Abstract
The recombinant phage endolysins AP50-31 and LysB4 were developed using genetic information from bacteriophages AP50 and B4 and were produced by microbial cultivation followed by chromatographic purification. Subsequently, appropriate formulations were developed that provided an acceptable stability of the recombinant endolysins. The bacteriolytic properties of the formulated endolysins AP50-31 and LysB4 against several bacterial strains belonging to the Bacillus genus including Bacillus anthracis (anthrax) strains were examined. AP50-31 and LysB4 displayed rapid bacteriolytic activity and broad bacteriolytic spectra within the Bacillus genus, including bacteriolytic activity against all the B. anthracis strains tested. When administered intranasally, LysB4 completely protected A/J mice from lethality after infection with the spores of B. anthracis Sterne. When examined at 3 days post-infection, bacterial counts in the major organs (lung, liver, kidney, and spleen) were significantly lower compared with those of the control group that was not treated with endolysin. In addition, histopathological examinations revealed a marked improvement of pathological features in the LysB4-treated group. The results of this study support the idea that phage endolysins are promising candidates for developing therapeutics against anthrax infection.
Similar content being viewed by others
Introduction
Bacillus anthracis (anthrax) is a bacterium of significant concern owing to its potential uses in bioterrorism and biowarfare. Currently, the medical countermeasure recommended for anthrax infection is the administration of antibiotics. Some strains of B. anthracis, however, show natural antibiotic resistance1,2. In addition, in vitro development of antibiotic resistance was demonstrated in a laboratory3. Strains that were even resistant to ciprofloxacin were generated by in vitro selection4,5. In the late 1980s, scientists of the former Soviet Union allegedly made a strain resistant to five antibiotics6. Therefore, there have been concerns about bioterrorism through the use of engineered antibiotic-resistant B. anthracis strains7,8,9. Despite such a potentially significant public health threat, there are currently no antibacterial therapeutic measures, while treatment with anti-toxin antibodies is a potential alternative10. Therefore, it is necessary to secure novel antibacterial agents and biodefence tools to respond to a potential future B. anthracis crisis. These novel antibacterial agents should be effective against both antibiotic-susceptible and antibiotic-resistant B. anthracis strains. To meet this requirement, the novel antibacterial agents should have a completely different mode of action than those of commonly used antibiotics. Additionally, because anthrax is an acute infectious disease, rapid bacteriolytic activity is required. Based on these requirements, phage endolysins have been proposed as candidate novel antibacterial agents for the specific use against B. anthracis 11,12.
Phage endolysins (also known as phage lysins or lysins) are enzymes of bacteriophages that degrade the peptidoglycan wall of infected bacteria, resulting in the release of progeny phages13. The exogenous application of the purified recombinant phage endolysin to Gram-positive bacteria induces rapid bacterial cell lysis and death13,14. Phage endolysins are promising antibacterial agents to use against pathogens because of their high specificity and low level of bacterial resistance development15. They are also promising antibacterial agents to use against antibiotic-resistant pathogens. Several prior studies have demonstrated the efficacy of endolysins against B. anthracis 11,12, Streptococcus pneumonia 16, Staphylococcus aureus 17, and Clostridium difficile 18, and animal model studies have indicated their potential to cure human infections16,19,20,21,22,23,24,25.
Phage endolysins differ from standard antibiotics in their potency, specificity, speed, and activity against antibiotic-resistant bacteria. Additionally, phage endolysins are usually specific for a particular target bacterial species and do not generally lyse non-target bacteria, including commensal bacteria, that may reduce clinical complications26. Thus, research on phage endolysins is one of the most promising areas on the development of novel antibacterials against human pathogens26. In this paper, we report on the development of novel antibacterial agents effective in treating B. anthracis infections through bacteriolytic activity based on phage endolysins.
Results
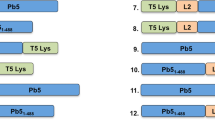
Selection of target endolysins
Based on publicly available genetic information for endolysins, we chose two phage endolysins: those of B. anthracis bacteriophage AP5027 and B. cereus bacteriophage B428,29. Phage endolysin AP50-31 was developed using genomic information from B. anthracis bacteriophage AP50, and phage endolysin LysB4 was developed using genomic information from B. cereus bacteriophage B4. Bacteriophage AP50 has two putative endolysin genes (ORFs 25 and 31) and the ORF 31 was selected due to its unique domain type. AP50-31 is predicted to have the amidase02_C and amidase_3 (N-acetylmuramoyl-l-alanine amidase) catalytic domains while lacking a cell wall binding domain. LysB4 is predicted to have a catalytic VanY (l-alanoyl-d-glutamate endopeptidase) domain and a cell wall binding SH3_5 domain28. AP50-31 and LysB4 do not have any signal peptides or transmembrane regions based on the analyses using SignalP30 and THMHH31 prediction programs. The characteristics of AP50-31 and LysB4 are presented in Supplementary Table S1.
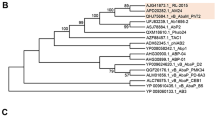
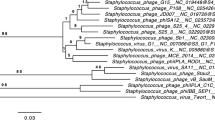
To understand the relationships between the target endolysins in this study and other phage endolysins, 23 putative endolysins were selected from Bacillus phages that were assigned as completely sequenced in the NCBI database. A phylogenetic tree was constructed for the 25 endolysins, including AP50-31 and LysB4 (Fig. S1). The phylogenetic tree placed AP50-31 into a group between PBC1 and BCJA1c, while LysB4 was determined to belong to SPO1, forming a cluster with Spock, AvesoBmore, Riley, and Troll. The amino acid sequences of endolysins LysB429, Spock32, Troll33, AvesoBmore34, and Riley33 were almost identical, although their parent bacteriophages were different (Fig. S2). The characteristics of the putative endolysins used in the construction of phylogenetic tree are presented in Supplementary Table S1.
Production and purification of AP50-31 and LysB4
Expression plasmids were constructed based on the pBAD expression system and were transformed with E. coli BL21 to produce the recombinant endolysins AP50-31 and LysB4 (Table 1). Recombinant phage endolysins were produced using these production hosts.
AP50-31, with no extraneous amino acid residues such as purification tags, was produced in a soluble form by decreasing the culture temperature to 30 °C immediately after the induction of expression. Using one-step cation-exchange chromatography, AP50-31 was purified from crude E. coli cell extracts with more than 90% purity, as confirmed by sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and size-exclusion chromatography/high-performance liquid chromatography (SEC-HPLC) analyses. This purity was sufficient for all of the experiments performed in this study. The appropriate pH range for binding to the column was narrow under the chromatographic conditions utilised in this study and was within less than ±0.5 deviation from pH 7.5. Using the expression and purification methods described in the Materials and Methods, approximately 72 mg of purified AP50-31 was routinely obtained from 1L of culture.
A soluble form of recombinant LysB4 was successfully produced without decreasing the culture temperature from 37 °C. The endolysin contained no extraneous amino acids. The expression level of LysB4 was similar to that of AP50-31. LysB4 was obtained using a one-step cation-exchange chromatography procedure with more than 90% purity, as confirmed by SDS-PAGE and SEC-HPLC analyses. A total of 132 mg of phage endolysin LysB4 was generally obtained from 1 L of culture.
Development of formulations adequate for the stable storage of AP50-31 and LysB4
We aimed to develop effective formulations that prevented the aggregation of the phage endolysins while still maintaining stability during 12 weeks of storage and also during a shorter period of physical stress such as agitation. An appropriate formulation for the stable storage and handling of LysB4 was developed through the preformulation screening of pH, buffer type, surfactant and additive while considering the commonly used drug compositions used for injection. The best formulation was comprised of 0.1% (w/v) polysorbate 80, 5% (w/v) sorbitol, and 10 mM l-histidine (pH 6). This formulation significantly stabilised LysB4 that showed nearly 100% integrity and biological activity after 12 weeks of storage at 4 °C and −20 °C or after constant vigorous agitation for up to 4 h. However, this formulation did not provide acceptable stability for storage at 25 °C, because significant degradation was observed after three weeks of storage. Although all of the formulation candidates tested did not provide sufficient stability for AP50-31 when stored at 4 °C, the formulation containing 0.5% (w/v) poloxamer 188, 5% (w/v) sorbitol, and 10 mM sodium phosphate (pH 7.5) provided relatively good stability. This formulation provided sufficient stability for AP50-31 after incubation under accelerated stability study conditions (40 °C for 16 h) under vigorous constant agitation (2,500 rpm) for up to 4 h, and after being stored at −20 °C for 12 weeks. Because AP50-31 was shown to be stable in the three conditions described above, we believed that the formulation containing 0.5% (w/v) poloxamer 188, 5% (w/v) sorbitol, and 10 mM sodium phosphate (pH 7.5) was sufficient to conduct the experiments planned in this study. Thus, the formulation containing 0.5% (w/v) poloxamer 188, 5% (w/v) sorbitol, and 10 mM sodium phosphate (pH 7.5) was chosen as a temporary formulation for the subsequent experiments in this study.
In vitro bacteriolytic properties
The bacteriolytic activities of AP50-31 and LysB4 were examined using a conventional turbidity reduction assay that measured the time required to reach one-half of the starting absorbance (TOD50) after each phage endolysin was added at a final concentration of 5 μg/mL to a bacterial cell suspension (optical density at 600 nm [OD600] = 1.0). The results obtained for the non-anthracis Bacillus strains are summarised in Table 2. AP50-31 and LysB4 displayed broad bacteriolytic spectra within the Bacillus genus and displayed rapid bacteriolytic properties. However, differences in bacteriolytic activity and the bacteriolytic spectrum range between the two endolysins were observed. LysB4 exhibited more rapid bacteriolytic activity, and a broader bacteriolytic spectrum range than the phage endolysin AP50-31. Additionally, AP50-31 and LysB4 exhibited rapid and effective bacteriolytic activities against all of the strains of B. anthracis tested (Table 3). Although LysB4 showed smaller TOD50 values against all four B. anthracis strains tested, the difference was statistically significant only for B. anthracis ATCC 14578 and B. anthracis HYU01 (Welch’s t-test, P < 0.05).
In vivo efficacy test of LysB4 against B. anthracis
Challenge with spores of B. anthracis caused physical signs of ill health in the buffer-treated mice that manifested as hunched backs, ruffed fur, piloerection, and ocular discharge (G1, Fig. 1A). These clinical signs appeared 3–4 days after the bacterial challenge and became aggravated in a time-dependent manner. LysB4 treatment markedly improved the clinical signs and no symptoms were observed in the high-dose LysB4-treated group (G3, 100 μg/head; Fig. 1B). In addition, LysB4 treatment efficiently rescued the infected mice, and no deaths were observed in the high-dose LysB4-treated group throughout the experimental period. The administration of high-dose LysB4 at 6, 24, and 48 h post-infection provided 100% survival (G3, 100 μg/head), while low-dose LysB4 treatment (G2, 10 μg/head) delayed the onset of death and significantly improved the survival rate (Fig. 1C). The mean body temperature of the mice decreased corresponding to the onset of clinical signs, and the decrease was more prominent in the buffer-treated group compared with the LysB4-treated groups (Fig. 1D).
Results of survival rate and body temperature in in vivo study. A/J mice were infected intranasally with approximately 4 times the 50% lethal dose of spores of B. anthracis Sterne. At 6, 24, and 48 h post-infection, buffer (G1) or endolysin LysB4 (G2: 10 μg/head, G3: 100 μg/head) were administered intranasally (8 mice per group). Clinical signs of buffer- (A) or LysB4- (B) treated mice, survival rate (C), and body temperature (D) were observed. ***P < 0.001 compared to the G1 group.
To determine the effect of LysB4 on bacterial clearance, the lungs, livers, spleens, and kidneys were extracted from buffer- or LysB4-treated mice at day 3 post-infection and the total count of bacteria (spores and vegetative cells) in each tissue was determined. In all of the tissues analysed, the bacterial count of the LysB4-treated group was significantly lower than that of the buffer-treated group. In the LysB4-treated group, most of the bacteria were cleared in the liver, spleen, and kidney, but a large number of the bacteria remained in the lung (Fig. 2). Histological observations revealed no remarkable pathological findings in the organs of the non-infected and non-treated control mice (Fig. 3A,D,G and J). In the lung tissue of the infected and buffer-treated group, the alveolar septum was slightly expanded and some alveolar spaces were filled with proteinaceous materials (Fig. 3B). In addition, there was marked vacuolar degeneration and necrosis of hepatocytes in the liver (Fig. 3E). Apoptotic lymphocytes characterised by fragmented and condensed nuclear debris were visible throughout the spleen in the infected and buffer-treated group (Fig. 3H). In addition, lymphocytes were significantly depleted in the white and red pulp of the spleen, and the sheath of the marginal zone was reduced (Fig. 3H). In the kidney of the infected and buffer-treated group, myriad bacilli were frequently observed in the glomeruli, tubules, and interstitial tissues (Fig. 3K). However, most of these pathological findings were markedly improved in the organs of the infected and LysB4-treated group (Fig. 3C,F,I and L), indicating that LysB4 had a protective effect against B. anthracis infection in mice.
Results of bactrial killing activity of LysB4 in in vivo study. B. anthracis-infected mice were treated with buffer (G4) or LysB4 (G5: 100 μg/head) at 6, 24, and 48 h post-infection and euthanized at day 3 post-infection (8 mice per group). Serial dilutions of lung, liver, spleen, and kidney homogenates were plated on tryptic soy agar plates and incubated at 37 °C overnight, and the colonies were counted. *P < 0.05, **P < 0.01 compared to G4 group.
Results of histopathological analysis in in vivo study. Organs of the non-infected and non-treated control, the infected and buffer-treated, and the infected and LysB4-treated mice were observed under light microscopy and representative histologic images of the lungs (A–C), livers (D–F), spleens (G–I), and kidneys (J–L) are shown. Arrowheads indicate apoptotic lymphocytes and arrows indicate clusters of bacilli. Haematoxylin and eosin staining; magnification × 200.
Discussion
With the rapid emergence of antibiotic-resistant bacteria worldwide, there is a need for new and innovative antibacterial agents with different modes of action than those of commonly used antibiotics. For B. anthracis, a potential biological weapon of mass destruction7,35, fears related to the possible engineering of antibiotic resistance necessitate a need to develop new bacteriolytic antibacterial agents. Phage endolysins are a potentially good candidate to act as antibacterial agents against B. anthracis 11.
Although many recombinant phage endolysins show a poor expression or insolubility when produced in their native forms36, the phage endolysins AP50-31 and LysB4 used in this study were successfully produced in their soluble forms and purified with high yield and purity. Compared to the previously reported production of endolysin LysB4 containing an N-terminal His-tag for purification28, the endolysins used in this study do not contain any extra amino acid residues including the His-tag, thus providing additional advantages for their use as therapeutic agents for use in human applications. The recombinant phage endolysins AP50-31 and LysB4 displayed broad bacteriolytic spectra within the Bacillus genus with different host susceptibilities and bacteriolytic activities. More importantly, they exhibited rapid bacteriolytic activities against all of the strains of B. anthracis tested, demonstrating their potential as antibacterial agents for B. anthracis infections. AP50-31 and LysB4 showed different TOD50 values against the same bacterial strain in the in vitro bacteriolytic activity experiment.
AP50-31 has 252 amino acids, and its molecular mass is 27.7 kDa. The theoretical isoelectric point of AP50-31 is estimated to be 6.44, and it contains catalytic amidase02_C and amidase_3 (N-acetylmuramoyl-l-alanine amidase) domains. In comparison, LysB4 has 262 amino acids, and its molecular mass is 27.9 kDa. The theoretical isoelectric point of LysB4 is estimated to be 9.21, and it has a catalytic VanY domain and a cell wall binding SH3_5 domain28. Although AP50-31 and LysB4 originate from bacteriophages and have similar molecular masses, there are significant differences between their isoelectric points and types of catalytic domains. We assume that these differences are the reason for the differences in TOD50 values observed for the two endolysins evaluated in this study. Additional research should be performed to analyse the structure-function relationships in detail.
This research represents the first report of the results of in vivo endolysin efficacy tests against B. anthracis using an animal model of B. anthracis infection. Previous in vivo studies used B. cereus ATCC 4342 (also known as RSVF1) as a surrogate for B. anthracis. B. cereus ATCC 4342 was isolated from milk and is categorised as a biosafety level 1 microorganism. This strain is frequently used as a surrogate for B. anthracis in biodefence studies. It was used as a bacterial challenge agent for in vivo experiments on endolysin PlyG11 and endolysin PlyPH12. Although the results of the in vivo experiments with B. cereus ATCC 4342 are valuable, the results obtained using this surrogate need careful interpretation since the pathogenic mechanisms of B. cereus and B. anthracis are substantially different. In particular, B. cereus ATCC 4342 lacks the pXO1 virulence plasmid that encodes unique anthrax toxins that include the protective antigen, lethal factor, and edema factor. For this reason, B. anthracis needs to be used for animal infection studies to prove the therapeutic effect of endolysins against anthrax. In addition, although growing vegetative cells of B. cereus were used for infection in previous studies, to simulate the actual situation, the use of spores is more suitable, since spores are expected to be the primary means of attack in potential bio-terrorism incidents involving anthrax37. Among the many routes of infection, the intranasal route was chosen since inhalational anthrax is the form of anthrax that would be most likely to be used in a bioterrorism attack to produce high mortality7. The intranasal route was chosen to administer the endolysin because we reasoned that delivering a therapeutic agent by the same route that infectious agents exploits to enter its host would significantly increase the probability of contact between the therapeutic and infectious agents. Indeed, the intranasal route of endolysin administration was effective, since delivering 100 μg of LysB4 at 6, 24, and 48 h post-infection saved 100% of the infected mice from death (Fig. 1C).
Compared to other tissues, a large number of bacteria remained in the lung (Fig. 2). Because the number of bacterial counts in the lung was the highest in the buffer-treated group (G4), and the spores were introduced intra-nasally, the higher number of bacterial counts observed in the lung in the endolysin-treated group (G5) might not be abnormal. However, an adequate explanation of this phenomenon was not possible until now. High variability in the number of remaining bacteria between individual mice was observed especially in the livers, spleens, and kidneys of the control G4 group (Fig. 2). This variability was also reported in other murine inhalational anthrax studies38,39,40.
We wish to emphasise that this is the first study to demonstrate the in vivo efficacy of endolysin against anthrax. However, our research lacks three experimental points that will be needed to fully evaluate the therapeutic potential of endolysin for treating human anthrax infection. First, the strain used for infection was B. anthracis Sterne. This strain, chosen for safety reasons, is an animal vaccine strain lacking the capsule-forming pXO2 plasmid that is necessary for full virulence. Even though the use of B. anthracis Sterne with A/J mice is a well-established model of anthrax infection, a fully virulent strain (pXO1+/pXO2+) is more desirable to show therapeutic efficacy. Second, a mouse model alone cannot fully simulate a human infection in many respects41. Various animal models are used in anthrax research, and each has its own advantages and disadvantages as a model of human anthrax41. Thus, the efficacy of endolysin needs to be tested in other animal models (ideally in a non-human primate model). Third, an aerosol challenge model is preferable to an intranasal challenge model to study the pathogenesis of inhalational anthrax42. To develop endolysins as therapeutics for human use, future studies should address these three aspects that could not be addressed in this study due to safety issues and a lack of highly specialised equipment and facilities.
Nonetheless, in this study we showed that the intranasal administration of the phage endolysin LysB4 could protect mice from lethal anthrax infections. We expect that the results and insights provided in this paper will assist in the development of phage endolysin-based therapeutics for use against anthrax in the future.
Materials and Methods
Selection of target phage endolysin sequences
The aim of this study was to develop phage endolysins that have antibacterial activity against B. anthracis. From the NCBI website (http://www.ncbi.nlm.nih.gov/genome/), we collected the genetic information of bacteriophages specific for B. anthracis, B. cereus, and B. thuringiensis. We included B. cereus and B. thuringiensis because they are close relatives of B. anthracis 43 and are often used as surrogates for B. anthracis 44,45. The genetic information from prophages was excluded. From the collected genetic information, the putative endolysin sequences were extracted. Subsequently, the target sequences of putative endolysins were selected based on an analysis of the types of catalytic domain of the putative phage endolysins using the NCBI BLASTP program (http://blast.ncbi.nlm.nih.gov/Blast.cgi).
Construction of expression hosts for the recombinant phage endolysins AP50-31 and LysB4
We chose the putative endolysin sequences of bacteriophage AP50 and bacteriophage B4 because bacteriophage AP50 is a B. anthracis bacteriophage27, and bacteriophage B4 is a B. cereus bacteriophage28,29 based on several criteria. The putative endolysin sequences of bacteriophage AP50 and bacteriophage B4 have low similarity with other endolysin sequences reported to have the anti-B. anthracis activity. In addition, the anti-B. anthracis activity of the phage endolysins of bacteriophage AP50 and bacteriophage B4 has not yet been reported. Using the genetic information available for bacteriophage AP50 (GenBank accession number EU408779) and bacteriophage B4 (GenBank accession number JN790865), the expression plasmids pBAD-AP50-31 and pBAD-B4 were constructed by inserting the genes encoding the endolysins of bacteriophage AP50 and bacteriophage B4, respectively, into pBAD::SAL-146. The nucleotide sequences used to construct pBAD-AP50-31 and pBAD-B4 are the sequences with the GenBank gene ID numbers 7018716 and 13828781, respectively. Oligonucleotides containing the genes encoding the endolysins of bacteriophages AP50 and B4 were prepared by chemical synthesis and inserted into the modified pBAD::SAL-1 plasmid by pre-incorporating an NcoI site at the translational start codon of pBAD::SAL-1 using the NcoI and NotI sites. The resulting plasmids were designated pBAD-AP50-31 and pBAD-B4, respectively, and were used as expression plasmids for the phage endolysins. E. coli BL21 cells were transformed with pBAD-AP50-31 and pBAD-B4, and the transformants were designated E. coli BL21-pBAD-AP50-31 and E. coli BL21-pBAD-B4, respectively. These cells were used as production hosts for the recombinant phage endolysins. The target phage endolysins were designated phage endolysin AP50-31 and phage endolysin LysB4.
Phylogenetic and bioinformatic analyses
To understand the evolutionary genetic relationship between our endolysins and other known Bacillus phage endolysins, we performed a phylogenic analysis of AP50-31 and LysB4 with other known Bacillus phage endolysins. First, sequences of 79 known Bacillus phage endolysins were retrieved from NCBI database. Second, we compared sequences of the retrieved Bacillus phage endolysins with our endolysins, and from this group of 79, we selected sequences of 23 known Bacillus phage endolysins to be used in subsequent multiple amino acid sequence alignments. We used two criteria for selecting which Bacillus phage endolysins to use in subsequent multiple sequence alignments. The first criterion was to find homologs which shared greater than 70% of the queried coverage in their amino acid sequences as listed in a BLASTP search of the NCBI protein sequence database (http://blast.ncbi.nlm.nih.gov/Blast.cgi). For the second criterion, we ensured that the searched homologs contained at least one catalytic or cell wall binding domain similar to those of endolysins AP50-31 and LysB4. Then, multiple sequence alignments with the selected homologs including our endolysins were carried out by the BLOSUM weight matrix of the ClustalW program47. Finally, the resultant file was subjected to phylogenic analysis using the MEGA 6.0 program (http://www.megasoftware.net/). The phylogenetic tree was constructed using the Maximum likelihood method with Jones-Taylor-Thornton model and 1,000 bootstrap replicates. Several characteristics of the putative phage endolysins and phage endolysins AP50-31 and LysB4 (molecular mass, pI, signal peptides, and transmembrane domains) were predicted by the proteomic tools available at ExPaSy (http://us.expasy.org).
Expression and purification of recombinant AP50-31 and recombinant LysB4
E. coli BL21-pBAD-AP50-31 was grown at 37 °C in a 10 L-fermenter jar containing 5 L of Luria–Bertani (LB) medium (5 g/L yeast extract, 10 g/L tryptone, and 10 g/L NaCl) supplemented with 50 μg/mL of kanamycin with agitation at 200 rpm and aeration of 5 L/min. Recombinant AP50-31 expression was induced by the addition of arabinose (0.2%, final concentration) when the OD600 of the culture reached 0.5. Following 4 h of incubation at 30 °C, the cells were collected by centrifugation (6,000 × g for 10 min) and resuspended in lysis buffer (20 mM Tris-HCl, pH 7.5). The cells were disrupted by a conventional ultrasonic treatment for 15 min (3 s pulse with 3 s rest intervals between pulses). After debris removal by centrifugation (13,000 × g for 20 min at 4 °C), the supernatant was recovered and subjected to cation-exchange chromatography (SP Sepharose® HP column; GE Healthcare, Little Chalfont, UK). The recovered supernatant was loaded onto an SP Sepharose® HP column pre-equilibrated with buffer A (20 mM Tris-HCl, pH 7.5). The column was washed with 5 CV (column volume) of buffer A until the absorbance at 280 nm decreased to 0.05. Then, the bound AP50-31 was eluted with a linear gradient of 0 to 0.5 M NaCl in buffer B (20 mM Tris-HCl and 0.5 M NaCl, pH 7.5).
To express and purify the recombinant LysB4, the same method was used as that described above with two modifications: E. coli BL21-pBAD-B4 was used as the expression host, and the pH of the buffers used (lysis buffer, buffer A and buffer B) was 8.0.
Development of formulations
Adequate liquid formulations to stabilise AP50-31 and LysB4 during storage or handling were developed through preformulation matrix screening. During the preformulation matrix screening, the effects on the stability of the following formulation parameters were examined (after incubation under accelerated stability study conditions (40 °C for 16 h), under vigorous constant agitation for up to 4 h, and after 12 weeks of storage at −20 °C, 4 °C, and 25 °C): pH (pH 7 vs. 7.5 for AP50-31 and pH 6 vs. 7 for LysB4); buffer type (10 mM l-histidine vs. 10 mM sodium phosphate); surfactant (0.5% poloxamer 188, 0.1% polysorbate 20, or 0.1% polysorbate 80); and additive (0.1% l-cysteine, 5% sorbitol, 1% sucrose, 5% mannitol, or 140 mM NaCl). All of the formulation candidates were prepared by dialyzing the elution fraction containing the phage endolysin against each formulation candidate and subsequently concentrated to 1 mg/mL using Amicon® Ultra-4 10 K filters (Millipore, Billerica, MA, USA). The stability of AP50-31 and LysB4 in the formulation candidates was evaluated for their visual appearance, turbidity by absorbance at 600 nm, and three analytical assessments (SDS-PAGE, SEC-HPLC, and a biological activity assay). SEC-HPLC was performed with a BioSep™-SEC-S 2000 column (Phenomenex, Torrance, CA, USA). The mobile phase (10 mM Tris-HCl and 150 mM NaCl, pH 7.0) was applied at a flow rate of 1.0 mL/min. Next, 50 μL of each sample was injected, and the sample elution was monitored for 30 min by measuring the absorbance at 280 nm. The conventional turbidity reduction assay was used as the biological activity assay. Briefly, a 1 μg/mL dilution of phage endolysin was added to the B. cereus ATCC 4342 cell suspension (OD600 = 1.0). The phage endolysin dilutions were prepared using 10 mM phosphate-buffered saline (PBS; pH 7.2) solution. The time required to reach one-half of the starting absorbance (TOD50, equivalent to a one-half log drop in the initial concentration of viable bacteria) was determined by examining changes in the bacterial density (OD600) recorded every 0.5 min for 20 min.
Expression host bacteria deposition
E. coli BL21-pBAD-AP50-31 and E. coli BL21-pBAD-B4 were deposited in the Korean Collection for Type Cultures (KCTC; Jeongeup, Republic of Korea). The deposition numbers for E. coli BL21-pBAD-AP50-31 and E. coli BL21-pBAD-B4 are KCTC 12708BP and KCTC 12709BP, respectively.
In vitro bacteriolytic activity test against Bacillus strains
The in vitro bacteriolytic activity test was performed against strains belonging to the Bacillus genus by a conventional turbidity reduction assay under the same conditions described above except for the final phage endolysin concentration (5 μg/mL). When the TOD50 could not be determined within 20 min, the endolysins were added in large amounts at a final concentration of 300 μg/mL. If the TOD50 could be determined at a final concentration of 300 μg/mL, this strain was marked as ND (not determined) because it is susceptible, but the exact TOD50 value could not be determined (≤300 μg/mL; >5 μg/mL). If not, it was marked as NS (not susceptible). The non-anthracis Bacillus bacterial strains tested are shown in Table 1.
In vitro bacteriolytic activity test against B. anthracis
In vitro bacteriolytic activity tests were performed against four B. anthracis strains (B. anthracis ΔSterne, B. anthracis Sterne, B. anthracis ATCC 14578, and B. anthracis HYU01). Strains of B. anthracis were grown on LB agar plates at 35 °C overnight. The next day, a single colony from each plate was inoculated into 20 mL brain heart infusion (BHI) medium in a 50-mL CELLSTAR® CELLreactor™ tube (Greiner Bio-One, Austria) and incubated at 35 °C with shaking (200 rpm) for 6 h. Then, 200 μL of the culture broth was transferred to 20 mL BHI medium in a 50-mL CELLSTAR® CELLreactor™ tube for overnight incubation at 35 °C with shaking (200 rpm). The next day, 100~200 μL of the culture broth was transferred to 20 mL BHI medium in a 50-mL CELLSTAR® CELLreactor™ tube until the culture reached the exponential growth phase. Then, the culture broth was harvested by centrifugation at 3,000 × g and 4 °C. The cell pellet was washed three times with ice-cold PBS solution. Then, the cell pellet was resuspended in ice-cold PBS solution to an OD600 of 1.0. The endolysins were added at a final concentration of 5 μg/mL, and the change of OD600 was monitored at 30 s intervals for 20 min to determine the TOD50. All tests using B. anthracis were approved by the institutional biosafety committee and conducted in a biosafety level 3 laboratory following the regulations of the Republic of Korea.
In vivo efficacy test of endolysin LysB4 against B. anthracis
Six-week-old female A/J mice were purchased from Japan SLC Inc. (Shizuoka, Japan) and used in this experiment after 7 days of acclimation. All of the mice were maintained in the experimental facility with unrestricted access to a rodent diet and water. All animal care and experiments were approved by the Institutional Animal Care and Use Committee of the Agency for Defense Development and performed according to the relevant regulations and guidelines issued by the Republic of Korea. The intranasal infection model was used to test the in vivo efficacy of endolysin LysB4 against B. anthracis. Briefly, the mice were anaesthetised by the intraperitoneal injection of 90 mg/kg ketamine (Yuhan Co., Seoul, Republic of Korea) and 10 mg/kg xylazine (Bayer Korea, Seoul, Republic of Korea), and 25 μL of spore suspension (1 × 107 CFU/mL) was inoculated intranasally (G1-G5). The inoculated dose was approximately four times the 50% lethal dose that had been reported previously48. To check the survival rate, clinical signs, and body temperature change, the mice were randomly assigned to three groups (G1–G3, n = 8). At 6, 24, and 48 h post-infection, the animals were anaesthetized, and 25 μL buffer (G1) or endolysin LysB4 (G2: low dose group, 10 μg/head; G3: high dose group, 100 μg/head) were instilled intranasally. The survival rate and clinical signs of each experimental group were monitored every 24 h up to 14 days post-infection, and the body temperature was measured every 24 h up to 7 days. To compare the bacterial count in tissues between the buffer- and endolysin-treated groups, the animals were randomly allocated and intranasally treated with buffer (G4) or endolysin LysB4 (G5, 100 μg/head) at 6, 24, and 48 h post-infection (8 mice per group). Three days after the bacterial challenge, the mice were euthanized, and the lungs, livers, spleens, and kidneys were collected in sterile PBS solution to count the bacteria. Each tissue sample was weighed, homogenised, and serially diluted, and 100 μL of each homogenate dilution was plated onto tryptic soy agar plates. The number of bacteria (CFU/g tissue) was calculated followed by the overnight culture of plates at 37 °C. For histopathological observations, parts of the lungs, livers, spleens, and kidneys were placed in 10% neutral buffered formalin, processed, and embedded in paraffin. Then, 3-μm-thick sections were prepared. After haematoxylin and eosin staining, the prepared tissue sections were examined under light microscopy. Tissues from non-infected and non-treated control mice were also prepared to compare the histopathological findings.
Statistical analysis
All statistical calculations were performed using Prism (GraphPad, La Jolla, CA, USA). The results of survival rates and tissue bacterial loads were analysed by the Mantel–Cox test and 2-way analysis of variance, respectively (*P < 0.05; **P < 0.01; ***P < 0.001).
Data availability
The data that supports the findings of this study are available in the article and the supplementary information or from the corresponding authors on request.
References
Ortatatli, M. et al. Antimicrobial susceptibility and molecular subtyping of 55 Turkish Bacillus anthracis strains using 25-loci multiple-locus VNTR analysis. Comp Immunol Microbiol Infect Dis 35, 355–361 (2012).
Coker, P. R., Smith, K. L. & Hugh-Jones, M. E. Antimicrobial susceptibilities of diverse Bacillus anthracis isolates. Antimicrob Agents Chemother 46, 3843–3845 (2002).
Choe, C. H., Bouhaouala, S. S., Brook, I., Elliot, T. B. & Knudson, G. B. In vitro development of resistance to ofloxacin and doxycycline in Bacillus anthracis Sterne. Antimicrob Agents Chemother 44, 1766 (2000).
Brook, I. et al. In vitro resistance of Bacillus anthracis Sterne to doxycycline, macrolides and quinolones. Int J Antimicrob Agents 18, 559–562 (2001).
Price, L. B. et al. In vitro selection and characterization of Bacillus anthracis mutants with high-level resistance to ciprofloxacin. Antimicrob Agents Chemother 47, 2362–2365 (2003).
Alibek, K. & Handelman, S. Biohazard: the chilling true story of the largest covert biological weapons program in the world, told from the inside by the man who ran it (1st ed.) (Random House New York. 1999).
Inglesby, T. V. et al. Anthrax as a biological weapon, 2002: updated recommendations for management. Jama 287, 2236–2252 (2002).
Bouzianas, D. G. Current and future medical approaches to combat the anthrax threat. J Med Chem 53, 4305–4331 (2010).
Enserink, M. Bioterrorism. Researchers question obsession with Cipro. Science 294, 759–761 (2001).
Huang, E. et al. Antitoxin treatment of inhalation anthrax: a systematic review. Health Secur 13, 365–377 (2015).
Schuch, R., Nelson, D. & Fischetti, V. A. A bacteriolytic agent that detects and kills Bacillus anthracis. Nature 418, 884–889 (2002).
Yoong, P., Schuch, R., Nelson, D. & Fischetti, V. A. PlyPH, a bacteriolytic enzyme with a broad pH range of activity and lytic action against Bacillus anthracis. J Bacteriol 188, 2711–2714 (2006).
Loessner, M. J. Bacteriophage endolysins-current state of research and applications. Curr Opin Microbiol 8, 480–487 (2005).
Loessner, M. J., Schneider, A. & Scherer, S. A new procedure for efficient recovery of DNA, RNA, and proteins from Listeria cells by rapid lysis with a recombinant bacteriophage endolysin. Appl Environ Microbiol 61, 1150–1152 (1995).
Fischetti, V. A. Bacteriophage endolysins: a novel anti-infective to control Gram-positive pathogens. Int J Med Microbiol 300, 357–362 (2010).
Jado, I. et al. Phage lytic enzymes as therapy for antibiotic-resistant Streptococcus pneumoniae infection in a murine sepsis model. J Antimicrob Chemother 52, 967–973 (2003).
O’Flaherty, S., Coffey, A., Meaney, W., Fitzgerald, G. F. & Ross, R. P. The recombinant phage lysin LysK has a broad spectrum of lytic activity against clinically relevant staphylococci, including methicillin-resistant Staphylococcus aureus. J Bacteriol 187, 7161–7164 (2005).
Mayer, M. J., Narbad, A. & Gasson, M. J. Molecular characterization of a Clostridium difficile bacteriophage and its cloned biologically active endolysin. J Bacteriol 190, 6734–6740 (2008).
Entenza, J. M., Loeffler, J. M., Grandgirard, D., Fischetti, V. A. & Moreillon, P. Therapeutic effects of bacteriophage Cpl-1 lysin against Streptococcus pneumoniae endocarditis in rats. Antimicrob Agents Chemother 49, 4789–4792 (2005).
Nelson, D., Loomis, L. & Fischetti, V. A. Prevention and elimination of upper respiratory colonization of mice by group A streptococci by using a bacteriophage lytic enzyme. Proc Natl Acad Sci USA 98, 4107–4112 (2001).
Loeffler, J. M., Djurkovic, S. & Fischetti, V. A. Phage lytic enzyme Cpl-1 as a novel antimicrobial for pneumococcal bacteremia. Infect Immun 71, 6199–6204 (2003).
McCullers, J. A., Karlstrom, A., Iverson, A. R., Loeffler, J. M. & Fischetti, V. A. Novel strategy to prevent otitis media caused by colonizing Streptococcus pneumoniae. PLoS Pathog 3, e28 (2007).
Loeffler, J. M., Nelson, D. & Fischetti, V. A. Rapid killing of Streptococcus pneumoniae with a bacteriophage cell wall hydrolase. Science 294, 2170–2172 (2001).
Cheng, Q., Nelson, D., Zhu, S. & Fischetti, V. A. Removal of group B streptococci colonizing the vagina and oropharynx of mice with a bacteriophage lytic enzyme. Antimicrob Agents Chemother 49, 111–117 (2005).
Rashel, M. et al. Efficient elimination of multidrug-resistant Staphylococcus aureus by cloned lysin derived from bacteriophage phi MR11. J Infect Dis 196, 1237–1247 (2007).
Fenton, M., Ross, P., McAuliffe, O., O’Mahony, J. & Coffey, A. Recombinant bacteriophage lysins as antibacterials. Bioeng Bugs 1, 9–16 (2010).
Sozhamannan, S. et al. Molecular characterization of a variant of Bacillus anthracis-specific phage AP50 with improved bacteriolytic activity. Appl Environ Microbiol 74, 6792–6796 (2008).
Son, B. et al. Characterization of LysB4, an endolysin from the Bacillus cereus-infecting bacteriophage B4. BMC Microbiol 12, 33 (2012).
Lee, J. H., Shin, H., Son, B., Heu, S. & Ryu, S. Characterization and complete genome sequence of a virulent bacteriophage B4 infecting food-borne pathogenic Bacillus cereus. Arch Virol 158, 2101–2108 (2013).
Petersen, T. N., Brunak, S., von Heijne, G. & Nielsen, H. SignalP 4.0: discriminating signal peptides from transmembrane regions. Nat Methods 8, 785–786 (2011).
Sonnhammer, E. L., von Heijne, G. & Krogh, A. A hidden Markov model for predicting transmembrane helices in protein sequences. Proc Int Conf Intell Syst Mol Biol 6, 175–182 (1998).
Maroun, J. W., Whitcher, K. J., Chamakura, K. R. & Kuty Everett, G. F. Complete genome of Bacillus thuringiensis myophage spock. Genome Announc 1, e00863–13 (2013).
Sauder, A. B. et al. Genomic characterization and comparison of seven Myoviridae bacteriophage infecting Bacillus thuringiensis. Virology 489, 243–251 (2016).
Erill, I. & Caruso, S. M. Genome sequences of two Bacillus cereus group bacteriophages, Eyuki and AvesoBmore. Genome Announc 3, e01199–15 (2015).
Mock, M. & Fouet, A. Anthrax. Annu Rev Microbiol 55, 647–671 (2001).
Fenton, M. et al. The truncated phage lysin CHAP(k) eliminates Staphylococcus aureus in the nares of mice. Bioeng Bugs 1, 404–407 (2010).
Goel, A. K. Anthrax: A disease of biowarfare and public health importance. World J Clin Cases 3, 20–33 (2015).
Lyons, C. R. et al. Murine model of pulmonary anthrax: kinetics of dissemination, histopathology, and mouse strain susceptibility. Infection and immunity 72, 4801–4809 (2004).
Loving, C. L., Kennett, M., Lee, G. M., Grippe, V. K. & Merkel, T. J. Murine aerosol challenge model of anthrax. Infection and immunity 75, 2689–2698 (2007).
Loving, C. L. et al. Role of anthrax toxins in dissemination, disease progression, and induction of protective adaptive immunity in the mouse aerosol challenge model. Infection and immunity 77, 255–265 (2009).
Welkos, S., Bozue, J., Twenhafel, N. & Cote, C. Animal models for the pathogenesis, treatment, and prevention of infection by Bacillus anthracis. Microbiol Spectr 3, TBS-0001–2012 (2015).
Loving, C. L., Kennett, M., Lee, G. M., Grippe, V. K. & Merkel, T. J. Murine aerosol challenge model of anthrax. Infect Immun 75, 2689–2698 (2007).
Helgason, E. et al. Bacillus anthracis, Bacillus cereus, and Bacillus thuringiensis-one species on the basis of genetic evidence. Appl Environ Microbiol 66, 2627–2630 (2000).
Fujinami, Y., Hosokawa-Muto, J. & Mizuno, N. Evaluation of tools for environmental sampling of Bacillus anthracis spores. Forensic Sci Int 257, 376–378 (2015).
Tufts, J. A., Calfee, M. W., Lee, S. D. & Ryan, S. P. Bacillus thuringiensis as a surrogate for Bacillus anthracis in aerosol research. World J Microbiol Biotechnol 30, 1453–1461 (2014).
Jun, S. Y. et al. Antibacterial properties of a pre-formulated recombinant phage endolysin, SAL-1. Int J Antimicrob Agents 41, 156–161 (2013).
Larkin, M. A. et al. Clustal W and Clustal X version 2.0. Bioinformatics 23, 2947–2948 (2007).
Wilson, M. K. et al. Bacillus cereus G9241 makes anthrax toxin and capsule like highly virulent B. anthracis Ames but behaves like attenuated toxigenic nonencapsulated B. anthracis Sterne in rabbits and mice. Infect Immun 79, 3012–3019 (2011).
Kim, S. K. et al. Complete genome sequence of Bacillus anthracis HYU01, isolated from soil samples in the Korean peninsula. Genome Announc 2, e00769–14 (2014).
Acknowledgements
This study was supported by the Military Biodefense Research Laboratory Program (911073202) funded by Agency for Defense Development.
Author information
Authors and Affiliations
Contributions
S.H.K. and S.T.J. conceived the project. S.P., C.H.K., S.Y.J., G.M.J., J.S.S., S.T.J., S.J.Y., S.Y.L. and S.H.K. performed the experiments and analysed the data. S.Y.J., G.M.J. and J.S.S. contributed to the construction of the expression hosts, expression and purification of the recombinant phage endolysins, the preformulation study, and the in vitro efficacy tests with non-anthracis Bacillus strains. J.S.S. and S.J.Y. contributed to selecting of the target phage endolysin sequences, and the bioinformatics and phylogenetic analyses. S.P. and C.H.K. contributed by conducting the in vitro and in vivo efficacy tests with B. anthracis. S.H.K. and S.Y.L. supervised the experimental analysis. S.P., C.H.K., S.Y.J., S.H.K. and S.Y.L. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, S., Jun, S.Y., Kim, CH. et al. Characterisation of the antibacterial properties of the recombinant phage endolysins AP50-31 and LysB4 as potent bactericidal agents against Bacillus anthracis . Sci Rep 8, 18 (2018). https://doi.org/10.1038/s41598-017-18535-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-18535-z
This article is cited by
-
New bacteriophage-derived lysins, LysJ and LysF, with the potential to control Bacillus anthracis
Applied Microbiology and Biotechnology (2024)
-
Knockdown of ELF4 aggravates renal injury in ischemia/reperfusion mice through promotion of pyroptosis, inflammation, oxidative stress, and endoplasmic reticulum stress
BMC Molecular and Cell Biology (2023)
-
Antitumor Activity of Taxol Engross Taxol-Caveolin-1 Interaction via Lipid Raft Structure—“Caveolae”
Applied Biochemistry and Biotechnology (2023)
-
Which cell death modality wins the contest for photodynamic therapy of cancer?
Cell Death & Disease (2022)
-
Alternative Treatment Strategies for Secondary Bacterial and Fungal Infections Associated with COVID-19
Infectious Diseases and Therapy (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.