Abstract
There is considerable interest in therapeutic transfer of regulatory T cells (Tregs) for controlling aberrant immune responses. Initial clinical trials have shown the safety of Tregs in hematopoietic stem cell transplant recipients and subjects with juvenile diabetes. Our hypothesis is that infusion(s) of Tregs may induce transplant tolerance thus avoiding long-term use of toxic immunosuppressive agents that cause increased morbidity/mortality. Towards testing our hypothesis, we conducted a phase I dose escalation safety trial infusing billions of ex vivo expanded recipient polyclonal Tregs into living donor kidney transplant recipients. Despite variability in recipient’s renal disease, our expansion protocol produced Tregs which met all release criteria, expressing >98% CD4+CD25+ with <1% CD8+ and CD19+ contamination. Our product displayed >80% FOXP3 expression with stable demethylation in the FOXP3 promoter. Functionally, expanded Tregs potently suppressed allogeneic responses and induced the generation of new Tregs in the recipient’s allo-responders in vitro. Within recipients, expanded Tregs amplified circulating Treg levels in a sustained manner. Clinically, all doses of Treg therapy tested were safe with no adverse infusion related side effects, infections or rejection events up to two years post-transplant. This study provides the necessary safety data to advance Treg cell therapy to phase II efficacy trials.
Similar content being viewed by others
Introduction
Kidney transplantation is the treatment of choice for most causes of end stage renal diseases1,2. While transplantation is effective in replacing the non-functional kidney, disparity between donor and recipient major histocompatibility antigens results in massive activation of the recipient’s immune system that, if left unchecked, leads to subsequent rejection of the organ. To prevent this, patients must take immunosuppressive drugs (IS) for life, generally a combination of agents including a calcineurin inhibitor (CNI), and corticosteroids3,4,5,6. However, dependence on IS tempers the substantial benefit obtained from transplantation1,2,3,4,5,6,7,8,9,10,11,12,13. Specifically, CNIs are nephrotoxic, a side effect of significant concern in transplantation while steroids exacerbate osteoporosis and hyperlipidemia, and cause avascular osteonecrosis. Development of alternate therapies that help to minimize the need for lifelong immunosuppression, or to eliminate them entirely through the induction of tolerance, are therefore of great interest.
Regulatory CD4+CD25+ T cells (Treg) derived from the thymus and/or peripheral tissues have been demonstrated to broadly control T cell reactivity14. Importantly, Tregs have been shown to control immune responsiveness to alloantigens and contribute to operational tolerance in pre-clinical transplantation models15,16,17,18,19,20. Initial efforts to evaluate the therapeutic effects of Tregs in humans have focused upon stem cell transplant recipients in an effort to control graft versus host disease (GVHD) or to treat autoimmune diseases21,22,23,24. There have been limited efforts to harness the therapeutic potential of Tregs in clinical solid organ transplantation (SOT), due to challenges with the isolation and expansion of Tregs for clinical use. In this manuscript we have tested the hypothesis whether we can develop a protocol for the isolation and large-scale expansion of human Tregs and conduct a phase I clinical trial of Treg adoptive cell transfer therapy following living donor kidney transplantation. Using our unique expansion protocol and experience with personalized cellular therapies;25 we enrolled nine living donor kidney transplant recipients into a three-tiered dose ranging study (0.5 × 109, 1.0 × 109, 5 × 109 Tregs / recipient). We subsequently monitored these patients post infusion and found maintained levels of Tregs throughout the study period. Importantly, there were no serious adverse events associated with Treg infusion and no clinical rejection events up to two years post-transplant. In addition, we report an in depth characterization of the nine Treg products infused into each recipient.
Results
Subjects
In late 2014, we initiated a Phase 1 trial of autologous polyclonal expanded TReg Adoptive Cell Therapy (TRACT) in living donor kidney transplant recipients, recruited through a Northwestern University Institutional Review Board (IRB) and FDA approved protocol after obtaining informed consent (NCT 02145325, IND 15898). This was a nonrandomized dose-ranging study with 3 tiers of cell dosing (0.5, 1, and 5 × 109 cells infused/recipient) with 3 recipients per dosing tier. The clinical protocol for the trial is graphically shown in (Fig. 1A). The inclusion and exclusion criteria considered in recipient recruitment are described in (Fig. 1B). The target population was adult recipients of living donor renal allografts that would not need hemodialysis during the first week following renal transplantation. Ten subjects were enrolled into this study. One subject was withdrawn following enrollment due to the development of medical problems that precluded him as a kidney transplant candidate. The nine recipients displayed diversity in sex, ethnicity, and cause of end stage renal disease (Fig. 1C). Recipients underwent leukopheresis, approximately one month prior to the kidney transplant. This leukopheresis product was cryopreserved for later isolation and manufacturing of Tregs. Recipients received alemtuzumab induction at the time of kidney transplantation to achieve lymphodepletion, based on our pre-clinical observation that a reduction in circulating effector T cells worked synergistically with Treg infusion to prolong allograft survival15. During the immediate post-transplant period, the recipients were placed on a tacrolimus and mycophenolate-based immunosuppressive drug therapy for rejection prophylaxis. At two months post-transplant, recipients were fully converted off of tacrolimus and onto the mTOR inhibitor sirolimus with the said conversion completed prior to Treg infusion; calcineurin inhibitors such as tacrolimus are known to block the production of IL-2, a critical survival cytokine for Tregs, and the Treg promoting features of sirolimus have been well described26,27,28,29,30. Conversion to sirolimus was successful in all but one patient who developed thrombocytopenia, a known potential side effect of sirolimus. An historical cohort of kidney transplant recipients who received identical induction and maintenance immunosuppression but no Treg infusion was utilized as a control group for comparison of serial immunophenotypic reconstitution over a 12 month period as presented below.
Clinical Protocol and subjects in the Phase I safety trial: (A) Outline of the clinical trial design from initiation to one-year follow-up. Although not listed patients were given intravenous corticosteroids of 500 mg pre-operatively, and weaned to 250 mg, 125 mg and 0 mg on post-operative days 1, 2 and 3 respectively. (B) The inclusion and exclusion criteria. The target population was adult recipients of living donor renal allografts that would not require hemodialysis during the first week following renal transplantation. (C) Demographics of living donor kidney transplant recipients receiving expanded autologous Tregs. Number of Tregs received by the Subjects: 1–3: 0.5 × 109, 4–6: 1 × 109, and 7–9: 5 × 109.
Ex Vivo GMP expansion of recipient Tregs
Building upon our previous preclinical work15, we optimized a protocol for polyclonal human Treg expansion and transitioned this technology to our GMP facility for large scale clinical manufacturing. The protocol for Treg expansion and quality testing are shown in (Fig. 2A); CD4+CD25+ Tregs were isolated from patient’s cryopreserved leukopheresis products using all CliniMACS® system and reagents. Treg expansion was initiated with stimulation using MACS GMP Exp-ACT Beads® and IL-2, TGFβ, and Sirolimus on days 0 and 7. Sirolimus was not added to the culture after day 9. In-process evaluation of the cultures was performed on day 14 and final testing was completed on day 21. The cellular product was harvested on day 21 and expansion beads were removed before Treg infusion into recipients (Fig. 2A). We observed robust expansion and met cell dose requirements in all nine Treg manufacturing runs, despite varying causes of end stage renal disease (Fig. 2B).
Expansion and Profile of nine expanded Treg products: (A) Outline of clinical good manufacturing expansion protocol established at the Mathews Center for Cellular Therapy, Northwestern Memorial Hospital. (B) Absolute cell number of all nine Treg products throughout expansion protocol; black bar represents grand median of all products (n=9). (C) Representative clinical phenotyping of Treg products, specifically CD4+CD25+FOXP3+ expression on post CD25 enrichment (day 0) as well as days 14 and 21 of culture. (D) Represents the average (±SD) of expression of Treg markers CD4; CD25; and FOXP3; also non-Treg markers CD8, CD20, and CD127 throughout expansion protocol (n=9). (E) Heat map of clinical Treg products and controls (day 0) depicting the percentage of methylation within 9 CpG sites of the conserved non-coding sequence 2 of FOXP3 gene in the expanded Tregs (TRK- 01–09; n=4). (F) Average (+SD) of the percent methylation in day 0 control products and day 21 expanded Treg products (n=4). ***p < 0.005, *p < 0.05; GM = growth medium (described under Materials).
Our expansion protocol generated Tregs with a classic CD4+CD25+CD127−FOXP3+ phenotype with < 1% contaminating CD8+ or CD19+ cells throughout culture (Fig. 2C and D). The expanded Tregs demonstrated high FOXP3 expression (Fig. 2D) and DNA demethylation of the FOXP3 promoter (Fig. 2E and F), suggesting the expanded cell product retained regulatory properties.
Expansion alters Treg surface receptor expression
In order for cellular therapies to be effective and survive in vivo they must home to sites of inflammation and secondary lymphoid tissues31,32,33,34 and undergo TCR engagement. Since the total cell product was infused into recipients (~ 98–99% CD4+), we characterized the expression of key chemokine and Treg associated receptors on total CD4+ T cells (Fig. S1A). Interestingly, we found a significant increase in CXCR4 expression post expansion (Fig. S1B). There was also a trend towards increased CXCR3 and CCR7 expression; however they did not reach statistical significance (Fig. S1B). The Treg-associated markers, CD62L, CTLA4, and GARP were all significantly increased post expansion (Fig. S1C). Finally, we observed a maintained memory phenotype with > 80% cells being CD45RO+ and < 10% being CD45RA+ post-expansion. Mean fluorescent intensity (MFI) was in accordance with percentages described above (Fig. S2). Taken together, these data suggested that our expanded Tregs had the ability to home to lymph nodes and exert cell contact mediated suppression through CTLA4 engagement.
Expanded Tregs retained clonal diversity
To assay the breadth and depth of TCR diversity in the expanded Tregs we performed high-throughput sequencing of 6 recipient apheresis samples (before Treg isolation) and day 21 Treg products. We found over 80 percent of the unique V, D, and J rearrangements to be productive, meaning they would produce a functional protein receptor (Fig. S3A). Of those productive rearrangements, we found the clonal diversity, % productive frequency, and top 10-clone frequency significantly decreased post expansion (Fig. S3B). This was likely due to non-expansion of lower frequency clones present in the apheresis product. There was also an increased entropy (i.e. Shannon’s entropy where higher value samples represent greater diversity and lower value samples will share more nucleotide sequences) in the expanded Treg product; however this did not reach statistical significance (Fig. S3B). Overall, Treg receptor diversity was maintained post expansion.
Expanded Tregs were potently suppressive and induced infectious tolerance
We analyzed the suppressive function of our Treg products throughout expansion, on days 0, 14 and 21 using a classic mixed lymphocyte reaction (MLR) suppression assay. Briefly, recipient PBMC’s (R), autologous to the expanded Tregs, were stimulated for 7 days with healthy volunteer allogeneic irradiated PBMCs (Sx) in the presence or absence of expanded Tregs. Treg expansion was associated with an enhanced suppressive potency; when the dose for 50% suppression was assessed, expanded Tregs required 8 fold lower cell number as compared to day 0 Tregs (Fig. 3A and B). MLR inhibition results were comparable on day 14 and day 21 of Treg culture. Therefore, day 14 suppression result was considered the in-process functional test before release and infusion into recipients.
In process testing of Tregs suppressive function: Suppression assays were performed. (R) denotes recipient PBMC’s; (Sx) denotes irradiated healthy allogeneic PBMC’s (stimulators); (Rx) denotes irradiated responder cells used as a control to keep cell number consistent across groups. (A) Graph shows raw count per minutes (±SD in triplicate cultures) of thymidine incorporation assay after six days of culture (representative). (B) Average (±SD) of percent suppression (n = 9) at varying Treg: Tresp ratios throughout clinical expansion protocol. Percent suppression calculated as described in materials and methods.
One mechanism by which Tregs mediate suppression is through de novo Treg generation from recipient’s native T cells, a process known as infectious tolerance35,36. To assess this in vitro, we used the Treg-MLR assay developed in the laboratory37. Briefly, suppression assays as described above were performed however, (R) PBMC’s were labeled with CFSE and (Sx) PBMCs with PKH-26 in presence of Tregs that were also labeled with PKH-26. Seven days later the percentage of CD4+CD127−CD25+FOXP3+ cells derived from the CFSE+PKH-26negative recipient PBMCs that proliferated (diluted CFSE) was calculated (Fig. S4A). We observed a significant increase in the percentage of CD4+CD127−CD25+FOXP3+ Tregs generated in the recipient proliferating PBMC when our Treg product was present compared to baseline (no Tregs present) (Fig. S4B).
Expanded Tregs met all release criteria
As per FDA requirements, prior to release of the expanded Tregs for recipient infusion, cells underwent extensive quality and safety testing (Table 1). It was found that the final formulation met and actually exceeded (Table 1) all the FDA approved release criteria of negative aerobic, anaerobic and fungal contaminations, negative mycoplasma and negative gram stain; <5.0EU/kg endotoxin; >70% viable; >70% CD4+ CD25+; <10% CD8+ and CD19+; <3000 Exp-Act® beads/10E8 cells (Table 1). With an eye toward future clinical trials, which require product potency determination prior to release, we included our MLR suppression assay as a part of the release criteria testing. Initial definition of this parameter was loose with a cut off of 50% suppression at a 1:2 ratio, however, we constantly exceeded this parameter obtaining 50% suppression at >1:16 ratio, thus enabling us to further define this potency level for future clinical trials.
Immune monitoring of recipients post Treg infusion
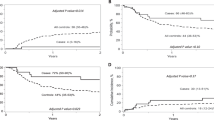
As previously mentioned, lymphocyte depletion, specifically the debulking of circulating effector T cells, was deemed important for the efficacy of Treg cell therapy. Therefore, kidney transplant recipients received alemtuzumab induction and thus displayed a significant decrease in all monitored cell subsets including B cells, NK cells and CD14+ monocytes at one month post-transplant (Fig. 4). By day +90 there was recovery of NK cells, naïve B cells, (Fig. 4) and CD14+ monocytes (not shown). Whereas total CD4+ T cells and total CD8+ T cells were still significantly reduced at day +90, absolute numbers and percentages of Tregs (Fig. 5A and B, respectively) approached or even exceeded pre-transplant circulating levels, a likely consequence of Treg infusion, which was performed on day +60 post-transplant. Most importantly, Treg infusion resulted in 5–20 fold increase in the percentages of Tregs in all subjects and this was stable in most patients until the end of the follow-up period of one year (Fig. 5C). This was in contrast to minimal enhancement of Tregs in a cohort of historical controls that underwent the exact same lymphodepletion and conversion from CNI’s to sirolimus but did not receive a Treg infusion (n = 10) (Fig. 5D).
Immune monitoring of recipients post Alemtuzumab induction and Treg infusion. Absolute cell numbers (symbols) and grand median (- line) of T, B, and NK, Tregs per uL of blood from pre-transplant to 12 months post-transplant in all nine recipients (n = 9). Note: Alemtuzumab was given on day 0 and 2 of transplant, and Tregs were infused at two months post-transplant.
Immune monitoring for Tregs in recipients post Alemtuzumab induction and Treg infusion. (A) Absolute cell numbers per uL of blood, and (B) percentage of Tregs from pre-transplant to 12 months post-transplant in all nine recipients (n = 9). (C) Fold Change in the percentage of Tregs within all nine recipients post Treg infusion when normalized against the pre-transplant percentages. (D) The controls were 10 renal transplant recipients treated with the same conditioning and immunosuppression but did not receive Tregs.
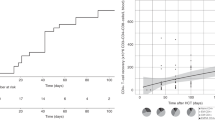
We also examined the recipients’ recall responses to various antigens from pre-transplant to post-Treg infusion to 1 year post-transplant as a measure of their immunocompetence. We found the level of response to PHA, ConA, and CMV reached a nadir immediately post-transplant and gradually recovered even though they never reached the pre-transplant levels (Fig. 6) possibly due to the maintenance immunosuppression. However, it should be noted that no infections occurred in any patient within the year following transplant suggesting a maintained ability to respond to pathogenic antigens.
Recipient’s recall response to various mitogens and antigens: Stimulation indices calculated from the thymidine incorporation assays of recipient PBMCs plus antigen versus recipient PBMCs plus media only. Individual patient responses are displayed as symbols (n=9) and the grand median as –line at indicated time points post-transplant. Pre-Tx = pre-transplant.
Infusion of expanded Tregs into kidney transplant recipients is safe
A potential concern with the infusion of polyclonal expanded Tregs in lymphodepleted/immunosuppressed patients is the development of opportunistic infections and/or malignancies as a consequence of off-target Treg effects. In addition, the well-described plasticity of Tregs has raised concerns that infused cells might develop effector functions and cause rejection. There were no serious adverse events attributable to Treg infusion in any subject (Table 2); importantly, opportunistic infections associated with profound nonspecific immunosuppression, such as polyoma virus nephropathy and tissue invasive CMV disease did not occur in any of the phase 1 trial subjects. Protocol biopsies performed one month after Treg infusion (three months post-transplant) did not show rejection nor did recipients demonstrate donor specific antibody (DSA) development in peripheral blood. At 1 year post-transplant protocol biopsy, there was an episode of subclinical rejection with C4d deposition and de novo DSA development in one patient (subject 8); this was associated with IS non-compliance and was successfully treated with corticosteroids. Additionally subject #1, developed low titer DSA at 1 year post-transplant that was not associated with rejection on biopsy; this patient received the lowest cell tier and had experienced leukopenia requiring marked reduction in mycophenolate dosing making it difficult to determine if the low cell dose or the decrease in mycophenolate was the cause of DSA development. Additional follow up of subjects out to two years was notable for primary disease recurrence in one subject (#1). Patient and graft survival at two years is 100%. Overall, these results demonstrated that infusion up to 5 × 109 polyclonally expanded recipient Tregs into renal transplant patients is safe.
Discussion
Patients that receive transplants are in desperate need of improved immune modulating options to control the alloresponse post-transplant. The long-term side effects of immunosuppressive medications has significantly tempered the short-term benefit of improved allograft survival. Therapeutic cell transfer in an effort to actively control the allogeneic immune response, allowing for minimization or complete elimination of drug based immunosuppression continues to be an unmet need. Initial studies in stem cell transplantation pioneered the way for adoptive Treg cell therapy as an alternative to classic immune suppression. We believe our study represents an important next step to the transition of Treg cell therapy into solid organ transplantation.
Treg cell therapy is still in its infancy with regards to commercialization, during this period of trial and error, there are considerable debates on a multitude of aspects. For example, how “pure” should the initial population be? Does that purity affect expansion? Potency? Efficacy? Purity can be defined differently across GMP cites and clinical centers but generally refers to a CD4+CD25+CD127− phenotype. The only way conclusions and standards will begin to be made is for investigators and centers to share their experience and results. To that end, we utilized an immunomagnetic selection (without CD127 depletion) using the CliniMACS platform for the purification of the starting Tregs. This isolation procedure required only one CliniMACS Plus instrument and 6 hours of labor. Our initial product contained a minor population of CD127+ cells; however, with addition of sirolimus to the expansion media, the final Treg product contained negligible CD127+ cells (Fig. 2D). Other selection methods that include CD127 depletion use BD FACS Canto cell sorters (2 required) and over 20 hours of labor, resulting in a highly “pure” population. (Communications by Sandy Feng, ATC 2017 meeting, Chicago; and Qizhi Tang 3rd Int. Workshop on Tolerance, Stanford, Sept. 8, 2017). We offer our selection and expansion protocol to the cell therapy community as a reproducible, cost-effective, streamlined approach toward commercialization whereas other methods may find trouble transferring their clinical protocols during the manufacturing scale up phase with industry partners. With purity still in mind and how it could affect product potency, we found our expanded Tregs demonstrated enhanced biologic activity, high FOXP3 expression and maintained epigenetic programming. These attributes were not part of the release criteria. However, their robustness is consistent with the notion that potential plasticity associated with Tregs might not be clinically relevant as FOXP3 expression is not inextricably linked with stability, consistent with the work of Sakaguchi et al38,39.
Previous studies have demonstrated that a high ratio of Tregs to conventional CD4+ T cells (Tconv), such as 1:1 or 1:2, may be needed to prevent transplant rejection40,41. A high prevalence of Tregs is, therefore, needed to thwart rejection by establishing a dominant tolerogenic milieu35,42. Considering the relatively small percentage of Tregs at normal steady state in peripheral blood (<5% of circulating CD4+ T cells), a drastic change of Tconv to Treg balance is achieved by, depletion of recipient alloreactive T cells and infusion of a sufficient number of expanded Tregs. As calculated by Tang et al. and ourselves, lymphodepletion using a T cell depleting monoclonal (Alemtuzumab) can reduce the CD4+ Tconv pool by 95–99% to 7.5 × 108 − 4.6 × 109 cells43,44. In our study, the infusion of the Tregs product was also deliberately delayed to allow for “wash out” of alemtuzumab to avoid the unintended destruction of the infused Tregs. In addition, conversion of patients from tacrolimus, which inhibits IL-2 production and theoretically would impair Treg survival, to sirolimus, a Treg-friendly IS agent, was completed before Treg infusion. Since this is a phase I trial we cannot conclude if Treg infusion was the reason why no adverse events or rejection events were observed, despite this deviation from our standard of care IS. However, we believe our approach allows for the best chance for Treg survival and enhanced potency post-infusion.
Only two other centers have successfully completed and published clinical trials utilizing expanded recipient Tregs in the context of solid organ transplantation45. Todo et al., have reported on the use of a “Treg-enriched” product generated in recipient anti-donor MLR in the presence of anti-CD80/86 monoclonal antibodies infused into liver recipients46. Lymphodepletion in subjects was achieved through the use of cyclophosphamide and splenectomy prior to Treg cell transfer. Immunosuppression was successfully weaned in 7 of 10 infused subjects; however, it should be noted that liver transplants are more tolerogenic than other transplants47. It is noteworthy that the “Treg enriched” cells infused by Todo et al. were comprised on average of 58.6% CD4+ and 16.9% CD8+ T cells with 24.8% of the CD4+ T cells expressing CD25+FOXP3+ Tregs. In contrast, our Treg product was composed on average of 98.8% CD4+CD25+, 0.7% CD8+, and ~80% FOXP3+ cells. The heterogeneous composition of the cell product utilized by Todo et al. raises questions as to what populations of cells infused are contributing to the ability to withdraw drug based immunosuppression. Furthermore, it remains unsettled as to what degree of purity of classical Tregs is minimally required for safe and efficacious clinical use. Ongoing work with therapeutic cell transfer using Tregs, such as work herein described, as well as that being conducted by the ONE Study (http://www.onestudy.org/), will hopefully provide additional insight in the near future. Recently, Chandran et al.48, reported on the UCSF experience with the infusion of 0.32 × 109 autologous polyclonal Tregs in kidney recipients. Unlike our phase 1 trial which was the first to be reported and designed to evaluate Tregs as prophylaxis against allograft rejection, this UCSF study used Tregs, to treat subclinical inflammation observed on 6-month protocol biopsies. While only three patients were infused, no adverse infusion reactions or adverse events (treatment related) were observed. Importantly, their study demonstrated recipients that have already undergone transplantation and are on active immunosuppression can have Tregs collected, expanded, and re-infused, which may prove to be essential if additional doses of Tregs are needed for long term efficacy.
It is important to note that we did not observe any adverse clinical events (infection/rejection) following Treg administration at any of the doses used. This suggests that Treg cell therapy using polyclonal autologous Treg product is safe in the context of kidney transplantation. The robust state of lymphodepletion achieved with the conditioning regimen used in our clinical trial allowed to detect a profound and sustained increase in circulating numbers of Tregs in patients receiving Treg infusion. In contrast, contemporaneous historical control patients who received identical conditioning and maintenance IS showed no significant increase in circulating numbers of Tregs (Fig. 5D). Unfortunately the profound lymphodepletion due to the Alemtuzumab treatment also prevented us from a pre-Treg infusion immunophenotyping at 2 months, as the patients did not have sufficient cells in the allowable quantity of blood that could be drawn. We also did not employ methodologies to specifically label and track Tregs, such as deuterium labeling which has been described (47).
De novo DSA development was observed in two subjects in our clinical trial. This was associated with suboptimal immunosuppression due to drug intolerance in one subject and overt noncompliance in the other. DSA development has been associated with reduced long-term renal allograft survival49,50. Importantly, the de novo use of CNI free immunosuppressive regimens with mTOR inhibitors such as sirolimus or everolimus, or CNI conversion to mTOR inhibitor has been associated with an increased risk of developing DSA post-transplant51,52. A recent review concluded that risk of de novo DSA development described with mTOR inhibitor use can be eliminated through combination with reduced CNI exposure53. We have recently reported a prospective randomized study of a steroid free, low dose tacrolimus with everolimus regimen in kidney transplant recipients. Combined low dose tacrolimus and everolimus resulted in greater rejection-free graft survival than standard dose tacrolimus and mycophenolate mofetil. We did not see an increased risk of de novo DSA development in the mTOR arm. Importantly, the combined use of low dose tacrolimus and everolimus was associated with higher circulating numbers of Tregs, indicating this combination provides a favorable milieu for Treg survival (Traitanon O, et al. submitted). Such an mTOR – low dose CNI regimen may be well suited for future therapeutic cell transfer approaches utilizing Tregs.
In conclusion, we have verified our hypothesis that we can develop a protocol for the large-scale isolation and expansion of human Tregs and conduct a phase I clinical trial of Treg adoptive cell transfer therapy following kidney transplantation. This also sets the stage for a phase II clinical trial testing the efficacy of Treg infusion for tolerance induction or drug minimization. It remains to be determined whether Treg therapy, as a single immunomodulatory agent, is capable of inducing immunosuppression-free operational tolerance. Some adjunctive drug-based immunosuppression, or perhaps that combinatorial cell therapy with donor hematopoietic stem cell and Treg infusions maybe required.
Methods
Phase I clinical trial design and approval
The protocol was approved by the Northwestern Institutional Review Boards and the FDA (Clinical trial registration number 02145325 dated May 22, 2014; IND 15898). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained for all subjects. No organs/tissues were procured from prisoners and the organs were procured by Gift of Hope (https://www.giftofhope.org/) and the transplants were performed at the Comprehensive Transplant Center at Northwestern University. Subjects met institutional criteria as suitable living-donor kidney transplant recipients. The Phase 1 clinical trial protocol is provided in the Supplementary Addendum. Briefly, this was a nonrandomized study with 3 dosing tiers (0.5, 1, and 5 × 109 cells infused/recipient,) with 3 recipients per tier. The clinical protocol is graphically shown in (Fig. 1A). Immunosuppression used included the use of induction antibody therapy in the form of alemtuzumab (Campath): 30 mg dose administered IV on day 0 (intraoperatively during kidney transplant) and on day +2 following kidney transplant. Corticosteroid induction (solumedrol 500 mg intravenously day 0, 250 mg day +1, and 125 mg day +2) was also employed; no maintenance oral corticosteroids were used. Maintenance immunosuppression consisted of 1) Mycophenolate (MPA; Myfortic): 720 mg–900 mg dosed twice daily orally starting Day −2 and continued post-transplant, 2) Tacrolimus (Prograf): dosed twice daily orally targeted to 12 hour trough concentrations of 8–12 ng/ml starting Day −2, continued until day +30 when conversion to sirolimus was initiated. Sirolimus (Rapamune) was dosed once daily, targeted to 24 hour trough concentrations of 8–12 ng/ml starting at Day +30 and then continued for the duration post-transplant. Conversion to sirolimus was completed before the infusion of expanded autologous Tregs which took place on Day +60 post-transplant. Protocol kidney biopsies were performed at 3 and 12 months post-transplant.
Leukopheresis and Cryopreservation
Peripheral blood mononuclear cells (PBMCs) were collected from eligible patients by a single leukopheresis, collecting an average of 2.4 × 1010 mononuclear cells. The collected apheresis product was cryopreserved in 10% DMSO in normal saline using a rate controlled freezer. The cryopreserved product was stored in a monitored liquid nitrogen freezer.
Thaw and Selection of CD25+ T-regulatory cells
Thawed apheresis product was washed and suspended in a de-clumping Buffer consisting of Miltenyi PBS/EDTA Buffer, 25% Human Serum Albumin (HSA), MgCl2, and Pulmozyme (Genentech). CD8 and CD19 depletion of the apheresis product, and subsequent CD25+ enrichment was carried out on the CliniMACS Plus using GMP reagents and protocols (Miltenyi). The resulting product was used to expand as the Tregs.
Expansion of Regulatory T cells
Growth media (GM) consisted of TexMACS medium supplemented with 5% heat-inactivated AB serum, 1,000 IU/ml IL-2, 100 ng/ml Sirolimus (SRL: Rapamycin; Sigma Aldrich) and 1 µg/ml TGF-β (Miltenyi). G-Rex bioreactor (Wilson Wolf,) cultures were initiated with 2 × 107 to 3 × 107 cells and Exp-Act® beads at a 4:1 bead: cell ratio. GM was added every two to three days to maintain a cell density of 1 × 106/mL. On Day 7, the cells were restimulated with Exp-Act® beads, at a ratio of 1:1 beads. On Day 14, in-process testing was preformed: 14-day aerobic and anaerobic sterility cultures, 30-day fungal culture, mycoplasma, endotoxin detection, cell counts, viability, phenotyping, and the Treg suppression assay. SRL was not added after Day 9 and cells were harvested on Day 21.
Exp-Act® beads removal and product safety testing
The harvested Treg product was processed on the CliniMACS Plus instrument to remove Exp-Act® beads. The eluted product was evaluated for residual Exp-Act® beads using flow cytometry. Final product safety testing included all tests performed on Day 14 with the addition of residual bead count. (Table 1).
Flow Cytometry
For research expansion samples on days 0, 14 and 21 as well as post-transplant immune monitoring, antibodies against CD4-FITC, CD127-PE, CD3-ECD, CD25-PC7 (all Beckman-Coulter) and FOXP3-PC5 (eBioscience, San Diego, CA) were used. Chemokine and receptor characterizations were performed using CXCR3/GARP-Pacific Blue, CXCR4/CD62L-PerCP-Cy5.5, CCR7/CD45RO-APC-Cy7, CD45RA-Alexa700, and CTLA-4-APC (all from eBioscience, San Diego, CA).
For the GMP expanded Treg products 1–9, three separate panels were used consistently throughout Treg expansion and all antibodies were purchased from Miltenyi. Panel one: CD8-APC, CD20-FITC, CD14/15/56-PE, CD45-Pacific Blue and 7AAD-PerCP-Cy5.5. Panel two: CD25-APC, CD4-FITC, CD127-PE, CD45-Pacific Blue and 7AAD-PerCP-Cy5.5. Panel three: CD4-FITC, CD25-PE, Foxp3-APC and CD45-Pacific Blue. Research grade flow cytometry was performed on a Beckman-Coulter FC500 whereas clinical flow cytometry was done on a BD-LSR, as previously described37,54,55.
Patient post-transplant flow cytometric analyses were done on a Beckman-Coulter FC500 using antibodies (all Beckman-Coulter) against CD4-FITC, CD127-PE, CD3-ECD, CD25-PC7 and FOXP3-PC5 (eBioscience); IL10-FITC, IgD/M-PE, CD19-ECD, CD27-PC5, CD24-PC7; Helios-FITC, CD3-ECD, CD28-PC5, CD8-PC7 and FOXP3-PE (eBioscience), among others.
Treg suppression assay
The responder cells consisted of cryopreserved CD8+CD19+CD4+CD25- cells obtained from pooled non-selected leukopheresis product fractions of Treg isolation, autologous to the Tregs (R-PBMC). They were stimulated with fresh allogeneic third party donor (I-PBMC) at a ratio of 1:1 in U-bottom 96-well plates in triplicate. Tregs or irradiated R-PBMC (control) were added at indicated Treg: Responder ratios at the initiation of the mixed lymphocyte reaction (MLR) suppression assays. After 5 days, 3H-thymidine (1uCi/well) was added to the cultures during the final 16–20 hours and incorporation of 3H-thymidine was used to measure proliferation. The MLR inhibition was quantified as previously described56,57:
Treg Infectious tolerance assay
The ability of expanded Tregs to generate new Tregs infectiously from naïve responder cells was measured using the “Treg-MLR” as described previously37. Recipient CFSE-labeled responder cells (R-PBMC) were stimulated with irradiated and PKH26-labelled I-PBMC in presence of PKH-labelled Tregs. On day 7, flow cytometry was performed on the cultured cells after labeling with CD127-PE, CD4-ECD, CD25-PC7, and FOXP3-PC5. PKH26-labelled modulators were gated out and CD4+ cells that proliferated were analyzed for CD25 and FOXP3 expressions.
Methylation Analysis
Cryopreserved Treg cell pellet were evaluated by EpigenDx for DNA extraction, bisulfite conversion, and pyrosequencing. Percent methylation was calculated as % methylated cytosine/ (% methylated cytosine + unmethylated cytosine).
TCRβ repertoire analysis
Expanded Tregs and apheresis cell pellets of 0.5 × 106 were sent to Adaptive Biotechnologies (Seattle, WA) for survey level TCRβ sequencing. Analyses of the sequencing data including Clonality index and number of productive and unique sequencing reads were done using algorithms developed by Adaptive Biotechnologies.
Mitogen and recall response assay
Lymphoproliferative responses of 1 × 105 recipient PBMCs were determined using optimized concentrations of mitogens and recall antigens using standard radioactive 3H-TdR incorporation assays as previously described55. Stimulation indices (SI) were calculated using the formula: CPM in Experimental Combinations / CPM in Unstimulated Controls.
Statistical Analysis
Paired Student T-tests and Wilcoxon signed rank tests for parametric and nonparametric calculations respectively were used. P values of ≤0.05 were considered statistically significant and are plotted as dotted lines in the Figures.
References
Eggers, P. W. Effect of transplantation on the Medicare end-stage renal disease program. N Engl J Med 318, 223–229, https://doi.org/10.1056/NEJM198801283180406 (1988).
Hariharan, S. et al. Improved graft survival after renal transplantation in the United States, 1988 to 1996. N Engl J Med 342, 605–612, https://doi.org/10.1056/NEJM200003023420901 (2000).
Barry, J. M. Immunosuppressive drugs in renal transplantation. A review of the regimens. Drugs 44, 554–566 (1992).
Suthanthiran, M. & Strom, T. B. Renal transplantation. N Engl J Med 331, 365–376, https://doi.org/10.1056/NEJM199408113310606 (1994).
Helderman, J. H., Van Buren, D. H., Amend, W. J. Jr. & Pirsch, J. D. Chronic immunosuppression of the renal transplant patient. J Am Soc Nephrol 4, S2–9 (1994).
Gaston, R. S. Maintenance immunosuppression in the renal transplant recipient: an overview. Am J Kidney Dis 38, S25–35 (2001).
Pirsch, J. D. et al. Hyperlipidemia and transplantation: etiologic factors and therapy. J Am Soc Nephrol 2, S238–242 (1992).
Shaw, L. M., Kaplan, B. & Kaufman, D. Toxic effects of immunosuppressive drugs: mechanisms and strategies for controlling them. Clin Chem 42, 1316–1321 (1996).
Boubenider, S. et al. Incidence and consequences of post-transplantation lymphoproliferative disorders. J Nephrol 10, 136–145 (1997).
Fishman, J. A. & Rubin, R. H. Infection in organ-transplant recipients. N Engl J Med 338, 1741–1751, https://doi.org/10.1056/NEJM199806113382407 (1998).
DeMario, M. D. & Liebowitz, D. N. Lymphomas in the immunocompromised patient. Semin Oncol 25, 492–502 (1998).
Sia, I. G. & Paya, C. V. Infectious complications following renal transplantation. Surg Clin North Am 78, 95–112 (1998).
Pirsch, J. D., Miller, J., Deierhoi, M. H., Vincenti, F. & Filo, R. S. A comparison of tacrolimus (FK506) and cyclosporine for immunosuppression after cadaveric renal transplantation. FK506 Kidney Transplant Study Group. Transplantation 63, 977–983 (1997).
Wood, K. J. et al. Regulatory cells in transplantation. Novartis Found Symp 252, 177–188, discussion 188–193, 203–110 (2003).
Xia, G., He, J. & Leventhal, J. R. Ex vivo-expanded natural CD4+ CD25+ regulatory T cells synergize with host T-cell depletion to promote long-term survival of allografts. Am J Transplant 8, 298–306, https://doi.org/10.1111/j.1600-6143.2007.02088.x (2008).
Xia, G., He, J., Zhang, Z. & Leventhal, J. R. Targeting acute allograft rejection by immunotherapy with ex vivo-expanded natural CD4+ CD25+ regulatory T cells. Transplantation 82, 1749–1755, https://doi.org/10.1097/01.tp.0000250731.44913.ee (2006).
Heinrichs, J. et al. Regulatory T-Cell Therapy for Graft-versus-host Disease. J Immunol Res Ther 1, 1–14 (2016).
Heinrichs, J. et al. CD8(+) Tregs promote GVHD prevention and overcome the impaired GVL effect mediated by CD4(+) Tregs in mice. Oncoimmunology 5, e1146842, https://doi.org/10.1080/2162402X.2016.1146842 (2016).
Li, J. et al. HY-Specific Induced Regulatory T Cells Display High Specificity and Efficacy in the Prevention of Acute Graft-versus-Host Disease. J Immunol 195, 717–725, https://doi.org/10.4049/jimmunol.1401250 (2015).
Semple, K., Yu, Y., Wang, D., Anasetti, C. & Yu, X. Z. Efficient and selective prevention of GVHD by antigen-specific induced Tregs via linked-suppression in mice. Biol Blood Marrow Transplant 17, 309–318, https://doi.org/10.1016/j.bbmt.2010.12.710 (2011).
Trzonkowski, P. et al. First-in-man clinical results of the treatment of patients with graft versus host disease with human ex vivo expanded CD4+ CD25+ CD127− T regulatory cells. Clin Immunol 133, 22–26, https://doi.org/10.1016/j.clim.2009.06.001 (2009).
Brunstein, C. G. et al. Infusion of ex vivo expanded T regulatory cells in adults transplanted with umbilical cord blood: safety profile and detection kinetics. Blood 117, 1061–1070, https://doi.org/10.1182/blood-2010-07-293795 (2011).
Di Ianni, M. et al. Tregs prevent GVHD and promote immune reconstitution in HLA-haploidentical transplantation. Blood 117, 3921–3928, https://doi.org/10.1182/blood-2010-10-311894 (2011).
Bluestone, J. A. et al. Type 1 diabetes immunotherapy using polyclonal regulatory T cells. Sci Transl Med 7, 315ra189, https://doi.org/10.1126/scitranslmed.aad4134 (2015).
Leventhal, J. et al. Chimerism and tolerance without GVHD or engraftment syndrome in HLA-mismatched combined kidney and hematopoietic stem cell transplantation. Sci Transl Med 4, 124ra128, https://doi.org/10.1126/scitranslmed.3003509 (2012).
Levitsky, J. et al. Allospecific Regulatory Effects of Sirolimus and Tacrolimus in the Human Mixed Lymphocyte Reaction. Transplantation 91, 199–206 (2011).
Gallon, L. et al. Differential Effects of Calcineurin and Mammalian Target of Rapamycin Inhibitors on Alloreactive Th1, Th17, and Regulatory T Cells. Transplantation 99, 1774–1784, https://doi.org/10.1097/tp.0000000000000717 (2015).
Kim, K. W., Chung, B. H., Kim, B. M., Cho, M. L. & Yang, C. W. The effect of mammalian target of rapamycin inhibition on T helper type 17 and regulatory T cell differentiation in vitro and in vivo in kidney transplant recipients. Immunology 144, 68–78, https://doi.org/10.1111/imm.12351 (2015).
Peccatori, J. et al. Sirolimus-based graft-versus-host disease prophylaxis promotes the in vivo expansion of regulatory T cells and permits peripheral blood stem cell transplantation from haploidentical donors. Leukemia 29, 396–405, https://doi.org/10.1038/leu.2014.180 (2015).
Schmidt, A., Eriksson, M., Shang, M. M., Weyd, H. & Tegner, J. Comparative Analysis of Protocols to Induce Human CD4+ Foxp3+ Regulatory T Cells by Combinations of IL-2, TGF-beta, Retinoic Acid, Rapamycin and Butyrate. PLoS ONE [Electronic Resource] 11, e0148474, https://doi.org/10.1371/journal.pone.0148474 (2016).
Sawitzki, B. et al. Regulatory tolerance-mediating T cells in transplantation tolerance. Transplant Proc 33, 2092–2093 (2001).
Lee, I. et al. Recruitment of Foxp3+ T regulatory cells mediating allograft tolerance depends on the CCR4 chemokine receptor. J Exp Med 201, 1037–1044, https://doi.org/10.1084/jem.20041709 (2005).
Zhang, N. et al. Regulatory T cells sequentially migrate from inflamed tissues to draining lymph nodes to suppress the alloimmune response. Immunity 30, 458–469, https://doi.org/10.1016/j.immuni.2008.12.022 (2009).
Graca, L., Cobbold, S. P. & Waldmann, H. Identification of regulatory T cells in tolerated allografts. J Exp Med 195, 1641–1646 (2002).
Francis, R. S. et al. Induction of transplantation tolerance converts potential effector T cells into graft-protective regulatory T cells. Eur J Immunol 41, 726–738, https://doi.org/10.1002/eji.201040509 (2011).
Gershon, R. K. & Kondo, K. Infectious immunological tolerance. Immunology 21, 903–914 (1971).
Levitsky, J. et al. The human “Treg MLR”: immune monitoring for FOXP3+ T regulatory cell generation. Transplantation 88, 1303–1311 (2009).
Ohkura, N. et al. T cell receptor stimulation-induced epigenetic changes and Foxp3 expression are independent and complementary events required for Treg cell development. Immunity 37, 785–799, https://doi.org/10.1016/j.immuni.2012.09.010 (2012).
Sakaguchi, S., Miyara, M., Costantino, C. M. & Hafler, D. A. FOXP3+ regulatory T cells in the human immune system. Nat Rev Immunol 10, 490–500, https://doi.org/10.1038/nri2785 (2010).
Hara, M. et al. IL-10 is required for regulatory T cells to mediate tolerance to alloantigens in vivo. J Immunol 166, 3789–3796 (2001).
Graca, L. et al. Both CD4(+)CD25(+) and CD4(+)CD25(−) regulatory cells mediate dominant transplantation tolerance. J Immunol 168, 5558–5565 (2002).
Kendal, A. R. et al. Sustained suppression by Foxp3+ regulatory T cells is vital for infectious transplantation tolerance. J Exp Med 208, 2043–2053, https://doi.org/10.1084/jem.20110767 (2011).
Tang, Q. & Lee, K. Regulatory T-cell therapy for transplantation: how many cells do we need? Curr Opin Organ Transplant 17, 349–354, https://doi.org/10.1097/MOT.0b013e328355a992 (2012).
Mathew, J. M. et al. Generation and Characterization of Alloantigen-Specific Regulatory T Cells For Clinical Transplant Tolerance. Scientific Reports 8, 1136, https://doi.org/10.1038/s41598-018-19621-6 (2018).
Todo, S. et al. A pilot study of operational tolerance with a regulatory T-cell-based cell therapy in living donor liver transplantation. Hepatology 64, 632–643, https://doi.org/10.1002/hep.28459 (2016).
Todo, S. & Yamashita, K. Anti-donor regulatory T cell therapy in liver transplantation. Hum Immunol 79, https://doi.org/10.1016/j.humimm.2017.12.010 (2018).
Knechtle, S. J. & Kwun, J. Unique aspects of rejection and tolerance in liver transplantation. Semin Liver Dis 29, 91–101, https://doi.org/10.1055/s-0029-1192058 (2009).
Chandran, S. et al. Polyclonal Regulatory T Cell Therapy for Control of Inflammation in Kidney Transplants. Am J Transplant 17, 2945–2954, https://doi.org/10.1111/ajt.14415 (2017).
Wiebe, C. et al. Evolution and clinical pathologic correlations of de novo donor-specific HLA antibody post kidney transplant. Am J Transplant 12, 1157–1167, https://doi.org/10.1111/j.1600-6143.2012.04013.x (2012).
Everly, M. J. et al. Incidence and impact of de novo donor-specific alloantibody in primary renal allografts. Transplantation 95, 410–417, https://doi.org/10.1097/TP.0b013e31827d62e3 (2013).
Rostaing, L. et al. Fibrosis progression according to epithelial-mesenchymal transition profile: a randomized trial of everolimus versus CsA. Am J Transplant 15, 1303–1312, https://doi.org/10.1111/ajt.13132 (2015).
Liefeldt, L. et al. Donor-specific HLA antibodies in a cohort comparing everolimus with cyclosporine after kidney transplantation. Am J Transplant 12, 1192–1198, https://doi.org/10.1111/j.1600-6143.2011.03961.x (2012).
O’Leary, J. G. et al. The Influence of Immunosuppressive Agents on the Risk of De Novo Donor-Specific HLA Antibody Production in Solid Organ Transplant Recipients. Transplantation 100, 39–53, https://doi.org/10.1097/TP.0000000000000869 (2016).
Leventhal, J. R. et al. Interim Results of a Phase 1 Trial of Treg Adoptive Cell Transfer (TRACT) in Living Donor Kidney Transplant Recipients. Am J Transplant 15, 3031 (2015).
Leventhal, J. R. et al. Nonchimeric HLA-Identical Renal Transplant Tolerance: Regulatory Immunophenotypic/Genomic Biomarkers. Am J Transplant 16, 221–234, https://doi.org/10.1111/ajt.13416 (2016).
Mathew, J. M. et al. Donor bone marrow-derived chimeric cells present in renal transplant recipients infused with donor marrow. I. Potent regulators of recipient antidonor immune responses. Transplantation 70, 1675–1682 (2000).
Levitsky, J., et al Inhibitory Effects of Belatacept on Allospecific Regulatory T-Cell Generation in Humans. Transplantation 96, 689–696, https://doi.org/10.1097/TP.1090b1013e31829f31607 (2013).
Acknowledgements
We would like to thank the kidney donors and recipients that participated in the study. We also like to thank Adaptive Biotechnologies for their fruitful contribution to this work. This study was funded in part by NMH Woman’s Board, Mathews Endowment for Regenerative Medicine and TRACT Therapeutics Inc.
Author information
Authors and Affiliations
Contributions
J.M.M. contributed to the experimental design, data analysis, and manuscript composition and editing. J.H.V. contributed to data acquisition and analysis, and manuscript composition and editing. J.H.; X.H.; and I.K. collected and analyzed data. A.L.; and C.S. manufactured the GMP Treg product for infusion, performed and reported all regulatory compliance testing. L.G.; M.J.A.; and A.S.; contributed to the recruitment and initiation of patients into the clinical trial, provided editing for manuscript submission. J.R.L. contributed to the experimental design, data analysis, patient recruitment and follow-up; manuscript composition and editing.
Corresponding authors
Ethics declarations
Competing Interests
J.R.L is Co-founder and Clinical Advisor of TRACT Therapeutics; Inc.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mathew, J.M., H.-Voss, J., LeFever, A. et al. A Phase I Clinical Trial with Ex Vivo Expanded Recipient Regulatory T cells in Living Donor Kidney Transplants. Sci Rep 8, 7428 (2018). https://doi.org/10.1038/s41598-018-25574-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-25574-7
This article is cited by
-
Kidney transplants from elderly donors: what we have learned 20 years after the Crystal City consensus criteria meeting
Journal of Nephrology (2024)
-
Feasibility of manufacture of chimeric antigen receptor-regulatory T cells from patients with end-stage renal disease
Translational Medicine Communications (2023)
-
Regulatory T cells in autoimmune kidney diseases and transplantation
Nature Reviews Nephrology (2023)
-
Typical and atypical properties of peripheral nerve allografts enable novel strategies to repair segmental-loss injuries
Journal of Neuroinflammation (2022)
-
Regulatory T cells in ischemic stroke
Acta Pharmacologica Sinica (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.