Abstract
This study aimed to establish an effective prognostic nomogram for predicting the probability of postoperative bone remodeling of patients with anterior disc displacement without reduction (ADDWoR). The nomogram was based on a retrospective study on patients underwent surgical approaches for ADDWoR at Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University from January, 2007 to January, 2017. A multivariate logistic regression analysis was used to develop variables suitable for probability estimation model. The predictive accuracy and discriminative ability were determined by ROC (AUC-index) and calibration curve. Results were validated using bootstrap resampling with all statistical tests two-sided. 1110 patients were included in the analysis. The probability of postoperative bone remodeling in ADDWoR was 0.51. Six independent prognostic factors including age of onset, nocturnal bruxism, disc morphology, BMD, Wilkes’ classification, and postoperative splint therapy were integrated to construct the nomogram. The probability estimation model showed good discrimination in both internal and external validation with AUC-index of 0.84. The calibration curves for probability of postoperative bone remodeling showed optimal agreement with actual observation. In conclusion, a nomogram was established to provide individual prediction of postoperative bone remodeling for patients with ADDWoR treated by arthroscopy surgery.
Similar content being viewed by others
Introduction
Temporomandibular joint (TMJ) disc displacement is a common disruption condition causing progressive joint dysfunction including arthralgia (pain), functional limitation, osteoarthritis (OA), and condylar resorption1,2. In general population, an estimated of 36% is reported of the internal derangement (ID), which usually occurs in people of all ages and with a prevalence in female aged twenties years old3,4. As early as 1966, Boering et al. found that disc displacement might lead to condylar resorption, thus causing maxillofacial abnormalities like mandibular deviation (MD), and mandibular retrusion (MR)5,6. According to Schwartz et al., disc abnormality interrupted the growth of mandibular ramus thus resulting in maxillofacial abnormalities7. In their research, they included 128 patients with ADDWoR, and discovered that 112 cases reported of various degrees of facial deviation. Correspondingly, among the 60 cases of mandibular retraction, ADDWoR was observed in 56 patients. And therefore, disc displacement without reduction, especially combined with significant clinical symptoms such as pain, dysfunction, and maxillofacial abnormalities or failed to conservative therapies is general indication for invasive intervention treatment8,9.
According to Wolford et al., the replaced disc was conducive to the prevention of further resorption and degeneration of condyle and meanwhile contribute to new bone formation, especially among young patients10. Meanwhile, the post-operative bone regeneration which deemed as an important index of the treatment effect can relieve or reverse maxillofacial abnormalities caused by ADDWoR. For years, correlative factors involving age, gender, genetic background, nutritional status, drugs abuse, repetitive oral habits, and treatment strategy have all been cited as triggers or aggravators for the postoperative evaluation11. However, none of the parameters mentioned above have been specifically developed for the postoperative prognostic prediction. At the moment, nomogram, an intuitive graph of a statistical predictive model, has been proposed as an alternative standard to guide treatment allocation for pathema by formalizing and interpreting potential factors for probability prognoses12. Thus, a prognostic nomogram model was conducted to assess individual prognostic risk factors in estimating the probability of postoperative bone remodeling for patients with ADDWoR based on multivariate analysis.
Results
Clinicopathological characteristics of patients
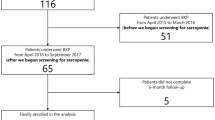
Of the 1110 patients that underwent arthroscopy surgery for ADDWoR between 2007 and 2017, 740 patients were in the primary set and 370 in the validation set. The detailed characteristics of selected patients are listed in Table 1.
The age of onset ranged from 10 to 35 years (mean, 20.63 ± 6.20 years) and the ratio of female/male was 2.00. The progress of the disease lasted for an average of 17.39 ± 16.23 months (3 to 120 month). According to physical examinations, 944 patients and 579 patients have the history of clicking and pain respectively, and nocturnal bruxism were reported in 610 patients. The MIO varied from 0 to 52 mm with a mean of 32.69 ± 0.88 mm. Based upon pre-operation evaluation, the disc perforation and osteopenia rates were 15.23% and 37.66% within the cohorts. In the Wilkes’ classification, 549 cases were in stage III, 403 in stage IV, and 158 in stage V.
Factors Associated with Postoperative bone remodeling in Patients with ADDWoR
Multivariate logistic regression analysis was performed in this study and the outcome indicated that factors including age of onset, nocturnal bruxism, disc morphology, BMD, Wilkes’ classification, and postoperative splint therapy were associated with the bone remodeling after surgery (Table 2).
In the analysis, onset age was the significant predictor and the post-operative bone remodeling concentrated among younger group with the OR of 0.39 (95% CI: 0.25 to 0.59, P < 0.001). According to Wilkes’ classification, patients in earlier stage achieved better outcomes (OR, 2.09; 95% CI, 1.10 to 3.96, P = 0.024). The following variables were considered as negative predictors: disc with perforation (OR, 0.08; 95% CI, 0.03 to 0.23, P < 0.001), lower BMD (OR, 0.53; 95% CI, 0.32 to 0.86, P = 0.011), and patients who have nocturnal bruxism experience (OR, 0.14; 95% CI, 0.10 to 0.21, P < 0.001). Meanwhile, a preferred result was also yield in patients with postoperative splint therapy with a OR of 1.40 (95% CI: 0.92 to 2.14, P = 0.120) (Fig. 1).
Prognostic Nomogram
A nomogram that incorporated the significant prognostic factors was established in Fig. 2. In the nomogram, points were assigned to all variable factors, and a sum of points within the factors were depicted on the total point scale. A straight line could then go down to determine the estimated probability of post-operative bone remodeling (linear predictor, probability) at each time point. In this study, the higher score of total points represented for a more probability of bone regeneration11. The result of the nomogram illustrated that the age of onset shared the largest contribution to postoperative condyle modification, followed by the nocturnal bruxism experience. The factors of Wilkes’ classification, disc morphology, condyle situation and the post-operative splint therapy showed a moderate to low impact on the result. In the primary setting, the ROC curve of discrimination for the established nomogram was good, with the AUC of 0.84 (95% CI, 0.80 to 0.89) after bias correction with 2,000 cycles of bootstrap resampling. The calibration plots also presented with a good agreement on the nomogram prediction and actual observation in the probability of post-operative bone remodeling (Appendix Fig. 1).
Prognostic nomogram for postoperative bone remodeling in patients with ADDWoR. (The individual patient’s value is located on each variable axis, and a line is drawn upward to determine the number of points received for each variable value. The sum of these numbers is located on the Total Points axis, and a line is drawn downward to the probability axes to determine the post-operative bone remodeling). Abbreviations: BMD, bone mineral density.
Methods
Patients and Study Design
A retrospective cohort study consisting of 1110 patients with ADDWoR treated by arthroscopy surgery at the Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University (Shanghai, China) was conducted from January, 2007 to January, 2017.
The inclusion criteria were as follows: (1) diagnosed of disc displacement without reduction; (2) treated by arthroscopy therapy; (3) with complete preoperative and postoperative MRI assessment. Exclusion criteria included patients with uncertain diagnose, with poor quality of MRI imaging, without complete data sheet or loss to follow-up.
The study was approved by the Ethics Committee of Shanghai Jiao Tong University School of Medicine and all participants (primary and validation cohort) provided informed participation consent in accordance with the relevant regulations and guidelines.
Diagnosis and Treatment
A routine investigation including personal information (age, gender) and detailed history (course of disease, nocturnal bruxism) were taken from all patients. Then examinations involving clicking, pain-related disorders, maximum interincisal opening (MIO), and bone mineral density (BMD) were taken into consideration13. In our study, the condyle condition (BMD) was composed of two indexes. According to the International Society of Clinical Densitometry (ISCD), the value of the lumbar spine (anterior-posterior at L2–L4) and proximal femur (femoral neck, trochanter, and Ward’s triangle) was measured using dual-energy X-ray absorptiometry (DEXA, DMS Lessos, France) in which a Z-score ≤ −2 was termed as low14,15. Besides, a condyle osteopenia was also measured using MRI examination in which a hypointense signal instead of a normal hyperintense signal was detected on T1 images of bone marrow area. The ‘osteopenia’ changes were required to present on at least two consecutive slices14,16.
The preoperative diagnosis of stage of ID was evaluated in relation to the Wilkes-Bronstein classification based upon clinical and MRI examination17. According to the classification, ADDWoR was reported in Stage III (serious jaw functional obstacles, chronic pain, and mild to moderate disc deformity, Stage IV (serious jaw functional obstacles, chronic pain, co-occurring with severe disc posterior band hypertrophy, and abnormal bone structure), and Stage V (serious jaw functional obstacles, chronic pain, obvious disc deformity, disc perforation, and degenerative bone changes)8.
Meanwhile, arthroscopy surgery was carried out for patient who was diagnosed of ADDWoR, complained of pain and/or dysfunction and failed to conservative therapies8,18. All treatments were performed according to the guidelines for TMD treatment and carried out by the same surgeon (with more than 40 years of experience in TMJ treatment)19. The surgical procedure was commonly involved three main parts including anterior release, disc reduction, and disc suture10. For all patients included, the technique began by local anesthesia (2% lidocaine 2 to 3 ml) injected into the superior joint space to avoid pain and to decrease bleeding. Firstly, a puncture aimed at a systematic diagnostic arthroscopy was injected on the top of the fossa. For anterior release, the second puncture located at the anterior surface of the eminence. Under this puncture, a coblation probe was inserted in and an incision from medial to lateral was carried out 2–3 mm anterior to the anterior band of the disc. To avoid the injury of both blood vessels and nerves, the depth of the anterior release was recommended to limited under 2 mm. After that, an obturator was applied for disc reduction. For disc suture, body projection was commonly 10 mm ahead of the first puncture. Under the direct visualization of arthroscopy, a 12-gauge suturing needle was injected into the border of the bilaminar zone and the posterior band. The needle was pushed in and out of the retrodiscal tissue directed from medial to laterial. Meanwhile, another puncture was performed through the point at the anterior wall of the external auditorycanal. Through these two punctures, customized suture grippers was inserted to hold surgical sutures. Finally, sutures were tied with the knots underneath the cartilage of the external auditory canal and the skin incision was closed. Then a 6 to 12 month post-operation functional splint treatment was conducted if an open bite over 2 mm was detected in patients. All patients were scheduled a complete physical examination at each of the follow-up visits (1, 3, 6, 12, 18, 24 month). A MRI was also performed once every 6 months in the following 2 years20.
Bone modification was evaluated upon pre- and post-operative MRI, in which either a smooth and continuous cortical bone in the condylar sagittal appearance and/or new bone tissue characterized by a mass hyperintense signal intensity on laterial of condyle (T1-and T2-weighted spin echo) was observed when compared with the baseline (Fig. 3A,B)16. In the study, all scans were executed at the Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University (Shanghai, China) by the same technician. Two independent readers reviewed each MRI of patient blindly in parallel. Any discrepancy was resolved through a discussion with a third investigator (C.Y, with more than 30 years of experience in oral surgery). In some cases, a 3D volume-rendering image based on CT scan was used to calculated the changes of condyle remodeling after the disc reposition treatment. In this study, a method of image fusion was carried out by using a multipoint registration21. According to landmark points (the genial tubercle, the mental foramen, the inferior loop of alveolar nerve, and the sigmoid notch), post-operative images in 12 months were moved to coordinate to the pretreatment 3D model voxel-by-voxel22,23 (Fig. 3C).
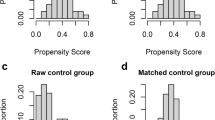
Statistical Analysis
Categorical variables grouped upon clinical and radiological findings are set in proportions. The result was evaluated by the X2 test or the Fisher’s exact test. Continuous variables were also compared under the t test for variables distribution. Logistic regression analysis was carried out for the multivariate analysis. Variables were formulated on a backward step-down model reduction, with the elimination criterion of P > 0.0524. The nomogram was then programmed based on the result of multivariate analysis. Performance was measured by operating characteristics curve (ROC) associated with AUC (area under the ROC curve) for discrimination25. Calibration was performed by comparing the predicted bone remodeling with the observed subject after bias correction in accordance with the calibration curve. According to the established nomogram, bootstraps with 2,000 resample were used in internal and external validation for average bias. The statistical analyses were conducted using R software with rms-package (http://www.r-project.org).
Discussion
Disc displacement in TMJ is a common disruption condition causing progressive joint dysfunction. Longitudinal clinical observations of orthodontics, orthognathics, and articulationes mandibularis suggested that disc displacement, in general, is associated with mandibular asymmetry1,2. In Hall et al. study, it has been deduced that disc displacement may give rise to condylar degeneration thus causing the bone resorption and the decrease of condylar height among patients5. For patients with unilateral ADDWoR, the growth of affected condyle was restricted, while the other side developing properly, and which may finally give rise to mandibular deviation. In the patients involving bilateral sides, accordingly, the development of mandible was obviously restrained. Instead of the normally forward and counterclockwise growth, a backward and clockwise trend was detected, thus causing mandibular retrusion. In addition, Cai et al. discovered that compared with short-term disc displacement, the length of disc was shorter with the distance of displacement getting farther and the height of condyle decreased in long-term cases26. As for patients of disc replacement, the operation of disc reposition remains estimated. According to Yang et al., it is unnecessary to have disc reposition in stable cases with no clinical symptoms, which includes patient of relatively completed growth, the integrity condylar cortical on MRI, no articular degeneration of joint, disc-like-change in bilaminar zone, and no clinical and imaging alternation of joint and maxillofacial during the interval of more than 6 months19. In Wilkes’ stage evaluation, similarly, invasive intervention treatment was recommended especially in those who have significant clinical symptoms such as pain, dysfunction, induced mandibular deviation, mandibular retrusion or failed to conservative therapies8.
During longitudinal follow-up, studies found that disc reposition can prevent the further resorption and degeneration of the condyle and produce adaptive amelioration as new bone formation. Especially in young patients with positive bone marrow quality, it is common to observe condylar regeneration27. This postoperative reconstruction could bring the increase of the height of the affected condyle for patients with unilateral ADDWoR, and therefore improve the facial and occlusal deviation. In the patients with bilateral defect, mandibular retraction (type II) will be corrected (type I) or improved with the advancement of mandibular.
As for the postoperative evaluation, potential factors involving age, gender, genetic background, nutritional status, repetitive oral habits, and treatment strategy have all been cited as trigger or aggravator11. However, none of the parameters have been specifically developed for the postoperative prognostic prediction. Our study was therefore to evaluate the condylar reconstruction after disc reposition treatment and its related factors.
A prognostic nomogram model for patients with ADDWoR treated by surgical approaches was constructed using post-operation bone remodeling as established curative modality. The AUC value of 0.84 calculated for the nomogram model indicated a high prognostic prediction accuracy.
In this cohort study, a multivariate logistic regression analysis was performed among potential factors including age of onset, course of disease, BMI, nocturnal bruxism, pain, disc morphology and BMD, and post-operative splint therapy. Our study detected a predominace in the parameter of age among other factors. Lower post-operative bone regeneration rate was found in aging population, with less than 50 points for age over 25 years old. Evidence suggested that the decrease in intrinsic properties of mesenchymal stem cells (MSCs) which compromise to bone remodeling, especially to bone loss are age-related28. According to Goncalves et al., a continuous and compact cortical bony layer was established at the age of twenties, which indicated a full development of the mandibular condyle29. In relevant, a complete cortical bony formation was also seen at the average age of 22 years for male and 21 for female. Meanwhile, osteogenic/adipogenic differentiation, and osteoclastogenesis activity also changed greatly during the aging process. Accordingly, the age-dependent growth of homocysteine in blood levels may lead to the potential decline in BMD among elder patients. Associated with BMD degeneration, the negative correlation also affects the viscosity bone pathology, which is responsible for impaired bone regeneration30. And therefore, superior bone remodeling was detected in younger group underwent earily treatment. In this study, condyle condition (BMD) was ranked as a factor in post-operative bone remodeling.
According to Liu et al., articular disc perforation occurred more frequently in anterior disc displacement without reduction, especially in the bilaminal zone. In our study, among 1110 joints, nearly 15.23% reported of disc perforation. Moreover, TMJ disc perforation has also been confederated in patients with heterotopic ossifications (HO), and rheumatic/inflammatory disease. Based on histological analysis, pathological features such as the earily formation of chondrocyte clusters, the thickening of cartilages, and the multifocal loss of cells were detected in condyle surface, which may then blemish on the subchondral bone, causing a diffuse loss of cells and proteoglycan content31. Besides, inflammatory mediators may come to assemble in perforation site causing synovial inflammation and resulting in pain and new bone erosion. Our study demonstrated that a high-quality disc trended to result in large improvements in the postoperative bone remodeling, with a mean improvement of 76 points at the two-year follow-ups. Thus, it was encouraged a well maintenance of disc condition in early time.
Furthermore, mechanical forces such as chewing and bruxism are other major factors in postoperative bone absorption. Li et al. analyzed the effect of pressure change on condyle and chondrocytes based on the model of rabbits32. The results showed that under the pressure of more than 200KPa, the proliferative ability of condylar chondrocytes decreases, with the necrosis and apoptosis increase significantly, which indicate that increasing pressure disturbs the proliferation of chondrocytes in condylar cartilage, and lead to the cartilage degeneration33. Occlusion splints, however, are effective in releasing TMJ involuntary overloading and to reduce the muscle hyperactivity. Moreover, a subsequent occlusion reconstruction achieved by postoperative splints can help to maintain an optimal environment within the TMJ, thus leading to bone osteogenesis and reducing relapse rate34. In our study, almost 610 patients have the habit of nocturnal bruxism and 345 patients took functional splint treatment after arthroscope surgery with 48.51% detected of bone remodeling. In recent research, functional splints have also been recommended with additional effect on the improvement of psychological aspects in TMDs35. Meanwhile, other factors involving long-term progress with pain and clicking are negative predictors in postoperative bone modification.
This is the first nomogram for predicting post-operative bone remodeling of patients with ADDWoR. The analysis was based on a large database with long-term follow-up. Multivariate analyses including age of onset, nocturnal bruxism, the Wilkes’ stage classification, disc morphology, BMD, and post-operative splint therapy were all taken into consideration. In order to enhance the accuracy and reliability of the findings, data extraction, and statistical analysis were all performed by two investigators independently. ROC curve (AUC-index) and calibration curve were calculated in evaluating predictive accuracy and discriminative ability.
Still, limitations in current nomogram must be considered. The study was established based on data obtained from a single institution and some potential prognostic parameters such as geographic and ethnic difference were failed to be incorporated. Therefore, further efforts on prospective data collection of multicenter are encouraged to improve this model. Besides the assessment of post-operative bone remodeling was primarily based on the MRI imaging. Although the diagnostic accuracy of MRI in detecting the TMJ is reported over 86%, there still existed a limitation to a certain extent. Thus, an enhanced CT evaluation was recommended in later research.
In conclusion, a novel nomogram for predicting post-operative bone remodeling of patient with ADDWoR was validated, which provided an objective and accurate individualized post-operative prediction for both physicians and patients.
References
Chen, M. J. et al. Synovial chondromatosis of the tempromandibular joint: relationship between MRI information and potential aggressive behavior. J Craniomaxillofac Surg 43, 349–354, https://doi.org/10.1016/j.jcms.2015.01.011 (2015).
Rammelsberg, P. et al. Variability of disk position in asymptomatic volunteers and patients with internal derangements of the TMJ. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 83, 393–399 (1997).
Miernik, M. & Wieckiewicz, W. The Basic Conservative Treatment of Temporomandibular Joint Anterior Disc Displacement Without Reduction–Review. Adv Clin Exp Med 24, 731–735, https://doi.org/10.17219/acem/35165 (2015).
Valladares-Neto, J. et al. TMJ response to mandibular advancement surgery: an overview of risk factors. J Appl Oral Sci 22, 2–14, https://doi.org/10.1590/1678-775720130056 (2014).
Hall, H. D. Intra-articular disc displacement Part II: Its significant role in temporomandibular joint pathology. J Oral Maxillofac Surg 53, 1073–1079 (1995).
Boering, G. Temporomandibular joint arthrosis and facial deformity. Trans Int Conf Oral Surg, 258–260 (1967).
Schwartz, R. D. Comments on pediatric internal derangements. Am J Orthod Dentofacial Orthop 105, 30A, 32A, 34A; author reply 39A (1994).
Wilkes, C. H. Internal derangements of the temporomandibular joint. Pathological variations. Northwest Dent 69, 25–32 (1990).
Ungor, C., Atasoy, K. T., Taskesen, F., Pirpir, C. & Yilmaz, O. Long-Term Outcome of Arthrocentesis Plus Hyaluronic Acid Injection in Patients With Wilkes Stage II and III Temporomandibular Joint Internal Derangement. J Craniofac Surg 26, 2104–2108, https://doi.org/10.1097/SCS.0000000000002078 (2015).
Wolford, L. M. & Cardenas, L. Idiopathic condylar resorption: diagnosis, treatment protocol, and outcomes. Am J Orthod Dentofacial Orthop 116, 667–677 (1999).
Liang, W. et al. Development and validation of a nomogram for predicting the survival of patients with non-metastatic nasopharyngeal carcinoma after curative treatment. Chin J Cancer 35, 98, https://doi.org/10.1186/s40880-016-0160-9 (2016).
Tang, L. Q. et al. Establishment and Validation of Prognostic Nomograms for Endemic Nasopharyngeal Carcinoma. J Natl Cancer Inst 108, https://doi.org/10.1093/jnci/djv291 (2016).
Larheim, T. A. Role of magnetic resonance imaging in the clinical diagnosis of the temporomandibular joint. Cells Tissues Organs 180, 6–21, https://doi.org/10.1159/000086194 (2005).
Wang, D. et al. Bone edema on magnetic resonance imaging is highly associated with low bone mineral density in patients with ankylosing spondylitis. PLoS One 12, e0189569, https://doi.org/10.1371/journal.pone.0189569 (2017).
Baim, S. et al. Official Positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD Pediatric Position Development Conference. J Clin Densitom 11, 6–21, https://doi.org/10.1016/j.jocd.2007.12.002 (2008).
Kellenberger, C. J., Junhasavasdikul, T., Tolend, M. & Doria, A. S. Temporomandibular joint atlas for detection and grading of juvenile idiopathic arthritis involvement by magnetic resonance imaging. Pediatr Radiol, https://doi.org/10.1007/s00247-017-4000-0 (2017).
Taskaya-Yylmaz, N. & Ogutcen-Toller, M. Clinical correlation of MRI findings of internal derangements of the temporomandibular joints. Br J Oral Maxillofac Surg 40, 317–321 (2002).
Zhu, Y., Zheng, C., Deng, Y. & Wang, Y. Arthroscopic surgery for treatment of anterior displacement of the disc without reduction of the temporomandibular joint. Br J Oral Maxillofac Surg 50, 144–148, https://doi.org/10.1016/j.bjoms.2011.02.004 (2012).
Yang, C., Cai, X. Y., Chen, M. J. & Zhang, S. Y. New arthroscopic disc repositioning and suturing technique for treating an anteriorly displaced disc of the temporomandibular joint: part I–technique introduction. Int J Oral Maxillofac Surg 41, 1058–1063, https://doi.org/10.1016/j.ijom.2012.05.025 (2012).
Zhang, S. Y. et al. New arthroscopic disc repositioning and suturing technique for treating internal derangement of the temporomandibular joint: part II–magnetic resonance imaging evaluation. J Oral Maxillofac Surg 68, 1813–1817, https://doi.org/10.1016/j.joms.2009.08.012 (2010).
Wong, R. W., Chau, A. C. & Hagg, U. 3D CBCT McNamara’s cephalometric analysis in an adult southern Chinese population. Int J Oral Maxillofac Surg 40, 920–925, https://doi.org/10.1016/j.ijom.2011.03.011 (2011).
Prados-Frutos, J. C., Salinas-Goodier, C., Manchon, A. & Rojo, R. Anterior loop of the mental nerve, mental foramen and incisive nerve emergency: tridimensional assessment and surgical applications. Surg Radiol Anat 39, 169–175, https://doi.org/10.1007/s00276-016-1690-1 (2017).
Haeni, D. L. et al. Three-dimensional volume measurement of coracoid graft osteolysis after arthroscopic Latarjet procedure. J Shoulder Elbow Surg 26, 484–489, https://doi.org/10.1016/j.jse.2016.08.007 (2017).
Gotto, G. T., Yu, C., Bernstein, M., Eastham, J. A. & Kattan, M. W. Development of a nomogram model predicting current bone scan positivity in patients treated with androgen-deprivation therapy for prostate cancer. Front Oncol 4, 296, https://doi.org/10.3389/fonc.2014.00296 (2014).
Wang, Y. et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J Clin Oncol 31, 1188–1195, https://doi.org/10.1200/JCO.2012.41.5984 (2013).
Cai, X. Y., Jin, J. M. & Yang, C. Changes in disc position, disc length, and condylar height in the temporomandibular joint with anterior disc displacement: a longitudinal retrospective magnetic resonance imaging study. J Oral Maxillofac Surg 69, e340–346, https://doi.org/10.1016/j.joms.2011.02.038 (2011).
Xie, Q. et al. Will unilateral temporomandibular joint anterior disc displacement in teenagers lead to asymmetry of condyle and mandible? A longitudinal study. J Craniomaxillofac Surg 44, 590–596, https://doi.org/10.1016/j.jcms.2016.01.019 (2016).
Zhou, P. et al. SATB2-Nanog axis links age-related intrinsic changes of mesenchymal stem cells from craniofacial bone. Aging (Albany NY) 8, 2006–2011, https://doi.org/10.18632/aging.101041 (2016).
Goncalves, J. R. et al. Temporomandibular joint condylar changes following maxillomandibular advancement and articular disc repositioning. J Oral Maxillofac Surg 71(1759), e1751–1715, https://doi.org/10.1016/j.joms.2013.06.209 (2013).
Kim, J. I., Moon, J. H., Chung, H. W., Kong, M. H. & Kim, H. J. Association between Homocysteine and Bone Mineral Density according to Age and Sex in Healthy Adults. J Bone Metab 23, 129–134, https://doi.org/10.11005/jbm.2016.23.3.129 (2016).
Embree, M. C. et al. Soft tissue ossification and condylar cartilage degeneration following TMJ disc perforation in a rabbit pilot study. Osteoarthritis Cartilage 23, 629–639, https://doi.org/10.1016/j.joca.2014.12.015 (2015).
Li, H. et al. Disc positions and condylar changes induced by different stretching forces in the model for anterior disc displacement of temporomandibular joint. J Craniofac Surg 25, 2112–2116, https://doi.org/10.1097/SCS.0000000000001065 (2014).
Li, H. et al. Study on the effects of gradient mechanical pressures on the proliferation, apoptosis, chondrogenesis and hypertrophy of mandibular condylar chondrocytes in vitro. Arch Oral Biol 73, 186–192, https://doi.org/10.1016/j.archoralbio.2016.10.017 (2017).
Mitsui, S. N., Yasue, A., Kuroda, S. & Tanaka, E. Long-term stability of conservative orthodontic treatment in a patient with temporomandibular joint disorder. J Orthod Sci 5, 104–108, https://doi.org/10.4103/2278-0203.186168 (2016).
Costa, Y. M., Porporatti, A. L., Stuginski-Barbosa, J., Bonjardim, L. R. & Conti, P. C. Additional effect of occlusal splints on the improvement of psychological aspects in temporomandibular disorder subjects: A randomized controlled trial. Arch Oral Biol 60, 738–744, https://doi.org/10.1016/j.archoralbio.2015.02.005 (2015).
Acknowledgements
This work was supported by the Youth Program of National Natural Science Foundation of China (81601915); Science and Technology Commission of Shanghai Funding/support: Municipality Science Research Project (14DZ2294300), and Shanghai Summit & Plateau Disciplines.
Author information
Authors and Affiliations
Contributions
C.Y., J.W.Z. and S.Y.Z. designed the experiments; X.H.L. and S.P. collected the date; X.H.L., S.Y.Z. and X.Y.W. did the calculation. X.H.L. wrote the main manuscript text and all authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, X., Shen, P., Wang, X. et al. A Prognostic Nomogram for Postoperative Bone Remodeling in Patients with ADDWoR. Sci Rep 8, 4361 (2018). https://doi.org/10.1038/s41598-018-22471-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-22471-x
This article is cited by
-
Temporomandibular joint disc repositioning and occlusal splint for adolescents with skeletal class II malocclusion: a single-center, randomized, open-label trial
BMC Oral Health (2023)
-
Prognostic indicators of arthroscopic discopexy for management of temporomandibular joint closed lock
Scientific Reports (2022)
-
The magnetic resonance imaging evaluation of condylar new bone remodeling after Yang’s TMJ arthroscopic surgery
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.