4%), platelet aggregation rate (65.9 to 57%) were all significantly lower on the 14th day after treatment. The changes in the mean values of APTT, PT and TT between pretreatment and the 14th day after admission attained statistical significance (difference in mean score: 8.60 s, 0.74 s and 3.35 s, respectively). All the hematologic and coagulation function parameters measured in the pretreatment and at the 14th day after admission were within the normal range according to our hospital’s test standard (Appendix 2).
Plasma fibrinogen levels consistently reduced from 3.18 ± 1.05 to 2.49 ± 1.03 to 2.29 ± 1.01 g/L from pretreatment (n = 1332) to the 3rd days after the first (n = 1317) and second infusions (n = 1135) of defibrase, reaching the lowest level after the third infusion (2.21 ± 0.83 g/L, n = 922). However, the plasma fibrinogen level increased to 2.67 ± 1.01 g/L on the 14th day after admission (n = 1320) (Fig. 2).
Changes in plasma fibrinogen levels. Fib-i: fibrinogen level measured at pretreatment; Fib-1st: fibrinogen level measured on the 3rd day after the first infusion of defibrase; Fib-2nd: fibrinogen level measured on the 3rd day after the second infusion of defibrase; Fib-3rd: fibrinogen level measured on the 3rd day after the third infusion of defibrase; Fib-14d: fibrinogen level measured on the 14th day after admission.
Outcomes and follow-up
Among the 1332 patients, within 24 hours of initial infusion of defibrase, repeated CT scan discovered that 15 patients had asymptomatic intracranial hemorrhage. During the 14 days after hospitalization, 12 were patients diagnosed with sICH, 12 patients died (five died of sepsis, three of sICH, three of severe pneumonia, and one from a heart attack), and 16 patients had bleeding at other sites (seven for ecchymosis or petechiae or bleeding gums, four for gastrointestinal bleeding, three for epistaxis, an two for hematuria). One hundred fifty-six patients (11.82%) were lost to follow-up after 3 months, and more patients (18.68%) failed to follow-up after 12 months. The differences of demographic (age, gender) and baseline clinical characteristics (high risk factors, stroke associated past history, hematology and coagulation function parameters, fibrinogen level and neurological function and condition of defibrase therapy) between the patients who were failed to follow-up and patients who were followed up at 3 months and 12 months were calculated. No significant differences were found between the two groups as listed in Appendix 3. The functional success rates were 39.84% assessed by BI score of 95 or 100 and 31.59% assessed by an mRS of 0 or 1 among 1320 patients at 3 months. At 12 months, the functional success rates were higher, reaching 42.23% by BI score and 42.13% by mRS among 1087 patients. At 3 months, among 1320 patients, 56 patients had died and 21 patients had suffered another stroke, accounting for 4.24% and 1.59%, respectively. The death and recurrence rate of stroke were 6.81% and 3.22% respectively, in 1087 patients at 12 months. The overall distribution of efficacy and safety outcomes, including mortality, recurrence rate of stroke and follow-up information at 3 months and 12 months, is shown in Fig. 3.
Overall distributions of Barthel Index score and mRS at 3 months and 12 months. mRS score of 0 and 1, and Barthel Index score of 95 and 100 were defined as functional success. For mRS, grades 0 or 1, 2 or 3, and 4 or 5 are considered as no or minimal disability, moderate disability, and severe disability, respectively. For Barthel Index, the higher scores demonstrated less severity of stroke. mRS: modified Rankin scale.
Appendix 4 shows the distribution by percentage of functional success of different initial fibrinogen levels, the numbers of administrations of defibrase, total doses of defibrase and time-to-treatment categories at 3 months and 12 months. Significant difference was found in different initial fibrinogen level (P = 0.017) and number of times of administration of defibrase (P = 0.049) measured by mRS of 0 or 1 at 3 months. The rates of functional success measured both by a Barthel Index of 95 or 100 and by mRS of 0 or 1 in different total dose of defibrase at 3 months and 12 months were significantly different (P < 0.01).
There was no obvious multicollinearity among variables, including age, initial NIHSS score, smoking or not, initial fibrinogen level, time to treatment, number of defibrase administrations and dose of defibrase. Factors of age, smoking, NIHSS score, initial fibrinogen level, time to treatment, the number of uses of defibrase and the total dose of defibrase showed significant in univariate analyses, and such factors were furtherly introduced to the multivariable analysis. Table 2 showed the results of multivariable analyses of the relation between demographics and dosing characteristics and the rate of functional success at 12 months. For the Barthel Index, analyses of the association between NIHSS score, initial fibrinogen (1.5~2.0 g/L), 10 U of defibrase, 15 U of defibrase and functional success yielded an adjusted odds ratio of 1.269 (95% CI: 1.022 to 1.576; P = 0.031), 1.697 (95% CI: 1.028 to 2.800; P = 0.039), 0.452 (95% CI: 0.210 to 0.9720; P = 0.042) and 0.520 (95% CI: 0.282 to 0.959; P = 0.036), respectively. For mRS, analyses of the association between smoking, 5 U, 15 U, 20 U, 25 U dose of defibrase showed an adjusted odds ratio of 1.760 (95% CI: 1.261 to 2.456; P = 0.001), 0.302 (95% CI: 0.120 to 0.761; P = 0.011), 0.225 (95% CI: 0.118 to 0.427; P < 0.001), 0.311 (95% CI: 0.177 to 0.545; P < 0.001) and 0.467 (95% CI: 0.267 to 0.815; P = 0.007), respectively.
Differences in functional success between the present study and the NINDS II
A landmark trial published in 1995 by the National Institute of Neurological Diseases and Stroke (NINDS) about rt-PA for treating acute ischemic stroke within 6 hours from stroke onset demonstrated that the likelihood of functional improvement (BI score of 95 or 100; mRS of 0 or 1) at three months was higher in the rt-PA treatment group than the control group, even though the difference of early stage outcome measured by NIHSS at 24 h after the onset of stroke was not significant between the two groups31. In NINDS II, there were 168 patients treated with rt-PA within 6 hours after stroke onset, and 84 of them obtained BI of 95 or 100, and 66 of them achieved mRS of 0 or 1. We compared the results that gained functional success at 3 months between the patients treated with defibrase within 72 hours after stroke onset in our study and 168 patients treated with rt-PA within 6 hours in NINDS II. As showed in Table 3, for outcome of BI of 95 or 100, NINDS II shows more effect in functional improvement than our study (P = 0.030); for outcome of mRS of 0 or 1, the difference between our study and NINDS II was not significant (P = 0.067). Furthermore, we compared the results of functional success from the 93 patients treated within 6 h after stroke onset in our study with that from 168 patients in NINDS II. No significant differences between our study and NINDS II were found (for BI: P = 0.194; for mRS: P = 0.423; Table 3). Lastly, the differences of mortality rate at 3 months between patients treated within 72 hours in our present study and patients treated within 6 hours in the study of NINDS, including NINDS I (n = 144) and NINDS II (n = 168) were calculated. Results showed that the rate of mortality was lower in our study (56/1320) than that in NINDS (54/312) at 3 months (P < 0.001).
Discussion
A homogeneous series of 1332 consecutive patients receiving a conservative and relatively individualized multiple-day dosing regimen of defibrase were observed in term of efficacy and safety in this study. The patients in this series were chosen with caution. The multiple-day dosing regimen extended the therapy window up to 72 hours after symptom onset. Defibrase has been used to treat strokes for decades. In previous studies, ischemic stroke patients were administered defibrinogenating agents (ancrod or defibrase) within 3 to 48 hours from stoke onset18,23,24,25,26,27,28. Additionally, a large multicenter randomized controlled trial was conducted to explore the effectiveness and safety of defibrase delivered within 24 hours after the onset of stroke symptom29. Fibrinogen level was regarded as a vital monitoring indicator in the current study. Whether to use of defibrase to treat stroke patients relied on plasma fibrinogen level measured before delivery. The variability of patients treated at different time points, with different doses, and with different courses of treatment were all depending on the plasma fibrinogen level. The reason for designing such a seemingly individualized protocol is to make sure each defibrase infusion is safety and cause less bleeding events. Strict patient selection, extended therapy window and cautious dosing regimen were applied to allow more eligible patients to receive defibrinogen therapy and to reduce the risk of hemorrhage as far as possible. This case series reported a conservative, moderate and relatively individualized defibrinogen therapy for the treatment of ischemic stroke patients in a time window of 72 hours from stroke onset for the first time.
In terms of Barthel Index score, according to worst-case-scenario intention-to-treat (ITT) analysis, the functional success rate at 3 months in our study was higher than that reported by the Cooperative Group for Reassessment of Defibrase in 2005 (39.84% versus 36.6%), in which patients also received defibrase as defibrinogenating agents within 12 hours of stroke onset25. However, other researchers have reported that functional success rate was higher than 39.84%, which included the patients whose Barthel Index score were less than 95 but at least equal to the pre-stroke value27. At 12 months, the functional success rate was further increased which was in line with the European Stroke Treatment with Ancrod Trial (ESTAT) report24. In addition, functional success was further investigated according to different categories. At 3 months, the differences of functional success rate assessed by mRS were statistically significant between groups with different initial fibrinogen level and among groups with different numbers of times treated with defibrase. Furthermore, significant differences were identified among groups with different total dose of defibrase for functional success rate both assessed by Barthel Index and mRS scores at 3 months and 12 months, however which doses was optimal for attaining functional success required further study. Unexpectedly, five different time-to-treatment groups had same effects on the functional success.
Regarding safety, the average of hematologic and coagulation function parameters at the 14th day was lower than that at admission, but all at normal levels which may be due to blood dilution caused by liquid supplement. In addition, the reduction of plasma fibrinogen level might result in a decrease in plasma viscosity and platelet aggregation rate. Therefore, the decreases of ATPP, PT and TT might be the combined results of the above. During defibrinogen therapy, symptomatic intracranial hemorrhage and death from all causes were lower most of the reported results. It may largely result from the close monitoring of fibrinogen level during the process of defibrinogenating therapy. Mortality rate at 3 months and 12 months (4.24% at 3 months and 3.2% at 12 months) were also lower than that of a recent systematical review and meta-analysis of eight RCTs16, in which the death from all cause at the end of follow-up in the fibrinogen depleting agents group was as high as 15%. Moreover, the recurrence rate of stroke at 12 months was only 3.22%, which was lower than that reported by Liu et al. and Hao et al.16,25.
Results from the comparisons of our study and NINDS II displayed that patients treated with rt-PA within 6 hours after stroke onset were more likely to obtain functional success (BI of 95 or 100) than that treated with defibrase within 72 hours from stroke symptom onset at 3 months. But no significant differences of functional success were detected when compared the patients treated with rt-PA within 6 hours of stroke onset in NINDS II and the patients treated with defibrase within 6 hours after stroke in the present study. It may imply that time-to-treatment played key roles in treatment of acute ischemic stroke. It conformed to the opinion that the earlier the treatment, the more benefit it would achieve. Additionally, we may try to infer that the treatment of rt-PA used in the NINDS II and the therapy of multiple-day dosing regimen applied in the present study plays equal effects in improving neural function in treating acute ischemic stroke within 6 hours of onset if there were no significant differences of demographic and baseline clinical characteristics between the 93 patients in our current study and 168 patients in NINDS II. The result that the mortality rate at 3 month was lower in our present study than that in NINDS among patients treated within 6 hours after the onset of stroke may largely owe to the close monitoring of fibrinogen level during the process of defibrinogenating therapy.
Based on the findings, the current study seems to indicate that for those patients who are not qualified for acute intervention with IV rt-PA, defibrinogen therapy appears safe and has similar outcomes, especially when used early, to a group of patients administrated IV rt-PA for acute stroke, and the effectiveness and safety of this defibrinogen therapy for stroke patients in this case series significantly improved compared with previous defibrinogenating therapy studies. Although the reasons for this disparity are unclear, it might because of patient selection, time to treatment, and dosing regimen strategies.
Patient selection is the first variable to explore. All the cases in this series were consecutively collected over the course of eight years and five months and treated by the same medical team. Since defibrase was the only defibrinogenating agent provided in this case series, the selection bias should have been minimized. The age, gender and medical history of the patients represented in this series were similar to patients in other studies. Patients of non-smoking, lower NIHSS score at admission are more likely to acquire functional success. However, unlike other trials25,29, patients with atrial fibrillation or history of prior stroke were also included in this series. Therefore, patient selection may not play a critical role.
The second variable is the treatment window of within 72 hours after stroke onset. The well-known term of “time is brain” underlines the rapidity of loss of neural structures during an ischemic stroke. It was reported, on average, to be 13.6 billion synapses, 11.9 km of neuronal fibers and 1.9 billion of neurons with each passing minute32. Therefore, timely recanalization in the occluded artery often makes for the salvage of ischemic penumbra, the restoration of cerebral perfusion and improvement of clinical outcomes33. However, in the current study, the time window of 72 h was made to allow more eligible stroke patients to receive the defibrinogen therapy. The feasible bases on some studies, which reported that fibrinogen level of patients was consistently higher within 72 hours after stroke onset than that of healthy control and hyperfibrinogenemia predicted risk of death after ischemic stroke34,35,36. Although none of previous studies delivered defibrinogenating agents to acute ischemic stroke patients in such an extended time window, the subgroup analysis by time to treatment showed no statistically significant difference in functional success reported by this case series and other studies24,27. In addition, it was reported that if patients were treated earlier, they functional improvement was better25. Thus, it would be difficult to attribute the differences between the results from this series and those from other related studies to purely extended therapeutic time window factors.
Finally, the differences in dosing regimen should also be investigated. Defibrase has been proved to be effective in improving functional outcomes among Chinese patients with acute ischemic stroke by Liu et al.25. The differences in outcomes might arise from the differences in dosing regimen strategies of fibrinolytic drugs. In our study, the multiple-day dosing regimen of defibrase was applied and mainly aimed to reduce bleeding events, such as sICH. Results showed that the number of defibrase administrations appeared not to be associated with functional success. However, higher total dose of defibrase appears to be conducive to higher functional success rates (Appendix 4). We may indicate that whether the neural function can improve decides on total dose of defibrase other than the number of defibrase administrations, but the latter combined fibrinogen lever measured before each delivery could contribute to reassess and predict the risk of bleeding caused by defibrinogenating therapy and confirm the safety. Compared with the briefer but more intense dosing applied by David et al.23 and unified multiple-day dosing regimen adopted by most of other studies24,25,26,27, such multiple-day dosing regimen used in the current series were moderate and relatively individualized with the fundamental purpose not to lower plasma fibrinogen level to the desired level but to maintain a low normal level and its ultimate goal of increasing blood flow in the infarct site and reducing the risk of intracranial hemorrhage37.
Limitations were also applied in this series of cases studies. First, There were incomplete outcome data for 11.82% of patients at 3 months and 18.68% at 12 months because of loss to follow-up. Although analyses that compared the differences of demographic and baseline clinical charateristics between the patients failed to follow-up and patients followed up at 3 months and 12 months identified no significant differences. Relatively high loss to follow-up may intend to influence the evaluation of effectiveness and safety of multiple-day dosing regimen adopted in the current study. Second, because this study is limited due to the inherent weaknesses of a retrospective review, information such as stroke etiology and volume of stroke infarction lesion were not available for us. These potential confounders were not tried to be controlled by statistical analysis and may exert some influences on the results. Last but not least, the present study was a case series other than a controlled trial, and we should be more caution in interpreting the results because of the lack of control group. Although the historical control was performed, the effects of such comparison are far more less than that of concurrent controls due to variable factors, such as the different participant cohort and different study conditions.
Conclusion
The multiple-day dosing regimen of defibrinogen therapy using defibrase applied in the present study could achieve functional improvement among acute ischemic stroke patients, with low risks of intracranial hemorrhage, mortality and stroke recurrence when compared with other similar studies. However, the efficacy and safety of such a defibrinogenating therapy is needed to be verified by RCTs with large sample size.
References
Lozano, R. et al. Global and Regional Mortality From 235 Causes of Death for 20 Age Groups in 1990 and 2010: A Systematic Analysis for the Global Burden of Disease Study 2010. LANCET. 380, 2095–2128 (2012).
O’Collins, V. E. et al. 1,026 Experimental Treatments in Acute Stroke. ANN NEUROL. 59, 467–477 (2006).
Tsai, C. F., Thomas, B. & Sudlow, C. L. Epidemiology of Stroke and its Subtypes in Chinese Vs White Populations: A Systematic Review. NEUROLOGY. 81, 264–272 (2013).
Tamm, A. et al. Impact of Stroke Care Unit On Patient Outcomes in a Community Hospital. STROKE. 45, 211–216 (2014).
Stroke Unit Trialists’ Collaboration Organised Inpatient (Stroke Unit) Care for Stroke. Cochrane Database Syst Rev. D197 (2013).
Emberson, J. et al. Effect of Treatment Delay, Age, and Stroke Severity On the Effects of Intravenous Thrombolysis with Alteplase for Acute Ischaemic Stroke: A Meta-Analysis of Individual Patient Data From Randomised Trials. LANCET. 384, 1929–1935 (2014).
Chen, C. J. et al. Endovascular Vs Medical Management of Acute Ischemic Stroke. NEUROLOGY. 85, 1980–1990 (2015).
Fuentes, B. et al. Benefits of Intravenous Thrombolysis in Acute Ischemic Stroke Related to Extra Cranial Internal Carotid Dissection. Dream Or Reality? INT J STROKE. 7, 7–13 (2012).
Riedel, C. H. et al. The Importance of Size: Successful Recanalization by Intravenous Thrombolysis in Acute Anterior Stroke Depends On Thrombus Length. STROKE. 42, 1775–1777 (2011).
Wahlgren, N. et al. Mechanical Thrombectomy in Acute Ischemic Stroke: Consensus Statement by ESO-Karolinska Stroke Update 2014/2015, Supported by ESO, ESMINT, ESNR and EAN. INT J STROKE. 11, 134–147 (2016).
Kannel, W. B., D’Agostino, R. B. & Belanger, A. J. Update On Fibrinogen as a Cardiovascular Risk Factor. ANN EPIDEMIOL. 2, 457–466 (1992).
Lee, A. J., Lowe, G. D., Woodward, M. & Tunstall-Pedoe, H. Fibrinogen in Relation to Personal History of Prevalent Hypertension, Diabetes, Stroke, Intermittent Claudication, Coronary Heart Disease, and Family History: The Scottish Heart Health Study. Br Heart J. 69, 338–342 (1993).
Qizilbash, N., Jones, L., Warlow, C. & Mann, J. Fibrinogen and Lipid Concentrations as Risk Factors for Transient Ischaemic Attacks and Minor Ischaemic Strokes. BMJ. 303, 605–609 (1991).
You, S. et al. Hyperfibrinogenemia is Significantly Associated with an Increased Risk of In-Hospital Mortality in Acute Ischemic Stroke Patients. CURR NEUROVASC RES. 14, 242–249 (2017).
Del, Z. G. et al. Hyperfibrinogenemia and Functional Outcome From Acute Ischemic. Stroke. STROKE. 40, 1687–1691 (2009).
Levy, D. E., Trammel, J. & Wasiewski, W. W. Ancrod for Acute Ischemic Stroke: A New Dosing Regimen Derived From Analysis of Prior Ancrod Stroke Studies. J Stroke Cerebrovasc Dis. 18, 23–27 (2009).
Ehrly, A. M. Influence of Arwin On the Flow Properties of Blood. BIORHEOLOGY. 10, 453–456 (1973).
Hossmann, V., Heiss, W. D., Bewermeyer, H. & Wiedemann, G. Controlled Trial of Ancrod in Ischemic Stroke. Arch Neurol. 40, 803–808 (1983).
Pollak, V. E., Glas-Greenwalt, P., Olinger, C. P., Wadhwa, N. K. & Myre, S. A. Ancrod Causes Rapid Thrombolysis in Patients with Acute Stroke. AM J MED SCI. 299, 319–325 (1990).
Sharp, A. A., Warren, B. A., Paxton, A. M. & Allington, M. J. Anticoagulant Therapy with a Purified Fraction of Malayan Pit Viper Venom. LANCET. 1, 493–499 (1968).
Gent, A., Ingram, G. I., Arocha-Pinango, C. L., Fenton, P. & Buckley, R. J. Central Retinal Vein Thrombosis: Serial Treatment with Defibrination, Aspirin and Plasminotropic Drugs. THROMB RES. 14, 61–66 (1979).
Tonnesen, K. H., Sager, P. & Gormsen, J. Treatment of Severe Foot Ischaemia by Defibrination with Ancrod: A Randomized Blind Study. Scand J Clin Lab Invest. 38, 431–435 (1978).
Levy, D. E. et al. Ancrod in Acute Ischemic Stroke: Results of 500 Subjects Beginning Treatment within 6 Hours of Stroke Onset in the Ancrod Stroke Program. STROKE. 40, 3796–3803 (2009).
Hennerici, M. G. et al. Intravenous Ancrod for Acute Ischaemic Stroke in the European Stroke Treatment with Ancrod Trial: A Randomised Controlled Trial. LANCET. 368, 1871–1878 (2006).
Cooperative Group for Reassessment of Defibrase. Reassessment of Defibrase in Treatment of Acute Cerebral Infarction: A Multicenter, Randomized, Double-Blind, Placebo-Controlled Trial. Chin Med Sci J. 20, 151–158 (2005).
Ancrod for the Treatment of Acute Ischemic Brain Infarction. The Ancrod Stroke Study Investigators. Stroke. 25, 1755–1759 (1994).
Sherman, D. G. et al. Intravenous Ancrod for Treatment of Acute Ischemic Stroke: The STAT Study: A Randomized Controlled Trial. Stroke Treatment with Ancrod Trial. JAMA. 283, 2395–2403 (2000).
Olinger, C. P. et al. Use of Ancrod in Acute Or Progressing Ischemic Cerebral Infarction. ANN EMERG MED. 17, 1208–1209 (1988).
The Cooperative Group for Reassessment of Defibrase. Reassessment of Defibrase in Treatment of Cerebral Infarction. Chin Med Sci J. 33, 263–267 (2000).
Hao, Z. et al. Fibrinogen Depleting Agents for Acute Ischaemic Stroke. Cochrane Database Syst Rev. D91 (2012).
Tissue Plasminogen Activator for Acute Ischemic Stroke. N Engl J Med. 333, 1581–1587 (1995).
Saver, J. L. Time is brain-quantified. Stroke 37, 263–6 (2006).
Rha, J. H. & Saver, J. L. The impact of re-canalization on ischemic stroke outcome: a meta-analysis. Stroke. 38, 967–73 (2007).
Dutta, J. et al. Plasma fibrinogen level in acute stroke - A hospital based study. J Assoc Physicians India. 64, 62–3 (2016).
Beg, M. et al. Role of serum fibrinogen in patients of ischemic cerebrovascular disease. Nepal Med Coll J. 9, 88–92 (2007).
Swarowska, M. et al. Hyperfibrinogenemia predicts long-term risk of death after ischemic stroke. J Thromb Thrombolysis 38, 517–21 (2014).
Lowe, G. D. Blood Rheology in General Medicine and Surgery. Baillieres Clin Haematol. 1, 827–861 (1987).
Acknowledgements
The authors thank Dr. Tianwu Chen for his English editing. This study was supported by the National Natural Science Foundation of China (No. 81571277).
Author information
Authors and Affiliations
Contributions
C.C. Ren conceptualized the study, analyzed and interpreted the data, and drafted and revised the manuscript. C.C. Ren had full access to all data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis. J. Chen, D.L. Sun and M.L. Liu analyzed and interpreted the data, drafted and revised the manuscript, and contributed to the statistical analysis. S.F. Zhang contributed to the statistical analysis. All authors collected data, revised the manuscript, and contributed to the writing.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, J., Sun, D., Liu, M. et al. Defibrinogen Therapy for Acute Ischemic Stroke: 1332 Consecutive Cases. Sci Rep 8, 9489 (2018). https://doi.org/10.1038/s41598-018-27856-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-27856-6
This article is cited by
-
Mechanistic correlation of molecular pathways in obesity-mediated stroke pathogenesis
Pharmacological Reports (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.