Abstract
High body mass index (BMI) predisposes to several chronic diseases, but a large-scale systematic and detailed study of dose-response relationship between BMI and chronic diseases has not been reported previously. In this study, we aimed to investigate the relationship between BMI and 3 chronic diseases (hypertension, dyslipidemia and MetS) in northeast China. A sample of 16412 participants aged 18~79 years old were included in Jilin province in 2012. The lambda-mu-sigma (LMS) method was applied to examine the trend of BMI by age, and the restricted cubic splines were used to investigate the non-linear associations (dose-response curve) between BMI and chronic diseases. It was pointed out that BMI increased rapidly when young, then kept steady in middle age, and finally declined slowly in old age, and accordingly age was divided into 3 segments, which were different by gender. The odds ratios (ORs) of BMI for the chronic diseases increased relatively slowly when young, then increased dramatically in middle-age and old population, especially for men. Further, the ORs of BMI among non-smokers were lower than those among smokers, and the same trend was shown to be more apparent among drinkers and non-drinkers. The risk of BMI for common chronic diseases increased dramatically in middle-aged, especially for men with drinking and smoking habits.
Similar content being viewed by others
Introduction
Obesity is believed as a major risk factor for common chronic diseases, like hypertension, dyslipidemia, diabetes and metabolic syndrome (MetS)1,2. And the prevalence of obesity is developing extremely fast worldwide nowadays, especially in China3,4. Therefore, understanding the effects of obesity on chronic diseases has never been more urgent, given the rapid rise in obesity worldwide in recent years5,6.
Many obesity indices have been used in the literatures, such as body mass index (BMI), waist circumference (WC) and waist-hip ratio, which have measured the obesity from different angles and in different aims. Whereas, a lot of studies have pointed out that BMI is not only a good predictor in the chronic disease studies7,8,9,10, but also has more classification (“Underweight”, “Normal weight”, “Overweight” and “Obese”) compared with other indices11,12,13,14. Therefore, BMI has become one of the most frequently used indices for obesity in the chronic disease studies.
However, it also has brought great limitations, because BMI is treated as a categorical variable in most studies. On one hand, it is illogical that the OR of the “Overweight” (with BMI from 25 to 30 kg/m2) was 2.03, while the OR rocketed to 6.11 for “Obese” (with BMI ≥30 kg/m2)8, especially those with BMI around 30 kg/m2. The comparison of the results from different populations is a little complex and hard to be standardized, due to the inconsistent cut-offs. On the other hand, the development of obesity is a continuous and long-term process, the categorical variable was less powerful and less sensitive in measuring the extent of obesity in its progress. Therefore, a continuous BMI is believed to be better than a categorical one in evaluating the obesity.
Fortunately, the dose-response curve can provide the continuous ORs15, especially for the non-linear associations between BMI and chronic diseases. In addition, the restricted cubic splines is one of the most ideal function models used in dose-response analysis, which allows the risk to vary without sudden jump from one interval to the next one16. In this study, we aimed to investigate the continuous ORs of BMI on three common chronic diseases (hypertension, dyslipidemia and MetS) in Jilin province in 2012. The BMI-chronic disease associations were analyzed stratified by gender, age, smoking and drinking status. We found that the ORs of BMI for 3 chronic diseases showed a nonlinear increased tendency with BMI, and the curves were different among the diseases.
Results
Descriptive characteristics of the participants by age
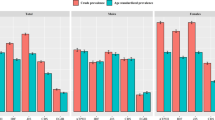
Figure 1 shows the smoothed BMI percentile curves by age for males and females. In males, BMI increased from 18 to 39 years old, then kept steady from 40 to 59 years old, and declined slowly after 60 years old. While in females, the BMI increased rapidly from 18 to 44 years old, then relatively stable from 45 to 64 years old, and finally decreased after 65 years old. Thus, 18~39, 40~59 and 60~79 can be viewed as BMI rising (Young), stable (Middle-age) and decline (Old) age groups for men, and 18~44, 45~64 and 65~79 were corresponding age groups for women.
The descriptive characteristics of the participants were shown in Table 1. The differences for all variables under consideration among age groups were statistically significant, where BMI and the prevalence of common chronic diseases were associated with age. Further, it was implied that the prevalence of common chronic diseases increased with age, which was different from the trend of BMI by age, so the subsequent analyses were listed respectively by age groups.
Association between BMI and chronic diseases with 95% CI
Figure 2 shows how the ORs of BMI developed in hypertension by gender and age. Generally, the ORs increased with BMI in hypertension, and for both males and females under different age groups. Further, the ORs of BMI increased relatively slowly in young group, and accelerated in middle-age and old groups. The dose-response curves for dyslipidemia and MetS showed the similar trend (see details in part 3 of the supplementary file), but the results for diabetes were not included, due to the relatively lower prevalence, which may cause unreliable tendency. Given the same BMI, the ORs of BMI were larger in old group than those in other age groups. Moreover, the 95% CIs of BMI beyond 18~30 were a little wider, due to that less than 10% participants were with BMI < 18 or BMI > 30, that was, the tendency of BMI within the range 18~30 was relatively reliable and stable.
Comparison of the BMI-chronic diseases associations by gender
The trends for ORs of BMI were similar among chronic diseases by gender, except dyslipidemia. The associations between BMI and chronic diseases were more marked in men than women in most cases (Fig. 3), and the ORs of higher BMI in males were extremely greater than those in females in dyslipidemia. Moreover, the ORs of BMI among dyslipidemia in females were fairly low as BMI increased. It should be pointed out that the gender gap in ORs of BMI peaked in the middle-aged.
Comparison of the BMI-chronic diseases associations by smoking and drinking status
Finally, smoking and drinking status were investigated, and Table 2 shows the prevalence of the chronic diseases under different smoking and drinking status, respectively. Similarly, Figs 4 and 5 shows how the ORs of BMI developed in hypertension, dyslipidemia and MetS for males under different smoking and drinking status, respectively (the results for women were not included, due to the relatively low prevalence of smoking and drinking, which may cause unreliable tendency). Generally, the trends of ORs of BMI were similar for either smoking or drinking, especially among young participants, and the ORs of BMI in the middle-age population with smoking or drinking habits had obviously increased. Meanwhile, the ORs of BMI among non-smokers were a little lower than those among smokers, but such analysis towards drinking status was different, that is, the ORs of BMI among drinkers were almost uniformly higher than those among non-drinkers.
Discussion
In this study, dose-repose curve was applied to provide the continuous ORs of BMI on hypertension, dyslipidemia and MetS in Jilin province in 2012. It was pointed out that the ORs of BMI for hypertension, dyslipidemia and MetS increased with BMI, and the ORs speeded up since middle age. The ORs of BMI for chronic diseases were usually more marked in men than those in women, especially for dyslipidemia. Moreover, the ORs of BMI among men with drinking and/or smoking habits were generally higher than those without these habits, and the differences were even more apparent in the analysis of drinking status.
Firstly, age is believed as an influencing factor for both BMI and the chronic diseases, which was divided into 3 segments in this study according to the smoothed BMI percentile curves. Women were 5 years older than men in different segments, which was consistent with the fact that the life expectancy of women was 5 years older than men17. And other studies also pointed out that BMI increased faster among young participants than the middle-aged group, and the rate of increase slowed down among old-aged group14. Further, men were more likely to be overweight than women in the young group, which was consistent with other studies18,19.
Compared with previous analyses7,8,9, the dose-response analysis we have employed is more appropriate, because the continuous ORs are more accurate, and the dose-response curve is better to reflect the overall trend for the ORs of BMI. It was found that the ORs of BMI for hypertension, dyslipidemia and MetS increased with BMI, and they had accelerating trend to go up in middle-aged. Besides, previous studies also have documented that the people aged 40–60 were more likely to suffer from chronic diseases20, and we provided a new insight from the perspective of graphical. Further, the basal metabolic rate of middle-aged people were lower than that of young people21,22, while the body functioning of young people were better than that of middle-aged, which might cause the ORs of BMI for chronic diseases among middle-aged were larger those among young people.
The other thing needs to be noticed is that the ORs of BMI for all 3 common chronic diseases were usually more marked in men than women, especially in dyslipidemia. The reason that men tended to have larger ORs of BMI for chronic diseases might be ascribed to the great differences in the diet and habits between genders, for example, men tended to smoke, drink (Tables 1 and 3) and eat more meat23,24. Another possible explanation was the differences in body function, e.g., estrogen was believed to play an important role in fat metabolism regulation, and to restrain fat accumulated in waist25,26,27. This might be the reason for such significant difference in dyslipidemia between males and females, since estrogen might help females to decline the risk of BMI towards dyslipidemia.
Furthermore, the rates of smoking and drinking were extremely high in Jilin province28, compared with the Chinese average rates29,30,31. And some studies also suggested that smoking/drinking was tightly linked with both obesity and chronic diseases32,33,34. Most researchers focused on young and elderly smokers rather than the middle-aged smokers35,36, while we found that the middle-aged smokers had the higher ORs of BMI for chronic diseases. One possible reason was that the middle-aged people suffer from decline in organ function21. Moreover, Prabhat et al.37 suggested that the risk of diseases was decreased if quitting smoking happens before the age of 40.
Many researches pointed out that alcohol consumption is a major contributor to the prevalence of chronic diseases30,38,39, which was consistent with our study. Moreover, a report from NHFPC (National Health and Family Planning Commission) indicated that the drinking rates in China had a rising tendency (Table 3) these years30,31, while the smoking rates had an expected downward trend. What’s more, the excessive consumption of alcohol had been paid more attention to, and the relevant policies had been adopted in most developed countries, such as USA and UK40,41,42,43. Whereas, there is no relevant laws or regulations to curb excessive consumption of alcohol in China. Therefore, controlling or stopping excessive consumption of alcohol became particularly urgent, especially for men with large BMI.
Some limitations of our studies should be pointed out here. Firstly, the smoking and drinking status of the participants were self-report, which might be subject to reporting bias. Secondly, gender, age, smoking and drinking statuses were investigated in our study; however, other confounders which might have impacts on these chronic diseases, such as physical activity, diet and genes, were not under our consideration this time, which might have some slight effects on our results. Finally, the results were conducted from a cross-sectional study in Jilin province, which might limit our ability to generalize the results.
Conclusions
The ORs of BMI for hypertension, dyslipidemia and MetS increased with BMI, and the risk of BMI had shown an accelerating trend to go up in middle-aged. The ORs of BMI among men with drinking and/or smoking habits were generally higher than those without these habits, and the differences were even more apparent in the analysis of drinking status.
Methods
Study population
Data were derived from a cross-sectional survey in Jilin Province of China in 2012. A total of 23050 participants who had lived in Jilin Province for more than 6 months and were 18–79 years old were selected through multistage stratified random cluster sampling44 (see details in Part 1 of the Supplementary Material online). For the purpose of the present analyses, some subjects were excluded due to missing values (6175 subjects) and the other subjects were excluded due to the fact that they were limited to do independent activities (463 subjects, who were paralyzed, disabled and other diseases that led to inactivity). Finally, a total of 16412 subjects were included in the present analyses.
Data measurement
Height (cm) was measured to the nearest 0.5 cm using a portable stadiometer against the wall, with participants standing in an upright position on a flat surface without shoes, with the back of the heels and the occiput on the stadiometer. Weight (kg) was measured to the nearest 0.1 kg, using an electronic digital scale. BMI was calculated by dividing weight in kilograms by height in meters squared. Blood pressure was measured using mercury sphygmomanometer in the sitting position after a 10-min rest period by trained professionals. Two readings each of SBP and DBP were recorded, and the average of each measurement was used for data analysis. If the first two measurements differed by more than 5 mmHg, additional two readings were taken. Fasting glucose and serum lipids were measured in plasma samples by using a fingertip blood glucose monitor (Bayer, Leverkusen, Germany) and a MODULE P800 biochemical analysis machine (Roche Co., Ltd., Shanghai, China) (see details in Part 2 of the Supplementary Material).
Assessment criteria
Hypertension was referred to those with systolic blood pressure (SBP) ≥140 mm Hg, diastolic blood pressure (DBP) ≥90 mm Hg, and/or the use of antihypertensive medications over the past 2 weeks45. Dyslipidemia was based on triglyceride (TG) ≥1.7 mmol/L, total cholesterol (TC) ≥5.2 mmol/L, high-density lipoprotein cholesterol (HDL-C) < 1.0 mmol/L, low-density lipoprotein cholesterol (LDL-C) ≥3.4 mmol/L46. Diabetes was defined as the use of hypoglycemic agents over the past 2 weeks or a self-reported history of diabetes or FBG ≥7.0 mmol/L47. MetS48,49 was defined as three or more of the following conditions clustered in one subject: a) WC ≥85 cm for males or ≥80 cm for females; b) TG ≥1.7 mmol/L; c) HDL-C < 1.00 mmol/L for males or <1.30 mmol/L for females; d) SBP ≥130 mmHg and DBP ≥85 mmHg, or ongoing antihypertensive drug therapy; and e) FBG ≥5.6 mmol/L or ongoing anti-diabetic drug treatment. Smoking was defined as having smoked at least one cigarette per day and more than 100 cigarettes in total over the past 30 days. Participants who drank alcoholic beverages at least once a week were characterized as drinkers.
Statistical analysis
The continuous variables were expressed as means ± standard deviations (SD) and compared using the t test. The categorical variables were expressed as counts or percentages and compared using the Rao-Scott-χ2 test. The LMS method in the VGAM package was used to determine the trends of BMI by age, and the restricted cubic splines in the Hmisc package were used to investigate the dose-response curve of BMI-chronic diseases associations. All statistical analyses were performed with R version 3.3.2 (University of Auckland, Oakland, New Zealand). Statistical significance was set at a P value < 0.05.
About the data
The survey was implemented by School of Public Health, Jilin University and Jilin Center for Disease Control and Prevention in Jilin Province in 2012. According to relevant regulations, we were sorry that the data can’t be shared.
References
Cripps, C. & Roslin, M. Endoluminal Treatments for Obesity and Related Hypertension: Updates, Review, and Clinical Perspective. Current hypertension reports 18, 79 (2016).
Susic, D. & Varagic, J. Obesity: A Perspective from Hypertension. The Medical clinics of North America 101, 139–157 (2017).
Wang, Z. et al. Current prevalence rates of overweight, obesity, central obesity, and related cardiovascular risk factors that clustered among middle-aged population of China. Zhonghua liu xing bing xue za zhi 35, 354–358 (2014).
Andegiorgish, A. K., Wang, J., Zhang, X., Liu, X. & Zhu, H. Prevalence of overweight, obesity, and associated risk factors among school children and adolescents in Tianjin, China. European journal of pediatrics 171, 697–703 (2012).
World Health Organization. World health statistics 2011. (World Health Organization, 2011).
Bhaskaran, K. et al. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet 384, 755–765 (2014).
Bennasar-Veny, M. et al. Body adiposity index and cardiovascular health risk factors in Caucasians: a comparison with the body mass index and others. PloS one 8, e63999 (2013).
Diederichs, C. & Neuhauser, H. The incidence of hypertension and its risk factors in the German adult population: results from the German National Health Interview and Examination Survey 1998 and the German Health Interview and Examination Survey for Adults 2008-2011. Journal of hypertension 35, 250–258 (2016).
Bays, H. E., Chapman, R. H. & Grandy, S. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: comparison of data from two national surveys. International journal of clinical practice 61, 737–747 (2007).
Ibe, A. & Smith, T. C. Diabetes in US women on the rise independent of increasing BMI and other risk factors; a trend investigation of serial cross-sections. BMC public health 14, 954 (2014).
Kawada, T. Body mass index is a good predictor of hypertension and hyperlipidemia in a rural Japanese population. Int J Obesity 26, 725–729 (2002).
Weber, M. A. et al. Effects of body size and hypertension treatments on cardiovascular event rates: subanalysis of the ACCOMPLISH randomised controlled trial. Lancet 381, 537–545 (2013).
Brown, C. D. et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res 8, 605–619 (2000).
Ouyang, Y. et al. Use of quantile regression to investigate changes in the body mass index distribution of Chinese adults aged 18-60 years: a longitudinal study. BMC public health 15, 278 (2015).
Polesel, J. et al. Estimating dose-response relationship between ethanol and risk of cancer using regression spline models. Int J Cancer 114, 836–841 (2005).
Desquilbet, L. & Mariotti, F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 29, 1037–1057 (2010).
World Health Organization. World health statistics 2015. (World Health Organization, 2015).
Tatsumi, Y. et al. BMI percentile curves for Japanese men and women aged 20–79 years who underwent a health check-up in 1980 and 2005. Obesity research & clinical practice 7 e401–406 (2013).
Gotay, C. C. et al. Updating the Canadian obesity maps: an epidemic in progress. Canadian journal of public health 104, e64–68 (2012).
Turin, T. C. et al. Hypertension and lifetime risk of stroke. Journal of hypertension 34, 116–122 (2016).
Christensen, R. A., Raiber, L., Wharton, S., Rotondi, M. A. & Kuk, J. L. The associations of resting metabolic rate with chronic conditions and weight loss. Clinical obesity 7, 70–76 (2017).
Schwartz, A. & Doucet, E. Relative changes in resting energy expenditure during weight loss: a systematic review. Obesity reviews: an official journal of the International Association for the Study of Obesity 11, 531–547 (2010).
Muga, M. A., Owili, P. O., Hsu, C. Y., Rau, H. H. & Chao, J. C. Association between Dietary Patterns and Cardiovascular Risk Factors among Middle-Aged and Elderly Adults in Taiwan: A Population-Based Study from 2003 to 2012. PloS one 11, e0157745 (2016).
Park, K. et al. Unprocessed Meat Consumption and Incident Cardiovascular Diseases in Korean Adults: The Korean Genome and Epidemiology Study (KoGES). Nutrients 9, 498 (2017).
Maffei, L. et al. A novel compound heterozygous mutation of the aromatase gene in an adult man: reinforced evidence on the relationship between congenital oestrogen deficiency, adiposity and the metabolic syndrome. Clinical endocrinology 67, 218–224 (2007).
Luglio, H. F. Estrogen and body weight regulation in women: the role of estrogen receptor alpha (ER-alpha) on adipocyte lipolysis. Acta medica Indonesiana 46, 333–338 (2014).
Spangenburg, E. E., Wohlers, L. M. & Valencia, A. P. Metabolic Dysfunction Under Reduced Estrogen Levels: Looking to Exercise for Prevention. Exerc Sport Sci Rev 40, 195–203 (2012).
Wang, S. B. et al. Prevalence and patterns of multimorbidity in northeastern China: a cross-sectional study. Public health 129, 1539–1546 (2015).
Commission(NHFPC), N. H. a. F. P. Regulations on the control of smoking in public (2014).
Commission(NHFPC), N. H. a. F. P. An Analysis Report of National Health Services Survey in China (2008).
Commission(NHFPC), N. H. a. F. P. An Analysis Report of National Health Services Survey in China (2013).
Shield, K. D., Parry, C. & Rehm, J. Chronic Diseases and Conditions Related to Alcohol Use. Alcohol Res-Curr Rev 35, 155–171 (2013).
Quinones, A. R. et al. Racial and ethnic differences in smoking changes after chronic disease diagnosis among middle-aged and older adults in the United States. BMC geriatrics 17, 48 (2017).
Watanabe, T. et al. Association between Smoking Status and Obesity in a Nationwide Survey of Japanese Adults. PloS one 11, 926 (2016).
Kleykamp, B. A. & Heishman, S. J. The older smoker. Jama 306, 876–877 (2011).
Shaw, B. A., McGeever, K., Vasquez, E., Agahi, N. & Fors, S. Socioeconomic inequalities in health after age 50: are health risk behaviors to blame? Soc Sci Med 101, 52–60 (2014).
Jha, P. et al. 21st-Century Hazards of Smoking and Benefits of Cessation in the United States. New Engl J Med 368, 341–350 (2013).
Forouzanfar, M. H. et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386, 2287–2323 (2015).
Lim, S. S. et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2224–2260 (2012).
Sacks, J. J., Gonzales, K. R., Bouchery, E. E., Tomedi, L. E. & Brewer, R. D. 2010 National and State Costs of Excessive Alcohol Consumption. American journal of preventive medicine 49, e73–79 (2015).
Burton, R. et al. A rapid evidence review of the effectiveness and cost-effectiveness of alcohol control policies: an English perspective. The Lancet 389, 1558–1580 (2016).
Tansil, K. A. et al. Alcohol Electronic Screening and Brief Intervention: A Community Guide Systematic Review. American journal of preventive medicine 51, 801–811 (2016).
Stahre, M., Roeber, J., Kanny, D., Brewer, R. D. & Zhang, X. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Preventing chronic disease 11, E109 (2014).
Wang, C. et al. Awareness, treatment, control of diabetes mellitus and the risk factors: survey results from northeast China. PloS one 9, e103594 (2014).
Yip, G. W. K. et al. Oscillometric 24-h ambulatory blood pressure reference values in Hong Kong Chinese children and adolescents. J Hypertens 32, 606–619 (2014).
Gu, D. F. et al. Prevalence of cardiovascular disease risk factor clustering among the adult population of china - Results from the International Collaborative Study of Cardiovascular Disease in Asia (InterAsia). Circulation 112, 658–665 (2005).
Gao, B. X., Zhang, L. X., Wang, H. Y. & D, C. N. S. C. K. Clustering of Major Cardiovascular Risk Factors and the Association with Unhealthy Lifestyles in the Chinese Adult Population. Plos One 8, 780 (2013).
Wu, Y. H. et al. Zinc Finger Protein 259 (ZNF259) Polymorphisms are Associated with the Risk of Metabolic Syndrome in a Han Chinese Population. Clin Lab 61, 615–621 (2015).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120 1640–1645 (2009).
Acknowledgements
I would like to express my gratitude to all those who have helped me during the writing of this thesis. This work was supported by the Natural Science Foundation of Science and Technology Department of Jilin Province, China (grant number: 20180101129JC), the Outstanding Youth Foundation of Science and Technology Department of Jilin Province, China (grant number: 20170520049JH); the National Natural Science Foundation of China (grant number: 11301213, 11571068); the National Key Research and Development Program of China (grant number: 2016YFC1303800); and the Scientific Research Foundation of the Health Bureau of Jilin Province, China (grant number: 2011Z116).
Author information
Authors and Affiliations
Contributions
Jianxing Yu and Lina Jin made substantial contributions to conception and design of this study. Jianxing Yu and Yuchun Tao drafted the manuscript. Jing Dou and Yaqin Yu revised the manuscript. Junsen Ye and Jianxing Yu made contribution to acquisition and performed the statistical analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yu, J., Tao, Y., Dou, J. et al. The dose-response analysis between BMI and common chronic diseases in northeast China. Sci Rep 8, 4228 (2018). https://doi.org/10.1038/s41598-018-22551-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-22551-y
This article is cited by
-
Muscle distribution in relation to all-cause and cause-specific mortality in young and middle-aged adults
Journal of Translational Medicine (2023)
-
Machine learning model to predict obesity using gut metabolite and brain microstructure data
Scientific Reports (2023)
-
Association of meat consumption with NAFLD risk and liver-related biochemical indexes in older Chinese: a cross-sectional study
BMC Gastroenterology (2021)
-
Lipid changes during the perioperative period in patients with early breast cancer: a real-world retrospective analysis
BMC Surgery (2021)
-
The associations between smoking and obesity in northeast China: a quantile regression analysis
Scientific Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.