Abstract
The use of poppers is highly prevalent in MSM, but little is known about the association between their use and HIV incidence in China. A prospective cohort study was conducted from 2011 to 2013 in MSM in Shenyang. 475(79.6%) of eligible HIV-negative MSM participated in this prospective survey and near one fourth MSM (23.4%) ever used poppers. About one-third of the participants had condomless anal intercourse, half had multiple sexual partners and 10.5% were syphilis positive. The HIV incidence densities were15.5 (95% CI:9.4–23.4)/100 PY[person-years]) and 4.6 (95% CI:2.9–7.0)/100 PY in poppers-users and non-poppers-users, respectively. Predictors of HIV seroconversion included poppers-using-behavior, having had more than two male partners, practicing group sex, unprotected anal intercourse(UAI) with male partners, and baseline syphilis positivity (all P < 0.05). In conclusion, the use of poppers, high-risk-sexual behaviors and syphilis infection significantly increase the HIV incidence among Shenyang MSM. It is essential for policy makers to add poppers to the official controlled illicit drug list to reduce HIV transmission among the MSM community. A comprehensive strategy should also be implemented to control both their high-risk-sexual behaviors and risk of syphilis infection, since these may represent novel ways to prevent new HIV infections in these MSM.
Similar content being viewed by others
Introduction
The use of inhaled nitrites (usually known as poppers, but also as rush poppers or rush in China) has been highly prevalent among men who have sex with men (MSM) in Western developed countries for many years1,2,3. Due to their effects to induce vasodilatation of peripheral blood vessels and dilation of the anal sphincter, poppers can facilitate anal intercourse and enhance sexual pleasure4. There are published studies demonstrating that users of poppers have more often UAI (unprotected anal intercourse),2,5,6,7, greater male sexual partner concurrency7,8,9,10,11, and more group sexual behaviors11,12.
HIV epidemics among MSM in China have been soaring in recent years. The proportion of MSM with yearly reported new HIV/AIDS cases has increased by more than 10 times i.e. from 2.50% in 2006 up to 28.25% in 201513. Previous prospective cohort studies from Beijing and Shenyang have described an increasing trend of HIV incidence density among MSM. The HIV incidence density among MSM in Shenyang increased from 4.7/100PY in 2007 to 10.2/100PY in 200914, while the HIV incidence among MSM in Beijing increased from 6.2/100PY in 2007 to 11.4/100PY in 201215. This is clear evidence that the risk factors leading to rapid HIV acquisition among MSM have not been effectively addressed.
Recently, poppers have been added to the list of drugs that are controlled in several developed countries16,17. However, in many other developing countries including mainland China, there is no restriction on the use of poppers, they are not controlled illicit drugs, and nowadays poppers have become popular among MSM in China, Malaysia and some other countries9,18. Poppers are cheap and can be conveniently purchased over the Internet; not surprisingly, poppers are increasingly popular within the Chinese MSM community19. From 2013 to 2015, the proportion of MSM using poppers in Beijing, Shenyang, Changsha and other major Chinese cities ranged from 19.2% up to 29.8%11,12,18,19. Furthermore, most of the above cross-sectional studies found that the use of poppers was associated with a higher HIV prevalence9,10,11. However, cross-sectional studies could not confirm a causal relationship between HIV incidence and use of poppers. Additionally, it is a controversial issue whether poppers use is a co-occurring phenomenon with HIV infection or a contributor of HIV infection20,21. For example, although the studies of Buchbinder, S. P.et al. and Plankey M Wetal. reported that the use of poppers was significantly related to a higher HIV seroconversion rate in American MSM (aHR = 2.2, aHR = 2.1)22,23, two other publications, Huhn, G. D. and Mimiaga, M. J et al. failed to detect any statistically significant association between the use of poppers and HIV incidence24,25. Our team has estimated the HIV incidence of Chinese MSM in a multicenter study based on evaluating HIV seroconversion by BED-CEIA; we found that recreational drug use(poppers were the most prevalent recreational drug) was correlated with a higher rate of recent HIV infection26. In view of the false positive rate of evaluating HIV seroconversion by BED-CEIA27, a prospective cohort study is the most reliable way to evaluate HIV incidence and to determine its relationship with poppers-using behavior. It is clearly important to clarify the causal relationship of the use of poppers and HIV seroconversion via a prospective cohort study since the results can be used as a basis for informed policy making.
A prospective cohort study was performed among MSM in Shenyang, the political, economic, and cultural center of Liaoning Province in northeast of China. The primary objective of this study was to verify the real association between the use of poppers and HIV seroconversion as well as with other high-risk sexual behaviors, and thereby to provide health policy makers with the first-hand data to support programs to combat poppers-related behavior in MSM and thus reduce their HIV incidence.
Results
Characteristics of participants
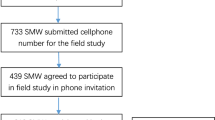
Our outreach program convinced a total of 668 MSM in Shenyang to attend the study between 2011 and 2013, of these 657 MSM attended the baseline-screening survey (Fig. 1). Of these MSM, 79.6% (475/597) were eligible and participated in the prospective cohort study and completed at least one follow-up visit.
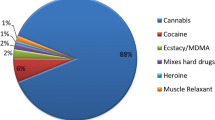
Among the 475 eligible participants, 61.7% (293/475) were younger than 30 years old, and 76.6% (364/475) were registered as living in Liaoning Province and 36.4% (174/475) attended college or above, 74.5% were single. About 23.4% (111/475), had used poppers, 4.8% (23/475), having used methamphetamine. If the time frame was the last 3 months, 18.9% (90/475) had used poppers and only 2.9% (14/475) consumed methamphetamine, 25.5% (121/475) had UAI with regular male partners, 29.7% (141/475) had UAI with casual male partners, 46.5% (221/475) had over 2 sexual partners and 12 participants had group sex. The median age when poppers were used for the first time was 24 years (IQR: 21–27), ranging from 16 years to 40 years. Additionally, the median time between first time use of poppers and participation in this survey was 1 year, and the median frequency of poppers use was 6 times.
Demographic and risky sexual behavioral factors correlated with poppers use
Table 1 presents the difference between poppers-users and non-poppers-users as assessed by the univariate analyses. Being younger than 30 years, having an educational level of college and above, being single, acting as a so-called money boy (MB), seeking homosexual partners through the Internet and having had group sex over the past 3 months were more prevalent among poppers-users than non-poppers-users (P < 0.05 for all features). Variables with the P < 0.10 in the univariate test were included in a multivariate stepwise logistic regression model. The variables which were significant at P < 0.05 were retained in the final logistic regression model as shown in Table 2. The factors that were independently associated with poppers use were age ≤30 years (aOR:2.3, 95%CI: 1.2–4.3), residence in some other province than Liaoning(aOR:2.0, 95%CI: 1.1–3.6), ever having sold sex to male partners (aOR:3.4, 95%CI: 1.4–8.0), seeking male sex partners over the Internet (aOR = 2.8,95%CI: 1.5–5.1) and having had group sex in the past 3 months (aOR:23.1,95%CI: 4.1–130.6) were independent factors associated with poppers-using behavior.
In the follow up 25 participates initiated popper use, 41 stopped using poppers and 45 always using poppers. Poppers group (n = 111) had higher bacterial STI (syphilis infection) than never use group (P = 0.010). While San Diego Early Test (SDET)scores were not significantly different among the four groups (P > 0.05) (Table 3).
HIV and syphilis incidence
A total of 657 eligible MSM were screened at baseline, of these 60 (9.1%, 95%CI: 7.0–11.6) were HIV-1 antibody positive and 69 (10.5%, 95%CI: 8.3–13.1) were syphilis positive. During the follow-up, 475 MSM who remained in the cohort representing a total of 568.5 person-years (PY); 39 MSM became HIV-1 seropositive and of these, 6 MSM were HIV-1 Pooled-RT-PCR positive. The calculated HIV-1 incidence density was 6.9(95%CI: 4.9–9.3)/100PY, and the syphilis incidence density was 8.3(95%CI: 6.1–10.8)/100PY. In poppers-users, there were 18 MSM who HIV-1 seroconverted, representing 46.2%(18/39) of the HIV-1 seropositive MSM. The HIV incidence was 15.5(95%CI: 9.4–23.4)/100PY. With respect to the non-poppers-users, there were 21 MSM who became HIV-1 seropositive (452.8PY), i.e. the HIV incidence density was 4.6(95%CI: 2.9–7.0)/100PY. The cumulative of HIV incidence increased over the 2-years of follow-up, the burden in the poppers user group was significantly higher than in non-poppers user group (Fig. 2).
Relationship between poppers-using behavior and HIV seroconversion
HIV seroconversion was the main outcome of interest. All potentially correlating factors in the past 3 months of the last follow-up were included in the Cox proportional hazard regression model. Univariate proportional hazard model analysis showed that seldom/never use of a condom with regular/casual male partners, having participated in group sex, having had more than two male partners, undertaking receptive anal intercourse, being syphilis positive as well as the use of poppers seemed to be significantly associated factors with HIV seroconversion (P < 0.20) (Table 4).
In model 1, after adjusting for all the covariates(e.g. age, level of education, registered residence, ethnicity, marital status, monthly income), multivariate Cox proportional hazard analysis revealed that any use of poppers (vs. non-poppers use) (aHR, 4.0, 95%CI: 2.1−7.7; P < 0.001), use of poppers in the past 3 months (vs. non-poppers use) (aHR, 3.6, 95%CI: 1.8−7.4; P < 0.001), baseline syphilis positive (aHR, 6.5, 95%CI: 3.2−13.2; P < 0.001), > 2 male partners in the past 3 months (vs. ≤ 2) (aHR, 2.0, 95%CI: 1.0−3.9; P = 0.044), having had group sex (aHR, 5.7, 95%CI: 2.0 −16.5; P = 0.001), seldom/never using a condom with regular male partners (vs. consistently using) (aHR, 2.6; 95%CI: 1.4−4.9; P = 0.003), and seldom/never using a condom with casual male partners (vs. consistently using) (aHR, 3.6; 95%CI: 1.8−6.9; P < 0.001) were independently associated factors with HIV seroconversion.
In model 2, multivariate Cox proportional hazard analysis also revealed that any use of poppers (vs. non-poppers use) (aHR, 3.9, 95%CI: 1.9−7.7; P < 0.001), baseline syphilis positive (aHR, 5.9, 95%CI: 3.0−11.8; P < 0.001), seldom/never using a condom with regular male partners (vs. consistently using) (aHR, 2.0; 95%CI: 1.0−3.8; P = 0.045), and seldom/never using a condom with casual male partners (vs. consistently using) (aHR, 2.8; 95%CI: 1.4−5.7; P = 0.003) were independently associated with HIV seroconversion.
Discussion
As far as we are aware, this is the first exploration of the association between the use of poppers and HIV seroconversion in a prospective cohort study of Chinese MSM. The HIV incidence in poppers-users was more than three times higher than in the control group (15.5vs. 4.6/100PY). Even after adjusting for other confounding factors in the multivariate Cox regression analysis, our study revealed that the use of poppers was an independent risk factor for HIV seroconversion. These results add to our understanding of the impact of popper-using behavior on HIV incidence in the MSM population, as well as confirming the association between popper-using behavior and HIV infection risk which had been postulated in previous Chinese cross-sectional studies9,10,11.
We found that nearly a quarter of MSM in Shenyang self-reported had used poppers at some time. Although our study site, Shenyang has the lowest GDP growth rate in China (−5.0% in 2016)28, the prevalence of the use of these compounds by MSM in Shenyang displayed no significant difference with more developed regions of China, such as Beijing (where the popper use incidence is 26.8%)9 and Changsha (21.4%)19, and even in cities in the developed countries, such as Toronto (27.27%)29 and Washington, DC (24.3%)30. In addition, we found that nearly every second poppers-user had started to use these compounds in the past year. Thus, it appears that the use of poppers is a relatively novel phenomenon among Shenyang MSM, in agreement with the results from a cross-sectional survey conducted in Beijing9. This indicates that health departments should strengthen HIV surveillance and develop prevention and intervention strategies targeting the Chinese poppers-using-MSM, irrespective of the economic growth level of the city in China.
Our study also showed that the use of poppers was more common in the younger, mobile population, who seek out male sex partners over the Internet and are willing to participate in group sex. Currently, China had the world’s largest number of cyber citizen (668 million people)31. Young MSM were more likely to accept new fashions, and this may explain their propensity to purchase poppers via the Internet. Additionally, up to 46.1% of MSM who are HIV-positive in China are so-called floating individuals32. After they leave the family home, they are more likely to buy cheap poppers and seek sexual stimulation with male partners because they are no longer restrained by traditional morality and ethical constraints. Although the Internet is a convenient conduit for the purchase and distribution of poppers in the MSM community, it also provides a good platform for behavior surveillance and implementing education, for example mounting web-based campaigns to prevent HIV infection in MSM.
Our study failed to find a statistically significant relationship between the use of poppers and unprotected anal intercourse, which is consistent with other previous publications9,11. But we found reporting recent poppers group had significant higher bacterial STI (syphilis) infection than never use group. It can also be seen sexual risk behavior/SDET score of our MSM subjects increased after initiate poppers use in group 1, but these differences were not significant. The pharmacological action of poppers is different from the synthetic stimulant drugs(such as methamphetamine)17; these latter agents can affect central nervous system function and influence decision-making, hence increasing the risk of unprotected anal intercourse33. However, our study showed that our group of poppers users had a significantly higher risk of participating in group sex. The reason might be the case that during group sex, the man will have many sessions of anal intercourse and poppers could relax the anal sphincter and thus facilitate multiple anal intercourses.
The HIV incidence in our poppers-user group among our studied MSM was 15.6/100PY, which was more than double the national average HIV incidence in Chinese MSM (5.61/100PY)34. The value was also higher than the HIV incidence in either Thai3 MSM (5.9/100PY) or American35 MSM (2.7/100PY). This highlights the alarming possibility that there may be a major HIV infection epidemic occurring in this vulnerable group of Chinese poppers-using MSM. Our prospective cohort study also confirmed that the use of poppers could significantly increase the risk of HIV seroconversion in these MSM. The adjusted hazard ratios associated with HIV seroconversion of life-time poppers-users and MSM who had used poppers in the past three months were 4.0 and 3.6 compared with non-poppers-users, respectively. Our study confirmed that poppers-using MSM had increased the risk of HIV infection and in fact, the elevated risk was greater than the value of 1.38 estimated by Zhang H.et al. in Beijing10 or the value of 1.88 elevated risk in the survey conducted by Chen X.et al. in Changsha11. The results were also consistent with the findings emerging from prospective cohort studies in American MSM22,23,35.The risks associated with poppers-using behavior of MSM population emphasize the need for some form of intervention. The regulatory authorities may consider following the parallel situation when they’re-classified methylmorphinephosphate into the list of illicit drugs36 i.e. the Chinese Food and Drug Administration, Ministry of Public Security of the People’s Republic of China and National Health and Family Planning Commission of the People’s Republic of China placed methyl morphine phosphate on the list of controlled psychotropic substances, which is expected to prevent its illegal distribution. It is the case that in our cohort study, the consumption of methylmorphinephosphate did not have any causal association with HIV seroconversion (HR: 1.3, P = 0.654). Since the use of poppers dramatically elevates the risk of HIV infection, we would recommend that poppers should be included in the controlled drugs list, as is the case in USA and Great Britain16. We would argue that legislation intended to significantly reduce the use of poppers could be an effective way to stop the spread of HIV in the Chinese MSM population.
In addition to the use of poppers, we also found that unsafe sexual practices were prevalent in the MSM population in Shenyang i.e. unprotected anal intercourse, having multiple male sex partners and syphilis infection; these were also associated with a statistically elevated HIV incidence. The influence of these factors on HIV incidence in the MSM population has been verified in many previous studies15,26,37,38. This indicates that comprehensive prevention and control measures, including condom distribution, peer education, syphilis diagnostics and referral and therapy, might be required to control HIV transmission among the local MSM population. Literature suggest that methamphetamines use is directly associated with HIV risk increase39, but methamphetamines use behavior was highly significant in the univariate model but fell out of the multivariate model in our study. It may be caused by low sample size and corresponding low statistical analysis efficiency. Additionally, given methamphetamines are illegal in China, our study methamphetamines using behavior was only measured basing on self-report, which may under estimate methamphetamines using number and using rate. So, methamphetamines using behavior should be measured by both self-reporting and related laboratory testing, and larger size surveys should be conducted to China MSM to further investigate their relationship of methamphetamines using behavior and HIV incidence later.
Our study has some strengths. Firstly, this is the first prospective cohort study to determine the influence of poppers use on HIV seroconversion among MSM in China; thus it can act as an important reference point for developing an effective HIV prevention strategy, especially one involving a control of the sale of poppers. Secondly, there are various derivatives and several Chinese names for poppers, and we provided both words and pictures about poppers and their derivatives during this project in order to reduce the possibility that our MSM subjects would not understand what we meant by the term “poppers” i.e. potential information bias was reduced. Thirdly, during the creation of the questionnaire survey, in order to ensure its comprehensibility, instead of using terms like “drugs” or “illicit” to describe poppers and methamphetamine, the question was phrased as “whether you have ever consumed special substances, usually called ‘rush’, ‘rush poppers’ and ‘ice’”. Furthermore, these sensitive questions were placed at the end of the questionnaire when the respondent was more at ease. We believe that all of these measures have reduced the possibility of social desirability bias, at least to some extent, and thus improve the quality of the questionnaire.
However, there are also some limitations. Above all, the sample sizes of our cohort (N = 475) were small, particular the low number of seroconversion in those who ever used poppers (only 18) and even lower number of methamphetamines users (only 2). A small sample (N = 400) study in Beijing China also did not find methamphetamines increasing the risk of HIV acquisition9 but different from a large cohort study in San Diego (N = 8905)39. The second, owing to the traditional culture of China, the MSM are a discriminated and underground population, and since our study used non-probability sampling, the results do not completely represent the entire MSM population in Shenyang; thus caution is necessary when extrapolating the study results. Next, there were some participants lost to follow-up (20.4%). Though the cohort retention rate was higher than the retention rate in previous domestic studies (52.4%-70.5%)37,40,41, the results do not represent the characteristics of these MSM lost to follow-up. Finally, we used interviewing and a questionnaire survey to ask sensitive questions, and the exposure of poppers use and high risk sexual behaviors might have been underestimated because of the social desirability bias. If this were the case, then it is possible that we have underestimated the association between the use of poppers and high risk sexual behaviors. Some of these limitations could possibly be avoided by developing some kind of social-bias neutral computer assisted questionnaire survey for posing sensitive questions.
In conclusion, the use of poppers was very popular in the Shenyang MSM. We confirmed the previous supposition that the use of these compounds increases the incidence of HIV in MSM. Poppers are not considered as controlled drugs and can be easily obtained either through the Internet or in other ways, therefore health authorities should implement actions to break the link between the use of these compounds and high risk sexual behaviors; this would be one effective way to prevent the spread of HIV. The Chinese drug control department should be encouraged to place poppers on the controlled substance list as is the case in some developed countries. If this cannot be done, then the health authorities should initiate a campaign to make MSM aware of the link between the use of poppers and the risk of acquiring HIV. If the intervention only achieves some limitation into the use of poppers, it is unlikely to prevent the potential HIV epidemic. This can only be combated by undertaking comprehensive interventions, focusing not only on the use of poppers but also on the related behaviors, such as multiple sex partners, group sex, UAI, and other high risk activities, in this population.
Methods
Ethics Statement
This study protocol was approved by the Institutional Review Board of the First Affiliated Hospital of China Medical University ([2011]-36). All study participants provided written informed consent for the interview and blood collection. This study was performed in accordance with the relevant guidelines and regulations.
Study Population
From January 2011 to January 2013, MSM subjects were enrolled through snowball sampling methods, with an open prospective cohort being recruited among MSM in Shenyang. Enrolled eligible MSM participants returned every 3 months for a follow-up interview at the same time as an HIV and syphilis test. The inclusion criteria were: 18 years or older, male, self-reporting anal and/or oral intercourse with male partners in the past 6 months, HIV-1 negative tested by enzyme linked immunosorbent assay (ELISA) and pooled-RT-PCR, willing and able to provide a written informed consent.
Study Procedures
This survey was arranged in the voluntary counseling and testing (VCT) center in the First Affiliated Hospital of China Medical University. Every enrolled participant was assigned a unique identifier code instead of the patient names. Qualified participants were investigated face-to-face by trained staff in a private counseling room. The questionnaire covered questions on demographics, sexual practices, and substance use, including history of recreational drug use and whether used poppers and/or methamphetamine in the past 3 months. For example, “Have you ever inhaled a special drug (poppers or rush) in a bottle before or during anal intercourse to enhance sexual pleasure?” Sexual practices and substance use were investigated at each follow-up visit. During the study, they could continue to participate or drop-out of the cohort according to their own accord. The outcome was HIV-1 seroconversion; if that occurred, the participants would receive a referral to CDC, so that they could receive antiretroviral therapy and undergo CD4 count testing.
HIV post-test counseling was provided to each MSM individual when they returned for their HIV test results within three days of blood sampling. Condoms and lubricants were freely distributed to each MSM subject.
San Diego Early Test (SDET) score was used to evaluated sexual risk behavior for every single testing subject42,43: condomless receptive anal intercourse (CRAI) with an HIV-positive MSM (3 points), the combination of CRAI plus greater than or equal to5 male partners (3 points), greater than or equal to10 male partners (2 points), and diagnosis of bacterial sexually transmitted infection (2points)—all as reported for the prior 12 months. The score is based on key risk variables that predict risk of HIV acquisition among MSM: condom less receptive anal intercourse (CRAI),number of male partners, and self-reported bacterial sexually transmitted infection (STI). We performed the syphilis in lab, as a supplement of self-reported STI.
We also made analyses on poppers use in repeat testers. Eligible participants were assigned to one of four groups based on their reported poppers use at the first and most recent repeat HIV testing encounter: i) Group 1: started using poppers (i.e. never-poppers to recent-poppers), ii) Group 2: stopped using poppers(i.e. recent-poppers to no recent-poppers), iii) Group 3: continued poppers (i.e. recent-poppers to recent-poppers), and iv) Group 4: does not use poppers (i.e. never-poppers to never-poppers)39,43.
Laboratory Test
A volume of 10 ml of venous blood was drawn from each participant for diagnosing HIV and syphilis after informed consent had been obtained. HIV-1 antibody screening was performed by enzyme-linked immunosorbent assay (ELISA) and positive cases were further confirmed by western blot (WB). HIV-1 antibody negative cases and positive cases in which WB was uncertain or negative were tested by HIV-1 Pooled-RT-PCR44, using the reagent kit [COBAS AMPLICOR HIV-1 MONITORTM Test,v1.5](ROCHE, 21118390123). Syphilis serology was performed with the rapid plasma regain [RPR] test (Shanghai Kehua, China), and positive cases were confirmed by the Treponemapallidum particle assay (TPPA, Serodia, Japan). Participants with plasma positive for both RPR and TPPA were deemed to be currently infected with syphilis.
Outcome Measures
MSM self-reporting ever used of poppers before or during anal intercourse were defined as poppers-users, otherwise the respondents were considered as non-popper-users. Baseline HIV antibody seronegative cases that became seroconverted during the follow-up or in whom HIV antibody was seronegative during the follow-up but the pooled RT-PCR tested positive and in whom there was evidence of HIV antibody seroconversion were defined as HIV seroconversion. The time of HIV seroconversion was defined as the middle time point between the last HIV-seronegative date and the first HIV-seropositive date.
Data analysis
Data were both double entered and then checked for accuracy using Epi Data 3.0. Data analyses were performed using SPSS (version 17.0; SPSS, Inc., Chicago, IL, USA). Chi-square test and stepwise logistic regression were used to evaluate which factors were associated with the use of poppers. Variables with p < 0.2 in univariate analysis were included in a multivariate stepwise logistic analysis, and variables significant at P < 0.05wereretained in the final model. Cox proportional hazards models with time-dependent covariates were used to assess hazard ratios for factors such as sexual behaviors and substance use to determine their effects on HIV incidence. Time-dependent covariates included condom use with regular/ casual male partners, group sex, number of male partners, use of poppers and/or methamphetamine in the past three months. The model 1 was adjusted for demographics, such as age, level of education, registered residence, ethnicity, marital status and monthly income. And model 2 was selected with a enter procedure, covariates included condom use with regular/ casual male partners, group sex, number of male partners, syphilis, and use of poppers. A two-sided P-valueless than0.05 was considered as statistically significant.
References
Wirtz, A. L. et al. Alcohol Use and Associated Sexual and Substance Use Behaviors Among Men Who Have Sex with Men in Moscow, Russia. AIDS Behav 20, 523–36 (2016).
Melendez-Torres, G. J., Hickson, F., Reid, D., Weatherburn, P. & Bonell, C. Drug use moderates associations between location of sex and unprotected anal intercourse in men who have sex with men: nested cross-sectional study of dyadic encounters with new partners. Sex Transm Infect 92, 39–43 (2016).
Van Griensven, F. et al. Evidence of an explosive epidemic of HIV infection in a cohort of men who have sex with men in Thailand. AIDS 27, 825–32 (2013).
Williams, J. F. & Storck, M. Inhalant abuse. Pediatrics 119, 1009–17 (2007).
Santos, G. M. et al. Dose-response associations between number and frequency of substance use and high-risk sexual behaviors among HIV-negative substance-using men who have sex with men (SUMSM) in San Francisco. J Acquir Immune Defic Syndr 63, 540–4 (2013).
Vanden Berghe, W., Nostlinger, C., Hospers, H. & Laga, M. International mobility, sexual behaviour and HIV-related characteristics of men who have sex with men residing in Belgium. BMC Public Health 13, 968 (2013).
Thomas M Lampinen, K.M., Keith Chan and Robert S Hogg. Nitrite inhalant use among young gay and bisexual men in Vancouver during a period of increasing HIV incidence. BMC Public Health (2007).
Wang, Z. et al. Prevalence and associated factors of inhaled nitrites use among men who have sex with men in Beijing, China. Drug Alcohol Depend 149, 93–9 (2015).
Li, D. et al. Nitrite inhalants use and HIV infection among men who have sex with men in China. Biomed Res Int 2014, 365261 (2014).
Zhang, H. et al. Poppers use and risky sexual behaviors among men who have sex with men in Beijing, China. Drug Alcohol Depend 160, 42–8 (2016).
Chen, X. et al. Club Drugs and HIV/STD Infection: An Exploratory Analysis among Men Who Have Sex with Men in Changsha, China. PLoS One 10, e0126320 (2015).
Prestage, G., Down, I., Grulich, A. & Zablotska, I. Sex partying among gay men in Sydney, Melbourne and Brisbane, Australia. AIDS Behav 15, 298–304 (2011).
CDC, N. N. C. Update on the AIDS/STD epidemic in China and main response in control and prevention in December, 2015? Chinese Journal of AIDS & STD 22, 69 (2016).
Zhang, M. et al. A rapidly increasing incidence of HIV and syphilis among men who have sex with men in a major city of China. AIDS Res Hum Retroviruses 27, 1139–40 (2011).
Jia, Z. et al. HIV burden in men who have sex with men: a prospective cohort study 2007–2012. Sci Rep 5, 11205 (2015).
Liss, B. I. Government, Trade and Industry and Other Preventative Responses to Volatile Substance Abuse. Human Toxicology 8, 327–30 (1989).
Frank Romanelli, K. M. S. & Alice, C. T. Claire Pomeroy. Poppers: Epidemiology and Clinical Management of Inhaled Nitrite Abuse. Pharmacotherapy 24, 69–78 (2004).
Lim, S. H. et al. Latent class analysis of substance use among men who have sex with men in Malaysia: Findings from the Asian Internet MSM Sex Survey. Drug Alcohol Depend 151, 31–7 (2015).
Xu, J. J. et al. Recreational drug use among Chinese men who have sex with men: a risky combination with unprotected sex for acquiring HIV infection. Biomed Res Int 2014, 725361 (2014).
Drumright, L. N., Patterson, T. L. & Strathdee, S. A. Club drugs as causal risk factors for HIV acquisition among men who have sex with men: a review. Subst Use Misuse 41, 1551–601 (2006).
Colfax, G. & Guzman, R. Club drugs and HIV infection: a review. Clin Infect Dis 42, 1463–9 (2006).
Plankey, M. W. et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr 45, 85–92 (2007).
Buchbinder, S. P. et al. Sexual risk, nitrite inhalant use, and lack of circumcision associated with HIV seroconversion in men who have sex with men in the United States. J Acquir Immune Defic Syndr 39, 82–9 (2005).
Mimiaga, M. J. et al. The effect of psychosocial syndemic production on 4-year HIV incidence and risk behavior in a large cohort of sexually active men who have sex with men. J Acquir Immune Defic Syndr 68, 329–36 (2015).
Huhn, G. D. et al. Factors associated with newly diagnosed HIV among persons with concomitant sexually transmitted diseases. Sex Transm Dis 35, 731–7 (2008).
Xu, J. J. et al. High HIV incidence epidemic among men who have sex with men in china: results from a multi-site cross-sectional study. Infect Dis Poverty 5, 82 (2016).
Parekh, B. S. & McDougal, J. S. Application of laboratory methods for estimation of HIV-1 incidence. Indian J Med Res 121, 510–8 (2005).
Li, X. Major cities in China in the first three quarters GDP growth rate ranking 2016 China’s urban development network, http://www.chinacity.org.cn/csph/csph/327149.html (2016).
Kesler, M. A. et al. Actual sexual risk and perceived risk of HIV acquisition among HIV-negative men who have sex with men in Toronto, Canada. BMC Public Health 16, 254 (2016).
Fisher, M. P., Ramchand, R., Bana, S. & MY, I. Risk behaviors among HIV-positive gay and bisexual men at party-oriented vacations. J Stud Alcohol Drugs 74, 158–67 (2013).
Center, C. I. N. I. China Internet network development state statistic report. Internet Communication, 54–59 (2015).
Qin Qianqian et al. The characteristics of HIV-positive men who have sex with men in China and predictors of their migration, 2008–2015. Zhonghua Yu Fang Yi Xue Za Zhi 50, 938–42 (2016).
Crosby, G. M., Stall, R. D., Paul, J. P., Barrett, D. C. & Midanik, L. T. Condom use among gay/bisexual male substance abusers using the timeline follow-back method. Addict Behav 21, 249–57 (1996).
Zhang, W. et al. HIV incidence and associated risk factors in men who have sex with men in Mainland China: an updated systematic review and meta-analysis. Sex Health (2016).
Ackers, M. L. et al. High and persistent HIV seroincidence in men who have sex with men across 47 U. S. cities. PLoS One 7, e34972 (2012).
Kong, D. Cough syrup can also lead to addiction. People’s Public Security, 18-18 (2015).
Xu, J. J. et al. Syphilis and HIV seroconversion among a 12-month prospective cohort of men who have sex with men in Shenyang, China. Sex Transm Dis 37, 432–9 (2010).
Das, A. et al. Factors associated with HIV and syphilis co-infection among men who have sex with men in seven Chinese cities. Int J STD AIDS 26, 145–55 (2015).
Hoenigl, M. et al. Clear Links Between Starting Methamphetamine and Increasing Sexual Risk Behavior: A Cohort Study Among Men Who Have Sex With Men. J Acquir Immune Defic Syndr 71, 551–7 (2016).
Mao, H. et al. High incidence of HIV and syphilis among migrant men who have sex with men in Beijing, China: a prospective cohort study. BMJ Open 4, e005351 (2014).
Wang, Q. Q. et al. HIV prevalence, incidence and risk behaviours among men who have sex with men in Yangzhou and Guangzhou, China: a cohort study. J Int AIDS Soc 17, 18849 (2014).
Hoenigl, M. et al. Development and validation of the San Diego Early Test Score to predict acute and early HIV infection risk in men who have sex with men. Clin Infect Dis 61, 468–75 (2015).
Hoenigl, M. et al. Repeat HIV-testing is associated with an increase in behavioral risk among men who have sex with men: a cohort study. BMC Med 13, 218 (2015).
Han, X. et al. Screening acute HIV infections among Chinese men who have sex with men from voluntary counseling & testing centers. PLoS One 6, e28792 (2011).
Acknowledgements
The authors thank the volunteers from Shenyang sunny group for helping with recruitment of the participants. We also thank all of the MSM who attended this study for sharing their information andtheir time. The study was supported by the Mega-Projects of national science research for the 12th Five-Year Plan (2012ZX10001–006) and Liaoning Educational Department project (LZ2014038).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: Z.X.C., H.S., J.J.X.; performed the study and experiments: Z.X.C., J.Z., Q.H.H. H.Y.W., K.Y.; analyzed the data: Z.X.C., Q.H.H; contributed materials/reagents/analysis tools: Y.J.J., W.Q.G.; wrote and revised the manuscript: Z.X.C. J.J.X., Y.H.Z., H.S. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chu, Zx., Xu, Jj., Zhang, Yh. et al. Poppers use and Sexual Partner Concurrency Increase the HIV Incidence of MSM: a 24-month Prospective Cohort Survey in Shenyang, China. Sci Rep 8, 24 (2018). https://doi.org/10.1038/s41598-017-18127-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-18127-x
This article is cited by
-
Homoprejudiced Violence Experiences and High-Risk Sexual Behaviors among Chinese Men Who Have Sex with Men: Depression Severity and Recreational Drug Usage as Potential Mediators
Archives of Sexual Behavior (2024)
-
Correlates of group sex participation among men who have sex with men in Chongqing, Southwestern China
BMC Public Health (2021)
-
HIV incidence and sexual behavioral correlates among 4578 men who have sex with men (MSM) in Chengdu, China: a retrospective cohort study
BMC Public Health (2021)
-
The use of inappropriate anal douching tool associates with increased HIV infection among men who have sex with men: a cross-sectional study in Shenyang, China
BMC Public Health (2021)
-
Natural presence of the V179D and K103R/V179D mutations associated with resistance to nonnucleoside reverse transcriptase inhibitors in HIV-1 CRF65_cpx strains
BMC Infectious Diseases (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.