Abstract
Significant variability exists in physical therapy early mobilization practice. The frequency of physical therapy or early mobilization of patients in the cardiothoracic intensive care unit and its effect on length of stay has not been investigated. The goal of our research was to examine variables that influence physical therapy evaluation and treatment in the intensive care unit using a retrospective chart review. Patients (n = 2568) were categorized and compared based on the most common diagnoses or surgical procedures. Multivariate semi-logarithmic regression analyses were used to determine correlations. Differences among patient subgroups for all independent variables other than age and for length of stay were found. The regression model determined that time to first physical therapy evaluation, Charlson Comorbidity Index score, mean days of physical therapy treatment and mechanical ventilation were associated with increased hospital length of stay. Time to first physical therapy evaluation in the intensive care unit and the hospital, and mean days of physical therapy treatment associated with hospital length of stay. Further prospective study is required to determine whether shortening time to physical therapy evaluation and treatment in a cardiothoracic intensive care unit could influence length of stay.
Similar content being viewed by others
Introduction
Patients who require intensive critical care during hospitalization have high morbidity and mortality rates, experience decline in functional status and incur high costs of care overall1. Impaired exercise capacity, persistent weakness, enduring neuropsychological impairments and high costs of healthcare utilization in these patients lead to a negative post ICU trajectory attributed to muscle wasting and weakness2,3,4. The suboptimal quality of life survivors report is likely related to the significant physical, psychological, and financial complications that endure over time5,6. Early active mobility during ICU care is now recommended by International guidelines and is often performed by interprofessional teams consisting of physical therapists and other ICU care team members7. Early active mobilization includes active or resistive range of motion exercises, position changes in bed, transfers out of bed, progressive mobility protocols and ambulation; and increasingly studies show promising results1,3,8,9,10,11,12. More importantly, this clinical practice has been found to be safe2,13,14 and highlights the improvement early active mobilization produces in the re-acquisition of mobility skills2,13 although prospective studies have not shown reductions in length of stay12,14,15,16.
Despite growing support for the benefits of early active mobilization of patients in the ICU, significant variability in this practice exists17. Timing and amount of physical therapy during critical illness, staffing levels sufficient to meet patients’ needs, guidelines or protocols for recommended care, leadership, staff education, and variability in type of staff used during early mobility programs have been attributed to these differences13,18,19,20. Little is known about the practice of early active mobilization with physical therapists or physical therapist assistants in patients with cardiac or neurologic conditions despite higher ICU utilization by these patients21. Complications related to clinical care are a risk for cardiothoracic ICU patients, who are increasingly diagnosed with frailty22,23,24,25,26, which may predict post-surgical complications including, mortality, prolonged ventilation, and poor medical and functional outcomes27,28. These complications and comorbidities have the potential to influence time to physical therapy evaluation and consistency of physical therapy treatment to achieve early active mobilization of patients, but it is currently unknown what factors influence timing and amount of treatment. Understanding current mobilization practices with physical therapists and/or other members of the care team is critical to the design and implementation of strategies to improve the early active mobilization to the diverse population of critically ill patients in the ICU17,29.
Physical therapy evaluation and treatment in the acute care setting is highly focused on functional mobility status with interventions related to patient functional ability (bed mobility, transfers, use of assistive devices, gait or ambulation, etc.) representing the greatest percentage of treatment30. Both early mobilization and rehabilitation begin upon achievement of hemodynamic stability and international consensus on guidelines for safe mobilization of ventilated patients was achieved using criteria established for a variety of medical considerations31,32,33,34. These considerations can be a barrier to initiation of physical therapy evaluation and consistent performance of physical therapy treatment sessions in the cardiothoracic intensive care unit20,35,36,37. Populations in the cardiothoracic ICU who experience pre-surgical frailty or functional impairment may be at increased risk of complications following the initiation of well-known ICU medications impacting utilization of physical therapy interventions38,39. How these delays and complications impact patient treatment is difficult to determine but may relate to outcomes for distinct diagnoses. Identifying current delivery of physical therapy treatment in this population supports opportunities to redirect or shift staff responsibilities, improve clinical care and focus physical therapy treatment on those patients with greatest need40,41.
The purpose of this study is to determine existing mobilization practices as measured by timing and amount of physical therapy in patients with cardiac and respiratory problems requiring intervention in the cardiothoracic ICU (CT ICU). In addition, we were interested in differences in the time to first physical therapy evaluation and treatment for select patient surgical procedures and medical diagnoses, considering the level of patient complexity in this population, which has not previously been addressed. A comparison of hospital and CT ICU LOS between select patient subgroups is warranted to identify potential opportunities for physical therapists to promote more timely, efficient, and cost-effective physical therapy delivery for the distinct patient populations. This includes determining that associations exist between LOS in this patient population and timing and amount of physical therapy.
Methods
Design and Participants
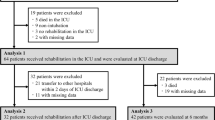
We performed a retrospective, cross-sectional study of patients in the CT ICU at University of Kentucky (UK) HealthCare from March 2012 to May 2015 who received physical therapy evaluation and/or treatment as part of the standard of care. The UK Institutional Review Board approved this study. We accessed data via the UK Center for Clinical and Translational Science (CCTS) searching Soft Med and Avega programs for hospital data. Our population (n = 2,568) was based on individual patient encounters for all patients ≥18 years of age. We excluded pregnant women and prisoners from our population. Our patient population was divided into subgroups based on the highest volume procedures or diagnoses in the CT ICU during the study timeframe defined by the International Classification of Diseases, Ninth Edition (ICD-9)42. This includes patients post coronary artery bypass graft (CABG, n = 638), post valve replacement surgery (Valve, n = 339), post ventricular assist device implantation (VAD, n = 53), requiring extracorporeal membrane oxygenation (ECMO, n = 27), diagnosed with respiratory failure (mechanical ventilation >96 hours, n = 186), post heart transplantation (Heart transplant, n = 35), and post lung transplantation (Lung transplant, n = 32). All other patient procedures and diagnoses are included in the entire cardiothoracic patient population during the study time frame (n = 1258).
Patients received physical therapy evaluation and treatment based on consultation from the primary physician service line (e.g. Cardiology, Thoracic surgery, Cardiothoracic surgery, etc.) providing care for the patient during the hospitalization. At UK HealthCare, physical therapists have 24 hours after receiving notice of consultation to provide an initial evaluation or communicate to the medical team that physical therapy evaluation and treatment is deferred due to medical reasons. To identify patients who received physical therapy evaluation and treatment provided by either a physical therapist or physical therapist assistant at this facility, we used standard current procedural terminology (CPT) codes. The specific CPT codes used reflect physical therapy evaluation (97001), re-evaluation (97002), and other common CPT codes that describe rehabilitation treatment most frequently used by physical therapist and physical therapist assistant staff at this facility: therapeutic activities (97530), therapeutic exercise (97110), neuromuscular re-education (97112), and gait training (97116)43. This method allowed us to determine both mean days of physical therapy treatment and time to first physical therapy evaluation in the CT ICU or hospital facility. Time to first physical therapy evaluation in the CT ICU and hospital was determined using the date/time of admission in the CT ICU or hospital then identifying the date/time of the first physical therapy evaluation using the evaluation CPT code. Any date with a physical therapy CPT code entered for a patient was considered a day of physical therapy evaluation, re-evaluation or treatment. No patient encounters in this dataset were found to not receive some form of physical therapy evaluation and/or treatment during the hospitalization.
Using a retrospective review of the data limited our assessment of patient or disease severity in this population as we lacked access to data commonly collected such as APACHE II scores. However, we were able to determine a measure of patient complexity using Charlson Comorbidity Index (CCI) scores. Using CCI scores to express comorbidity has been a common method to control for confounding in epidemiologic studies and scores are used in predicting health outcomes, healthcare utilization, and healthcare expenditures44. Examining the CCI scores allows us to account for ICU treatment complexity required in the medical care of patients in the study population. The index lists 19 comorbid conditions, each assigned a weight from one to six. The CCI is the sum of the weights for all conditions for each patient44. We used the five digit enhanced ICD-9-CM (Clinical Modification) codes to determine CCI scores based on the algorithm developed by Quan H, et al.45.
The independent variables of interest for this analysis were mean days of physical therapy treatment during hospitalization (including in the CT ICU and after transfer or admission to the floor), means days requiring mechanical ventilation, time to first physical therapy evaluation (in the CT ICU or on other units within the hospital) in days, comorbidity score, and age during hospitalization. We distinguished between time to first physical therapy evaluation in the CT ICU as well as within the hospital facility, as patients may admit to other units before transfer to the CT ICU or may require physical therapy evaluation and treatment prior to surgery. The dependent variables of interest include CT ICU LOS and hospital LOS. Hospital LOS, measured in days, is used as an outcome measure of efficiency and resource utilization in hospital services. It is ultimately a measure of hospital quality, processes of care and access to healthcare46. Previous literature suggests that greater patient mobilization and physical therapy treatment provided during critical illness is associated with decreased hospital length of stay9,47.
All data were analyzed using JMP®, Version 12. SAS Institute Inc., Cary, NC, 2015. Initial descriptive statistics were calculated. The procedure and/or diagnoses were dummy coded for each subgroup in the patient population for comparison. One way analyses of variance (ANOVA) was performed where comorbidity score was not a significant factor between groups, and analyses of covariance (ANCOVA), where comorbidity was a significant factor between groups, to compare all variables except for age for the following populations: CABG, Valve, VAD, heart transplant or lung transplant, ECMO and respiratory failure. Pairwise multiple comparison procedures were performed using LSD method. Given our large sample size and our understanding of potential bias in our data, patients not included in any or included in more than one subgroup were excluded from the ANOVA and ANCOVA analysis. We had 1258 patients with greater than one or none of the diagnosis or surgical procedure during the study timeframe. Multivariate linear regression equations were estimated to examine the association between the independent variables and the dependent variables, using specification tests to rule out omitted variable bias. After performing a correlational matrix of the independent variables, we determined low correlation between variables with the exception of mean days of physical therapy and mean days of mechanical ventilation (0.49). Variance inflation factors suggested minimal risk of multicollinearity in the model. A logarithmic transformation of the dependent LOS variable (hospital and CT ICU LOS) was performed to create normal distribution and improve model fit. Multivariate semi-logarithmic regression models were estimated using the same independent variables in the linear regression models.
Ethics Approval and Consent to participate
We received ethics approval from the University of Kentucky Institutional Review Board, Office of Research Integrity, IRB #15-0276-P1H. Informed consent was waived since the study was a retrospective review of data. All research procedures were carried out in accordance with relevant guidelines and regulations.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to restrictions from the healthcare system under study but are available from the corresponding author on reasonable request.
Results
Descriptive Statistics
Table 1 includes the demographic information and descriptive statistics of our patient population including comorbidity for each patient subgroup (Table 1). Racial and ethnic categories were not described since analysis of the data revealed the population to be predominately homogenous (Caucasian).
Differences between Distinct Patient Subgroups
Analysis of variance or analysis of covariance if more appropriate indicates differences among certain patient subgroups for all variables other than age are greater than would be expected by random chance. See Tables 2–4 for all ANOVA results.
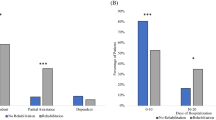
Differences in mean days of physical therapy and time to first physical therapy evaluation were observed for the subgroups (Table 2). Patients post CABG and Valve surgery had fewer mean days of physical therapy than all other subgroups. Patients post heart and lung transplant both had an average of 8 days of physical therapy and this was greater than patients post CABG and Valve surgery and fewer than patients diagnosed with respiratory failure. Days to first PT evaluation show patient procedure or diagnosis influenced initiation of PT in the hospital and CT ICU (Table 2). Patients with respiratory failure had on average more days until the first PT session in the ICU than all the other subgroups. Patients requiring more invasive cardiac surgery or support (patients post heart transplant and who required ECMO) had greater delay in days to first PT in the CT ICU compared to patients requiring less invasive cardiac surgery (post CABG, Valve, and VAD) (Table 2). Patients with heart transplant and respiratory failure had the greatest mean days to PT in the hospital. Data for patients not included in the subgroups were added for comparison, but were not part of the ANOVA analysis.
Comorbidity score was found to be significantly different between select patient subgroups (Table 3). Patients post CABG and Valve surgery showed the lowest CCI scores in the population and were different from all subgroups other than patients requiring ECMO (Table 3). Patients with respiratory failure had a much larger CCI score compared to patients requiring ECMO (Table 3). Mean days of mechanical ventilation were also found to be different between select subgroups. However, no distinguishable difference was found between patients post lung transplant, requiring ECMO and with respiratory failure (Table 3). Data for patients not included in the subgroups were added for comparison, but were not part of the ANOVA analysis.
Table 4 shows differences in hospital and CT ICU LOS between the distinct patient subgroups. There is no difference between the hospital or CT ICU LOS for patients post VAD, heart transplant, lung transplant, and requiring ECMO (Table 4). Interestingly, patients post CABG or post Valve surgery have shorter CT ICU and hospital LOS overall, yet statistically significant differences exist between these two patient subgroups for hospital LOS (Table 4). Patients with respiratory failure are significantly different than all other subgroups, showing significant differences in hospital and CT ICU LOS compared to all other subgroups (Table 4). Data for patients not included in the subgroups were added for comparison, but were not part of the ANOVA analysis.
Regression Results
We ran a semi logarithmic regression model to determine if timing and amount of physical therapy is associated with hospital and CT ICU LOS and how strongly the variables in the model explain hospital and CT ICU LOS for the patient subgroups (Tables 5 and 6). Using the variables time to first PT in the ICU, CCI score, mean days of PT, and mean days of mechanical ventilation showed strong and large variances in hospital (Table 5) and CT ICU LOS (Table 6). When using this semi logarithmic regression model for hospital LOS in each sub population of CT ICU patients, all patient subgroups showed adjusted R2 greater than 0.49 (49%) (Table 5). Nearly 50% of the variability of hospital LOS in these patient subgroups can be explained by the independent variables. For example, in patients post lung transplant, this model explained 74% of the variability in hospital LOS.
The variables most frequently determined to be statistically significant for each subgroup model were time to first PT in the CT ICU, mean days of PT, and mean days of mechanical ventilation (Tables 5 and 6). Using this model to explain CT ICU LOS in each patient subgroup showed smaller variance for certain subgroups (CABG, Valve and respiratory failure) and larger variance in others (VAD, heart transplant and lung transplant) (Table 6). The same variables for timing and amount of physical therapy demonstrated strong associations with CT ICU LOS (Table 6).
Discussion
We have successfully investigated variables related to timing and amount of physical therapy for select patient subgroups in a CT ICU. Our results indicate that timing and amount of physical therapy is more strongly correlated to procedure or medical intervention during hospitalization than to patient comorbidity. In addition, time to first PT session, mean days of PT, CCI, mean days of ventilation, and age explained large variability of hospital LOS for patients in the subgroups examined and of these, mean days of mechanical ventilation show the highest correlation.
Patients in the CT ICU experience shorter time to first PT evaluation and treatment compared to the time to first PT evaluation and treatment while on a hospital floor unit. This may reflect a practice culture signifying a strong commitment to mobilization of appropriate patients in this hospital’s CT ICU. At this facility, there has been a gradual increase in physical therapist or physical therapist assistant presence in the CT ICU and cardiothoracic floor units over the study timeframe. We hypothesize that barriers to physical therapy at hospital admission or in the Emergency Department exist that prevent CT ICU patients from receiving earlier PT evaluation and treatment before they are admitted to the CT ICU. Patients experiencing a delay in transfer to the CT ICU where PT evaluation and treatment appears to begin sooner may be at higher risk for immobility and development of weakness prior to surgical intervention. Immobility and functional decline during hospitalization has negative consequences, which can include prolonged LOS11,31. Further study is required to determine whether patients admitted directly to the CT ICU or more quickly receiving PT evaluation and treatment on other units could improve patient outcomes after CT surgery or mechanical ventilation through pre-habilitation.
Patients post lung transplantation experienced the shortest time to PT evaluation in the CT ICU, yet it was not significantly different from patients post VAD, CABG and Valve surgery. These patients have the second highest CCI score in the data, which was found to be different from those patients post CABG and Valve surgery. Interestingly, patients post lung transplant had mechanical ventilation needs that differed from patients post CABG, Valve or heart transplantation. Clearly, additional factors other than CCI and mechanical ventilation were influencing timing and amount of physical therapy treatment in these patients. Overall, studies have indicated that survival post lung transplantation is suboptimal with patients at high risk for adverse outcomes such as renal failure, malignancy, infection and poor quality of life48,49. The Center for Medicare and Medicaid Services closely monitors all transplant program outcomes, specifically for observed and expected mortality50. Programs are required to self-report their quality data to the Organ Procurement and Transplantation Network. For this reason, lung transplant program outcomes are scrutinized and program sustainability is an ongoing high priority for hospitals51. Our findings indicate that high risk post lung transplant patients receive physical therapy during acute critical illness and physical therapy ICU staff may have prioritized patients with lung transplantation. This contrasts starkly to the delay patients requiring more invasive cardiac intervention (VAD and heart transplant) experience in time to first PT evaluation in the hospital and in the CT ICU (heart transplant patients only). A reason for delay in time to first PT evaluation in patients post heart transplant or VAD implantation is beyond the scope of this manuscript, but we hypothesize it was related to delayed chest closure and initial cardiac hemodynamic instability after surgery. The reasons for open chest management are varied52, and have been associated with an increase in LOS53 and mechanical ventilation52. Despite the shorter time to first PT evaluation and treatment in patients post lung transplant, there was no statistically significant difference in hospital or CT ICU LOS between patients post lung transplant, post heart transplant, or post VAD. Similarly, mean days of PT during hospitalization were not significantly different between those three groups. Additional institutional factors that may have confounded the LOS data are individual physician practices in discharge from the ICU to the hospital floor and limitations in bed availability on hospital floor units. Future physical therapy research in the CT ICU should address the most effective and efficacious physical therapy interventions, including intensity, frequency and dosage for these subgroups to determine impact on LOS.
CT ICU LOS was not statistically significantly different for patients post CABG or Valve replacement surgery which may be explained by the similarities in average CCI score and mechanical ventilation requirements. However, overall hospital LOS difference suggests that once these patients leave the CT ICU, LOS trajectory is altered. One explanation may be related to mobility after patients are transferred to the floor. Critical care patients experience low mobility once transferred to floor units including delays in mobility or physical therapy treatment after transfer and in some cases regression in mobility level54,55,56. There may be differences in mobility level of patients post CABG and Valve surgery after transfer off the CT ICU, or differences in complication rates unable to be determined from this study.
Regression results showed that variables related to timing and amount of physical therapy (time to first PT, mean days of PT and mean days of mechanical ventilation) were highly correlated with hospital, and especially CT ICU LOS for patients post VAD, heart transplant and lung transplant. Additionally, the variables mean days of mechanical ventilation and mean days of PT were statistically significant in the three subgroup models with the largest Beta values. Mean days of mechanical ventilation explain a greater percentage of variability in hospital and CT ICU LOS. Enhanced management of mechanical ventilation and education about Acute Respiratory Distress Syndrome (ARDS) may be indicated. In a recent study of 50 ICUs nationally, clinician recognition of ARDS was poor as was the implementation of evidence-based therapy57. Frequently cited barriers to mobilization in the general ICU population include sedation and endotracheal intubation17,19. Examples of processes that streamline physical therapy consultation and mobility in the ICU for patients requiring mechanical ventilation include timing and coordination of spontaneous breathing trials with physical therapy assessments and changing sedation practices19 or sedation holidays in patients requiring prolonged mechanical ventilation. This is important knowledge for clinicians in the ICU because it indicates that clinical practice can be changed to influence LOS in these populations.
There are several limitations with this study. Using retrospective, administrative data limits the causality of our conclusions. The validity and reliability of ICD-9 CM diagnosis coding in administrative studies has been questioned, as the ICD-9 CM system was not designed for research purposes58. There are many factors related to the accuracy of coding including physician documentation, coder training and experience and ICD-9 code ambiguity42,58. When measuring physical therapy, we considered one day of PT as any day where patients’ had a physical therapy CPT code documented yet we are unable to determine the quantity of the CPT code (minutes) or which code was documented. Thus, we were unable to identify the amount of therapy or level of mobility achieved for patients each day. Without more description of the physical therapy activities or the intensity of physical therapy patients received, we were limited in determining factors associated with physical therapy practice. However, strong correlations were found in the variables chosen for this study.
This study represents a comprehensive analysis of variables related to physical therapy evaluation and treatment during CT ICU hospitalization. We found that timing and amount of physical therapy in patients with cardiac and respiratory illness differs more based on procedure required during hospitalization than on patient comorbidity. Timing and amount of physical therapy is associated with hospital and CT ICU LOS in this patient population. The data provided here indicate that variables such as time to first physical therapy evaluation in the ICU and the hospital, and mean days of physical therapy need to be considered in future prospective studies.
References
Perme, C. & Chandrashekar, R. Early mobility and walking program for patients in intensive care units: creating a standard of care. Am. J. Crit. Care 18, 212–221, https://doi.org/10.4037/ajcc2009598 (2009).
Adler, J. & Malone, D. Early mobilization in the intensive care unit: a systematic review. Cardiopulm. Phys. Ther. J. 23, 5–13 (2012).
Burtin, C. et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit. Care Med. 37, 2499–2505, https://doi.org/10.1097/CCM.0b013e3181a38937 (2009).
Herridge, M. S. et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N. Engl. J. Med. 348, 683–693, https://doi.org/10.1056/NEJMoa022450 (2003).
Herridge, M. S. et al. Functional disability 5 years after acute respiratory distress syndrome. N. Engl. J. Med. 364, 1293–1304, https://doi.org/10.1056/NEJMoa1011802 (2011).
Herridge, M. S. Legacy of intensive care unit-acquired weakness. Crit. Care Med. 37, S457–461, https://doi.org/10.1097/CCM.0b013e3181b6f35c (2009).
Gosselink, R. et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med. 34, 1188–1199, https://doi.org/10.1007/s00134-008-1026-7 (2008).
Cameron, S. et al. Early mobilization in the critical care unit: A review of adult and pediatric literature. J. Crit. Care 30, 664–672, https://doi.org/10.1016/j.jcrc.2015.03.032 (2015).
Engel, H. J., Tatebe, S., Alonzo, P. B., Mustille, R. L. & Rivera, M. J. Physical therapist-established intensive care unit early mobilization program: quality improvement project for critical care at the University of California San Francisco Medical Center. Phys. Ther. 93, 975–985, https://doi.org/10.2522/ptj.20110420 (2013).
Morris, P. E. et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit. Care Med. 36, 2238–2243, https://doi.org/10.1097/CCM.0b013e318180b90e (2008).
Needham, D. M. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA 300, 1685–1690, https://doi.org/10.1001/jama.300.14.1685 (2008).
Schweickert, W. D. et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 373, 1874–1882, https://doi.org/10.1016/s0140-6736(09)60658-9 (2009).
Hodgson, C. L., Berney, S., Harrold, M., Saxena, M. & Bellomo, R. Clinical review: early patient mobilization in the ICU. Crit. Care 17, 207, https://doi.org/10.1186/cc11820 (2013).
Bailey, P. et al. Early activity is feasible and safe in respiratory failure patients. Crit. Care Med. 35, 139–145, https://doi.org/10.1097/01.ccm.0000251130.69568.87 (2007).
Denehy, L. et al. Exercise rehabilitation for patients with critical illness: a randomized controlled trial with 12 months of follow-up. Crit. Care 17, R156, https://doi.org/10.1186/cc12835 (2013).
Bernhardt, J. et al. Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): a randomised controlled trial. Lancet 386, 46–55, https://doi.org/10.1016/s0140-6736(15)60690-0 (2015).
Harrold, M. E., Salisbury, L. G., Webb, S. A. & Allison, G. T. Early mobilisation in intensive care units in Australia and Scotland: a prospective, observational cohort study examining mobilisation practises and barriers. Crit. Care 19, 336, https://doi.org/10.1186/s13054-015-1033-3 (2015).
Bakhru, R. N., Wiebe, D. J., McWilliams, D. J., Spuhler, V. J. & Schweickert, W. D. An Environmental Scan for Early Mobilization Practices in U.S. ICUs. Crit. Care Med. 43, 2360–2369, https://doi.org/10.1097/ccm.0000000000001262 (2015).
Dafoe, S., Chapman, M. J., Edwards, S. & Stiller, K. Overcoming barriers to the mobilisation of patients in an intensive care unit. Anaesth. Intensive Care 43, 719–727 (2015).
Parry, S. M. et al. Factors influencing physical activity and rehabilitation in survivors of critical illness: a systematic review of quantitative and qualitative studies. Intensive Care Med. 43, 531–542, https://doi.org/10.1007/s00134-017-4685-4 (2017).
Barrett, M. L., Smith, M. W., Elixhauser, A., Honigman, L. S. & Pines, J. M. Utilization of Intensive Care Services, 2011. STATISTICAL BRIEF# 185, http://www.hcup-us.ahrq.gov/reports/statbriefs/sb185-Hospital-Intensive-Care-Units-2011.pdf (2014).
Jha, S. R. et al. The Prevalence and Prognostic Significance of Frailty in Patients With Advanced Heart Failure Referred for Heart Transplantation. Transplantation 100, 429–436, https://doi.org/10.1097/tp.0000000000000991 (2016).
Fukui, S. et al. Physical frailty in older people with severe aortic stenosis. Aging Clin. Exp. Res. 28, 1081–1087, https://doi.org/10.1007/s40520-015-0507-0 (2016).
Kreider, M. & Kotloff, R. M. Selection of candidates for lung transplantation. Proc. Am. Thorac. Soc. 6, 20–27, https://doi.org/10.1513/pats.200808-097GO (2009).
Kennedy, C. C., Mirza, S. & Wilson, M. E. The importance of frailty in lung transplantation and chronic lung disease. Current Pulmonology Reports 5, 145–151 (2016).
Singer, J. P. et al. Frailty Phenotypes, Disability, and Outcomes in Adult Candidates for Lung Transplantation. Am. J. Respir. Crit. Care Med. 192, 1325–1334, https://doi.org/10.1164/rccm.201506-1150OC (2015).
Rodes-Cabau, J. et al. Long-term outcomes after transcatheter aortic valve implantation: insights on prognostic factors and valve durability from the Canadian multicenter experience. J. Am. Coll. Cardiol. 60, 1864–1875, https://doi.org/10.1016/j.jacc.2012.08.960 (2012).
Schoenenberger, A. W. et al. Predictors of functional decline in elderly patients undergoing transcatheter aortic valve implantation (TAVI). Eur. Heart J. 34, 684–692, https://doi.org/10.1093/eurheartj/ehs304 (2013).
Malone, D. et al. Physical Therapist Practice in the Intensive Care Unit: Results of a National Survey. Phys. Ther. 95, 1335–1344, https://doi.org/10.2522/ptj.20140417 (2015).
Jette, D. U., Brown, R., Collette, N., Friant, W. & Graves, L. Physical therapists’ management of patients in the acute care setting: an observational study. Phys. Ther. 89, 1158–1181, https://doi.org/10.2522/ptj.20080338 (2009).
Hopkins, R. O., Spuhler, V. J. & Thomsen, G. E. Transforming ICU culture to facilitate early mobility. Crit. Care Clin. 23, 81–96, https://doi.org/10.1016/j.ccc.2006.11.004 (2007).
Korupolu, R., Gifford, J. M. & Needham, D. M. Early mobilization of critically ill patients. Contemporary Critical Care 6, 1–11 (2009).
Needham, D. M., Feldman, D. R. & Kho, M. E. The functional costs of ICU survivorship. Collaborating to improve post-ICU disability. Am. J. Respir. Crit. Care Med. 183, 962–964, https://doi.org/10.1164/rccm.201012-2042ED (2011).
Hodgson, C. L. et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit. Care 18, 658–658, https://doi.org/10.1186/s13054-014-0658-y (2014).
Needham, D. M. & Korupolu, R. Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Top. Stroke Rehabil. 17, 271–281, https://doi.org/10.1310/tsr1704-271 (2010).
Mendez-Tellez, P. A. et al. Factors associated with timing of initiation of physical therapy in patients with acute lung injury. J. Crit. Care 28, 980–984, https://doi.org/10.1016/j.jcrc.2013.06.001 (2013).
Leditschke, I. A., Green, M., Irvine, J., Bissett, B. & Mitchell, I. A. What are the barriers to mobilizing intensive care patients? Cardiopulm. Phys. Ther. J. 23, 26–29 (2012).
Rozenberg, D. et al. Thoracic muscle cross-sectional area is associated with hospital length of stay post lung transplantation: a retrospective cohort study. Transpl. Int.. https://doi.org/10.1111/tri.12961 (2017).
Humphrey, R., Buck, L., Cahalin, L. & Morrone, T. Physical Therapy Assessment and Intervention for Patients with Left Ventricular Assist Devices. Cardiopulm. Phys. Ther. J. 9, 3–7 (1998).
Bakhru, R. N., McWilliams, D. J., Wiebe, D. J., Spuhler, V. J. & Schweickert, W. D. Intensive Care Unit Structure Variation and Implications for Early Mobilization Practices. An International Survey. Ann Am Thorac Soc 13, 1527–1537, https://doi.org/10.1513/AnnalsATS.201601-078OC (2016).
van der Peijl, I. D. et al. Exercise therapy after coronary artery bypass graft surgery: a randomized comparison of a high and low frequency exercise therapy program. Ann. Thorac. Surg. 77, 1535–1541, https://doi.org/10.1016/j.athoracsur.2003.10.091 (2004).
Quan, H., Parsons, G. A. & Ghali, W. A. Validity of procedure codes in International Classification of Diseases, 9th revision, clinical modification administrative data. Med. Care 42, 801–809 (2004).
Dotson, P. CPT® Codes: What Are They, Why Are They Necessary, and How Are They Developed? Adv. Wound Care 2, 583–587 (2013).
Schneeweiss, S. et al. Performance of comorbidity scores to control for confounding in epidemiologic studies using claims data. Am. J. Epidemiol. 154, 854–864 (2001).
Quan, H. et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 43, 1130–1139 (2005).
Younis, M. Z. Length of hospital stay of Medicare patients in the post-prospective-payment-system era. J. Health Care Finance 31, 23–30 (2004).
Needham, D. M. et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch. Phys. Med. Rehab. 91, 536–542, https://doi.org/10.1016/j.apmr.2010.01.002 (2010).
Yusen, R. D. et al. The Registry of the International Society for Heart and Lung Transplantation: Thirtieth Adult Lung and Heart-Lung Transplant Report–2013; focus theme: age. J. Heart Lung Transplant. 32, 965–978, https://doi.org/10.1016/j.healun.2013.08.007 (2013).
Trulock, E. P. et al. Registry of the International Society for Heart and Lung Transplantation: twenty-fourth official adult lung and heart-lung transplantation report-2007. J. Heart Lung Transplant. 26, 782–795, https://doi.org/10.1016/j.healun.2007.06.003 (2007).
CMS. Medicare Program; Hospital Conditions of Participation; Requirements for Approval and Re-approval of Transplant Centers To Perform Organ Transplants; Final Rule. Fed. Regist. 72, 15198–15280 (2007).
McDiarmid, S., Pruett, T. & Graham, W. The oversight of solid organ transplantation in the United States. Am. J. Transplant. 8, 739–744 (2008).
Yanagida, R., Rajagopalan, N., Tribble, T., Bradley, M. & Hoopes, C. Routine Delayed Sternal Closure after Left Ventricular Assist Device Implantation with Vacuum Assisted Device. J. Heart Lung Transplant. 32, S281 (2013).
Stulak, J. M. et al. Delayed sternal closure does not increase late infection risk in patients undergoing left ventricular assist device implantation. J. Heart Lung Transplant. 31, 1115–1119 (2012).
Hopkins, R. O. et al. Physical therapy on the wards after early physical activity and mobility in the intensive care unit. Phys. Ther. 92, 1518–1523, https://doi.org/10.2522/ptj.20110446 (2012).
Pandullo, S. M. et al. Time for critically ill patients to regain mobility after early mobilization in the intensive care unit and transition to a general inpatient floor. J. Crit. Care 30, 1238–1242, https://doi.org/10.1016/j.jcrc.2015.08.007 (2015).
Salisbury, L. G., Merriweather, J. L. & Walsh, T. S. Rehabilitation after critical illness: could a ward-based generic rehabilitation assistant promote recovery? Nurs. Crit. Care 15, 57–65, https://doi.org/10.1111/j.1478-5153.2010.00382.x (2010).
Bellani, G. et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 315, 788–800, https://doi.org/10.1001/jama.2016.0291 (2016).
Gologorsky, Y., Knightly, J. J., Lu, Y., Chi, J. H. & Groff, M. W. Improving discharge data fidelity for use in large administrative databases. Neurosurg. Focus 36, E2, https://doi.org/10.3171/2014.3.focus1459 (2014).
Acknowledgements
We would like to thank Dr. Joan Darbee for her scientific expertise during the planning of this research and review of the manuscript prior to submission. We would also like to thank Andrew McLaughlin for his assistance with data collection, management and statistical analysis. The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1TR000117. This funding supported the data collection and assistance with data analysis during the study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
Audrey Johnson assisted in the conception of the study, performed data collection and statistical analysis, and developed the written manuscript. Angela Henning conceived the research study and assisted with writing the manuscript. Esther Dupont-Versteegden conceived the study, assisted with data interpretation and analysis and critically revised the manuscript. Peter Morris conceived the study, provided research guidance and critically revised the manuscript. Alejandro G. Villasante Tezanos performed statistical analysis and assisted in writing the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Johnson, A.M., Henning, A.N., Morris, P.E. et al. Timing and Amount of Physical Therapy Treatment are Associated with Length of Stay in the Cardiothoracic ICU. Sci Rep 7, 17591 (2017). https://doi.org/10.1038/s41598-017-17624-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-17624-3
This article is cited by
-
Using technology to increase the reach of educational innovation: globalization of a novel departmental journal club
Global Surgical Education - Journal of the Association for Surgical Education (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.