Abstract
Spatiotemporally-localised prediction of virus emergence from wildlife requires focused studies on the ecology and immunology of reservoir hosts in their native habitat. Reliable predictions from mathematical models remain difficult in most systems due to a dearth of appropriate empirical data. Our goal was to study the circulation and immune dynamics of zoonotic viruses in bat populations and investigate the effects of maternally-derived and acquired immunity on viral persistence. Using rare age-specific serological data from wild-caught Eidolon helvum fruit bats as a case study, we estimated viral transmission parameters for a stochastic infection model. We estimated mean durations of around 6 months for maternally-derived immunity to Lagos bat virus and African henipavirus, whereas acquired immunity was long-lasting (Lagos bat virus: mean 12 years, henipavirus: mean 4 years). In the presence of a seasonal birth pulse, the effect of maternally-derived immunity on virus persistence within modelled bat populations was highly dependent on transmission characteristics. To explain previous reports of viral persistence within small natural and captive E. helvum populations, we hypothesise that some bats must experience prolonged infectious periods or within-host latency. By further elucidating plausible mechanisms of virus persistence in bat populations, we contribute to guidance of future field studies.
Similar content being viewed by others
Introduction
When a previously-unknown infectious disease emerges in human populations, wildlife species are often the focus of investigations aimed at identifying the natural reservoir host. However, this is just the first challenge; predicting, managing and preventing spillover of emerging infectious diseases to people and domestic animals depends on data, on reservoir host distribution, ecology, and immunology, as well as the mechanisms governing pathogen persistence within, and transmission among, its populations1. Due to the inherent challenges of studying wildlife and the diversity of potential hosts of zoonotic pathogens, such data are generally sparse.
Mathematical modelling approaches can circumvent some of these challenges and allow exploration of underlying processes, which can then be tested across a broad range of systems. For example, we recently investigated the importance of seasonal birth pulses and population immunity on viral persistence in closed populations across a diverse range of wild mammals2. By examining the critical community size (CCS, the threshold population size below which a virus is more likely to fade out than persist3), we showed that viruses are more likely to go extinct when the majority of the annual births take place within a short period (e.g. 1 month), compared with a species with year-round births. The effect on CCS of virus introduction into immune populations varied with the timing of the birth pulse relative to the initial epidemic peak: immunity either dampened epidemics and increased persistence (similar to the ‘priming for persistence’ phenomenon demonstrated by Pulliam et al.4,5), or resulted in higher rates of endemic fadeout and thereby decreased persistence2.
One factor rarely considered, but which might counteract the “boom and bust” virus dynamics generated by birth pulses, and thereby increase CCS, is maternal transfer of immunity6,7,8,9. Although maternally-derived antibodies (MatAb) have been reported in many vertebrate species (reviewed by 6,10, see also Supplementary Text 1), few studies have measured the persistence of those antibodies in wildlife or explored the effect of MatAb on viral dynamics (Supplementary Text 1). Compared with MatAb studies in domesticated animals11, challenges exist in model parameterisation for wildlife systems since pathogens are often endemic and affected by seasonal demography and MatAb persistence is largely unknown.
The simplifying assumptions often made in modelling studies (e.g. single, closed population of a single species), are analogous to the simplifications provided by empirical island studies. Logistical challenges aside, island populations therefore provide ideal natural experiments for studying host and disease ecology at a population level12. This is particularly the case for bats, where species traits such as nomadicism and fission-fusion population structures13,14, make it otherwise challenging to separate the dynamical effect of pathogen reintroduction into a study population from the transmission dynamics expected within a closed population. The population of African straw-coloured fruit bats (Eidolon helvum) on the remote Annobón island, Equatorial Guinea presents a rare opportunity to study viral dynamics in bat populations. This species is common and widely-distributed across continental sub-Saharan Africa and offshore islands, and recognised as a reservoir host for several potentially-zoonotic viruses across its range, including African bat henipavirus and Lagos bat virus (LBV, genus Lyssavirus)15. Located more than 180 km from the nearest island and 350 km from the African continent, the population of E. helvum bats on Annobón are both physically and genetically isolated15.
We have previously shown that persistence of the henipavirus Hendra virus was unlikely within single populations with the short infectious period demonstrated in experimentally infected animals16. Endemic circulation of Hendra virus in Australian flying foxes17, as well apparent persistence of henipaviruses in E. helvum on Annobón (estimated < 2500 bats) and in small captive colonies18 suggests that factors important for viral persistence in those systems were absent from the model2.
Here, we aim to elucidate fundamental processes governing viral dynamics in African bats, building on an extensive body of work on straw-coloured fruit bats (Eidolon helvum). We focus on two viruses for which E. helvum is a reservoir (LBV and African henipavirus), we look for evidence for the presence of MatAb in wild E. helvum and, uniquely, we use unique age-specific data to model waning rates of maternally- and infection- derived antibodies. We then focus specifically on population-level persistence of African henipavirus in the presence of MatAb, in both naive and non-naive populations, using the data to inform parameterisation of a stochastic seasonal birth model. We predict that the presence and increasing duration of MatAb will effectively reduce the ‘tightness’ of the birth pulse by dispersing the supply of susceptibles over a longer period. Applied to E. helvum bats in the isolated population on Annobón island, our results suggest that viral persistence would require long infectious periods or within-host viral latency, allowing us to narrow in on plausible mechanisms of virus persistence in bat populations and better understand infectious disease emergence.
Methods
Sample collection methods, locations and serological analyses have been described elsewhere13,15,19, and the dataset is available online (Dryad Digital Repository: http://dx.doi.org/10.5061/dryad.2fp34). In brief, fieldwork was conducted with appropriate local permissions and Zoological Society of London Ethics Committee approval (WLE/0489 and WLE/0467) and all methods were performed in accordance with the relevant guidelines and regulations. Bats were caught in mist nets or samples were obtained from other research groups or from bats hunted for human consumption (Sample sizes are shown in Supplementary Table 1). Morphometric (forearm length and body mass) and demographic (age, sex, reproductive status) data were recorded. Criteria for assessing age, reproductive status and the phase in the reproductive cycle (months since the beginning of the previous birth pulse) are described in Peel et al.19.
Blood samples were collected from Ghana, Tanzania, Bioko, São Tomé, Príncipe and Annobón under manual restraint as described previously19. From bats that were hunted, or euthanased for associated virological studies or on welfare grounds (Ghana, Tanzania, São Tomé and Príncipe), upper canine teeth were extracted, air dried and processed histologically to allow ageing based on tooth cementum annuli (Matson’s laboratory, USA)19,20. The age of all wild-caught bats was estimated to the nearest month. Neonates (N, <2 months), juveniles (J, 2 –<6 months) and sexually immature individuals (SI, 6 –<24 months) were aged from body size, sexual development and knowledge of the birth pulse timing13. For adults (A, ≥2 years), the age in years from tooth cementum data was converted to months and added to the number of months since the previous birth pulse, to give a total age in months.
Serological assays
While full genome sequence has documented the existence of African bat henipavirus21, it has not yet been isolated and cross-reactive serological assays must be used to detect its presence22. Antibodies against African henipaviruses were detected using a Nipah virus (NiV) Luminex microsphere binding assay23. Our use of the terms ‘henipavirus/henipaviruses’ is generic and represents the unknown cross-reactivity with this and other unknown African henipaviruses. Bayesian mixture models22 were used to determine a conservative cutoff threshold for seropositivity so that samples with median fluorescent intensity (MFI) readings above this cutoff were ≥99% likely to be true seropositives (MFI = 94.2, see19). Antibodies against LBV (LBV.NIG56-RV1) were detected using a mFAVN assay, using the LBVNig56 isolate, as previously described19,24. Titres were considered positive at IC100 endpoint reciprocal dilutions >1:9 (100% neutralisation of virus).
Statistical analyses
All statistical analyses were performed with the R software25. Variations in LBV and henipavirus seroprevalences across sampling events were analysed, first using univariate comparisons and χ2 tests, followed by linear mixed-effects models, to characterise changes in seroprevalence as a function of bat demography, while accounting for among-site and among-year variation. Specifically, age category (N, J, SI, A), sex and reproductive status (whether adult females were pregnant or lactating) were fixed effects, and roost location (to the country-level) and year were explored as random effects (see Supplementary Text 2 for further details). For henipavirus data, ln(MFI) was the response variable. Following Zuur et al.26, generalised linear regression models were assessed against linear mixed-effects models with various random effect structures (using the glm function, and the lme function in the nlme package27, respectively). Selection of terms for deletion or inclusion (including two-way interactions) was based on Akaike’s information criterion (AIC). The optimal AIC model was tested for significant improvement (at the 5% level) over simpler models using ANOVAs to arrive at the minimum adequate (hereafter, ‘best’) model. For LBV data, we used the glmer function in the lme4 package28 with binary neutralization assay results as the response variable.
Correlation between serological results of dam and suckling pup pairs (n = 16 pairs) was assessed using Spearman’s rank correlation (for LBV mFAVN titres) and Pearson’s product-moment correlation (for henipavirus Luminex MFIs). A Wilcoxin signed rank test was used to compare the means of paired dam-pup titres. Dam-pup pair data are presented in Supplementary Table 2.
Modelling of antibody dynamics
While the serostatus of an adult typically reflects past viral exposure and infection, serostatus in a neonate or juvenile bat may be due to the presence and subsequent waning of maternally-derived antibodies, a different and independent process. To explore signatures of waning antibodies in neonate and juvenile bats, and assess whether antibody waning also occurred subsequent to natural infection, a three-compartment susceptible-immune model (distinguishing maternally-derived from infection-acquired immunity) was created to predict age-specific seroprevalence as a function of four parameters:
p 0 = the proportion of individuals seropositive at birth (estimated from neonate seroprevalence)
λ = the force of infection, that is, the rate at which susceptible individuals become infected and immune per year (assuming negligible infection-associated mortality)
r i = the rate of antibody waning following natural infection-associated immunity
r m = the rate of maternally-derived antibody waning following birth
We assume that the population is at steady state (no temporal variations in the numbers of individuals in each category) and that antibodies confer immunity to infection.and model serology as a function of age. For any age (a), let S(a), M(a) and I(a) be the proportions of bats that are respectively seronegative (susceptible to infection), seropositive with maternally derived immunity, or seropositive due to past or current infection. We describe the dynamics of the system with two independent compartmental sub-models, one for the cohorts of bats who were protected by maternal immunity at birth (proportion p0), and the other for the cohorts of bats who were not protected at birth (proportion 1− p0). Maternal immunity is lost at rate r m , and infection-induced immunity at rate r i . We assume endemic equilibrium, an age-independent force of infection λ, an age-independent death rate d and no infection-associated mortality (no clinical signs have been demonstrated in henipavirus-infected bats16, and death from LBV infection appears to be rare in this species29). At steady state the birth rate is equal to the death rate. Furthermore, because the death rate is age-independent and infection-independent, the equations for the proportions S(a), I(a), M(a) at a given age are independent of the death rate. This can be checked by writing the equations for the number of individuals in each category, and normalising by the population size
The model is governed by this linear system of ordinary differential equations:
with boundary conditions M(0) = p0, S(0) = 1 − p0, I(0) = 0. This linear system of differential equations can be solved analytically, producing the following age distribution of seropositive individuals P(a) = I(a) + M(a):
The basic reproduction ratio of the infection, R0, is given by the inverse of the proportion of seronegative bats at a steady state (R0 = 1/S*), which can be expressed as a function of the four model parameters plus the bats’ natural death rate d by integrating over all ages:
Assuming that a bat of age a has a probability I(a) of being seropositive, given the values of the four parameters of the model we can form the likelihood of a dataset formed by N pairs (a n , x n ) where a n is the age in years of bat n and x n is its immunological status (1 for positive and 0 for negative), as follows:
The model was fitted to a binary serology dataset for each virus (sample sizes shown in Supplementary Table 1) by maximising a binomial likelihood function with respect to its four parameters, using the powell30 optimisation package in R version 3. The model was compared to one in which acquired immunity was assumed to be lifelong (i.e. r i = 0) using AIC. In order to produce confidence regions on the four parameters and R0, we generated 1000 bootstrap maximum likelihood estimates after randomly resampling each dataset with replacement. 95% confidence intervals were computed as the 2.5–97.5% interpercentile range from the set of bootstrap estimates for each parameter.
Stochastic simulations of population-level virus dynamics
To explore patterns in population-level persistence of henipaviruses, we then ran simulations of a stochastic model incorporating maternally-derived immunity and waning immunity (MSIRS: Maternally immune – Susceptible – Infectious – Recovered – Susceptible). For henipaviruses, this infection cycle is justified by experimental evidence: Hendra virus excretion followed by recovery in the absence of clinical signs has been demonstrated in experimentally infected bats16; however, almost nothing is known about henipavirus infection and its outcomes in bats following natural exposure1,31. We chose not to simulate infection dynamics for Lagos Bat virus, because Lyssaviruses in bats generally follow more complex infection cycles32,33,34,35.
The demographic model structure was based on Peel et al.2, with an annual birth pulse modelled as a periodic Gaussian function and a density-independent death rate (m) was matched so that population size was stable inter annually. The birth pulse tightness parameter (s) was estimated from published E. helvum birth records36,37. Transmission was frequency-dependent. The main modification of our previous model was the addition of a proportion (ρ) of pups from immune dams being born with maternal antibodies (M), which decay at rate (η), and the loss of acquired immunity for recovered bats (at rate ζ). Transmission and transition rates are outlined in Supplementary Table 3. Parameter ranges were selected based on expectations for E. helvum from this and previous empirical studies (Table 1). At the start of simulations, five infectious individuals were introduced 3 months prior to the birth pulse peak to minimise the likelihood that MatAb from the previous birth pulse would be present in the population in simulations with population immunity. The simulations were run using the adaptivetau package38 in R, which implements Cao et al.’s adaptive tau-leap algorithm39. We imposed an upper limit on the size of the leap to ensure minute changes in birth rates between consecutive time steps. Critical community sizes (CCS, the population size at which infection is expected to persist for 10 years at least 50% of the time, conditional on successful invasion) were calculated by fitting a binomial generalised linear model to extinctions using the dose.p function in the MASS package40 in R. The R code is available on github: https://github.com/orestif/metapopulation/blob/master/MSIR/Models/.
Data Availability
Data used in this study is available from the Dryad Digital Repository (http://dx.doi.org/10.5061/dryad.2fp34), with the exception of the dam – pup serology titres, which are provided in Supplementary Table 2.
Results
Evidence for maternal transfer of immunity was demonstrated by highly significant correlations for both LBV mFAVN reciprocal titre (ρ = 0.93, S = 50.676, p < 0.001) and NiV Luminex binding MFI (r = 0.88, t = 6.77, df = 14, p < 0.001) for 16 dam-pup pairs, in which the pups were suckling neonates (Fig. 1). Henipavirus titres were significantly higher in pups than dams (V = 11, p = 0.002).
Correlation between NiV ln(MFI) values (left) and LBV mFAVN log2 reciprocal titres (right) of dam-pup pairs. The line represents equality of dam:pup titres. Points on the LBV plot have been jittered to demonstrate multiple overlaying points. Raw data are provided in Supplementary Table 2.
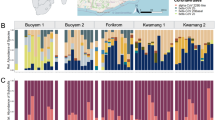
LBV and henipavirus seroprevalence was highest among neonate, juvenile and adult age classes (Fig. 2). For henipaviruses, a fixed-effect generalised linear model was optimal to predict seroprevalence, with age class, sex and the interaction between age class and sex as explanatory variables (Supplementary Text 2), with no support for inclusion of random effects.
Henipavirus and Lagos Bat Virus (LBV) seroprevalence by age class (N: Neonate, J: Juvenile, SI: Sexually Immature, A: Adult) across all sites (A) and by roost site (B). Bars show binomial 95% confidence intervals. Sample sizes are shown in Supplementary Table 1.
A mixed effect model for LBV was supported, with age class and sex as fixed effects and country as a random intercept, largely due to the significantly lower seroprevalence in Annobón (Fig. 2). Taking this into account, age class was the strongest determinant on seroprevalence (χ2(3) = 90.3, p < 0.01), with seroprevalence significantly lower in sexually immature bats compared with other age classes (Supplementary Text 2). Increasing seroprevalence with age (in years) across the entire dataset was supportive of endemic transmission (Fig. 3). Although age-specific data from teeth were not available from bats on Annobón, seroprevalence by extended age-classifications was also supportive of endemic transmission (Supplementary Fig. 1).
Age-specific seroprevalences, predicted as a function of neonate seroprevalence (p 0 ), force of infection (λ), and two rates of waning antibodies (r i and r m ), showed a good fit to both LBV and henipavirus datasets, although the LBV fit was better for the older age groups (Fig. 3). Comparable parameter estimates were obtained when using data from all populations (results shown here), versus only from panmictic populations (Ghana, Tanzania, Bioko) or data only from genetically connected island populations (São Tomé and Príncipe). For both viruses, the AIC analysis supported the inclusion of waning acquired immunity (compared to a model with life-long immunity, r i = 0), however for LBV this was marginal (ΔAIC = 2.3 c.f. henipaviruses: ΔAIC > 10), indicating that acquired immunity to LBV may be lifelong (Full model results shown in Supplementary Text 3). Given that the oldest individual in this study was 15 years, and the median age was 4.7 years, and the estimated mean duration of acquired immunity to LBV was 12 years (95% CI 5 – Infinity, Table 2), even the model with waning acquired immunity supports effective lifelong immunity to LBV. In contrast, the mean duration of acquired immunity to henipaviruses was just 4.1 years (95% CI 2.7–7.2, Table 2).
The rate of loss of maternally-derived immunity was comparable for both viruses, with a trough in seroprevalence around 11–12 months (Fig. 3) and estimates for the mean duration of maternal immunity of 5.2 months (95% CI 3.7–8.2) for LBV and 6.7 months (95% CI 5.4–8.4) for henipaviruses (Table 2).
Parameter estimates for neonate seroprevalence and force of infection were higher (with non-overlapping confidence intervals) for henipaviruses than for LBV (Table 2, Supplementary Fig. 4). On average, bats acquired immunity to LBV within 5 years 9 months of birth versus just 2 years 3 months for henipaviruses. Corresponding to the differences in force of infection, the R0 for henipavirus (2.1, 95% CI 1.9–2.3) was significantly higher than for LBV (1.6, 95% CI 1.5–1.8). These model-fitted R0 estimates were comparable to estimates calculated as 1/proportion seronegative (2.2 and 1.5 for henipavirus and LBV, respectively). We used the estimates from the fitted model as a basis for the simulations for the sake of coherence.
We developed an MSIRS model to explore the presence and rapid waning of maternal antibodies and long-lasting infection-induced antibodies. An invasion threshold occurs where the effective reproductive number (Reff) is less than one: here, given Reff = R0(1 − PI) and R0 = 2.1, infection cannot spread if PI > 0.5341. As expected, the probability of successful invasion decreased as population immunity (PI) increased (according to the formula (1/Reff)5 when infection was seeded with 5 initial cases42, Supplementary Fig. 5). However, after conditioning on successful invasion, MatAb and population immunity had non-monotonic effects on viral persistence (Supplementary Figs 5–10. When Reff > 1, successful invasion was followed by either persistent endemic cycles or ‘boom and bust’ epidemic fadeout. Epidemic fadeouts (time to extinction <2 years on Fig. 4A) typically occurred with short infectious periods in naïve populations, resulting in large CCS (Fig. 4A,C,E with PI = 0). Increasing population immunity (whilst keeping Reff > 1) markedly decreased the CCS (Fig. 4E, PI = 0.5): high PI values dampened dynamics and allowed stochastic persistence through the post-epidemic trough in an increasing proportion of simulations (Supplementary Fig. 8). In these circumstances addition and increasing duration of MatAb had comparably little effect on dynamics and CCS (Fig. 4A,C,E, Supplementary Fig. 9).
Effect of the duration of maternal antibody protection (in months, MAb), proportion of acquired population immunity (PI) and infectious period (left panels IP.d = 10 days, right panels, IP.d = 30 days) on: (A and B) persistence of infection, (C and D) number of infected individuals in a population, and (E and F) the population size for which successful of invasion and persistence of infection is more probable than not (critical community size, CCS). In A and B, stacked histograms show time to pathogen extinction (conditional on successful invasion) in series of 1000 stochastic simulations run for 10 years in a population size of 25,600 individuals. In deterministic simulations in C and D, population sizes are the same as in A and B. In E and F: grey dotted lines show the mean duration of maternal immunity, as calculated in the age-specific immunity model (henipaviruses = 6.7 months). For some sets of parameter values, probability of invasion was very low (Supplementary Fig. 5), resulting in low precision of the CCS estimate, as demonstrated by the jagged lines. Parameter values: mean lifespan = 4.5 years, s = 14.3, τ = 0.25, R0 = 2.13.
Alternatively, when successful invasion led to more stable infection dynamics (e.g. with longer infectious periods, partially-immune populations; Fig. 4D), fadeout was either rare (Fig. 4B, PI = 0.3) or driven by stochastic endemic fadeout when prevalence was low (Fig. 4A, PI = 0.5). When the rate of endemic fadeout is low (pink colours in Fig. 4B), the effect of MatAb on CCS is again limited (e.g. nearly flat lines in Fig. 4F). However, where endemic fadeout is higher and centred around the 50% threshold (observed as a trickle of fadeouts each year, resulting in the full spectrum of colours observed in Fig. 4A, Supplementary Figs 6 & 8), increasing population immunity beyond the invasion threshold (so that Reff < 1) further depletes susceptible individuals (Fig. 4A, PI = 0.7), resulting in low invasion success and return to a high CCS comparable with that in naïve populations (Fig. 4E, Supplementary Fig. 8). Additionally, at such high levels of population immunity, transmission is severely dampened. The fraction of introductions resulting in successful invasion propagate as slow, smouldering, low-amplitude transmission cycles8 until either endemic fadeout occurs or an epidemic eventually takes off (Supplementary Fig. 8, Supplementary Fig. 10). Here, the effect of the addition of MatAb is more apparent: transmission can smoulder for more than a year before initiating an epidemic. This long duration makes them more susceptible to annual smothering with the reduced influx of susceptible individuals during the birth pulse, which further dampens and slows transmission, leading to higher fadeout rates and higher CCS (Fig. 4B, PI = 0.7).
In general, trends are therefore dependent on unique combinations of demographic and transmission parameters. The diversity of the effects of acquired population immunity and maternally-derived immunity on CCS are shown in Supplementary Figs 5–10
Discussion
To move beyond identification of broad geographic ‘hotspots’ of zoonotic viral emergence towards spatiotemporal prediction, management, and prevention of spillover at a local scale, we need to understand the finer scale drivers of disease dynamics in the reservoir host, and how seasonality and host immunity affect the timing of outbreak risk. Using empirical data from a wildlife host apparently capable of supporting endemic circulation of multiple viruses, we estimated relevant parameters and explored their effect on viral persistence in closed populations with seasonal births. We tested current alternative hypotheses on viral transmission dynamics in bats by applying these results to a natural system bearing strong resemblance to our model: a small, isolated island population, with an absence of alternative host species and immigration from other populations.
The existence of MatAb was supported by significant correlation of dam-pup assay titres, consistent with previous reports for bat rabies virus43, and for henipaviruses in captive bats18. Our observation of higher offspring titres than paired maternal titres is also consistent with those studies and with human studies (for example44,45). Furthermore, we estimated an average duration of maternally derived immunity to around 6 months for both viruses. This is in line with direct measurements by repeated sampling of captive-born E. helvum bats (6–7 months)18,46. The observed trough in seroprevalence in 1-year-old wild caught bats is consistent with captive E. helvum, where sexually immature bats were mostly found to seroconvert between 16–24 months18. Seroprevalence thereafter increased with age, with henipaviruses showing a significantly higher estimated force of infection than LBV, translating to a higher R0, an earlier age at first infection and more rapid rise in seroprevalence with age. Hayman et al.24,47 previously estimated R0 as 1.6 (95% CI 1.3–2.0) for both viruses from a single cross-sectional serosurvey of 59 bats in Ghana in 2007, based on the inverse of the proportion of seronegative individuals. With an expanded dataset (LBV: 1400 bats, henipaviruses: 2272 bats), our estimates using this method were comparable for LBV (95% CI 1.5–1.7) but greater for henipaviruses (2.1–2.3).
These empirical estimates enabled us to parameterise an infection model based solely on serological data from wild caught individuals, facilitating exploration of the critical community size for African henipaviruses in E. helvum bats as a function of their (as yet unknown) infectious periods. In most cases, the critical population size required for viral persistence was only minimally affected by the presence and duration of MatAb. The smaller proportion of the population capable of possessing MatAb also meant that the magnitude of the effect of these short-lived Ab was comparatively less than the presence of acquired immunity within the population as a whole.
Applying the predictions from our model to the isolated population of E. helvum on the remote island Annobón in the Gulf of Guinea, with an estimated size of <2500 bats, the persistence of henipavirus following a single introduction would require an infectious period of at least 40 days (Supplementary Figure 11). This estimate is considerably longer than current expectations: the infectious period for African henipaviruses are unknown but is ~7 days for the related Hendra virus in Australian fruit bats16. Alternatively, previous unsuccessful viral introductions, resulting in existing immunity within the population for the next introduction may play a role in henipaviral persistence in small populations4,5. Repeat migration events within the expected lifespan of immune bats, which would be required to establish persistent infection on Annobón, is not supported by the strong genetic differentiation and low number of mitochondrial haplotypes present in bats on the island15. Future age-specific serosurveys and genetic studies on Annobón are required to demonstrate seroconversion in bats born in the seven years since our first survey, confirm endemic circulation, and make further inferences on the likelihood of migrants contributing to persistence. Additionally, while preliminary explorations of the sensitivity of the MSIRS model to the estimated birth pulse duration indicated that even constant year-round births in Annobón would not significantly improve persistence (Supplementary Figure 11), further explorations of this across a more generic and wider range of parameter values would be valuable.
An alternative to long infectious periods and priming for persistence contributing to persistence of henipaviruses in small populations is the possibility that at least some individuals experience prolonged periods of viral latency or prolonged incubation periods. The similar antibody dynamics and waning estimates for LBV estimated parameters provide support for the need for at least some individuals to experience prolonged incubation periods. For LBV, a Lyssavirus, this would be consistent with expectations from field and laboratory studies of rabies virus-infected bats in the Americas, where individuals experience extended incubation periods between exposure until manifestation of clinical disease and infectiousness, for example33,48. A complexity not explored in our general model is that infection outcome may be dependent on the infection route and dose and that exposure of bats to rabies virus can induce seroconversion in the absence of clinical signs or becoming infectious33. Incubation periods and seroconversion in the absence of infectiousness have not yet been demonstrated for LBV in E. helvum, however future modelling studies would benefit from exploring this further. Persistent latent infection, with viral shedding during times of immunological stress has been suggested as contributing to henipavirus transmission dynamics1,31. Life-long latent infections with continuous or intermittent excretion would be expected to considerably lower the CCS. For some viruses in some animal species, persistent infections such as this may occur if infection happens during particular age ranges (e.g. foetal pestivirus infection in ruminants and camelids49 or neonatal arenavirus infection in wild rodents (Mastomys natalensis) result in persistent infection and long-lasting viral excretion, with or without antibody development50). Further models to explore the effect of latency on transmission dynamics and CCS are required.
We acknowledge that estimation of antibody waning rates (both for MatAb and infection-induced antibodies) with the method we used is challenged by accurate age estimation, irregular sampling periods and individual heterogeneity in initial titre. Environmental and seasonal effects on maternal physiology and immune status are expected to influence dam-pup MatAb transfer and subsequent waning times will be longer in individuals with high MatAb titres at birth e.g.51. The variable period over which waning of MatAb occurs (providing a ‘trickle’ of susceptible individuals), combined with the observation that bats born to seronegative dams are likely to become infected earlier than those born with MatAb18, could dampen the effect of the birth pulse on transmission and persistence. However, Baker et al.’s18 multi-year study in a small captive population demonstrated that seroconversions in adult females and in sexually immature bats all occurred within tight windows around pregnancy and breeding periods. It is unclear how henipaviruses are persisting in a small captive population between these periods. Similar windows of increased paramyxovirus transmission, apparently late pregnancy, have also been demonstrated in wild bat populations52.
Anamnestic responses (ongoing ‘boosting’ of antibody levels due to repeated infection) would complicate estimation of waning rates. These were supported by Baker et al.’s finding that18 73% of positive henipavirus seroconversions in adult bats (>fourfold increase in antibody titre) represented antibody ‘boosting’, that is, occurred in already seropositive bats. Big brown bats (E. fuscus) experimentally infected with bat rabies virus48 developed antibodies which waned within 6 months in bats after a single exposure, but persisted for longer after each repeated exposure. Similarly, a study of wild E. fuscus bats demonstrated mean seroprevalence for anti-rabies virus antibodies was ~18% in wild adult females, yet their probability of seroconverting in a given year approached one53. Together with Turmelle et al.’s48 observation that some bats did not develop a detectable antibody response at all, these studies suggest that the proportion of bats within a natural population that have previously been exposed to rabies virus is likely to be considerably greater than the seroprevalence suggests. Similar findings have recently been reported in Egyptian rousette bats (Rousettus aegyptiacus) in an experimental setting, where Marburg virus infection led to viral excretion and seroconversion, followed by rapid antibody waning54. Re-exposure of these seronegative bats to Marburg virus resulted in rapid seroconversion in the absence of any evidence of viral replication or excretion55. This has implications for the parameterisation of viral dynamic models: we assume that anitbodies represent resistence to infection and that waning leads to an individual becoming susceptible. If infection leads to lifelong resistance to infection (and infectiousness) via other immune pathways, even in seronegative bats55, then critical community sizes would be larger than those estimated here. Further insights into bat immunology and longitudinal studies of individually isolated, naturally infected bats would be required to resolve this across multiple host-viral systems. Modelling SIR or SIRS dynamics with boosted antibody response in recovered individuals would also provide further insight.
Serosurveys have many benefits and a clear role in identifying reservoirs, however they present limitations for the inference of viral dynamics1,56. Availability of age-specific data was key to this study. In the absence of age-specific data (as is often the case in wildlife studies), exciting new approaches integrating laboratory studies and serological titres from cross-sectional field surveys show promise for the inference of time of infection, force of infection, and subsequently, population-level dynamics57,58. Yet, these methods rely on the existence of antibody titre data, measured repeatedly from multiple individuals. Generally this exists through experimental infection studies or, in some cases, in wild populations where high individual recapture rates are possible. For bat species, such as E. helvum, where the recapture of wild bats is exceptionally unlikely, and for emerging viruses, where experimental infections of highly pathogenic zoonoses are challenging and expensive, these data generally do not exist59. Additionally, a strong reliance on expected antibody dynamics inferred from model systems means these methods are “currently inaccessible for diseases with poorly understood or unpredictable immunological dynamics”58, such is the case for most bat viral infections1,48. Possibly due to unrealistic expectations that seronegative wild-caught bats have not previously been exposed to a particular virus, individual bat serological responses to experimental infections have been idiosyncratic. Despite these challenges, these methods are extremely promising and the additional insight that could be obtained from existing large cross-sectional serological datasets for emerging bat viruses provides further incentive for pursuing better understanding of bat immunology and immunological responses to specific bat pathogens.
Conclusions
Elucidating bat viral dynamics faces many challenges, particularly that bat immunological responses are poorly understood and observed patterns in empirical data could equally result from multiple underlying processes and transmission mechanisms1. Here, we use age-specific serological data to obtain an unprecedented level of detail on bat viral dynamics and present the first quantification of viral antibody dynamics in wild African bats. While mechanisms like repeat introductions and metapopulation structure may drive viral dynamics in the large panmictic continental population of E. helvum, we have demonstrated that prolonged infectious periods or within-host latency are required to explain henipavirus persistence within small natural and captive populations18,60. Experimental and field studies exploring mechanisms of within-host viral persistence in bats should be a priority area for future research to inform our understanding of infectious disease emergence. Applicable across wildlife disease systems more broadly, we show that dynamic models informed by existing empirical data can help narrow-in on the most plausible competing hypothesis and guide future field studies61.
References
Plowright, R. K. et al. Transmission or Within-Host Dynamics Driving Pulses of Zoonotic Viruses in Reservoir-Host Populations. PLoS Negl Trop Dis 10, e0004796 (2016).
Peel, A. J. et al. The effect of seasonal birth pulses on pathogen persistence in wild mammal populations. Proc. R. Soc. B 281, 20132962 (2014).
Bartlett, M. Measles periodicity and community size. J. Roy. Statistical Society 120, 48–70 (1957).
Pulliam, J. R. C., Dushoff, J. G., Levin, S. A. & Dobson, A. P. Epidemic enhancement in partially immune populations. PLoS ONE 2, e165 (2007).
Pulliam, J. R. C. et al. Agricultural intensification, priming for persistence and the emergence of Nipah virus: a lethal bat-borne zoonosis. J R Soc Interface 9, 89–101 (2012).
Boulinier, T. & Staszewski, V. Maternal transfer of antibodies: raising immuno-ecology issues. Trends Ecol Evol 23, 282–288 (2008).
Fouchet, D., Marchandeau, S., Langlais, M. & Pontier, D. Waning of maternal immunity and the impact of diseases: The example of myxomatosis in natural rabbit populations. Journal of Theoretical Biology 242, 81–89 (2006).
Plowright, R. K. et al. Urban habituation, ecological connectivity and epidemic dampening: the emergence of Hendra virus from flying foxes (Pteropus spp.). Proc. R. Soc. B 278, 3703–3712 (2011).
Wells, K. et al. Timing and severity of immunizing diseases in rabbits is controlled by seasonal matching of host and pathogen dynamics. J R Soc Interface 12, 20141184–20141184 (2015).
Hasselquist, D. & Nilsson, J.-Å. Maternal transfer of antibodies in vertebrates: trans-generational effects on offspring immunity. Philosophical Transactions of the Royal Society B: Biological Sciences 364, 51–60 (2009).
Cador, C., Rose, N., Willem, L. & Andraud, M. Maternally Derived Immunity Extends Swine Influenza A Virus Persistence within Farrow-to-Finish Pig Farms: Insights from a Stochastic Event-Driven Metapopulation Model. PLoS ONE 11, e0163672 (2016).
Clutton-Brock, T. H. & Pemberton, J. M. Soay Sheep. (Cambridge University Press, 2004).
Peel, A. J. et al. How Does Africa’s Most Hunted Bat Vary Across the Continent? Population Traits of the Straw-Coloured Fruit Bat (Eidolon helvum) and Its Interactions with Humans. Acta Chiropterologica 19, 77–92 (2017).
Patriquin, K. J. & Ratcliffe, J. M. In Sociality in Bats 101, 65–103 (Springer International Publishing, 2016).
Peel, A. J. et al. Continent-wide panmixia of an African fruit bat facilitates transmission of potentially zoonotic viruses. Nature Communications 4, 3770 (2013).
Halpin, K. et al. Pteropid Bats are Confirmed as the Reservoir Hosts of Henipaviruses: A Comprehensive Experimental Study of Virus Transmission. Am J Trop Med Hyg 85, 946–951 (2011).
Field, H. E. et al. Spatiotemporal Aspects of Hendra Virus Infection in Pteropid Bats (Flying-Foxes) in Eastern Australia. PLoS ONE 10, e0144055 (2015).
Baker, K. S. et al. Viral antibody dynamics in a chiropteran host. J Anim Ecol 83, 415–428 (2013).
Peel, A. J. et al. Bat trait, genetic and pathogen data from large-scale investigations of African fruit bats, Eidolon helvum. Sci Dat 3, 160049 (2016).
Matson, G. et al. A laboratory manual for cementum age determination of Alaska brown bear first premolar teeth. (Matson’s Laboratory, 1993).
Drexler, J. F., Corman, V. & Müller, M. Bats host major mammalian paramyxoviruses. Nature Communications 3, 1–12 (2012).
Peel, A. J. et al. Use of cross-reactive serological assays for detecting novel pathogens in wildlife: assessing an appropriate cutoff for henipavirus assays in African bats. Journal of Virological Methods 193, 295–303 (2013).
Bossart, K. N. et al. Neutralization assays for differential henipavirus serology using Bio-Plex Protein Array Systems. Journal of Virological Methods 142, 29–40 (2007).
Hayman, D. T. S. et al. Antibodies against Lagos bat virus in megachiroptera from West Africa. Emerg Infect Dis 14, 926–928 (2008).
R Core Team, R: A language and environment for statistical computing. Version 3, 0 (2016).
Zuur, A., Ieno, E. N., Walker, N., Saveliev, A. A. & Smith, G. M. Mixed Effects Models and Extensions in Ecology with R. (Springer Science & Business Media, 2009).
Pinheiro, J., Bates, D. & DebRoy, S. R Core Team. nlme: Linear and Nonlinear Mixed Effects Models. (2016).
Bates, D., Maechler, M., Bolker, B. & Walker, S. lme4: Linear mixed-effects models using Eigen andS4. (2014).
Suu-Ire, R. et al. Lagos Bat Virus Infection Dynamics in Free-Ranging Straw-Colored Fruit Bats (Eidolon helvum). Tropical Medicine and Infectious Disease 2017, 2, 25 (2017).
Dorai-Raj, S. powell: Powell’s UObyQA algorithm. CRAN (2006).
Sohayati, A. R. et al. Evidence for Nipah virus recrudescence and serological patterns of captive Pteropus vampyrus. Epidemiol Infect 139, 1570–1579 (2011).
Kuzmin, I. V. & Rupprecht, C. E. In Bats and Viruses (eds Wang, L.-F. & Cowled, C.) 47–97 (John Wiley & Sons, 2015). https://doi.org/10.1002/9781118818824.
Franka, R. et al. Susceptibility of North American big brown bats (Eptesicus fuscus) to infection with European bat lyssavirus type 1. J Gen Virol 89, 1998–2010 (2008).
George, D. B. et al. Host and viral ecology determine bat rabies seasonality and maintenance. PNAS 108, 10208–10213 (2011).
Blackwood, J. C., Streicker, D. G., Altizer, S. & Rohani, P. Resolving the roles of immunity, pathogenesis, and immigration for rabies persistence in vampire bats. PNAS 110, 20837–20842 (2013).
Hayman, D. T. S. Biannual birth pulses allow filoviruses to persist in bat populations. Proc. R. Soc. B 282, 20142591–20142591 (2015).
Hayman, D. T. S. & Peel, A. J. Can survival analyses detect hunting pressure in a highly connected species? Lessons from straw-coloured fruit bats. Biol Conserv 200, 131–139 (2016).
Johnson, P. adaptivetau: Tau-Leaping Stochastic, R package version 2.2, available from https://CRAN.R-project.org/package = adaptivetauSimulation.
Cao, Y., Gillespie, D. T. & Petzold, L. R. Adaptive explicit-implicit tau-leaping method with automatic tau selection. Journal of Chemical Physics 126, 224101–224109 (2007).
Venables, W. N. & Ripley, B. D. Modern Applied Statistics with S. (Springer, 2002).
Lloyd-Smith, J. O. et al. Should we expect population thresholds for wildlife disease? Trends Ecol Evol 20, 511–519 (2005).
Diekmann, O. & Heesterbeek, J. A. P. Mathematical Epidemiology of Infectious Diseases: Model Building, Analysis and Interpretation. (John Wiley & Sons, 2000).
Constantine, D. G., Tierkel, E. S., Kleckner, M. D. & Hawkins, D. M. Rabies in New Mexico cavern bats. Public Health Rep 83, 303–316 (1968).
Sato, H., Albrecht, P., Reynolds, D. W., Stagno, S. & Ennis, F. A. Transfer of measles, mumps, and rubella antibodies from mother to infant. Its effect on measles, mumps, and rubella immunization. Am. J. Dis. Child. 133, 1240–1243 (1979).
Pitcher-Wilmott, R. W., Hindocha, P. & Wood, C. B. The placental transfer of IgG subclasses in human pregnancy. Clin. Exp. Immunol. 41, 303–308 (1980).
Epstein, J. H. et al. Duration of Maternal Antibodies against Canine Distemper Virus and Hendra Virus in Pteropid Bats. PLoS ONE 8, (2013).
Hayman, D. T. S. et al. Evidence of henipavirus infection in West African fruit bats. PLoS ONE 3, e2739 (2008).
Turmelle, A. S., Jackson, F. R., Green, D., McCracken, G. F. & Rupprecht, C. E. Host immunity to repeated rabies virus infection in big brown bats. J Gen Virol 91, 2360–2366 (2010).
Nelson, D. D., Duprau, J. L., Wolff, P. L. & Evermann, J. F. Persistent Bovine Viral Diarrhea Virus Infection in Domestic and Wild Small Ruminants and Camelids Including the Mountain Goat (Oreamnos americanus). Front. Microbiol. 6, 171 (2016).
Borremans, B. et al. Shedding dynamics of Morogoro virus, an African arenavirus closely related to Lassa virus, in its natural reservoir host Mastomys natalensis. Sci. Rep. 5, 56 (2015).
Grindstaff, J. L. Initial levels of maternally derived antibodies predict persistence time in offspring circulation. J Ornithol 151, 423–428 (2010).
Dietrich, M. et al. Leptospira and paramyxovirus infection dynamics in a bat maternity enlightens pathogen maintenance in wildlife. Environmental Microbiology n/a–n/a https://doi.org/10.1111/1462-2920.12766 (2015).
O’Shea, T. J., Bowen, R. A., Stanley, T. R., Shankar, V. & Rupprecht, C. E. Variability in Seroprevalence of Rabies Virus Neutralizing Antibodies and Associated Factors in a Colorado Population of Big Brown Bats (Eptesicus fuscus). PLoS ONE 9, e86261 (2014).
Schuh, A. J. et al. Modelling filovirus maintenance in nature by experimental transmission of Marburg virus between Egyptian rousette bats. Nature Communications 8, 14446 (2017).
Schuh, A. J. et al. Egyptian rousette bats maintain long-term protective immunity against Marburg virus infection despite diminished antibody levels. Sci. Rep. 7, 535 (2017).
Gilbert, A. T. et al. Deciphering Serology to Understand the Ecology of Infectious Diseases in Wildlife. Ecohealth 10, 1–16 (2013).
Borremans, B., Hens, N., Beutels, P., Leirs, H. & Reijniers, J. Estimating Time of Infection Using Prior Serological and Individual Information Can Greatly Improve Incidence Estimation of Human and Wildlife Infections. PLoS Computational Biology 12, e1004882 (2016).
Pepin, K. M. et al. Inferring infection hazard in wildlife populations by linking data across individual and population scales. Ecology Letters https://doi.org/10.1111/ele.12732 (2017).
Hayman, D. T. S. et al. Demography of straw-colored fruit bats in Ghana. J Mammal 93, 1393–1404 (2012).
Peel, A. J. et al. Henipavirus neutralising antibodies in an isolated island population of African fruit bats. PLoS ONE 7, e30346 (2012).
Restif, O. et al. Model-guided fieldwork: practical guidelines for multidisciplinary research on wildlife ecological and epidemiological dynamics. Ecology Letters https://doi.org/10.1111/j.1461-0248.2012.01836.x (2012).
Acknowledgements
We acknowledge Raina Plowright for thoughtful comments on an earlier draft of this manuscript. The authors thank the governments of Ghana, Tanzania, Malawi, Zambia, Uganda, Equatorial Guinea, and São Tomé and Príncipe for facilitating this research. For their invaluable support in planning and implementing the field work, we also thank Guy-Crispin Gembu; Tiziana Lembo; Iñaki Rodriguez-Prieto; Alex Torrance; Lucrecia Bilé Osa Ahara; Heidi Ruffler; Ricardo Castro César de Sá; Ricardo Faustino de Lima; Mariana Carvalho; Richard Suu-Ire; Andy Alhassan; and Meyir Ziekah. Funding for this study was provided by the Isaac Newton Trust (AJP), a Queensland Accelerate Postdoctoral Research Fellowship (AJP), a Wellcome Trust Clinical Research Career Development Fellowship (106690/A/14/Z), the Alborada Trust (JLNW, OR), a European Union FP7 project ANTIGONE (Anticipating Global Onset of Novel Epidemics 278976) (ACB, JLNW, AAC), a Royal Society Wolfson Research Merit Award (AAC), and a Royal Society University Research Fellowship (OR).
Author information
Authors and Affiliations
Contributions
A.J.P., K.S.B., D.T.S.H., A.A.C., J.L.N.W., A.R.F. and O.R. conceived the research. A.J.P., K.S.B. and D.T.S.H. conducted fieldwork. A.J.P., K.S.B. and D.T.S.H. conducted serological assays. A.J.P. and O.R. performed analyses and wrote the manuscript. C.C.B. designed and produced the Luminex antigens used in serological assay. A.A.C., J.L.N.W. and A.R.F. provided funding and contributed to data interpretation. R.G. contributed to the manuscript. All co-authors read and edited the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peel, A.J., Baker, K.S., Hayman, D.T. et al. Support for viral persistence in bats from age-specific serology and models of maternal immunity. Sci Rep 8, 3859 (2018). https://doi.org/10.1038/s41598-018-22236-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-22236-6
This article is cited by
-
Selective replication and vertical transmission of Ebola virus in experimentally infected Angolan free-tailed bats
Nature Communications (2024)
-
Longitudinal monitoring in Cambodia suggests higher circulation of alpha and betacoronaviruses in juvenile and immature bats of three species
Scientific Reports (2021)
-
Seasonal shedding patterns of diverse henipavirus-related paramyxoviruses in Egyptian rousette bats
Scientific Reports (2021)
-
Effects of Waning Maternal Immunity on Infection Dynamics in Seasonally Breeding Wildlife
EcoHealth (2021)
-
Reproduction of East-African bats may guide risk mitigation for coronavirus spillover
One Health Outlook (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.