Abstract
The HOXB13 G84E variant is associated with risk of prostate cancer (PCa), however the role this variant plays in PCa development is unknown. This study examined 751 cases, 450 relatives and 355 controls to determine the contribution of this variant to PCa risk in Tasmania and investigated HOXB13 gene and protein expression in tumours from nine G84E heterozygote variant and 13 wild-type carriers. Quantitative PCR and immunohistochemistry showed that HOXB13 gene and protein expression did not differ between tumour samples from variant and wild-type carriers. Allele-specific transcription revealed that two of seven G84E carriers transcribed both the variant and wild-type allele, while five carriers transcribed the wild-type allele. Methylation of surrounding CpG sites was lower in the variant compared to the wild-type allele, however overall methylation across the region was very low. Notably, tumour characteristics were less aggressive in the two variant carriers that transcribed the variant allele compared to the five that did not. This study has shown that HOXB13 expression does not differ between tumour tissue of G84E variant carriers and non-carriers. Intriguingly, the G84E variant allele was rarely transcribed in carriers, suggesting that HOXB13 expression may be driven by the wild-type allele in the majority of carriers.
Similar content being viewed by others
Introduction
Family history is a widely recognised risk factor for prostate cancer (PCa) with an estimated heritability of 58%, the highest of any cancer1,2. While approximately 33% of familial risk is explained by common, low penetrance variants, a study by Mancuso and colleagues estimates that as much as 42% of ‘missing’ heritability is likely to be explained by rare variants3,4. Several recent studies have applied next-generation sequencing (NGS) technologies to familial PCa datasets with the aim of identifying rare disease-causing variants5,6,7. In particular, a targeted NGS study of 94 familial PCa probands, with evidence of linkage to chr17q21, identified a rare non-synonymous mutation in HOXB13 (G84E; rs138213197)5. Ewing and colleagues observed that the case carrier frequency was higher in a familial cohort, 4.7% (OR 68.1, p = 0.001), compared to a population cohort, 1.4% (OR 20.1, p < 0.001)5. Several studies have since replicated this finding in Caucasian familial and case-control populations and estimate the variant to be associated with a 4- to 8-fold increase in PCa risk, as well as with early-onset disease8,9,10,11,12,13,14.
In the normal prostate, the highly expressed HOXB13 transcription factor plays a key role in prostate development15. Notably, HOXB13 has been shown to interact with the androgen receptor (AR), a protein essential for prostate development and required for all stages of PCa growth16. Norris and colleagues (2009) demonstrated that HOXB13 acts as both a repressor and coactivator of AR target genes; in target genes with an androgen-response element (ARE) the HOXB13:AR complex inhibits transcription, but in genes with a HOX element, the complex enhances transcription16. HOXB13 has been reported to function as a growth promoter and growth suppressor in prostate cancer models, depending on factors such as tumour androgen sensitivity status and cellular localisation of the protein (reviewed in17). Therefore, the role of HOXB13 in prostate tumour development remains unclear and the mechanism by which the HOXB13 gene and, specifically, the G84E variant promotes prostate carcinogenesis, is largely unknown. Further analyses are required to determine whether the G84E variant causes a gain or loss of gene function, or increases PCa risk through other mechanisms.
The objective of this study was to investigate the functionality of the HOXB13 G84E variant by examining transcription, translation, and possible epigenetic modification of the gene, in archival prostate tumour specimens obtained from several variant carrier and non-carrier cases identified in a Tasmanian familial PCa cohort.
Results
Identification of the HOXB13 G84E variant in a Tasmanian PCa cohort
The G84E HOXB13 variant was identified in existing whole-genome sequencing data obtained from a case and his daughter from a Tasmanian PCa family (Fig. 1; PcTas72–2, and PcTas72–97). Subsequent genotyping of all available PcTas72 family members (n = 61) confirmed the two carriers and identified a further five heterozygous carriers of the G84E variant, including three cases and two female relatives. Figure 1 shows segregation of the variant in cases from two branches of PcTas72 but not the third, underscoring the heterogeneity of this cancer, even within a single family.
Segregation of the G84E variant in the familial prostate cancer pedigree, PcTas72. The G84E variant (+) was originally identified in individuals PcTas72–2 and PcTas72–97 using existing WGS data, with an additional five carriers identified in subsequent genotyping. Squares indicate males and circles females, with a slash indicating the subject is deceased. Individual identification numbers and age at diagnosis of cases are shown under each symbol. An arrow indicates a tumour specimen was obtained.
Association between PCa risk and the HOXB13 G84E variant in the Tasmanian population
To assess the contribution of the G84E variant to PCa in the Tasmanian population, all individuals from the familial (n = 699) and case-control (n = 850) PCa cohorts were genotyped. A further 12 variant carriers were identified; six in five additional PcTas families (Supplementary Table 1), and four in the case-control cohort (three sporadic cases and one control). We also examined tumour tissue derived from pathology specimens for seven cases from the six variant carrier families, where germline DNA from blood or saliva was not available, and identified a further five carriers from two families (Supplementary Table 1). MQLS analysis18 of the combined familial and case-control genotyping data demonstrated a significant association between PCa risk and the G84E variant in the Tasmanian population (OR = 6.59; p = 4.2 × 10−5) (Table 1). For the familial cases, the age at diagnosis and tumour grade of carriers in the six PcTas families were similar to non-carriers in these same families.
The effect of the G84E variant on HOXB13 gene expression
FFPE pathology blocks were obtained for 22 PcTas cases, 11 of which had G84E carrier status determined from a germline DNA sample (Table 2). Genotyping of prostate tissue DNA from the 22 blocks confirmed four and identified five additional heterozygous G84E carriers, including a case whose germline DNA was genotyped as wildtype (PcTas22–203; Table 2). Repeat genotyping of PcTas22–203 germline and re-extracted tumour DNA samples confirmed the discordant result. First-degree relatives of this individual were genotyped as G84E wildtype. No additional samples were available for this individual (deceased), therefore this anomaly could not be resolved to determine whether a pathology sample mix-up had occurred, mosaicism was present in the individual or the variant arose somatically. To investigate HOXB13 gene expression, RNA was extracted from both adjacent benign and malignant cells for 10 cases. Due to the restricted availability of tissue, RNA was extracted from only benign cells for four cases, only malignant cells for four cases, and a mixed cell population for one case (Supplementary Table 2). HOXB13 expression was initially investigated in the ten paired malignant-benign samples, where we observed significantly higher expression in malignant compared to benign cells (1.5-fold increase; p = 0.01; Fig. 2A). However, when HOXB13 expression was compared between the malignant cells of G84E variant carriers (n = 6) and non-carriers (n = 8), there was no significant difference between the two (p = 0.21; Fig. 2B). There was also no detectable difference in HOXB13 gene expression between the benign cells of variant carriers (n = 4) and non-carriers (n = 10; p = 0.29).
HOXB13 gene expression analysis in FFPE prostate tumours. (A) A 1.5-fold increase in HOXB13 expression was observed in malignant (n = 10) compared to benign cells (n = 10; p = 0.01). (B) No significant difference in HOXB13 expression was observed between the tumour cells of variant carriers (n = 6) and non-carriers (n = 8; p = 0.21).
We next examined whether the variant transcript was detectable in the tumour tissue of seven G84E carriers. Next-generation sequencing applied to cDNA from freshly cut FFPE sections indicated that only two of seven variant carriers (28.6%) showed evidence of variant allele transcription (Supplementary Table 2). The variant transcript was detectable in both malignant and benign cells in one individual and in benign cells only in the second individual.
To determine whether imbalanced allele transcription was related to HOXB13 G84E carrier status, allele-specific transcription was determined for another variant in relatively close proximity to the G84E variant. The HOXB13 variant, rs9900627 (MAF 11.2%), is 262 bp centromeric to G84E in exon 1, and one heterozygous carrier of this variant was identified in our tissue cohort (PcTas11–11; G84E negative). Unlike carriers of G84E, the variant and wild-type alleles of rs9900627 were detectable in equal proportions in PcTas11–11.
The effect of the G84E variant on HOXB13 protein expression
Immunohistochemistry was undertaken on all 22 FFPE pathology samples to determine whether protein expression differed between malignant and benign prostate tissue, and between HOXB13 variant and non-variant carriers. HOXB13 staining ranged from weak to strong across the dataset (Fig. 3; Supplementary Table 2). Analyses of the quasi-continuous nuclear scores from 16 samples with paired malignant and benign cells did not reveal any significant difference in HOXB13 protein expression between malignant and benign cells (p = 0.45). Analysis of malignant cells from G84E variant carriers (n = 9) versus non-carriers (n = 9) also indicated no significant difference between the two groups (p = 0.68). A similar result was observed for benign cells (p = 0.84).
HOXB13 protein expression in G84E non-carriers (A and B) and carriers (C and D). Immunohistochemistry staining intensity of HOXB13 was not consistent with G84E carrier status (A and C) weak staining; (B and D) strong staining). HOXB13 was predominantly expressed in the nuclei of prostate gland cells, while cytoplasmic cells were often negative or only weakly positive for the protein. Images were taken on a Leica 2500 microscope (x200) using the Lieca Application Suite V3.
Methylation of HOXB13 CpG islands
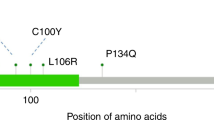
We next examined DNA methylation in tumour samples at two HOXB13 CpG islands, one spanning the promoter region and exon 1 of the gene, and the second located ~4.5 kb upstream of the HOXB13 transcription start site (Supplementary Figure 1). Allele-specific methylation was also examined at nine CpG sites within the promoter/exon 1 CpG island and surrounding the G4E variant, to determine if differential methylation explained the observed unbalanced allele transcription. Very low levels of DNA methylation were observed across both CpG islands in both variant (n = 3) and non-variant carriers (n = 3; Supplementary Figure 2). Allele-specific methylation was consistently low across all nine CpG sites within the promoter/exon 1 CpG island in both variant carriers (n = 7) and non-carriers (n = 7); however, methylation of the variant allele was lower than that of the wild-type allele in all instances (Fig. 4). Significant differences in CpG site-specific methylation between the variant allele and wild-type alleles of carriers and/or non-carriers was observed at three CpG sites (p < 0.05; Fig. 4), while no difference was observed between the wild-type alleles of carriers and non-carriers. No correlation between methylation and transcription of the variant allele, or absolute gene expression of HOXB13 was observed (data not shown).
Average methylation (%) across nine CpG sites located within a CpG island surrounding the G84E variant. Average methylation for both carriers and non-carriers was low across all CpG sites. The variant allele was less methylated at all sites (solid black line) when compared to the wild-type allele of both variant carriers (grey solid line) and non-carriers (dotted line). The difference in methylation was statistically significant between all alleles at CpG site 5, and between the variant allele and the non-carrier wildtype allele at CpG sites 6 and 9 (*p < 0.05, **p < 0.001).
Discussion
The HOXB13 G84E variant is a PCa risk variant reported to be of particular relevance to early onset familial disease5,19,20. Here, a Tasmanian PCa family was shown to be segregating the HOXB13 variant, which was subsequently demonstrated to be significantly associated with PCa risk in the Tasmanian population (OR = 6.59). While the HOXB13 gene is known to play a key role in prostate development15 and to interact with the AR to influence transciption16, little is known about how the HOXB13 G84E variant causes increased PCa risk.
A computational modeling study by Chandrasekaran et al. (2017) has suggested that the G84E variant increases HOXB13 protein stability21, which may in turn cause increased transcription of downstream target genes promoting cell proliferation and invasion22. However, in an in vitro cell model study using site directed mutatgenesis, Cardoso and colleagues (2016) found that the G84E variant had no phenotypic impact, i.e. there was no change in proliferation or apoptosis compared to the wild-type cell model23. In our study of FFPE prostate tumour tissue, we found no difference in HOXB13 protein expression between G84E carriers and non-carriers; a finding supported by a larger IHC study of radical prostatectomy samples from 101 G84E carriers and 99 non-carriers24. Furthermore, we demonstated that gene expression was comparable between carriers and non-carriers. Although tumour tissue samples from carriers were demonstrated to be heterozygous for the G84E variant, the variant allele transcript was rarely detectable in G84E carrier prostate tissue (benign or malignant). In fact, the variant allele was only detectable in two of seven carriers and at lower levels than the wild-type allele. To further examine HOXB13 allelic expression, transcription of another HOXB13 variant (rs9900627) in close proximity to G84E was examined. Comparable transcription of both the wild-type and variant rs9900627 alleles was evident in the tumour tissue of a non-G84E carrier. We therefore hypothesize that the unbalanced allele transcription may be related to the presence of the G84E variant. Unbalanced allele transcription has been reported previously in a study of breast cancer patients25. Benz et al. (2006) investigated the common ERBB2 variant, G1170C, in ERBB2-positive and ERBB2-negative breast cancer patients and found that ERBB2-positive germline heterozygotes had markedly skewed tumour genotype frequencies to homozygosity of either allele and monoallelic transcript amplification25. While this was not unexpected given previous research26,27, when the tumours of ERBB2-negative germline heterozygotes were examined, Benz et al. found that although tumour genotyping supported the heterozygous state, similar to our study, 70% of tumours showed preferential transcription of one allele, or unbalanced allele transcription. The authors suggested the unbalanced allele transcription in ERBB2-negative tumours may be due to epigenetic mechanisms, whereby methylation silences a particular allele.
Two CpG islands are located within or near the HOXB13 gene: the first spans the promoter and exon 1 region of the gene and the second is ~4.5 kb upstream of the HOXB13 transcription start site28. In a study of colorectal cancer, Ghoshal and colleagues (2010) found very little methylation in the promoter/exon 1 CpG island in both tumour and normal cell lines, whilst the upstream CpG island was significantly more methylated in tumour compared to normal cell lines28. Furthermore, they found that hypermethylation of the upstream CpG island partially supressed HOXB13 expression and speculate that this region may function as an enhancer. In our study, we observed very low levels of DNA methylation at both CpG islands in all tumour samples tested (G84E carriers and non-carriers). When we looked further at allele-specific methylation of nine CpG sites surrounding the G84E variant in exon 1, although methylation was lower at three CpG sites on the variant allele, the overall level of methylation across this region was again so low that the biological impact this would have on gene transcription is questionable. It therefore seems unlikely that methylation differences explain the unbalanced allele transcription we observe in the G84E carriers. Alternatively, copy number variation at the HOXB13 site or rapid targeted degradation of the variant mRNA transcript may underpin the observed allelic imbalance and warrants further investigation.
Interestingly, while the numbers were too small for formal analyses, examination of clinical characteristics revealed that HOXB13 G84E variant carriers that transcribed the variant allele (PcTas12–3 and PcTas72–6) had lower tumour grades and Gleason scores (GS) than variant carriers that did not transcribe the variant allele. The tumours from both PcTas12–3 and PcTas72–6 were well- to moderately-differentiated with GS < 6, whereas where there was no evidence for variant allele transcription, the tumours were predominantly poorly differentiated with GS ≥ 7, with the exception of one sample (PcTas12–8; GS6). Due to insufficient tumour material, allele-specific transcription was not able to be determined for two variant carriers, PcTas22–637 and PcTas72–154, who had a poorly differentiated and well differentiated tumour grade respectively. Several previous studies have investigated possible associations between G84E and clinicopathological factors, and the majority have found no association between carrier status and GS5,11,29,30. However, two studies have presented contrary results. A Danish study of 995 patients (25 carriers) found G84E carrier status was significantly associated with GS ≥ 7 versus GS < 731, whilst another study of 1,457 patients (18 carriers) observed that the G84E variant was more strongly associated with GS ≥ 7(4 + 3) disease but this was not significantly different to the association with GS ≤ 7(3 + 4) disease13. While it has to again be noted that our observations are based on limited numbers, these conflicting results may be due to the underlying variability in variant allele transcription that we have observed and this should be explored in a larger HOXB13 G84E tumour dataset.
This study has provided important insights into the effect the HOXB13 variant has on gene transcription in prostate tumour tissue but there are some limitations in the interpretation of data. Due to the rarity of the variant and the limited availability of informative tumour tissue specimens, the number of samples available for G84E variant carriers was restricted. The quality of DNA and RNA extracted from FFPE tissues is also fairly poor, therefore it is important that our findings are validated in larger FFPE cohorts or, if available, fresh frozen samples. In our IHC experiment, the antibody used was not specific to the variant form of the HOXB13 protein and it would be valuable to verify our gene expression results with a variant-specific protein antibody.
In summary, this study has demonstrated that HOXB13 gene and protein expression do not differ in the tumours of G84E carriers and non-carriers. We have also demonstrated that in our tumour population, only a minority of variant carriers transcribe the G84E variant allele but the mechanism behind this unbalanced allele transcription is still unknown. Furthermore, we observed that clinicopathological features tended to be less aggressive in the tumours of carriers that did transcribe the variant allele. It is important that these findings are validated in a larger tissue cohort of HOXB13 G84E carriers.
Methods
Study Resource
Tasmanian Prostate Cancer Familial Cohort
This cohort is comprised of a rare collection of 52 PCa families from the founder population of Tasmania. The number of affected men in these families range from five to over 140, and include up to five affected brothers and multiple father/son and uncle/nephew pairs. DNA samples from blood and saliva have been collected for 249 affected men and 450 male and female relatives. Archived prostate tissue pathology blocks from HOXB13 G84E variant carriers and a random selection of non-carriers were targeted for collection from pathology labs. Sectioned FFPE pathology blocks were histologically reviewed by RM and SD to provide a contemporary grading of the tumours and to mark regions of malignant and benign cells.
Tasmanian Case-Control Cohort
The Tasmanian Case-Control Prostate Cancer Study is a population-based cohort, which includes blood or saliva samples from 495 cases and 355 controls. Cases were identified from the Tasmanian Cancer Registry (TCR) and considered eligible for this study if they were diagnosed under the age of 75 between the years 1996 and 2005. Controls were selected at random from the Tasmanian electoral roll and frequency matched by five year age groups to the cases. Controls are periodically checked against the TCR for PCa diagnosis.
Ethics approval for both cohort studies was obtained from the Human Research Ethics Committee Tasmania, Australia (H9999 and H007740) and written informed consent was obtained from all participating individuals. For deceased familial cases, a waiver of consent was obtained to collect prostate tissue specimens.
Nucleic Acid Extractions
DNA was extracted from blood using the Nucleon BACC3 Kit (GE Healthcare) and from saliva using the Oragene DNA Kit (DNA Genotek) according to the manufacturers’ directions. FFPE tissue blocks were sectioned to 8 μm, dewaxed and rehydrated using a standard xylene-ethanol deparaffinisation protocol. Tumour and benign glands were marked on haematoxylin and eosin stained tissue sections by a pathologist (SD, RM). Marked tumour and benign regions were macro-dissected separately for both DNA and RNA. DNA was extracted using the QIAamp DNA FFPE Tissue Kit (QIAGEN) according to the manufacturer’s instructions and eluted in 50 μL of ATE Buffer. DNA was quantified using the Nanodrop® ND-1000 UV-vis spectrophotometer (Nanodrop® Technologies). RNA was extracted using the RecoverAll Total Nucleic Acid Isolation Kit (ThermoFisher Scientific) according to the manufacturer’s instructions and eluted in 30 μL of dH2O. RNA quality and quantity was assessed using the 2100 Bioanalzyer (Agilent). The SuperScriptTM VILOTM cDNA Synthesis Kit (Invitrogen) was used for cDNA conversion, as per the manufacturer’s instructions.
Next-Generation Sequencing Data
Existing whole-genome and whole-exome sequencing data was previously generated for several PcTas72 individuals (Fig. 1) at the Illumina Genome Network, USA, on the HiSeq 2500 s or the Kinghorn Centre for Clinical Genomics, Australia, on the Illumina HiSeq XTM Ten platform using the TruSeq Nano library preparation. Data had been analysed using the Variant Analysis of Sequenced Pedigrees (VASP) analytical pipeline, developed specifically to detect disease causing variants in sequenced pedigrees32,33. The presence of the HOXB13 G84E variant was examined in the annotated variant list generated using the Ensembl Variant Effect Predictor and overlapped with Ensembl canonical transcripts.
Sanger Sequencing
Sanger sequencing was performed to validate the WGS results in the original PcTas72 carriers, as well as determine the HOXB13 variant carrier status of deceased affected men who only had a tumour specimen available for genotyping. HOXB13 primers were designed using Primer3Plus34,35 (Supplementary Table 3) and PCR conditions are available on request.
Genotyping
A TaqMan SNP genotyping assay (Applied Biosystems) was used to genotype the HOXB13 G84E variant in the familial and case-control cohorts on the LightCycler® 480 system (Roche). Heterozygous individuals were confirmed by Sanger sequencing, as described above.
Real-Time qPCR Analysis
SYBR green real-time quantitative PCR (qPCR) assays were performed to determine gene expression of HOXB13 and two housekeeping genes, GAPDH and β-Actin. Amplification was performed on 50ng FFPE cDNA using published HOXB13, GAPDH and β-Actin primers (Integrated DNA Technologies; Supplementary Table 3)36,37. Standard curves were generated for HOXB13, GAPDH, and β-Actin to determine PCR efficiency and normalise absolute HOXB13 gene expression.
MiSeq cDNA Sequencing
Transcription of the wild-type and mutant alleles of HOXB13 were determined using the MiSeq platform (Illumina). A 157 bp region of HOXB13, covering the G84E mutation, was FFPE cDNA amplified and barcoded with unique forward and reverse tags (Supplementary Table 3). Barcoded DNA fragments were pooled, purified and libraries were sequenced on the Illumina MiSeq platform using the MiSeq® V2 300 Cycle Reagent Kit (Illumina).
FASTQ files were aligned to the hg19 reference genome using Galaxy version 16.04 (usegalaxy.org)38,39,40. The raw sequence data (FASTQ files) were converted to Sanger and Illumina 1.8+ format using the FASTQ Groomer tool, followed by realignment using BWA-MEM. The allele frequency at the variant position was visualised using IGV 2.3.6841. FastQC of BAM files was used to assess the quality of the raw sequence data.
Methylation Analysis
FFPE DNA (~200 ng) was bisulphite converted using the EZ DNA Methylation-GoldTM Kit (Zymo Research Corp). Two primer sets were designed to amplify fragments covering the HOXB13 promoter/exon 1 CpG island and a CpG island ~4.5 kb upstream of the transcription start site (Supplementary Figure 1; Supplementary Table 3). Fragments were purified using the QIAquick Gel Extraction Kit (Qiagen), as per the manufacturer’s instructions, and cloned in to the p-GEM®-T Easy Vector Kit (Promega Corporation), using a 3:1 ratio of insert to vector. Top10 competent cells (Invitrogen) were transformed with 2 µL of ligations. Ten white clones per sample were selected for amplification and DNA extraction, using the QIAprep Spin Miniprep Kit (Qiagen), as per the manufacturer’s instructions. Clone inserts were sequenced using the reverse Sp6 primer. Each clone CpG site was scored as either 1 (methylated) or 0 (non-methylated), and bubble maps were generated using the CpG Bubble Chart Generator, Version 20061209 Alpha, created by Mark A Miranda.
Allele-specific methylation involved the PCR amplification of a 175 bp region of HOXB13, including the G84E mutation and nine surrounding CpG sites, using bisulphite-converted FFPE DNA, as described above (Supplementary Figure 1; Supplementary Table 3). Products were barcoded with unique forward and reverse tags and sequenced on the Illumina MiSeq platform, as described above. FASTQ files were quality score checked and separated into reads containing the G84E variant allele or the wild-type allele. A beta value (β), the ratio of methylated versus non-methylated reads, was determined for all of the nine CpG sites.
Immunohistochemistry
Tissue sections (3.5 μm) were pre-treated with Target Retrieval Solution (Dako), followed by inactivation of endogenous peroxidases using 3% hydrogen peroxidase (Sigma-Aldrich). Non-specific staining was blocked using Protein Block (Dako). Sections were incubated with primary HOXB13 antibody (sc-28333; Santa Cruz Biotechnology; working dilution 1:50) in a humidified chamber for one hour, followed by 30 min incubation with an anti-mouse HRP-Labelled Polymer (Dako). HOXB13 protein staining was visualised with 3–3′ diaminobenzidine (DAB) for 10 min, and the sections were counterstained using Mayer’s haematoxylin. Normal prostate glands (Abcam), ascertained as HOXB13 wildtype by Sanger sequencing, were used as positive controls for the immunohistochemical reactions. Negative controls included primary antibody only, secondary antibody only, and a mouse IgG1 isotype control (Dako).
The immuno-stained sections were scored by a pathology registrar (RM) blinded to the HOXB13 carrier status. Nuclear staining was scored as none/weak, moderate or strong, depending on the most common staining intensity in the entire tissue section. Immunostaining was assessed using a quasi-continuous nuclear score, created by multiplying each intensity level (1 for no/weak stain, 2 for moderate stain, and 3 for intense stain) by the corresponding percentage of positive cells. As benign prostate tissue was also present in some sections, immunostaining was assessed for both tumour and benign cells separately.
Statistical Analyses
Association analyses
HOXB13 genotype data was analysed using MQLS 18, an association analysis that maximises power by performing tests of association in the combined familial and case-control datasets, while taking into account relatedness of individuals. MQLS uses variance components to examine the significance of association for related individuals, and when the disease status is known for first-degree relatives of cases, MQLS obtains more power by giving increased weighting to those individuals with closely related disease-carrying relatives.
Gene expression
The paired Student’s t-test was used to compare absolute HOXB13 gene copy numbers between tumour and adjacent benign cells. The unpaired Student’s t-test was used to compare absolute HOXB13 gene copy numbers in the tumour cells of G84E variant carriers versus non-carriers, and in the benign cells of G84E variant carriers versus non-carriers. P values < 0.05 were considered to be significant. Fold changes were also presented in box plot format using R version 3.4.0.
Protein expression
The paired Student’s t-test was used to compare HOXB13 protein expression between tumour and adjacent benign cells. Unpaired Student’s t-tests were used to compare HOXB13 protein expression in the tumour cells of G84E variant carriers versus non-carriers, and in the benign cells of G84E carriers versus non-carriers. P values < 0.05 were considered to be significant.
Methylation
Unpaired Student’s t-tests were used to compare methylation (β value) in reads containing the G84E variant allele versus reads with the wild-type. P values < 0.05 were considered to be significant.
Data Availability
The data generated during this study are either available in the Supplementary Materials section or from the corresponding author on reasonable request.
References
Hjelmborg, J. B. et al. The heritability of prostate cancer in the Nordic Twin Study of Cancer. Cancer Epidemiol Biomarkers Prev. 23, 2303–2310 (2014).
Lichtenstein, P. et al. Environmental and heritable factors in the causation of cancer–analyses of cohorts of twins from Sweden, Denmark, and Finland. N Engl J Med. 343, 78–85 (2000).
Al Olama, A. A. et al. A meta-analysis of 87,040 individuals identifies 23 new susceptibility loci for prostate cancer. Nat Genet. 46, 1103–1109 (2014).
Mancuso, N. et al. The contribution of rare variation to prostate cancer heritability. Nat Genet. 48, 30–35 (2016).
Ewing, C. M. et al. Germline mutations in HOXB13 and prostate-cancer risk. N Engl J Med. 366, 141–149 (2012).
Fitzgerald, L. M. et al. Germline missense variants in the BTNL2 gene are associated with prostate cancer susceptibility. Cancer Epidemiol Biomarkers Prev. 22, 1520–1528 (2013).
Karyadi, D. M. et al. Whole exome sequencing in 75 high-risk families with validation and replication in independent case-control studies identifies TANGO2, OR5H14, and CHAD as new prostate cancer susceptibility genes. Oncotarget. 8, 1495–1507 (2017).
Akbari, M. R. et al. Association between germline HOXB13 G84E mutation and risk of prostate cancer. J Natl Cancer Inst. 104, 1260–1262 (2012).
Chen, Z. et al. The G84E mutation of HOXB13 is associated with increased risk for prostate cancer: results from the REDUCE trial. Carcinogenesis. 34, 1260–1264 (2013).
Karlsson, R. et al. A population-based assessment of germline HOXB13 G84E mutation and prostate cancer risk. Eur Urol. 65, 169–176 (2014).
Kote-Jarai, Z. et al. Prevalence of the HOXB13 G84E germline mutation in British men and correlation with prostate cancer risk, tumour characteristics and clinical outcomes. Ann Oncol. 26, 756–761 (2015).
MacInnis, R. J. et al. Population-based estimate of prostate cancer risk for carriers of the HOXB13 missense mutation G84E. PLoS One. 8, e54727 (2013).
Stott-Miller, M. et al. HOXB13 mutations in a population-based, case-control study of prostate cancer. Prostate. 73, 634–641 (2013).
Xu, J. et al. HOXB13 is a susceptibility gene for prostate cancer: results from the International Consortium for Prostate Cancer Genetics (ICPCG). Hum Genet. 132, 5–14 (2013).
Economides, K. D. & Capecchi, M. R. Hoxb13 is required for normal differentiation and secretory function of the ventral prostate. Development. 130, 2061–2069 (2003).
Norris, J. D. et al. The homeodomain protein HOXB13 regulates the cellular response to androgens. Mol Cell. 36, 405–416 (2009).
Brechka, H., Bhanvadia, R. R., VanOpstall, C. & Vander Griend, D. J. HOXB13 mutations and binding partners in prostate development and cancer: Function, clinical significance, and future directions. Genes Dis. 4, 75–87 (2017).
Thornton, T. & McPeek, M. S. Case-control association testing with related individuals: a more powerful quasi-likelihood score test. Am J Hum Genet. 81, 321–337 (2007).
Laitinen, V. H. et al. HOXB13 G84E mutation in Finland: population-based analysis of prostate, breast, and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev. 22, 452–460 (2013).
Witte, J. S. et al. HOXB13 mutation and prostate cancer: studies of siblings and aggressive disease. Cancer Epidemiol Biomarkers Prev. 22, 675–680 (2013).
Chandrasekaran, G. et al. Computational Modeling of complete HOXB13 protein for predicting the functional effect of SNPs and the associated role in hereditary prostate cancer. Sci Rep. 7, 43830 (2017).
Kim, I. J., Kang, T. W., Jeong, T., Kim, Y. R. & Jung, C. HOXB13 regulates the prostate-derived Ets factor: implications for prostate cancer cell invasion. Int J Oncol. 45, 869–876 (2014).
Cardoso, M., Maia, S., Paulo, P. & Teixeira, M. R. Oncogenic mechanisms of HOXB13 missense mutations in prostate carcinogenesis. Oncoscience. 3, 288–296 (2016).
Lotan, T. L. et al. Somatic molecular subtyping of prostate tumors from HOXB13 G84E carriers. Oncotarget. 8, 22772–22782 (2017).
Benz, C. C. et al. Altered promoter usage characterizes monoallelic transcription arising with ERBB2 amplification in human breast cancers. Genes Chromosomes Cancer. 45, 983–994 (2006).
Hosokawa, Y. & Arnold, A. Mechanism of cyclin D1 (CCND1, PRAD1) overexpression in human cancer cells: analysis of allele-specific expression. Genes Chromosomes Cancer. 22, 66–71 (1998).
Schuur, E. R. & Weigel, R. J. Monoallelic amplification of estrogen receptor-alpha expression in breast cancer. Cancer Res. 60, 2598–2601 (2000).
Ghoshal, K. et al. HOXB13, a target of DNMT3B, is methylated at an upstream CpG island, and functions as a tumor suppressor in primary colorectal tumors. PLoS One. 5, e10338 (2010).
Beebe-Dimmer, J. L. et al. Prevalence of the HOXB13 G84E prostate cancer risk allele in men treated with radical prostatectomy. BJU Int. 113, 830–835 (2014).
Smith, S. C. et al. HOXB13 G84E-related familial prostate cancers: a clinical, histologic, and molecular survey. Am J Surg Pathol. 38, 615–626 (2014).
Storebjerg, T. M. et al. Prevalence of the HOXB13 G84E mutation in Danish men undergoing radical prostatectomy and its correlations with prostate cancer risk and aggressiveness. BJU Int. 118, 646–653 (2016).
Field, M. A., Cho, V., Andrews, T. D. & Goodnow, C. C. Reliably Detecting Clinically Important Variants Requires Both Combined Variant Calls and Optimized Filtering Strategies. PLoS One. 10, e0143199 (2015).
Field, M. A. et al. Reducing the search space for causal genetic variants with VASP. Bioinformatics. 31, 2377–2379 (2015).
Koressaar, T. & Remm, M. Enhancements and modifications of primer design program Primer3. Bioinformatics. 23, 1289–1291 (2007).
Untergasser, A. et al. Primer3–new capabilities and interfaces. Nucleic Acids Res. 40, e115 (2012).
Ma, X. J. et al. A two-gene expression ratio predicts clinical outcome in breast cancer patients treated with tamoxifen. Cancer Cell. 5, 607–616 (2004).
Mori, R., Wang, Q., Danenberg, K. D., Pinski, J. K. & Danenberg, P. V. Both beta-actin and GAPDH are useful reference genes for normalization of quantitative RT-PCR in human FFPE tissue samples of prostate cancer. Prostate. 68, 1555–1560 (2008).
Blankenberg, D., Von Kuster, G., Coraor, N., Ananda, G., Lazarus, R., Mangan, M. et al. Galaxy: a web-based genome analysis tool for experimentalists. Curr Protoc Mol Biol. Chapter 19: Unit 19.10.11-21 (2010).
Giardine, B. et al. Galaxy: a platform for interactive large-scale genome analysis. Genome Res. 15, 1451–1455 (2005).
Goecks, J., Nekrutenko, A. & Taylor, J. Galaxy: a comprehensive approach for supporting accessible, reproducible, and transparent computational research in the life sciences. Genome Biol. 11, R86 (2010).
Robinson, J. T. et al. Integrative genomics viewer. Nat Biotechnol. 29, 24–26 (2011).
Acknowledgements
We would like to acknowledge the histology assistance provided by Ms. N Phillips. JLD is supported by an Australian Research Council Future Fellowship. KR is supported by an Australian Government Research Training Program Scholarship. We are also greatly indebted to the participants of our prostate cancer studies, the Tasmanian Cancer Registry staff, Tasmanian urologists, pathologists and the wider Tasmanian clinical and research community for their ongoing support.
Author information
Authors and Affiliations
Contributions
L.M.F. and K.R. wrote the main manuscript and prepared the tables. K.R. prepared the figures. K.R. and J.R.M. performed the laboratory work. K.R., M.A.F. and R.J.T. performed the analyses. A.B. traced the participants and R.M. and S.D. sourced and reviewed the pathology material. N.B.B. and J.C.C. were involved in the generation and analysis of the sequencing data. J.L.D. and L.M.F. designed and directed the study and all authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
FitzGerald, L.M., Raspin, K., Marthick, J.R. et al. Impact of the G84E variant on HOXB13 gene and protein expression in formalin-fixed, paraffin-embedded prostate tumours. Sci Rep 7, 17778 (2017). https://doi.org/10.1038/s41598-017-18217-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-18217-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.