Abstract
Malaria control program in the Arabian Peninsula, backed by adequate logistical support, has interrupted transmission with exception of limited sites in Saudi Arabia and sporadic outbreaks in Oman. However, sustained influx of imported malaria represents a direct threat to the above success. Here we examined the extent of genetic diversity among imported P. vivax in Qatar, and its ability to produce gametocytes, compared to parasites in main sites of imported cases, the Indian subcontinent (india) and East Africa (Sudan and Ethiopia). High diversity was seen among imported P. vivax in Qatar, comparable to parasites in the Indian subcontinent and East Africa. Limited genetic differentiation was seen among imported P. vivax, which overlapped with parasites in India, but differentiated from that in Sudan and Ethiopia. Parasite density among imported cases, ranged widely between 26.25–7985934.1 Pv18S rRNA copies/µl blood, with a high prevalence of infections carried gametocytes detectable by qRT-PCR. Parasitaemia was a stronger predictor for P. vivax gametocytes density (r = 0.211, P = 0.04). The extensive diversity of imported P. vivax and its ability to produce gametocytes represent a major threat for re-introduction of malaria in Qatar. The genetic relatedness between P. vivax reported in Qatar and those in India suggest that elimination strategy should target flow and dispersal of imported malaria into the region.
Similar content being viewed by others
Introduction
Global concerted and collaborative efforts, backed by WHO, have resulted in remarkable reduction in the burden of malaria, and disease elimination in many areas. Nonetheless, imported malaria represents a significant threat to the above achievements1. The escalating volume of international travel among people in endemic areas, driven by desire to improve quality of life and political unrest, has increased the risk of malaria importation into non-endemic areas, including Europe2.
Local malaria transmission in the Gulf Cooperation Council (GCC) countries has been interrupted as a result of sustained vector control3, and active case detection to define existing malaria foci. Consequently, this has brought local transmission to a halt in many countries in the region, including Bahrain, Kuwait and the United Arab Emirates (UAE), and more recently Oman3. However, some sites in Yemen and southern Saudi Arabia remain malarious, with a high prevalence of drug-resistant Plasmodium falciparum4. The success of control programs in the region has prompted the health authorities in GCC countries to shift strategies towards malaria elimination and prevention of re-introduction in receptive areas5.
However, the above success is vulnerable to a possible resurgence of local transmission caused by imported parasites via asymptomatic travellers from malaria-endemic areas6,7. The risk of malaria resurgence depends on the combined effect of receptivity and vulnerability. Receptivity is a function of the presence of local vectors and environmental conditions that favour malaria transmission, while vulnerability reflects the probability of importation of malaria parasites into a country8. The region is highly vulnerable to re-introduction of malaria, given the high volume of immigration from malaria endemic regions. This has been implicated in the persistence of high rates of imported malaria in many GCC countries9. For example, while a significant reduction in locally acquired malaria cases was observed between 2000 and 2014 in Saudi Arabia, imported cases remained consistent averaging between 250 and 830 cases per year6,10. Imported malaria is also common in Qatar, Bahrain, Kuwait and the UAE7,11,12,13, and has been implicated in repeated malaria outbreaks in Oman14. In Qatar, malaria transmission has been interrupted since 197015, however, a constant influx of imported malaria by the large number of immigrant workers from the Indian Subcontinent, and Sub-Saharan Africa, poses a risk for re-introduction11,16. Receptivity of the country to a re-introduction of malaria is evident by the presence of two potential vectors, Anopheles stephensi and A. multicolour17. The proportion of all imported malaria reported amongst travellers in Qatar has increased over the past decade, with P. vivax being the main prevalent parasite11.
The impact of imported malaria, often as asymptomatic infection, on local epidemiology and local transmission is not well defined in Qatar and surrounding regions. However the ability of asymptomatic P. falciparum and P. vivax infections to produce gametocytes is well documented18,19. Currently there is no clear information on the actual magnitude of asymptomatic parasite reservoir in areas where malaria has been eliminated in the GCC countries and its population structure. Thus, the present study examined the source of imported P. vivax into the transmission free setting of Qatar, assessed its genetic complexity and its ability to produce gametocytes and transmit malaria. In addition, we compared the extent of diversity and genetic relatedness of imported parasites into Qatar with that in three countries of origin of immigrant malaria into Qatar, in Africa (Sudan and Ethiopia) and the Indian Subcontinent (India). Such knowledge would allow regional and national control programs to develop targeted policies to reduce the size of infectious reservoir, define the source of outbreaks and limit the risk of re-introduction of malaria.
Results
Demographic characteristics of imported malaria in Qatar
Out of 583 patients examined by microscopy for malaria between January 2013 and October 2016 in Qatar, 448 (76.8%) were found to be positive. Species-specific PCR revealed a high prevalence of P. vivax cases (n = 318 [70.9%]), while P. falciparum (n = 118 [26.3%]) and mixed infection, with P. falciparum and P. vivax, was less frequent (n = 12 [2.7%]) (Fig. 1).
The vast majority of imported P. vivax cases were young males (93.7%), mean age 32 years, from the Indian Subcontinent (n = 264 [83%]); including, India (n = 148 [46.5%]), Pakistan (n = 104, [32.7%]) and Nepal (n = 12, [3.7%]). However, a small proportion of imported P. vivax cases were from Africa (n = 53 [16.7%]), including Sudan (n = 24, [7.5%]), and other African countries (n = 19, [6%]). On the contrary, the vast majority of imported P. falciparum cases were from Africa (n = 88 out of 118, [75%] [75%]), with a fewer number of patients from the Indian Subcontinent (n = 23, [19%] [%]) and others (n = 7 [6%]) (Table 1 and Fig. 1).
Parasitaemia and gametocyte carriage among imported P. vivax
Ninety-five imported P. vivax isolates originated from the Indian Subcontinent (India, n = 59 [62.10%], Pakistan, n = 35 [36.84%] and Nepal, n = 1 [1.05%]) were successfully examined by qPCR and qRT-PCR to quantify total parasitaemia and gametocyte density, respectively. Total parasite density estimated as transcript of Pv18s rRNA ranged between 26.2 and 7985934.1 copies/µl of blood (median = 1029.0).
Out of 95 P. vivax isolates examined by RT-qPCR, 94 (98.9%) had detectable transcripts of Pvs25, indicative of the presence of gametocytes. The copy number of Pvs25 transcript, among the examined isolates ranged from 0.33 to −78441.24 copies of Pvs25/µl of blood (median = 300.3).
Spearman’s rank-order correlation test showed a positive relationship between the copy numbers of Pv18srRNA and Pvs25 transcripts (Correlation Coefficient, r = 0.211, P = 0.04), suggesting an association between parasitaemia and gametocyte density (Fig. 2).
Diversity of P. vivax
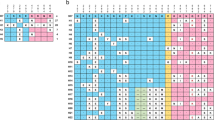
Microsatellite analysis was carried out among 265 imported P. vivax isolates in Qatar, as well as P. vivax isolates collected in endemic sites, where the majority of imported malaria into Qatar originated, in Sudan (n = 137), Ethiopia (n = 87) and India (n = 40). There was a high degree of polymorphism in all microsatellites, with number of alleles per locus varied from 8 for MS1 to 38 for MS8 among imported parasites in Qatar, 6 for MS7 to 22 for MS20 among parasites in Sudan, 4 for MS7 to 22 for MS8 among parasites in Ethiopia and 6 for MS5 to 19 for MS8 among Indian isolates (Table 2).
There was an extensive diversity among imported P. vivax in Qatar (HE = 0.782) similar to that seen in endemic sites in Sudan (HE = 0.726), Ethiopia (HE = 0.684) and India (HE = 0.797) (Table 2). A total of 142 alleles in all loci were found among imported P. vivax in Qatar compared to 96, 93 and 87 alleles in Sudan, Ethiopia and India, respectively. However, many private alleles were seen in some loci in all sites, imported parasites, Qatar (n = 48), Ethiopia (n = 34), Sudan (n = 33) and India (n = 30) (Table 2).
The predominant allele at each locus in each isolate was used to construct multi-locus genotypes (haplotypes). Each P. vivax isolate, among imported cases as well as parasites collected in Sudan, Ethiopia and India, carried a distinct multi-locus genotype, with exception of 5 pairs (10 isolates) in Sudan each shared a distinct genotype.
Linkage disequilibrium
The multi-locus genotype (haplotypes) data was used to estimate the standard index of association (ISA). This determines whether there is an association between alleles on different loci, and if the above high levels of diversity observed in P. vivax populations could be explained by frequent genetic exchange.
Limited linkage disequilibrium (LD) was seen among the imported cases in Qatar ISA = 0.0050 while a relatively higher LD value was seen among parasites in Sudan (0.0958) compared to parasites from Ethiopia (0.0367) and India (0.0265) (Table 3). These values, suggest that a particular combination of alleles on different chromosomes exist at a higher frequency than that expected among randomly mating parasites.
Population differentiation
To assess the genetic relatedness among imported P. vivax in Qatar, the isolates were divided into three populations (India [n = 132], Pakistan [n = 89] and Sudan [n = 24]) based on the nationality of patients. Pairwise analysis showed a close relationship between parasites from Pakistan and India (FST = 0.0008), compared to that seen between parasites from Sudan and India (FST = 0.0037) or Sudan and Pakistan (FST = 0.0011). Nonetheless, imported P. vivax from the three countries can be considered as one population. Similar close genetic relatedness was seen between imported P. vivax in Qatar, treated as one population, and isolates collected in India (FST = 0.0594). However, imported P. vivax in Qatar was slightly diverged from local parasite in Sudan (FST = 0.1435) and Ethiopia (FST = 0.1896).
The above results were supported by Principal Component Analysis (PCoA) (Fig. 3). The Ethiopian P. vivax population was distanced from the imported parasites in Qatar, while the Sudanese and Ethiopian parasites were slightly overlapped (Fig. 3). Analysis of molecular variance (AMOVA) indicated that most of the genetic variation (86%) was contained within parasites in each region and only 14% can be explained by differences between regions.
Structure analysis showed a clear separation between the imported P. vivax in Qatar and the East African isolates (Sudan and Ethiopia) when K = 2. However, when K = 3 there was some overlap between Sudanese isolates and imported cases in Qatar in agreement with the FST analysis. However, when K = 4, a clear overlap between the imported parasites to Qatar and parasite in Sudan and Ethiopia (Fig. 4A), suggesting a likely existence of 4 sub-populations (Fig. 4A). Moreover, re-analysis of the data using the imported cases as single population revealed a high relationship between the isolates collected in India with the imported P. vivax in Qatar compared to the parasites in Sudan and Ethiopia (Fig. 4B).
(A) Population Structure. Bar plot illustrating the population structure at K = 2–6 in P. vivax among imported cases in Qatar and parasites from endemic sites in India, Sudan and Ethiopia. Each vertical bar represents an individual sample, and each colour represents one of the K clusters (subpopulations). (B) Population Structure. Bar plot illustrating the population structure at K = 2–6 in P. vivax among imported cases in Qatar and parasites from endemic sites in India, Sudan and Ethiopia. Each vertical bar represents an individual sample, and each colour represents one of the K clusters (subpopulations).
Multiplicity of infection (MOI)
MOI defined as presence of more than one allele in any locus, was high among imported P. vivax from India (67.9%), Sudan (60.6%), and Pakistan (50.5%). Similar, high MOI was seen among local P. vivax in Sudan (44.70%), Ethiopia (67%) and India (62.5%).
Moreover, the minimum number of clones (MNC), estimated as the minimum number of alleles per locus, across all loci, was relatively low among imported P. vivax from India (1.6), Sudan (0.7), and Pakistan (1.2) compared to that seen among endemic parasites in Sudan (2.4), Ethiopia (2.00) and India (2.00).
Discussion
The GCC countries have achieved great success in the fight against malaria. Four out of the six states accomplished complete interruption of malaria transmission and a malaria-free status, while limited sites in southwest Saudi Arabia10 and sporadic outbreaks in Oman14 represent the final stage in the battle to eliminate endemic malaria in the region. However, the above success is threatened by the high influx of imported malaria by young immigrants from endemic countries in the Indian subcontinent (India, Pakistan) and East Africa (Sudan).
The findings of the present study are in line with previous reports, demonstrating that the Indian Subcontinent is the most likely source for imported P. vivax malaria into GCC countries while Africa is the main origin of P. falciparum malaria. For some decades, the oil-rich region has been a popular destination for temporary labour workers, seeking employment opportunities. The high migratory turnover of immigrants from malarious areas is accompanied by increased reports of imported malaria in GCC countries9, reflecting a high vulnerability for re-introduction of malaria in areas where the disease has been eliminated. Though, receptivity, defined as the presence of the Anopheles vector, is limited as the result of current efficient vector control programs8,20. Nonetheless, autochthonous malaria cases were seen near livestock farms and building sites, where a large number of immigrants work, and environmental conditions favour vector habitats14. Analysis of a recent malaria outbreak in Oman identified Anopheles culicifacies as the vector involved14. Therefore, to minimize vulnerability, to re-introduction of malaria, a stringent surveillance system, based on highly sensitive molecular tools, should be structured to ensure timely detection and management of outbreaks seeded by imported malaria.
The vulnerability to re-introduction of local transmission is emphasised by the high prevalence of gametocytes carriage among imported P. vivax in Qatar. Out of 95 P. vivax isolates successfully examined by RT-PCR, 83 (87.37%) harboured gametocytes evident by detectable transcripts of Pvs25 gene. This accords well with the findings of the high prevalence of low-density gametocyte carriage among P. vivax infection in many endemic sites21. P. vivax isolates examined in the present study were obtained from clinical cases. However, imported malaria often exists as asymptomatic low-level parasitaemia detectable only by PCR22 that may easily be missed by traditional microscopy and serological surveillance methods. An additional feature of asymptomatic infection, of particular relevance to prevention of re-introduction in areas where malaria has been eliminated, is its extended longevity. Asymptomatic P. falciparum infection can persist for several years, and discovered only when an individual develops clinical malaria23. Clinical presentations of P. falciparum malaria among immigrants have been found to delay by as long as 8 years after patients have left malaria-endemic areas24. Thus, asymptomatic parasite carriers can sustain long-term threat to malaria elimination programs.
The presence of gametocyte among low-density asymptomatic parasite carriers is well documented25. Amplification-based techniques are sensitive enough to detect and quantify gametocytes as low as 0.02–10 gametocytes per microliter25,26. Such low gametocytes densities are unlikely to be detected by microscopy and can make significant contributions to transmission23,27. In addition, parasites can increase gametocyte conversion rate in response to clues for transmission opportunity25,27,28. For example, the reappearance of Anopheles mosquitoes following the long dry period in areas of seasonal transmission can promote surge in gametocyte densities among asymptomatic parasite carriers26. This may explain the success of imported asymptomatic malaria to raise regular outbreaks in receptive sites, with low mosquito density in some GCC countries such as Oman14 and southern Europe29. Thus, molecular surveillance of migrants from endemic areas, in GCC countries and other receptive areas, can estimate the risk of re-introduction and allow targeted control measures to interrupt potential transmission.
High level of diversity was seen among imported P. vivax parasites into Qatar [average HE = 0.782], similar to that in endemic sites where the majority of imported cases originate, in India [average HE = 0.797] and East Africa (Sudan [average HE = 0.726], Ethiopia [average HE = 0.684]). This is consistent with previous reports on diversity of P. vivax in the Indian Subcontinent30 and East Africa31. The high level of diversity seen among imported P. vivax in Qatar reflects a constant flow of importation of diverse strains from multiple origins. This hypothesis is supported by the close genetic relatedness of imported P. vivax in Qatar and local parasite in India as shown by FST and PCoA analysis (Fig. 3), and some overlap with parasites in East Africa. The introduction of novel lineages into the region can increase effective population size (Ne) and enhance the parasite diversity, as there is a direct relationship between the expected level of diversity and Ne32. In addition, the appearance of drug resistance in countries of origin such as India33, Pakistan34 and Ethiopia35 can augment the ability of the parasite to establish and evolve in the face of current control measures, if local transmission arises.
The extent of diversity among imported P. vivax is higher than that seen amongst P. falciparum reported by immigrants in Qatar at the same time of the present study36. This is in line with data from different endemic areas that examined sympatric P. vivax and P. falciparum populations37. This has been attributed to the fact that the global P. vivax population is older, efficient in transmission, very diverse and less structured than P. falciparum37,38. This is conistsnt with the findings of low level of genetic differentiation between imported P. vivax in Qatar and local parasites in India (FST = 0.0594), and moderate differentiation between imported parasites in Qatar and that in East Africa (Fig. 3). Thus, analysis of imported P. vivax in transmission-free areas and autochthonous malaria in the GCC countries, can predict the genetic relatedness and the likelihood of success of integrated intervention strategy applied across the whole region.
In summary, the present study highlighted the vulnerability of GCC countries to resurgence of malaria via parasite carried by immigrants from endemic areas. Imported P. vivax infection in Qatar is characterised by a high rate of genetic diversity and ability to produce gametocytes to transmit disease. The genetic diversity and complexity of imported parasites can lead to appearance of novel genotypes, that can escape current treatment regimen should local transmission starts. However, the risk of receptivity and malaria resurgence is limited, as a result of adequate vector control programs, despite the presence of local vectors and ecological conditions favourable to malaria transmission39.
Material and Methods
Study sites and P. vivax isolates
A total of 583 patients reported to Hamad Medical Corporation (HMC) and Alkhor Hospital; Hamad General Hospital in Al-Doha city and Alkhor Hospital in the north area are the two main hospitals within HMC that assigned to admit patients with malaria, were examined microscopically for malaria between January 2013 and October 2016. All cases were diagnosed using conventional microscopic examination of Giemsa stained thick (100 fields) and thin blood (1000 RBCs). A total of 448 (76.8%) were found to be positive for the malaria parasites.
All subjects were interviewed using a structured questionnaire to collect demographic information, including age, gender, nationality, history of travel and treatment. Patients were given treatment as per the Ministry of Public Health, Qatar.
The present study focused on analysis of 265 isolates obtained from patients with P. vivax infection, in Qatar. In addition, we also used 137 confirmed infected samples from Sudan, collected in Whatman qualitative filter paper, grade 3 between 2013–2014, 87 confirmed infected samples from Ethiopia collected in Whatman qualitative filter paper, grade 3 between 2010–2013 and 40 confirmed P. vivax samples from India collected between 2014–2016.
Ethical approvals were obtained from the Institutional Review Board of WCM-Q and HMC (Protocol no. 14-00097), ethical committee of the Postgraduate Institute of Medical Education and Research, Chandigarh, India (PGI/IEC/2014/88), Research Review Committee of Institute of Endemic Diseases, University of Khartoum (certificate research number 9/2016), and the Ethiopian isolates were reviewed and approved by the respective Ethical Boards of the Addis Ababa University College of Natural Sciences, Ethiopia (RERC/002/05/2013) and National Research Ethics Review Committee of Ethiopia (Ref.no. 3.10/580/06)35. Samples were collected after obtaining a written informed consent from the patients or guardians. All experiments in this study were performed in accordance with relevant guidelines and regulations of the above institutes.
Extraction of DNA and RNA
DNA was extracted from 200 µl of venous blood from the imported P. vivax isolates in Qatar and parasites collected in India, using QIAamp DNA Blood Mini Kit as described by the manufacturer (QIAGEN,CA, USA). DNA was isolated from blood collected on filter paper (Whatman qualitative filter paper, grade 3) from Sudan and Ethiopia using Chelex extraction method40.
RNA was extracted from 100 µl blood of P. vivax isolate obtained from imported cases in Qatar using SV Total RNA Isolation kit (Promega, UK). Conventional PCR was used to confirm the absence of co-extracted genomic DNA, and then RNA samples were converted to cDNA using the High Capacity cDNA Reverse Transcription Kit (ThermoFisher, UK).
Detection and quantification of total parasitaemia and gametocytes among imported P. vivax in Qatar
Species identification of P. vivax was confirmed using species-specific PCR as described by41. Total parasitaemia was quantified as copy number of the 18S rRNA transcripts in reverse transcriptase quantitative polymerase chain reaction (RT-qPCR) assays based on TaqMan probe chemistry, primers and probes sequences are provided in Table 419. Pv18s rRNA copy numbers were estimated using in-plate standard curve generated from a 10-fold serial dilution (starting with 3.79 × 107 copies/µl, limit of detection 0.37 copy/µl) of a purified PCR product. Gametocytes were detected and quantified using RT-qPCR, targeting transcripts of Pvs25 gene, as described elsewhere21, with the use of modified probes and primers sequences (Table 4).
Genotyping of P. vivax
We examined 9 polymorphic single copy tri-nucleotide repeats microsatellites (MS1, MS5, MS6, MS7, MS8, MS9, MS12, MS15, MS20), distributed across the whole parasite genome. In 25 μl premix containing Taq polymerase (2U), MgCl2 (1.5 mM), dNTPs (50 µM of each dNTPs) and 10 pmole of each primer. PCR conditions were, 94 °C/3 min, 35 cycles at 94 °C/30 s, 59.8 °C/30 s and 72 °C/45 s, and a final extension step at 72 °C/5 min42.
PCR products were analysed using ABI 3130XL Genetic analyser (Applied Biosystems,UK) with relative to an internal reference Genescan 500 LIZ (Applied Biosystems, UK). GeneMapper v4.0 (Applied Biosystems, UK) for allele calling and quantification of peak height43.
Data analysis
Multiplicity of Infection (MOI)
The multiplicity of infection (MOI) refers to presence of more than one allele per isolate at least in one locus. To avoid overestimation of MOI, multiple alleles per locus were scored if electrophoretic peaks corresponding to minor alleles were ≥33% the height of the predominant allele44. The minimum number of alleles across the 9 loci in each sample was calculated and this index value represented the minimum number of clones (MNC) (genotypes) per isolate. Then the average MNC for all isolates in each region was calculated44.
Population genetic indices
Genetic diversity parameters were calculated for the entire dataset using GenAlex v6.545. This included determining the number of alleles per locus, and expected heterozygosity (HE). These two parameters were used to assess the level of polymorphism at each locus and determine diversity. HE was calculated using the formula for ‘unbiased heterozygosity’ also termed haploid genetic diversity, HE = [n/(n − 1)][1 − ∑p2] where n is the number of isolates and p the frequency of each different allele at a locus46.
The predominant allele in each of the examined 9 microsatellites was used to construct multi-locus haplotypes to determine whether the P. vivax populations in different regions comprised a single panmictic population with a high degree of genetic exchange. Multilocus linkage disequilibrium (LD = non-random association of allele among loci) of the alleles at pairs of loci was estimated as the standard index of association (ISA) using the program LIAN version 3.547. The software tests for independent assortment of alleles by determining the number of loci at which each pair of MLGs differs, and from the distribution of mismatch values a variance VD (the variance of the number of alleles shared between all pairs of haplotypes observed in the population) is calculated, which is then compared with the variance expected for LE, termed Ve. The null hypothesis that VD = Ve is tested by a Monte Carlo simulation and a parametric method and the results provide 95% confidence limits, which are denoted LMC and LPARA, respectively. If there is limited or no association between alleles at different loci, indicating panmixia, a value close to zero is obtained, whereas if association is detected, a value significantly greater than 0 is obtained, indicating non-panmixia47. The variance of pairwise difference (VD) between the data and that predicated for panmixia14 and L (LMC & LPARA), were calculated in order to test the hypothesis of panmixia. Therefore, when the VD value exceeds the L value, LD is indicted and the null hypothesis of panmixia is discarded. When the VD is less than L, LE is indicated and the null hypothesis of panmixia is accepted47.
The genetic association between population pairs was evaluated by Wright’s fixation index (FST) using Gene pop web interface48. Molecular variance (AMOVA) was calculated to estimate the variation within and between population and Principal component analysis (PCoA) was used to visualise the relationship between MLGs using GenAlEx 6.545.
Structure software was used to elucidate the genetic structure and to detect the most likely number of clusters (K)49. STRUCTURE analysis runs were performed exploring K from 1 to 6 (10 iterations each), consisting of a burn-in period of 10,000 iterations followed by 100,000 Markov Chain Monte Carlo (MCMC) iterations, assuming a mixture model and correlated allele frequencies. K was defined according to49 by calculating the rate of change of K, ΔK using STRUCTURE HARVESTER v0.6.9450. Additional analysis of structure results was conducted using CLUMMP51 and DISTRUCT52. CLUMMP aligns the cluster assignment across replicate analyses while DISTRUCT performs a graphical display of the aligned cluster assignments.
References
Broderick, C. et al. Clinical, geographical, and temporal risk factors associated with presentation and outcome of vivax malaria imported into the United Kingdom over 27 years: observational study. bmj 350, h1703 (2015).
Färnert, A., Wyss, K., Dashti, S. & Naucler, P. Duration of residency in a non-endemic area and risk of severe malaria in African immigrants. Clinical Microbiology and Infection 21, 494–501, https://doi.org/10.1016/j.cmi.2014.12.011 (2015).
Snow, R. W. et al. The malaria transition on the Arabian Peninsula: progress toward a malaria-free region between 1960–2010. Advances in parasitology 82, 205 (2013).
Al-Mekhlafi, A. M., Mahdy, M. A., Al-Mekhlafi, H. M., Azazy, A. A. & Fong, M. Y. High frequency of Plasmodium falciparum chloroquine resistance marker (pfcrt T76 mutation) in Yemen: an urgent need to re-examine malaria drug policy. Parasites & vectors 4, 94, https://doi.org/10.1186/1756-3305-4-94 (2011).
Meleigy, M. The quest to be free of malaria. Bulletin of the World Health Organization 85, 501–568 (2007).
Cotter, C. et al. The changing epidemiology of malaria elimination: new strategies for new challenges. Lancet 382, 900–911, https://doi.org/10.1016/S0140-6736(13)60310-4 (2013).
Ismaeel, A. Y., Senok, A. C., Jassim Al-Khaja, K. A. & Botta, G. A. Status of malaria in the Kingdom of Bahrain: a 10-year review. Journal of travel medicine 11, 97–101 (2004).
Le Menach, A. et al. Travel risk, malaria importation and malaria transmission in Zanzibar. Scientific Reports 1, 93, https://doi.org/10.1038/srep00093 (2011).
Odolini, S., Gautret, P. & Parola, P. Epidemiology of Imported Malaria in the Mediterranean Region. Mediterranean Journal of Hematology and Infectious Diseases 4, e2012031, https://doi.org/10.4084/MJHID.2012.031 (2012).
El Hassan, I. M. et al. Progress toward malaria elimination in Jazan province, Kingdom of Saudi Arabia: 2000–2014. Malaria journal 14, 444 (2015).
Al-Kuwari, M. G. Epidemiology of imported malaria in Qatar. Journal of travel medicine 16, 119–122, https://doi.org/10.1111/j.1708-8305.2008.00285.x (2009).
Sultan, D. M., Khalil, M. M., Abdouh, A. S., Doleh, W. F. & Al Muthanna, A. A. M. Imported malaria in United Arab Emirates: evaluation of a new DNA extraction technique using nested PCR. Korean J Parasitol 47, 227–233, https://doi.org/10.3347/kjp.2009.47.3.227 (2009).
Iqbal, J., Hira, P. R., Al-Ali, F. & Sher, A. Imported malaria in Kuwait (1985–2000). Journal of travel medicine 10, 324–329 (2003).
Simon, B. et al. An outbreak of locally acquired Plasmodium vivax malaria among migrant workers in Oman. Parasite 24, 25, https://doi.org/10.1051/parasite/2017028 (2017).
WHO, W. H. O. World Malaria Report 2011 (2011).
Beljaev, A. The malaria situation in the WHO eastern Mediterranean region. Meditsinskaia parazitologiia i parazitarnye bolezni, 12–15 (2000).
Mikhail, M., Al-Bursheed, K., Abd, E.-H. A. & Morsy, T. Studies on mosquito borne dieases in Egypt and Qatar. Journal of the Egyptian Society of Parasitology 39, 745–756 (2009).
Okell, L. C., Ghani, A. C., Lyons, E. & Drakeley, C. J. Submicroscopic infection in Plasmodium falciparum-endemic populations: a systematic review and meta-analysis. The Journal of infectious diseases 200, 1509–1517, https://doi.org/10.1086/644781 (2009).
Wampfler, R. et al. Strategies for detection of Plasmodium species gametocytes. PloS one 8, e76316, https://doi.org/10.1371/journal.pone.0076316 (2013).
Coleman, M. et al. A Country on the Verge of Malaria Elimination – The Kingdom of Saudi Arabia. PloS one 9, e105980, https://doi.org/10.1371/journal.pone.0105980 (2014).
Tadesse, F. G. et al. The shape of the iceberg: quantification of submicroscopic Plasmodium falciparum and Plasmodium vivax parasitaemia and gametocytaemia in five low endemic settings in Ethiopia. Malaria journal 16, 99 (2017).
Mangold, K. A. et al. Real-time PCR for detection and identification of Plasmodium spp. Journal of clinical microbiology 43, 2435–2440, https://doi.org/10.1128/JCM.43.5.2435-2440.2005 (2005).
Babiker, H. A., Gadalla, A. A. & Ranford-Cartwright, L. C. The role of asymptomatic P. falciparum parasitaemia in the evolution of antimalarial drug resistance in areas of seasonal transmission. Drug Resistance Updates 16, 1–9 (2013).
Szmitko, P. E., Kohn, M. L. & Simor, A. E. Plasmodium falciparum malaria occurring 8 years after leaving an endemic area. Diag. Micr. Infec. Dis. 63, 105–107, https://doi.org/10.1016/j.diagmicrobio.2008.08.017 (2009).
Babiker, H. A., Schneider, P. & Reece, S. E. Gametocytes: insights gained during a decade of molecular monitoring. Trends in parasitology 24, 525–530, https://doi.org/10.1016/j.pt.2008.08.001 (2008).
Gadalla, A. A. et al. Associations between season and gametocyte dynamics in chronic Plasmodium falciparum infections. PloS one 11, e0166699 (2016).
Bousema, T., Okell, L., Felger, I. & Drakeley, C. Asymptomatic malaria infections: detectability, transmissibility and public health relevance. Nature reviews Microbiology 12, 833–840 (2014).
Reece, S. E., Ali, E., Schneider, P. & Babiker, H. A. Stress, drugs and the evolution of reproductive restraint in malaria parasites. Proceedings of the Royal Society of London B: Biological Sciences, rspb20100564 (2010).
Antinori, S. et al. Severe Plasmodium falciparum malaria in the intensive care unit: A 6-year experience in Milano, Italy. Travel medicine and infectious disease 17, 43–49, https://doi.org/10.1016/j.tmaid.2017.05.012 (2017).
Kim, J. R. et al. Genetic diversity of Plasmodium vivax in Kolkata, India. Malar J 5, 71, https://doi.org/10.1186/1475-2875-5-71 (2006).
Getachew, S. et al. Variation in complexity of infection and transmission stability between neighbouring populations of Plasmodium vivax in Southern Ethiopia. PloS one 10, e0140780 (2015).
Awadalla, P., Walliker, D., Babiker, H. & Mackinnon, M. The question of Plasmodium falciparum population structure. Trends in parasitology 17, 351–353 (2001).
Ghosh, S. K. Molecular monitoring of antimalarial drug resistance in India. Indian Journal of Medical Microbiology 35, 155 (2017).
Raza, A., Ghanchi, N. K., Khan, M. S. & Beg, M. A. Prevalence of drug resistance associated mutations in Plasmodium vivax against sulphadoxine-pyrimethamine in southern Pakistan. Malaria journal 12, 261 (2013).
Getachew, S. et al. Chloroquine efficacy for Plasmodium vivax malaria treatment in southern Ethiopia. Malar J 14, 525, https://doi.org/10.1186/s12936-015-1041-4 (2015).
AL-Rumhi, A. O. H. Genetic Diversity and Transmissibility of Imported P. falciparum into the Malaria Free State of Qatar. Master of Biomedical Science In Biochemistry and Molecular Biology thesis, Sultan Qaboos University (2017).
Jennison, C. et al. Plasmodium vivax populations are more genetically diverse and less structured than sympatric Plasmodium falciparum populations. PLoS neglected tropical diseases 9, e0003634, https://doi.org/10.1371/journal.pntd.0003634 (2015).
Rice, B. L. et al. The origin and diversification of the merozoite surface protein 3 (msp3) multi-gene family in Plasmodium vivax and related parasites. Molecular phylogenetics and evolution 78, 172–184 (2014).
Ahmed, R. I. The most common mosquitoes at Al- Rayyan municipality (Qatar state) and their potential for transmitting malaria. Master of Science/Arts thesis. Qatar University (2015).
Plowe, C. V., Djimde, A., Bouare, M., Doumbo, O. & Wellems, T. E. Pyrimethamine and proguanil resistance-conferring mutations in Plasmodium falciparum dihydrofolate reductase: polymerase chain reaction methods for surveillance in Africa. The American journal of tropical medicine and hygiene 52, 565–568 (1995).
Snounou, G. Genotyping of Plasmodium spp. Nested PCR. Methods in molecular medicine 72, 103–116, https://doi.org/10.1385/1-59259-271-6:103 (2002).
Karunaweera, N. D., Ferreira, M. U., Hartl, D. L. & Wirth, D. F. Fourteen polymorphic microsatellite DNA markers for the human malaria parasite Plasmodium vivax. Molecular Ecology Notes 7, 172–175, https://doi.org/10.1111/j.1471-8286.2006.01534.x (2007).
Kantartzi, S. K. In Methods in Molecular Biology Vol. 1006 Methods in Molecular Biology (ed. Stella K. Kantartzi) XI, 339 (Humana Press, 2013).
Anderson, T. J., Su, X. Z., Bockarie, M., Lagog, M. & Day, K. P. Twelve microsatellite markers for characterization of Plasmodium falciparum from finger-prick blood samples. Parasitology 119(Pt 2), 113–125 (1999).
Peakall, R. & Smouse, P. E. GenAlEx 6.5: genetic analysis in Excel. Population genetic software for teaching and research–an update. Bioinformatics 28, 2537–2539 (2012).
Anon, A. The Evaluation of Forensic DNA Evidence. National Academy Press, Washington, DC (1996).
Haubold, B. & Hudson, R. R. LIAN 3.0: detecting linkage disequilibrium in multilocus data. Bioinformatics 16, 847–849, https://doi.org/10.1093/bioinformatics/16.9.847 (2000).
Rousset, F. Genepop’007: a complete re‐implementation of the genepop software for Windows and Linux. Molecular ecology resources 8, 103–106 (2008).
Evanno, G., Regnaut, S. & Goudet, J. Detecting the number of clusters of individuals using the software structure: a simulation study. Molecular Ecology 14, 2611–2620, https://doi.org/10.1111/j.1365-294X.2005.02553.x (2005).
Earl, D. A. & vonHoldt, B. M. STRUCTURE HARVESTER: a website and program for visualizing STRUCTURE output and implementing the Evanno method. Conservation Genetics Resources 4, 359–361, https://doi.org/10.1007/s12686-011-9548-7 (2012).
Jakobsson, M. & Rosenberg, N. A. CLUMPP: a cluster matching and permutation program for dealing with label switching and multimodality in analysis of population structure. Bioinformatics 23, 1801–1806, https://doi.org/10.1093/bioinformatics/btm233 (2007).
Rosenberg, N. A. Distruct: a program for the graphical display of population structure. Molecular Ecology Notes 4, 137–138, https://doi.org/10.1046/j.1471-8286.2003.00566.x (2004).
Acknowledgements
We would like to thank all patients involved in all study sites. We are grateful to the Medical and Paramedical staff of HMC, Doha, Qatar, for helping with blood samples collection, and the staff of Biochemistry department, college of Medicine and Health Sciences, Sultan Qaboos University, Oman for helping with laboratory analysis. We thank Prof Arnab Pain, King Abdullah University of Science & Technology (KAUST), Saudi Arabia, for comments on an earlier version of the manuscript. MHA is a recipient of a PhD studentship, Sultan Qaboos University, Oman. This work was supported by Qatar National Research Fund (a member of Qatar Foundation), grant [NPRP 5-098-3-021] to AAS.
Author information
Authors and Affiliations
Contributions
A.M.H., B.D., G.H.A., A.S., A.Z.: Experimental laboratory and data analysis. G.S., M.M.M., M.M.A., Z.S.I., S.R., K.H.: Provided materials. A.A., S.A., B.H., I.M.: Conceived and developed idea. A.M.H., B.H.: Manuscript preparation.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelraheem, M.H., Bansal, D., Idris, M.A. et al. Genetic diversity and transmissibility of imported Plasmodium vivax in Qatar and three countries of origin. Sci Rep 8, 8870 (2018). https://doi.org/10.1038/s41598-018-27229-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-27229-z
This article is cited by
-
Influx of diverse, drug resistant and transmissible Plasmodium falciparum into a malaria-free setting in Qatar
BMC Infectious Diseases (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.