Abstract
Juvenile onset open-angle glaucoma (JOAG) affects patients before 40 years of age, causing high intraocular pressure and severe optic nerve damage. To expand the mutation spectrum of the causative genes in JOAG, with a view to identify novel disease-causing mutations, we investigated MYOC, OPTN, NTF4, WDR36 and CYP1B1 in a cohort of 67 unrelated Chinese JOAG patients. Whole exome sequencing was used to identify possible pathogenic mutations, which were further excluded in normal controls. After sequencing and the use of a database pipeline, as well as predictive assessment filtering, we identified a total of six mutations in three genes, MYOC, OPTN and CYP1B1. Among them, 2 heterozygous mutations in MYOC (c. 1109C > T, p. (P370L); c. 1150G > C, p. (D384H)), 2 heterozygous mutations in OPTN (c. 985A > G, p.(R329G); c. 1481T > G, p. (L494W)) and 2 homozygous mutations in CYP1B1 (c. 1412T > G, p.(I471S); c. 1169G > A, p.(R390H)) were identified as potentially causative mutations. No mutation was detected in NTF4 or WDR36. Our results enrich the mutation spectra and frequencies of MYOC, OPTN and CYP1B1 in JOAG among the Chinese population. Further studies are needed to address the pathogenicity of each of the mutations detected in this study.
Similar content being viewed by others
Introduction
Glaucoma, the second leading cause of irreversible blindness worldwide1, is a group of heterogeneous optic neuropathies characterized by retinal nerve fibre layer damage and visual field defects. The disease is progressive and leads to permanent visual impairment and even blindness in some patients2. Age and high intraocular pressure (IOP) are the main risk factors. Primary open-angle glaucoma (POAG) is a common form of glaucoma, which can be further subdivided into juvenile-onset open-angle glaucoma (JOAG) and adult-onset POAG according to the age of onset3. JOAG patients often have higher intraocular pressure (IOP) and suffer from more severe optic nerve damage than adult-onset POAG patients4.
Genetic factors play an important role in the development of glaucoma5. Several genes have been identified to be associated with POAG, primary congenital glaucoma (PCG) and JOAG, including myocilin (MYOC)6; optineurin (OPTN)7; WD repeat domain 36 (WDR36)8; neurotrophin 4 (NTF4)9; and cytochrome P450 family 1, subfamily B(CYP1B1)10. The same candidate gene may lead to different phenotypes of glaucoma11. MYOC is the first candidate gene mapped for POAG and has been confirmed to be associated with both POAG and JOAG12. Mutations of OPTN were found in POAG and amyotrophic lateral sclerosis (ALS)13,14. CYP1B1 is a PCG gene but has also been reported in association with JOAG15,16. To date, the mutations of known genes only account for approximately 5% of patients with POAG17. Compared with adult-onset POAG, JOAG may be more likely to be genetically determined and less likely the consequence of environment16. Investigation of the POAG genes in JOAG might provide a good opportunity for understanding the genetic components and heterogeneity of JOAG.
Whole-exome sequencing (WES) is available in commercial service and has been proved to be useful in mapping disease genes. It is rapid and comparatively more cost-effective than other genomic technologies, especially for complex diseases18. In developmental and congenital glaucoma, WES has led to the identification of novel variants in LTBP2 and PXDN19. It has also been used to identify mutations in known genes in primary glaucoma effectively and quickly20. In the current study, we performed WES on 67 Chinese JOAG patients to detect the full spectra of variants in MYOC, OPTN, NTF4, WDR36 and CYP1B1, with a view to identify novel disease-causing mutations for JOAG.
Results
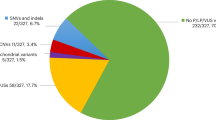
From the whole exome results of 67 Chinese JOAG patients, totally 79 variants in MYOC, 354 variants in OPTN, 139 variants in WDR36, 45 variants in NTF4 and 199 variants in CYP1B1 were detected. Among them, a total of 6 variants in MYOC, OPTN and CYP1B1 were identified as potential disease-causing mutations in 8 patients (11.94%) after a series of filtering steps (Tables 1 and 2). These variants included 2 variants in MYOC, 2 variants in OPTN and 2 variants in CYP1B1 (Fig. 1). The variants were confirmed by Sanger sequencing. No MYOC or OPTN potential disease causing mutations were detected in 125 controls, while two heterozygous mutations of CYP1B1 (c. 1169G > A p. (R390H)) were found in controls (Table 1).
In MYOC, there were two heterozygous mutations (c. 1109C > T, p. (P370L); c. 1150G > C, p. (D384H)) detected from two cases in this study, among which p.D384H was novel (Fig. 2A). Substitution of p.D384H was predicted to affect protein function by Polyphen-2, SIFT and Mutation Taster. Additionally, the mutated amino acid is highly conserved among all the tested species (Fig. 3A). p. (P370L) was a reported mutation associated with POAG.
In OPTN, 2 heterozygous mutations (c. 985A > G, p. (R329G); c.1481T > G, p. (L494W)) were detected in two unrelated individual. Among them, p. (R329G) was novel and p. (L494W) was reported in amyotrophic lateral sclerosis (ALS) (Fig. 2B,C). p. (R329G) was predicted to be disease causing by Mutation taster and probably damaging by Polyphen-2. Furthermore, the p. (R329G) mutation occurred at a remarkably conserved region in all the tested species apart from danio (Fig. 3B).
In CYP1B1, 2 homozygous mutations (c.1412T > G, p. (I471S); c.1169G > A, p. (R390H)) were detected in two patients. Both mutations were predicted to be a pathogenic mutation in all three pathogenicity prediction tools used in this study. The I471S mutation was reported in a Chinese primary congenital glaucoma (PCG) study21.
Discussion
In this study, the results of exome sequencing data from 67 JOAG patients identified 6 mutations in the MYOC, OPTN and CYP1B1 genes in 8 unrelated patients. Among them, D384H in MYOC and R329G and L494W in OPTN were novel. These mutations are predicted to affect protein function and were absent in 125 control individuals without glaucoma.
MYOC is the first identified glaucoma-causing gene22. Over 20 mutations in MYOC have been reported, and the frequency of mutation ranged from 10% to 30%6,23,24 in study cohorts with the familial trait. In the present study, 5.97% (4/67) of JOAG patients carry a heterozygous mutation in MYOC. Three patients have mutant p. (P370L) in the third exon in MYOC. It has been reported that the turnover rate of mutant p. (P370L) in MYOC fusion proteins was much prolonged compared with wild type25. The ubiquitin-proteasome function is compromised and autophagy is induced with mutant p. (P370L) in MYOC25. Further study showed a causal association between this p. (P370L) mutation of MYOC and juvenile glaucoma with goniodysgenesis26. Of the two mutations detected in the present study, p. (P370L) has been previously reported26,27. p. (D384H) is a novel mutation in the third exon of MYOC, near the position of p. (P370L). Further studies are needed to investigate the biological functions of these two mutations.
The reported role of OPTN in JOAG remains inconsistent. Previous studies have identified several mutations in OPTN associated with POAG7, including c.C160G28 and p.(Lys322Glu)29. On the other hand, several studies have shown an absence of OPTN mutations in POAG or JOAG30,31,32. L494W has been reported in a Chinese amyotrophic lateral sclerosis study but not in any glaucoma study33. The patient who carries p. (L494W) is 33 years old. After a detailed systemic review, we confirmed that she has no manifestation f ALS. The mean age at onset of ALS range from 52.9 to 59.9 years in several reports33,34. Therefore, it is necessary to follow that patient at regular intervals. p. (R329G) is a novel mutation in OPTN in our study. Further studies are needed to understand the role of mutations in OPTN in JOAG.
CYP1B1 is associated with PCG, characterized by an autosomal recessive model. CYP1B1 is also involved in the development of JOAG. CYP1B1 (G61E, R368H, R390H, E229K, and 4340delG) may be associated with severe or moderate angle abnormalities and plays an important role in PCG35. Suri, F., R, et al. first reported that mutations in CYP1B1 were implicated in POAG among Iranians, notably in the juvenile-onset form36. Suri, F., R, et al. further reported that PCG nonpenetrant individuals harbouring CYP1B1 mutations may develop JOAG or POAG to varying degrees37. The c.1169 G > A, p. (Arg390His) mutation of CYP1B1 may be a risk factor for the development of JOAG38. In the current study, a homozygous mutation of R390H in the third exon of CYP1B1 was found in this Chinese JOAG group, consistent with previous reports38. A homozygous mutation of I471S in the third exon of CYP1B1 was identified. The locations of Arg390 and I470 at CYP1B1 are in the K helix and L helix, respectively. Both helixes are conserved regions for CYP1B1 and are expected to be involved in proper folding of the molecule. p. (I471S) was first reported to be associated with PCG in a Chinese PCG study21, indicating that same genotype may have a different degree of phenotypic expression in Chinese PCG and JOAG. López-Garrido et al. have found that the onset of glaucoma in mutant CYP1B1 genotypes may vary even when CYP1B1 activity is completely absent. Residual CYP1B1 activity levels can influence the phenotypic outcome of both homozygous and compound heterozygous carriers, leading to either congenital or non-dominant juvenile glaucoma39. These findings help explain why the two homozygous mutations of CYP1B1 found in our study led to the development of JOAG but not PCG. Further studies are needed to elucidate the role of mutations in CYP1B1 in the development of JOAG in Chinese patients.
No mutations were detected in NTF4 orWDR36. The role of NTF4 in POAG remains controversial. NTF4 is not found to be candidate gene for glaucoma in several studies40,41. However, the results of Chen et al., Pasutto et al. and Vithana et al. supported its implication in POAG42,43,44. The mutation frequency of NTF4 is known to be low in the Chinese population42,44. Thus, it is not surprising that no mutation was detected in our small cohort. Mutations of WDR36 have been detected in different JOAG populations, including German and Chinese45,46. The frequency of mutation of WDR36 is unclear in the Chinese population, and further studies are needed to estimate the WDR36 mutation frequency in this population.
This study is limited by the lack of parents’ samples so that we are not able to perform segregation analysis. The mutations carriers’ parents were reported to be free of glaucoma. Therefore, whether the mutations detected are de novo mutations cannot be confirmed as for now. Also, there could be other factors that might have affected the penetrance of the mutations so that the patients, even carried the mutations, might not have developed the disease. JOAG may belongs to heterogeneity with different variants in numerous genes, which makes it some familial but most occurring sporadically.
In summary, six variants of MYOC, OPTN and CYP1B1 were found in 11.94% of this Chinese JOAG cohort, including two heterozygous mutations in MYOC in four patients, two heterozygous mutations in OPTN in two patients, and two homozygous mutations in CYP1B1 in two patients. No mutation of NTF4 or WDR36 was detected in this cohort. Although the sample size of this study is small and we have not conducted segregation analysis or functional analyses of the novel mutations, our results provide additional evidence of the mutation spectra and frequencies in Chinese JOAG.
Materials and Methods
Patient recruitment
We recruited unrelated Chinese JOAG patients at the Shantou University/Chinese University of Hong Kong Joint Shantou International Eye Center, Shantou, Guangdong Province, China. Written informed consent was obtained from the participants or their guardians. The study was conducted following the tenets of the Declaration of Helsinki and was approved by the institutional review board and ethics committee of Joint Shantou International Eye Center.
The inclusion criteria for patients with JOAG are based on an age of onset between 3 years of age and early adulthood and the manifestation of highly elevated intraocular pressures without angle abnormalities3. Briefly, the recruited patients have an onset of open-angle glaucoma between 3 to 40 years old, an intraocular pressure elevated greater than 22 mmHg, characteristic optic disc damage and/or visual field damage, and open angles under gonioscopy. Patients recruited in this study are sporadic JOAG. Blood samples from patients’ parents or siblings were not available. The control subjects were recruited from patients with mild cataracts and age 60 years or above who attended an ophthalmic check-up. The control subjects did not have ophthalmic or systemic diseases.
Mutational screening
Total genomic DNA was extracted from peripheral blood using a DNA Extraction Kit (QIAGEN, QIAamp® DNA Blood Mini Kit) according to the manufacturer’s instructions. DNA was quantified with Nanodrop 1000 (ND-1000 3.1.0, NanoDrop Spectrophotometer).
WES was performed with an Agilent Sure Select All Human Exon v5.0 kit (Santa Clara, US.). DNA fragments were sequenced using an Illumina HisSeq. 4000 system (Illumina, San Diego, CA). The average sequencing depth was 100-fold. The results were mapped against UCSC hg19 by Burrows-Wheeler Aligner.
Exome sequencing results were filtered with the following steps: (1) Noncoding variants without altering splicing sites predicted by the Berkeley Drosophila Genome Project (available in the public domain at http://www.fruitfly.org/seq_tools/splice.html) were excluded; (2) The synonymous variants without altering splicing sites were removed; (3) SNPs with minor allele frequency (MAF) greater than or equal to 1% in the 1000Genome database were excluded; (4) Missense variants predicted to be benign on protein function consistently by Polyphen-2 (http://genetics.bwh.harvard.edu/pph/), SIFT (availablehttp://sift.jcvi.org)and Mutation Taster (http://www.mutationtaster.org/) were removed. Detected variants affecting coding residues in MYOC, OPTN, NTF4, WDR36 and CYP1B1 were selected for further validation and analysis.
Sanger sequencing was used to confirm the candidate variants after filtering. Primers were designed using the Primer3 online tool (Table 3). The methods used to perform Sanger sequencing, including amplification, sequencing, and analysis of the target fragments, have been previously described47. Sequence alignment and analysis of variations were performed by using the NovoSNP program48.
Bioinformatics analysis
Clustal Omega (http://www.ebi.ac.uk/Tools/msa/clustalo/) was used to acquire multiple-sequence alignment of MYOC and OPTN in different species, including Homo sapiens, Pan troglodytes, Macaca mulatta, Bos taurus, Felis catus, Mus musculus, Gallus gallus and Danio rerio. Crystal structures of mutant and wild-type proteins were evaluated by Phyre248 (http://www.sbg.bio.ic.ac.uk/phyre2/html/page.cgi? id = index)49 and further visualized using Pymol Molecular Graphics System (Pymol).
References
Quigley, H. A. Glaucoma. Lancet 377, 1367–1377, https://doi.org/10.1016/S0140-6736(10)61423-7 (2011).
Turalba, A. V. & Chen, T. C. Clinical and genetic characteristics of primary juvenile-onset open-angle glaucoma (JOAG). Seminars in ophthalmology 23, 19–25, https://doi.org/10.1080/08820530701745199 (2008).
Goldwyn, R., Waltman, S. R. & Becker, B. Primary open-angle glaucoma in adolescents and young adults. Arch Ophthalmol 84, 579–582 (1970).
Foster, P. J., Buhrmann, R., Quigley, H. A. & Johnson, G. J. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol 86, 238–242 (2002).
Abu-Amero, K., Kondkar, A. A. & Chalam, K. V. An Updated Review on the Genetics of Primary Open Angle Glaucoma. Int J Mol Sci 16, 28886–28911, https://doi.org/10.3390/ijms161226135 (2015).
Stoilova, D. et al. Novel TIGR/MYOC mutations in families with juvenile onset primary open angle glaucoma. J Med Genet 35, 989–992 (1998).
Forsman, E. et al. The role of TIGR and OPTN in Finnish glaucoma families: a clinical and molecular genetic study. Mol Vis 9, 217–222 (2003).
Hauser, M. A. et al. Distribution of WDR36 DNA sequence variants in patients with primary open-angle glaucoma. Invest Ophthalmol Vis Sci 47, 2542–2546, https://doi.org/10.1167/iovs.05-1476 (2006).
Pasutto, F. et al. Heterozygous NTF4 mutations impairing neurotrophin-4 signaling in patients with primary open-angle glaucoma. Am J Hum Genet 85, 447–456, https://doi.org/10.1016/j.ajhg.2009.08.016 (2009).
Acharya, M. et al. Primary role of CYP1B1 in Indian juvenile-onset POAG patients. Mol Vis 12, 399–404 (2006).
Wiggs, J. L. Genetic etiologies of glaucoma. Arch Ophthalmol 125, 30–37, https://doi.org/10.1001/archopht.125.1.30 (2007).
Souzeau, E. et al. A novel de novo Myocilin variant in a patient with sporadic juvenile open angle glaucoma. BMC Med Genet 17, 30, https://doi.org/10.1186/s12881-016-0291-5 (2016).
Goldstein, O. et al. OPTN 691_692insAG is a founder mutation causing recessive ALS and increased risk in heterozygotes. Neurology 86, 446–453, https://doi.org/10.1212/WNL.0000000000002334 (2016).
Xiao, Z. et al. A novel optineurin genetic mutation associated with open-angle glaucoma in a Chinese family. Mol Vis 15, 1649–1654 (2009).
Souzeau, E. et al. Occurrence of CYP1B1 Mutations in Juvenile Open-Angle Glaucoma With Advanced Visual Field Loss. JAMA Ophthalmol 133, 826–833, https://doi.org/10.1001/jamaophthalmol.2015.0980 (2015).
Abu-Amero, K. K., Morales, J., Aljasim, L. A. & Edward, D. P. CYP1B1 Mutations are a Major Contributor to Juvenile-Onset Open Angle Glaucoma in Saudi Arabia. Ophthalmic Genet 36, 184–187, https://doi.org/10.3109/13816810.2013.841961 (2015).
Fingert, J. H. Primary open-angle glaucoma genes. Eye (Lond) 25, 587–595, https://doi.org/10.1038/eye.2011.97 (2011).
Reis, L. M. et al. Whole exome sequencing identifies multiple diagnoses in congenital glaucoma with systemic anomalies. Clin Genet, https://doi.org/10.1111/cge.12816 (2016).
Micheal, S. et al. Identification of Novel Variants in LTBP2 and PXDN Using Whole-Exome Sequencing in Developmental and Congenital Glaucoma. PLoS One 11, e0159259, https://doi.org/10.1371/journal.pone.0159259 (2016).
Huang, X. B. et al. Mutation Analysis of Seven Known Glaucoma-Associated Genes in Chinese Patients With Glaucoma. Invest Ophth Vis Sci 55, 3594–3602, https://doi.org/10.1167/iovs.14-13927 (2014).
Yang, M. et al. Investigation of CYP1B1 mutations in Chinese patients with primary congenital glaucoma. Mol Vis 15, 432–437 (2009).
Kubota, R. et al. Genomic organization of the human myocilin gene (MYOC) responsible for primary open angle glaucoma (GLC1A). Biochem Biophys Res Commun 242, 396–400, https://doi.org/10.1006/bbrc.1997.7972 (1998).
Taniguchi, F., Suzuki, Y., Shirato, S. & Ohta, S. Clinical phenotype of a Japanese family with primary open angle glaucoma caused by a Pro370Leu mutation in the MYOC/TIGR gene. Jpn J Ophthalmol 43, 80–84 (1999).
Yoon, S. J., Kim, H. S., Moon, J. I., Lim, J. M. & Joo, C. K. Mutations of the TIGR/MYOC gene in primary open-angle glaucoma in Korea. Am J Hum Genet 64, 1775–1778, https://doi.org/10.1086/302407 (1999).
Qiu, Y., Shen, X., Shyam, R., Yue, B. Y. & Ying, H. Cellular processing of myocilin. PLoS One 9, e92845, https://doi.org/10.1371/journal.pone.0092845 (2014).
Chen, X. et al. Sequence analysis of MYOC and CYP1B1 in a Chinese pedigree of juvenile glaucoma with goniodysgenesis. Mol Vis 15, 1530–1536 (2009).
Campos-Mollo, E. et al. MYOC gene mutations in Spanish patients with autosomal dominant primary open-angle glaucoma: a founder effect in southeast Spain. Molecular vision 13, 1666–1673 (2007).
Huang, X. et al. Mutation analysis of seven known glaucoma-associated genes in Chinese patients with glaucoma. Invest Ophthalmol Vis Sci 55, 3594–3602, https://doi.org/10.1167/iovs.14-13927 (2014).
Yuan, H. P. et al. Study of novel mutation of OPTN gene in two primary open angle glaucoma families in northeast China. Zhonghua Yan Ke Za Zhi 44, 147–151 (2008).
Yen, Y. C., Yang, J. J., Chou, M. C. & Li, S. Y. Absence of optineurin (OPTN) gene mutations in Taiwanese patients with juvenile-onset open-angle glaucoma. Mol Vis 14, 487–494 (2008).
Corcia, P. et al. Absence of the OPTN mutation in a patient with ALS and familial primary open angle glaucoma. J Neurol Sci 309, 16–17, https://doi.org/10.1016/j.jns.2011.07.044 (2011).
Lopez-Martinez, F. et al. Role of MYOC and OPTN sequence variations in Spanish patients with primary open-angle glaucoma. Mol Vis 13, 862–872 (2007).
Soong, B. W. et al. Extensive molecular genetic survey of Taiwanese patients with amyotrophic lateral sclerosis. Neurobiol Aging 35(2423), e2421–2426, https://doi.org/10.1016/j.neurobiolaging.2014.05.008 (2014).
Maruyama, H. et al. Mutations of optineurin in amyotrophic lateral sclerosis. Nature 465, 223–U109, https://doi.org/10.1038/nature08971 (2010).
Hollander, D. A. et al. Genotype and phenotype correlations in congenital glaucoma: CYP1B1 mutations, goniodysgenesis, and clinical characteristics. Am J Ophthalmol 142, 993–1004, https://doi.org/10.1016/j.ajo.2006.07.054 (2006).
Suri, F. et al. Screening of common CYP1B1 mutations in Iranian POAG patients using a microarray-based PrASE protocol. Molecular vision 14, 2349–2356 (2008).
Suri, F. et al. Variable expressivity and high penetrance of CYP1B1 mutations associated with primary congenital glaucoma. Ophthalmology 116, 2101–2109, https://doi.org/10.1016/j.ophtha.2009.04.045 (2009).
Su, C. C., Liu, Y. F., Li, S. Y., Yang, J. J. & Yen, Y. C. Mutations in the CYP1B1 gene may contribute to juvenile-onset open-angle glaucoma. Eye (London, England) 26, 1369–1377, https://doi.org/10.1038/eye.2012.159 (2012).
Lopez-Garrido, M. P. et al. Null CYP1B1 genotypes in primary congenital and nondominant juvenile glaucoma. Ophthalmology 120, 716–723, https://doi.org/10.1016/j.ophtha.2012.09.016 (2013).
Liu, Y. T. et al. No Evidence of Association of Heterozygous NTF4 Mutations in Patients with Primary Open-Angle Glaucoma. Am J Hum Genet 86, 498–499, https://doi.org/10.1016/j.ajhg.2009.11.018 (2010).
Rao, K. N. et al. Variations in NTF4, VAV2, and VAV3 Genes Are Not Involved with Primary Open-Angle and Primary Angle-Closure Glaucomas in an Indian Population. Invest. Ophthalmol. Vis. Sci. 51, 5, https://doi.org/10.1167/iovs.10-5553 (2010).
Chen, L. J. et al. Evaluation of NTF4 as a causative gene for primary open-angle glaucoma. Molecular vision 18, 1763–1772 (2012).
Pasutto, F. et al. Heterozygous NTF4 Mutations Impairing Neurotrophin-4 Signaling in Patients with Primary Open-Angle Glaucoma. Am J Hum Genet 85, 447–456, https://doi.org/10.1016/j.ajhg.2009.08.016 (2009).
Vithana, E. N. et al. Identification of a novel mutation in the NTF4 gene that causes primary open-angle glaucoma in a Chinese population. Molecular vision 16, 1640–1645 (2010).
Pasutto, F. et al. Profiling of WDR36 missense variants in German patients with glaucoma. Invest Ophthalmol Vis Sci 49, 270–274, https://doi.org/10.1167/iovs.07-0500 (2008).
Fan, B. J. et al. Different WDR36 mutation pattern in Chinese patients with primary open-angle glaucoma. Mol Vis 15, 646–653 (2009).
Chen, J. H., Qiu, J., Chen, H., Pang, C. P. & Zhang, M. Rapid and cost-effective molecular diagnosis using exome sequencing of one proband with autosomal dominant congenital cataract. Eye 28, 1511–1516, https://doi.org/10.1038/eye.2014.158 (2014).
Weckx, S. et al. novoSNP, a novel computational tool for sequence variation discovery. Genome Res 15, 436–442, https://doi.org/10.1101/gr.2754005 (2005).
Kelley, L. A., Mezulis, S., Yates, C. M., Wass, M. N. & Sternberg, M. J. E. The Phyre2 web portal for protein modeling, prediction and analysis. Nat Protoc 10, 845–858, https://doi.org/10.1038/nprot.2015.053 (2015).
Acknowledgements
The authors thank all of the patients and controls for their participation in this study. This study was supported by the National Natural Science Foundation of China (81470636).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: M.Z., C.P. Performed the experiments: C.H., Y.C., Y.Z. Analysed the data: C.H., Y.C. Contributed reagents/materials/analysis tools: L.X., Z.W., Y.Z. Wrote the paper: C.H., C.P.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, C., Xie, L., Wu, Z. et al. Detection of mutations in MYOC, OPTN, NTF4, WDR36 and CYP1B1 in Chinese juvenile onset open-angle glaucoma using exome sequencing. Sci Rep 8, 4498 (2018). https://doi.org/10.1038/s41598-018-22337-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-22337-2
This article is cited by
-
The comparison of corneal densitometry in cases with glaucoma following childhood cataract surgery and juvenile glaucoma
International Ophthalmology (2024)
-
A novel heterozygous c.733 T > G MYOC mutation associated with juvenile-onset open-angle glaucoma in a Chinese family
Eye (2023)
-
Identification of candidate genes and pathways in retinopathy of prematurity by whole exome sequencing of preterm infants enriched in phenotypic extremes
Scientific Reports (2021)
-
Olfactomedin domain-containing proteins: evolution, functional divergence, expression patterns and damaging SNPs
Molecular Genetics and Genomics (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.