Abstract
This trial was designed to assess the prevalence and characteristics of Jackhammer esophagus (JE), a novel hypercontractile disorder associated with progression to achalasia and limited outcomes following anti-reflux surgery in patients with typical symptoms of GERD and responsiveness to proton pump inhibitor (PPI) therapy. Consecutive patients, who were referred for surgical therapy because of PPI responsive typical symptoms of GERD, were prospectively assessed between January 2014 and May 2017. Patients diagnosed with JE subsequently underwent rigorous clinical screening including esophagogastroduodenoscopy (EGD), ambulatory pH impedance monitoring off PPI and a PPI trial. Out of 2443 evaluated patients, 37 (1.5%) subjects with a median age of 56.3 (51.6; 65) years were diagnosed with JE and left for final analysis. Extensive testing resulted in 16 (43.2%) GERD positive patients and 5 (13.9%) participants were observed to have an acid hypersensitive esophagus. There were no clinical parameters that differentiated phenotypes of JE. The prevalence of JE in patients with typical symptoms of GERD and response to PPI therapy is low. True GERD was diagnosed in less than half of this selected cohort, indicating the need for objective testing to stratify phenotypes of JE. (NCT03347903)
Similar content being viewed by others
Introduction
Gastroesophageal reflux disease (GERD) is suggested to be involved in the induction of a novel hypercontractile condition that is not observed in healthy volunteers and was nicknamed Jackhammer esophagus (JE)1,2. According to the Chicago Classification (CC) version 3.0, an algorithm classifying high-resolution manometry (HRM) studies, this new phenotype of hypercontractility was determined to be present in subjects where ≥20% of swallows exceeded a distal contractile integral (DCI) of >8000 mmHg-s-cm in context of normal contractile propagation3.
Worryingly, recent observations indicated a progressive nature of the disease in 25% of patients with further development to type II and III achalasia4,5. Furthermore, nutcracker esophagus, a phenotype of hypercontractility that, in contrast to JE, was also observed in healthy controls, was associated with adverse postoperative outcomes following laparoscopic anti-reflux surgery6. Conceptually, these findings irritate surgical considerations, as implementation of HRM as a mandatory preoperative examination in patients with high evidence of GERD is discussed controversially in literature7,8,9,10,11. As a consequence, there is a subgroup of patients, where despite of surgical excellence and specialization, we fail to achieve good outcomes.
Therefore, this trial was designed to assess the prevalence and characteristics of JE in patients presenting with typical symptoms of GERD and therapeutic PPI response, referred for surgical anti-reflux therapy at a specialized centre.
Results
Baseline data
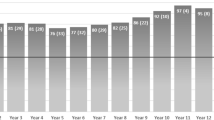
Out of 2443 patients referred and evaluated within the study period, 41 (1.7%) subjects were diagnosed with JE. Four patients had to be excluded due to previous gastrointestinal surgery (n = 2) and denial of pH metry (n = 2), which left 37 (females n = 18, 48.6%) individuals for the final analysis. Patients included in this trial had a median age of 56.3 (51.6; 65) years with 54.1% (n = 20) presenting with hiatal hernia in EGD. Esophagitis was observed in 9 patients (24.3%), consisting of 2 (22.2%) participants with LA grade B, 4 (44.4%) individuals with LA grade C and 3 (33.3%) patients with LA grade D esophagitis. Histopathology revealed the diagnosis of Barrett’s esophagus in 3 (8.1%) patients. Further baseline data are delineated in Table 1.
GERD was diagnosed in 16 (43.2%) patients, whereas acid hypersensitive esophagus was observed in 5 (13.9%) participants. Sixteen patients (43.2%) had no evidence of GERD (Fig. 1).
Symptom assessment and PPI response
Patients reported heartburn (54.1%; n = 20) and dysphagia (51.4%; n = 19) as predominant symptoms with overall symptom duration of 2 (0.13; 9.5) years. Non-cardiac chest pain was noticed in 35.1% (n = 13), whereas regurgitations were observed in 18 (48.6%) patients (Table 2). All patients reported more than one symptom. Daily PPI intake was registered in 29 (78.4%) subjects. Patients experienced PPI mediated complete resolution of heartburn and or/regurgitation in 10% (n = 2) and partial resolution in 90% (n = 18). As far as typical JE symptoms are concerned, partial response to medical therapy was monitored in 6.9% (n = 2), whereas 93.1% (n = 27) described no effect of a PPI trial.
Subgroup analysis
There were no differences concerning age (p = 0.445), sex (p = 0.337) or BMI (0.463) between JE-GERDpos, JE-GERDneg and JEHyper patients. Furthermore, symptoms like heartburn (p = 0.167), regurgitation (p = 0.250), dysphagia (p = 0.714) or non-cardiac chest pain (p = 0.906) as well as their duration (p = 0.319) did not discriminate groups. Intake of PPI (p = 0.377) and effect on heartburn (p = 0.494) or Jackhammer specific symptoms (p = 0.287) were also similar.
JE-GERDpos patients had significantly higher counts of total reflux episodes (p = 0.027), which was mainly credited to acidic reflux episodes (p = 0.022) and not to non-acidic (p = 0.852) or gas containing (p = 0.583) reflux. CBR was significantly impaired in patients with JE-GERDpos. Quality of life and HRM did not allow differentiation between groups. Descriptive data are provided in Table 3.
Discussion
This is the first study prospectively assessing the prevalence of JE in a selected cohort of patients presumptive of GERD. We could demonstrate that JE was found in 1.7% of patients referred for surgical therapy at a specialized academic centre. Clinical presentation and response to PPI was insufficient to stratify phenotypes of JE. Acidic reflux episodes discriminated JE and GERD supporting the thesis of an acidic reflux induced phenotype of hypercontractility.
The introduction of HRM studies revisited the concept of esophageal hypercontractility and led to the introduction of a novel hypercontractile disorder, which in contrast to nutcracker esophagus was never observed in healthy controls1. Interestingly, JE, named after its common multi-peaked appearance, was registered in 1.7% of patients with typical symptoms of GERD responsive to PPI therapy, which goes in line with recent observations, where JE was found in up to 5% of unselected patients undergoing HRM12,13.
From a pathophysiological point of view, affected patients seem to represent a heterogeneous population with demanding therapeutic implications. First and foremost, outflow obstruction may mediate hypercontractility. Burton et al. reported that overfilling of a laparoscopic adjustable gastric band resulted in hypercontractile and repetitive esophageal contractions, which was also observed in another study, when functional obstruction was present14,15. In our population, 45.9% of subjects where diagnosed with concomitant outflow obstruction, significantly more frequent in GERD negative patients, discriminating a distinct phenotype of disease. As confirmation, Jia et al. observed similar outflow obstruction rates results in their cohort13. Secondly, a hyper-cholinergic state may lead to asynchrony between muscular layers noticed frequently in hyerpcontractility that can be reversed by atropine16,17.
Moreover, GERD is suggested to play a major role in induction of hypercontractility. Early acid perfusion studies have demonstrated that acid was able to provoke spasms, motility changes and the perception of non-cardiac chest pain, a symptom frequently observed in JE18,19. Unfortunately, there is hardly any data focusing on GERD in JE. Mallet et al. observed that prevalence of GERD was higher in JE when compared to the general population12. Nevertheless, endoscopy and ambulatory pH monitoring, cornerstones in the diagnosis of GERD, were not performed in nearly a third of their patients. Additionally, ambulatory pH monitoring was used without impedance, which limits diagnostic yield20.
Importantly, GERD was only diagnosed in 43.2% of patients with JE all presumptive of GERD. Although typical symptoms of heartburn and regurgitation are most reliable for making a presumptive diagnosis of GERD based on history alone and are endorsed by societies as a pragmatic approach in daily clinical practice, modern recommendations include empiric PPI trial and objective testing to substantiate diagnosis of true GERD11,21,22.
We could observe that total reflux episodes were higher in JE-GERDpos patients, which was based on more acidic reflux episodes. As far as gas reflux and non-acidic reflux is concerned, there were no differences between groups. Furthermore, JE-GERDpos patients were associated with impaired complete bolus rates. Therefore, our data support the pathophysiological concept of JE induction by reflux of acidic gastric contents.
Acid-hypersensitive esophagus was remarked in 13.5% of our cohort. Thus, our data acknowledge that functional esophageal disorders are associated with visceral hypersensitivity and are not always a result of GERD23. Mujica et al. recognized that symptoms in patients with nutcracker esophagus could be reproduced by stepwise balloon distensions emphasizing a lower threshold for visceral sensitivity24. This may explain the fact that 43.2% of our patients reported typical PPI responsive symptoms without evidence of GERD.
Therapeutic aspects of GERD in JE are complex. Recently, a longitudinal study revealed that 25% of patients with JE progressed to type III achalasia within 2 years, whereas progression to type II achalasia was also observed4,5. Potentially, these individuals may profit from modern peroral endoscopic myotomy (POEM) to overcome obstructed outflow and were represented in our JE-GERDneg subgroup25.
Currently, it is unknown if control of GERD will limit development to achalasia, improve JE or if JE itself is responsible for a proportion of adverse postoperative outcomes at specialized centres. Data on surgical or medical therapy for GERD in JE are more than scarce. Crespin et al. reported on two patients with JE that underwent laparoscopic Nissen fundoplication (LNF) and returned to regular esophageal motility26. Furthermore, Roman et al. followed 12 patients with JE that received PPI or LNF for control of GERD and realized that 7 of them improved significantly2. In contrast, PPI failed to achieve symptom control in a randomized placebo controlled trial in nutcracker esophagus, a hypercontractile condition that was similar in treatment response to JE in a small uncontrolled trial27,28. Furthermore, Winslow et al. reported that patients with spastic motor disorders had higher rates of persisting GERD symptoms and postoperative dysphagia after laparoscopic anti-reflux surgery6. Nevertheless, preoperative manometry, which is necessary to detect JE in this selected cohort is discussed controversially in literature. Whereas gastroenterological societies and an expert advisory panel recommend preoperative manometry mainly to exclude conditions like achalasia or distal esophageal spasm, large surgical societies still question the support in literature for its mandatory use7,9,10,11. Frantzides et al. reported a series of 628 consecutive laparoscopic floppy Nissen procedures, where manometry was either used as routine evaluation or selective in presence of dysphagia, odynophagia or abnormal motility on videofluoroscopy29. The authors stated that selective use of manometry was cost effective and safe, as it did not increase rates of postoperative dysphagia even if dysmotility was diagnosed. Following this concept nearly half of our cohort would miss the diagnosis of JE, as they did not experience dysphagia. Furthermore, prospective randomized data of preoperative and postoperative use of manometry failed to affect or detect postoperative surgical outcomes30,31. Given that we could show that JE was rather low in our cohort, these conflicting statements may just be a result of underpowered studies.
Limitations of this study have also to be addressed. Although this is the largest study prospectively evaluating patients with JE, single centre design and low prevalence restrict the number of patients with disease. Furthermore, we emphasize that the Chicago classification uses JE as a term for a heterogeneous population with varying pathophysiological background that may influence symptoms and reflux burden. Therefore, our results and conclusions have to be interpreted with care. Strengths represent the prospective assessment of data that limits potential selection bias and the rigorous examination of patients by diagnostic cornerstones of GERD.
In conclusion, this study shows that the prevalence of JE in patients with typical symptoms of GERD and empirical response to PPI therapy is low. True GERD was diagnosed in less than half of this selected cohort, indicating the need for additional objective testing to stratify phenotypes of JE. Mandatory preoperative HRM should be recommended by surgical societies to determine presence of hypercontractile disorders that potentially limit postoperative outcomes.
Methods
Patient selection
All consecutive patients, who were referred for surgical therapy because of PPI responsive typical symptoms of GERD (heartburn and/or regurgitation) between January 2014 and May 2017, were included in this trial and underwent HRM at our tertiary academic referral centre for gastrointestinal research and service. Patients showing ≥20% of swallows with DCI >8000 mmHg-s-cm in context of normal contractile propagation3 were analysed. Exclusion criteria were presence of achalasia, distal esophageal spasm, history of previous gastrointestinal surgery, mechanical esophageal obstruction or other diseases explaining their symptoms (i.e. eosinophilic esophagitis, systemic sclerosis).
Study flow
After inclusion, subjects underwent esophagogastroduodenoscopy (EGD) off PPI to determine presence of GERD, classified according to the Los Angeles (LA) classification32. Medical history, symptoms and Impact Dysphagia Questionnaire (IDQ) were assessed in a face-to-face interview with study participants being at least 14 days off PPI. Dysphagia and non-cardiac chest pain were graded utilizing a standardized assessment according to Mellow and Pinkas33. Response to PPI therapy was tested by an 8-week double-dose course of esomeprazole therapy to differentiate between improvement of typical (heartburn, regurgitation) and/or Jackhammer specific symptoms (dysphagia, non-cardiac chest pain). Partial response to PPI therapy was defined as any reduction of symptom intensity, whereas full response to PPI therapy resulted in resolution of symptoms. For subgroup analysis patients were divided in GERD positive (JE-GERDpos), GERD-negative (JE-GERDneg) and patients with acid hypersensitive esophagus (JEHyper).
Quality of life was determined using the Gastroesophageal Reflux Disease-Health Related Quality of Life (GERD-HRQL) on (GERD-HRQL/+PPI) and at least 8 weeks off PPI therapy (GERD-HRQL/−PPI). Concluding, 24 h impedance pH metry was performed in all patients. All patients underwent informed consent and the institutional review board of the Medical University of Vienna approved the study protocol. All methods were performed in accordance with relevant guidelines and regulations.
High-resolution impedance manometry
High-resolution impedance manometry was performed using a solid-state catheter with 32 circumferential pressure transducers at 1 cm intervals and dual impedance sensors (Sandhill Scientific, Highlands Ranch, CO, USA) as previously described34,35. In brief, the catheter was inserted transnasally and positioned to record pressure from hypopharynx to the stomach in supine position. Esophageal body motility was assessed with 10 liquid swallows of 5 ml at 30-second intervals. BioView™ (Sandhill Scientific, Highlands Ranch, CO, USA) was utilized to interpret data according to the CC v3.03. The DCI was calculated from the proximal pressure trough to the proximal level of the LES integrating amplitude, duration and length of contraction exceeding 20 mmHg. In addition to regular CC specific metrics all hypercontractile swallows were evaluated. Complete bolus transit was defined as described by Tutuian et al. with complete bolus rate (CBR) being the percentage of complete bolus transit referred to all liquid swallows36.
Ambulatory 24-hour pH impedance monitoring
Patients had to stop PPI or H2 blocker intake at least 10 days before monitoring. A catheter containing impedance tracers and electrodes with internal reference for pH measuring was utilized (ComforTec ZAN-44; Sandhill Scientific, Highlands Ranch, CO, USA). Electrodes were positioned after locating the lower esophageal sphincter (LES) by HRM as previously described37. Patients were instructed to stick to their daily routine and enter symptoms, body position and meals. GERD was defined as the percentage of endoluminal pH < 4 exceeding 4.2% in the distal esophagus and/or endoscopic visible lesions according to the LA classification. An acid-hypersensitive esophagus was registered when normal esophageal acid exposure was associated with a symptomatic index greater than 50% and/or a symptom association probability (SAP) greater than 95%.
Statistical analysis
Demographics are presented as mean with standard deviation if normally distributed or as median with interquartile ranges otherwise. Categorical variables are displayed as absolute numbers and percentages. High-resolution impedance manometry metrics are delineated as median with interquartile ranges. Chi-square or Wilcoxon rank test were applied as appropriate for comparison between groups. The Kruskal-Wallis method was applied for comparison between three groups. P-values ≤ 0.05 were considered statistically significant. Analyses were done using SPSS for Macintosh Version 24.0 (IBM Corp., Armonk, NY, USA). The dataset analyzed during the current study are available from the corresponding author on request.
References
Roman, S. et al. Phenotypes and clinical context of hypercontractility in high-resolution esophageal pressure topography (EPT). Am J Gastroenterol 107, 37–45, https://doi.org/10.1038/ajg.2011.313 (2012).
Roman, S. & Kahrilas, P. J. Management of spastic disorders of the esophagus. Gastroenterol Clin North Am 42, 27–43, https://doi.org/10.1016/j.gtc.2012.11.002 (2013).
Kahrilas, P. J. et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27, 160–174, https://doi.org/10.1111/nmo.12477 (2015).
Abdallah, J. & Fass, R. Progression of Jackhammer Esophagus to Type II Achalasia. J Neurogastroenterol Motil 22, 153–156, https://doi.org/10.5056/jnm15162 (2016).
Huang, L., Pimentel, M. & Rezaie, A. Do Jackhammer contractions lead to achalasia? A longitudinal study. Neurogastroenterol Motil 29, https://doi.org/10.1111/nmo.12953 (2017).
Winslow, E. R. et al. Influence of spastic motor disorders of the esophageal body on outcomes from laparoscopic antireflux surgery. Surg Endosc 17, 738–745, https://doi.org/10.1007/s00464-002-8538-y (2003).
Stefanidis, D. et al. Guidelines for surgical treatment of gastroesophageal reflux disease. Surg Endosc 24, 2647–2669, https://doi.org/10.1007/s00464-010-1267-8 (2010).
Lundell, L. et al. Comparing laparoscopic antireflux surgery with esomeprazole in the management of patients with chronic gastro-oesophageal reflux disease: a 3-year interim analysis of the LOTUS trial. Gut 57, 1207–1213, https://doi.org/10.1136/gut.2008.148833 (2008).
Jobe, B. A. et al. Preoperative diagnostic workup before antireflux surgery: an evidence and experience-based consensus of the Esophageal Diagnostic Advisory Panel. J Am Coll Surg 217, 586–597, https://doi.org/10.1016/j.jamcollsurg.2013.05.023 (2013).
Kahrilas, P. J. et al. American Gastroenterological Association Medical Position Statement on the management of gastroesophageal reflux disease. Gastroenterology 135(1383–1391), 1391 e1381–1385, https://doi.org/10.1053/j.gastro.2008.08.045 (2008).
Katz, P. O., Gerson, L. B. & Vela, M. F. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 108(308–328), quiz 329, https://doi.org/10.1038/ajg.2012.444 (2013).
Mallet, A. L. et al. Prevalence and characteristics of acid gastro-oesophageal reflux disease in Jackhammer oesophagus. Dig Liver Dis 48, 1136–1141, https://doi.org/10.1016/j.dld.2016.06.030 (2016).
Jia, Y. et al. Frequency of Jackhammer Esophagus as the Extreme Phenotypes of Esophageal Hypercontractility Based on the New Chicago Classification. J Clin Gastroenterol 50, 615–618, https://doi.org/10.1097/MCG.0000000000000496 (2016).
Burton, P. R. et al. The effect of laparoscopic adjustable gastric bands on esophageal motility and the gastroesophageal junction: analysis using high-resolution video manometry. Obes Surg 19, 905–914, https://doi.org/10.1007/s11695-009-9845-3 (2009).
Gyawali, C. P. & Kushnir, V. M. High-resolution manometric characteristics help differentiate types of distal esophageal obstruction in patients with peristalsis. Neurogastroenterol Motil 23, 502–e197, https://doi.org/10.1111/j.1365-2982.2011.01672.x (2011).
Jung, H. Y. et al. Asynchrony between the circular and the longitudinal muscle contraction in patients with nutcracker esophagus. Gastroenterology 128, 1179–1186 (2005).
Korsapati, H., Bhargava, V. & Mittal, R. K. Reversal of asynchrony between circular and longitudinal muscle contraction in nutcracker esophagus by atropine. Gastroenterology 135, 796–802, https://doi.org/10.1053/j.gastro.2008.05.082 (2008).
Crozier, R. E., Glick, M. E., Gibb, S. P., Ellis, F. H. Jr. & Veerman, J. M. Acid-provoked esophageal spasm as a cause of noncardiac chest pain. Am J Gastroenterol 86, 1576–1580 (1991).
Herregods, T. V., Smout, A. J., Ooi, J. L., Sifrim, D. & Bredenoord, A. J. Jackhammer esophagus: Observations on a European cohort. Neurogastroenterol Motil 29 https://doi.org/10.1111/nmo.12975 (2017).
Zerbib, F. et al. Esophageal pH-impedance monitoring and symptom analysis in GERD: a study in patients off and on therapy. Am J Gastroenterol 101, 1956–1963, https://doi.org/10.1111/j.1572-0241.2006.00711.x (2006).
Dent, J. et al. Accuracy of the diagnosis of GORD by questionnaire, physicians and a trial of proton pump inhibitor treatment: the Diamond Study. Gut 59, 714–721, https://doi.org/10.1136/gut.2009.200063 (2010).
Gyawali, C. P. et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. https://doi.org/10.1136/gutjnl-2017-314722 (2018).
Remes-Troche, J. M. The hypersensitive esophagus: pathophysiology, evaluation, and treatment options. Curr Gastroenterol Rep 12, 417–426, https://doi.org/10.1007/s11894-010-0122-3 (2010).
Mujica, V. R., Mudipalli, R. S. & Rao, S. S. Pathophysiology of chest pain in patients with nutcracker esophagus. Am J Gastroenterol 96, 1371–1377, https://doi.org/10.1111/j.1572-0241.2001.03791.x (2001).
Khan, M. A. et al. Is POEM the Answer for Management of Spastic Esophageal Disorders? A Systematic Review and Meta-Analysis. Dig Dis Sci 62, 35–44, https://doi.org/10.1007/s10620-016-4373-1 (2017).
Crespin, O. M. et al. Esophageal hypermotility: cause or effect? Dis Esophagus 29, 497–502, https://doi.org/10.1111/dote.12367 (2016).
Borjesson, M., Rolny, P., Mannheimer, C. & Pilhall, M. Nutcracker oesophagus: a double-blind, placebo-controlled, cross-over study of the effects of lansoprazole. Aliment Pharmacol Ther 18, 1129–1135 (2003).
Al-Qaisi, M. T. et al. The clinical significance of hypercontractile peristalsis: comparison of high-resolution manometric features, demographics, symptom presentation, and response to therapy in patients with Jackhammer esophagus versus Nutcracker esophagus. Dis Esophagus 30, 1–7, https://doi.org/10.1093/dote/dox085 (2017).
Frantzides, C. T., Carlson, M. A., Madan, A. K., Stewart, E. T. & Smith, C. Selective use of esophageal manometry and 24-Hour pH monitoring before laparoscopic fundoplication. J Am Coll Surg 197 358-363; discussion 363–354, https://doi.org/10.1016/S1072-7515(03)00591-X (2003).
Fibbe, C. et al. Esophageal motility in reflux disease before and after fundoplication: a prospective, randomized, clinical, and manometric study. Gastroenterology 121, 5–14 (2001).
Yang, H. et al. Esophageal manometry and clinical outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg 11, 1126–1133, https://doi.org/10.1007/s11605-007-0224-x (2007).
Lundell, L. R. et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 45, 172–180 (1999).
Mellow, M. H. & Pinkas, H. Endoscopic therapy for esophageal carcinoma with Nd:YAG laser: prospective evaluation of efficacy, complications, and survival. Gastrointest Endosc 30, 334–339 (1984).
Schwameis, K. et al. Modern GERD treatment: feasibility of minimally invasive esophageal sphincter augmentation. Anticancer Res 34, 2341–2348 (2014).
Shi, Y. et al. Normative data of high-resolution impedance manometry in the Chinese population. J Gastroenterol Hepatol 28, 1611–1615, https://doi.org/10.1111/jgh.12285 (2013).
Tutuian, R., Vela, M. F., Shay, S. S. & Castell, D. O. Multichannel intraluminal impedance in esophageal function testing and gastroesophageal reflux monitoring. J Clin Gastroenterol 37, 206–215 (2003).
Ringhofer, C. et al. Waist to hip ratio is a better predictor of esophageal acid exposure than body mass index. Neurogastroenterol Motil 29 https://doi.org/10.1111/nmo.13033 (2017).
Acknowledgements
We thank Jack Morley for linguistic revision of the manuscript.
Author information
Authors and Affiliations
Contributions
I.K. designed the trial, conducted the trial, wrote the paper K.S. conducted the trial, important intellectual input S.M. Data collection, conducted the trial A.K. performed statistical analyses, important intellectual input E.R. important intellectual input, data collection M.P. conducted the trial, data collection G.J. data collection, important intellectual input S.F.S. designed the trial, wrote the paper, important intellectual input
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kristo, I., Schwameis, K., Maschke, S. et al. Phenotypes of Jackhammer esophagus in patients with typical symptoms of gastroesophageal reflux disease responsive to proton pump inhibitors. Sci Rep 8, 9949 (2018). https://doi.org/10.1038/s41598-018-27756-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-27756-9
This article is cited by
-
Management of Non-achalasia Esophageal Hypercontractility: EGJ Outflow Obstruction and Hypercontractile Esophagus
Current Treatment Options in Gastroenterology (2023)
-
Hypercontractile esophagus responsive to potassium-competitive acid blockers: a case report
BMC Gastroenterology (2022)
-
Silent Gastroesophageal Reflux Disease in Patients with Morbid Obesity Prior to Primary Metabolic Surgery
Obesity Surgery (2020)
-
Minor esophageal functional disorders: are they relevant?
Current Treatment Options in Gastroenterology (2020)
-
Modern Esophageal Function Testing and Gastroesophageal Reflux Disease in Morbidly Obese Patients
Obesity Surgery (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.