Abstract
Outdoor fine particulate air pollution (PM2.5) is known to increase mortality risk and is recognized as an important contributor to global disease burden. However, less is known about how oxidant gases may modify the chronic health effects of PM2.5. In this study, we examined how the oxidant capacity of O3 and NO2 (using a redox-weighted average, Ox) may modify the relationship between PM2.5 and mortality in the 2001 Canadian Census Health and Environment Cohort. In total, 2,448,500 people were followed over a 10.6-year period. Each 3.86 µg/m3 increase in PM2.5 was associated with nonaccidental (Hazard Ratio (HR) = 1.095, 95% CI: 1.077, 1.112), cardiovascular (HR = 1.088, 95% CI: 1.059, 1.118), and respiratory mortality (HR = 1.110, 95% CI: 1.051, 1.171) in the highest tertile of Ox whereas weaker/null associations were observed in the middle and lower tertiles. Analysis of joint non-linear concentration-response relationships for PM2.5 and Ox suggested threshold concentrations between approximately 23 and 25 ppb with Ox concentrations above these values strengthening PM2.5-mortality associations. Overall, our findings suggest that oxidant gases enhance the chronic health risks of PM2.5. In some areas, reductions in Ox concentrations may have the added benefit of reducing the public health impacts of PM2.5 even if mass concentrations remain unchanged.
Similar content being viewed by others
Introduction
Numerous studies have documented the relationship between long-term exposure to outdoor fine particulate air pollution (PM2.5) and mortality and these pollutants are recognized as important contributors to global disease burden1. However, PM2.5 is only one component of complex air pollution mixtures and it is not clear how/if the magnitude of PM2.5 health risks depend on concentrations of oxidant gases. This is an important question as populations are simultaneously exposed to both PM2.5 and oxidant gases (e.g. O3 and NO2) but it is not clear how the chronic health risks PM2.5 may depend on these other pollutants.
Crouse et al.2 recently examined multi-pollutant and cumulative-risk models for the relationship between PM2.5, NO2, O3, and non-accidental mortality and noted positive associations for all three pollutants; however, this study did not specifically evaluate how these oxidant gases may modify the chronic health effects of PM2.5. Nevertheless, existing evidence suggests that such effect modification is biologically plausible. For example, elevated O3 concentrations are known to deplete anti-oxidants in the lung lining fluid3 and increase the permeability of the lung epithelium4,5,6,7. Therefore, PM2.5 exposures may be more harmful in regions with increased levels of oxidant gases owing to decreased oxidant defense at the initial site of pulmonary deposition as well as a more permeable lung epithelial barrier.
In this study, we evaluated the extent to which oxidant gases may modify associations between outdoor PM2.5 mass concentrations and non-accidental, cardiovascular, and respiratory mortality in a large population-based cohort of Canadians. Our primary interest was in evaluating how the combined oxidant capacity of these gases (calculated using their redox-weighted average (Ox), described below) may potentiate PM2.5 health effects.
Results
Participant characteristics are summarized in Table 1. In total, 233,340 non-accidental, 77,000 cardiovascular, and 21,100 respiratory deaths were observed during the 10.6-year follow-up period. As expected, residential estimates of outdoor air pollution concentrations across Canada were low (Table 2) with PM2.5 concentrations ranging from approximately 1 to 20 µg/m3 with a mean value of 7.37 µg/m3. PM2.5 and Ox were moderately correlated (r = 0.66). Spatial variations in NO2, O3, Ox, and PM2.5 across Canada are shown in Supplemental Figures S1–S4.
Single Pollutant Models
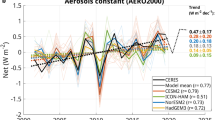
All four pollutants (PM2.5, NO2, O3, and Ox) were associated with increased nonaccidental, cardiovascular, and respiratory mortality in single pollutant models including linear terms for each pollutant (Table 3). Hazard ratios for Ox were generally higher than for O3 or NO2 individually except for respiratory mortality which was similarto that for NO2. For PM2.5, analyses across tertiles of Ox suggested consistently stronger associations in areas with higher oxidant gas concentrations for all three mortality outcomes (Fig. 1 and Supplemental Table 1). Similar trends were less apparent across tertiles of NO2 or O3 individually, particularly for O3; however, risks of nonaccidental and respiratory mortality did increase across tertiles of NO2 (Supplemental Table 2). The three-dimensional plots shown in Fig. 2 illustrate interactions across tertiles of PM2.5 and Ox for nonaccidental, cardiovascular, and respiratory mortality: for all three outcomes PM2.5-mortality associations were strongest in the highest tertile of Ox.
Three-dimensional plots of hazard ratios (HR) for (a) nonaccidental, (b) cardiovascular, and (c) respiratory mortality across tertiles of PM2.5 and Ox in CanCHEC 2001. Mean values across PM2.5 tertiles are 4.58 µg/m3 (1), 7.18 µg/m3 (2), and 10.35 µg/m3 (3). Mean values across Ox tertiles are 23.0 ppb (1), 29.2 (2), and 35.3 ppb (3).
Two Pollutant Models (PM2.5 and Ox)
When two-pollutant models were examined including linear terms for PM2.5 and Ox, hazard ratios for PM2.5 decreased for all three mortality outcomes but remained elevated. The largest change occurred for the hazard ratio between PM2.5 and cardiovascular mortality which decreased from 1.107 (95% CI: 1.089, 1.127) in the single pollutant model to 1.024 (95% CI: 1.004, 1.044) in the two-pollutant model. The best fitting model for cardiovascular mortality included PM2.5, Ox, and their interaction term (Table 4). For nonaccidental and respiratory mortality, model fit was similar between two pollutant models (i.e. containing PM2.5 and Ox) and models including both pollutants and their interaction term. The spatial distribution of PM2.5*Ox is presented in Fig. 3 and highlights that the highest combined concentrations of PM2.5 and Ox occur in the most populated areas of Ontario and Quebec and along the southern border of Canada.
Spatial distribution of PM2.5*Ox (ppb*μg/m3) across Canada. Map created in ArcGIS Desktop 10.0. ESRI, Redlands, CA (http://desktop.arcgis.com/en/arcmap/).
Joint Non-linear Models for PM2.5 and Ox
Effect modification by Ox was also apparent when we examined non-linear model forms for PM2.5 -mortality associations (Fig. 4). Specifically, the shapes of associations between Ox and θ (the parameter describing the magnitude of association between PM2.5 and mortality) were similar for all three causes of death (Fig. 4, panels a, c, and e) with threshold concentrations of 23.71 ppb, 25.08 ppb, and 25.13 ppb for cardiovascular, respiratory and nonaccidental mortality, respectively. The rate of change in θ per ppb of Ox above the threshold was greatest for cardiovascular mortality and similar for both non-accidental and respiratory mortality (λ values in the Supplemental Methods). Figure 4 (panels b, d, and e) illustrates non-linear concentration response relationships for PM2.5 and nonaccidental, cardiovascular, and respiratory mortality at Ox concentrations of 20.26 ppb (red solid line) and 37.6 ppb (blue solid line) which represent mean concentrations in the first and tenth deciles respectively of the Ox distribution. This Figure clearly illustrates considerable variations in PM2.5-mortality associations at these two Ox concentrations.
Predicted values (solid blue line) of \(\hat{\theta }(O{}_{x})=\hat{\eta }+\hat{\lambda }{({O}_{x}-\omega )}_{+}\) by cause of death with uncertainty bounds (shaped gray area) (panels a, c, and e). Predicted values of \(R(P{M}_{2.5})={(1+P{M}_{2.5})}^{\hat{\theta }({O}_{x})/(1+\exp (-z/2))}\) for Ox = 37.60 ppb (solid blue line) and Ox = 20.26 ppb (solid red line) with uncertainty intervals (dashed lines) (panels b, d, f).
Finally, Fig. 5 highlights areas of Canada with estimated Ox concentrations above 23 ppb. Based on the evidence above, reductions in Ox concentrations in these regions are expected to reduce the chronic health effects of PM2.5 even if mass concentrations remain unchanged.
Regions of Canada with estimated Ox concentrations above 23.0 ppb. Reductions in Ox concentrations in these areas are expected to decrease the chronic health risks of PM2.5 even if mass concentrations remain unchanged. Map created in ArcGIS Desktop 10.0. ESRI, Redlands, CA (http://desktop.arcgis.com/en/arcmap/).
Discussion
To our knowledge, this is the first large population-based cohort study to evaluate how oxidant gases may modify the chronic health risks of PM2.5. In general, our findings suggest that oxidant gases act to enhance PM2.5-mortality associations and that this effect modification occurs at Ox concentrations above approximately 23 ppb. This finding should be confirmed in future cohort studies as to our knowledge this study is the first to report such a relationship. If confirmed, these findings are important as they indicate that in some areas reductions in Ox concentrations may have the added benefit of reducing the public health impacts of PM2.5 even if mass concentrations remain unchanged.
While other studies have not examined the impact of oxidant gases on the chronic health effects of PM2.5, we previously reported that Ox modified the association between short-term changes in ambient PM2.5 and the risk of emergency room visits for myocardial infarction8. In addition, others have reported associations between daily variations in Ox and mortality in London, England9. One possibility is that spatial variations in Ox concentrations are reasonable surrogates for the presence/absence of harmful air pollution mixtures and/or sources that are more relevant to health and thus PM2.5 in these regions tends to be more harmful. However, other biological mechanisms may also explain our observation of stronger PM2.5-mortality associations in regions with higher Ox concentrations. First, ozone rapidly saturates the lung epithelial lining fluid where it degrades surfactants and depletes anti-oxidants; thus, oxidant gases may reduce our natural defense against reactive oxygen species generated in response to PM2.5 components including transition metals, polycyclic aromatic hydrocarbons, or quinones3,10. In addition, ozone increases the permeability of the lung epithelium barrier4,5,6,7 and thus may facilitate the translocation of particles (or inflammatory proteins) from the lungs directly into the systemic circulation. Moreover, endogenous sources of oxidative stress may also pay an important role as NO2 has been shown to induce the release of reactive oxygen species from alveolar macrophages11. Alternatively, photochemical aging of PM2.5 has been shown to increase the oxidative potential of particles themselves12,13; therefore, this process may also contribute to our observation of stronger PM2.5-mortality associations in regions with higher oxidant gas concentrations as photochemical oxidation would be greater in these areas.
One interesting finding in our investigation was that the rate of change in θ (the parameter describing the magnitude of association between PM2.5 and mortality) per ppb of Ox above the threshold was greater for cardiovascular mortality than respiratory mortality. One explanation for this finding may be that PM2.5 components and/or inflammatory mediators must first reach the systemic circulation from the lung in order to contribute to cardiovascular morbidity. If this process happens more quickly/efficiently at higher Ox concentrations (perhaps owing to increased lung permeability as noted above) this may explain the larger slope for θ in cardiovascular mortality. While we could not directly evaluate this question in the current study, future studies should aim to replicate this result as it may contribute to our understanding of how particulate air pollution influences cardiovascular morbidity/mortality.
This study had several important advantages including a large population-based sample of Canadians, exposure information for multiple air pollutants updated for residential mobility, detailed non-linear concentration-response modeling, and individual-level information on many important socio-economic factors. However, we cannot rule out potential confounding by unmeasured variables including smoking and obesity. In addition, as in all large scale epidemiological studies, exposure measurement error is a challenge and likely impacted our results. Specifically, the spatial scale of O3 estimates was large and greater resolution is needed to refine or assessment of the spatial distribution of Ox (and PM2.5*Ox) and associated health impacts. In general, measurement error for all air pollutants likely contained components of both Classical (i.e. grid-cell mean values distributed around true long-term ambient concentrations) and Berkson-type error (i.e. true individual-level exposures distributed around grid-cell mean values). Classical type error would tend to bias risk estimates toward the null whereas Berkson type error would tend to increase uncertainty in our estimates (i.e. wider confidence intervals). In either case, this error is not a likely explanation for our observed pattern of stronger PM2.5-mortaltiy associations in areas with higher Ox concentrations. Moreover, it is important to note that there is no clear consensus on the optimal spatial scale at which to evaluate long-term exposures to outdoor air pollution. Currently, the same spatial scale is applied to all cohort members but a more optimal approach may be to tailor the spatial scale of exposure assessment to match the size of individual-level activity spaces based on individual-level covariates such as age, sex, or socioeconomic status (e.g. older people may spend more time at home and thus a smaller spatial scale may be more appropriate for older cohort members). In some cases, larger spatial scales may be more appropriate if cohort members are highly mobile within their region and thus larger grid sizes are not necessarily a limitation. Nevertheless, more work is needed to refine air pollution exposure assessment in large population-based studies and our future work will aim to address several of these issues.
In summary, the results of our cohort study suggest that oxidant gases may act to enhance the chronic health impacts of PM2.5. If confirmed, our findings may provide additional flexibility for regulators/risk managers in reducing the overall public health impacts of PM2.5. In particular, there may be important co-benefits to reducing Ox as reductions in oxidant gas concentrations may also reduce the chronic health impacts of PM2.5 even if mass concentrations remain unchanged. The choice of which pollutant(s) to target in a given area will likely be situation-specific; however, knowledge of how oxidant gases and PM2.5 may interact to cause adverse health impacts could improve the efficiency of risk management activities and ultimately public health.
Methods
Study Population
This study uses the 2001 Canadian Census Health and Environment Cohort (CanCHEC) described in Pinault et al.14. Briefly, the 2001 Census long-form questionnaire was distributed to approximately 20% of Canadian households including 4,500,200 Census respondents aged 19 years or older who did not reside in institutions and who lived in Canada15. Of these, 78.6% (n = 3,537,500) were linked to income tax files to obtain annual postal code histories and Social Insurance Numbers through standard deterministic and probabilistic linkage techniques16. These subjects were then deterministically linked to the Amalgamated Mortality Database using Social Insurance Numbers. All deaths that occurred between census day (May 15, 2001) and December 31, 2011 were eligible for linkage.
Respondents who were not assigned air pollution estimates due to living outside the boundaries of air pollution models were excluded (n = 86,100) as were those less than 25 years of age or older than 90 years (n = 319,900 additional persons excluded). All immigrants were also excluded from the cohort (n = 683,100) since their previous air pollution exposures were unknown. The final analytical sample was 2,448,500 respondents: sample sizes are rounded to the nearest hundred for confidentiality.
Postal code histories obtained from tax records were used to geocode respondent addresses. Statistics Canada’s Postal Code Conversion File plus (PCCF+) v.6c uses a population-weighted random allocation algorithm to assign geographic coordinates to postal codes based on centroids of different scales of Census geography17. The gaps in postal code reporting (approximately 18% of all person-years) were imputed using a probabilistic imputation method developed at Statistics Canada, which assigned postal code common characters from postal codes provided before and after the gap in reporting18. The method included a non-null probability that missing postal codes would be different from adjacent years, and the probability of non-matches increased with increasing gap length. In cases where postal codes were not imputed using any common characters, the national mean exposure estimate was assigned. In a validation exercise with the 1991 CanCHEC, when 5% of postal codes were randomly deleted and then imputed using the program, 4.2% of imputed postal codes had an absolute PM2.5 difference greater than 0.1 μg/m3 18. In general, 2001 CanCHEC members were more likely to be married or common-law, have higher income or higher educational attainment, or be employed than were the general Canadian population14.
Exposure Assessment
Cohort members were assigned air pollution exposure estimates for PM2.5, NO2, and O3 using models that have been previously described. Specifically, PM2.5 exposures were derived from a surface model that combines information for total column aerosol optical depth retrievals from the Moderate Resolution Imaging Spectroradiometer (MODIS) with near-surface PM2.5 emissions estimated from the GEOS-Chem chemical transport model19. Yearly (2012 to 2014) average surface layers of PM2.5 (at 1 km2 resolution) were obtained by applying geographically weighted regression, and extended back in time to 1998 by applying inter-annual variation from a published model20. Within North America, mean PM2.5 estimates were strongly correlated with ground level measurements (R2 = 0.82, slope = 0.97, n = 1440)19. Estimates of PM2.5 that were greater than 20 μg/m3 were excluded from the analysis because they likely represented inaccurate satellite retrievals.
Outdoor NO2 concentrations were estimated using the 2006 annual mean from a national land use regression model that used National Air Pollution Surveillance (NAPS) fixed-site monitoring data combined with satellite NO2 estimates, road length within 10 km, industrial land use areas within various buffers, and mean summer rainfall21. Ground-level NO2 estimates were derived using GEOS-Chem from satellite tropospheric NO2 columns22. During validation, the model explained 73% of the variance in 2006 NAPS estimates. Local variation in NO2 was captured by applying kernel density measures of highways and major roads as a multiplier to the model21.
A surface for average daily 8-hr maximum O3 concentration was generated for the months of May to October for the period of 2002 to 2009 using an air pollution-specific interpolation technique to generate a 21 km2 grid2,23. This method incorporates modeled O3 from the Canadian Hemispheric Regional Ozone and NOx system (CHRONOS) air quality forecast model24 with observations from Canada and the United States.
All NO2 and ozone data were year-adjusted using ground-based time-series measurements from 24 Census Divisions (CD)s between 1981 and 2012. The time series for NO2 and O3 were derived from NAPS daily average concentrations (if at least 18 hourly concentrations were recorded in a day), and averaged for CDs with more than one monitoring station25. Missing time-series data were imputed using an interpolation algorithm that combines classical prediction techniques and the phase-and frequency-fitting tools via the multi-taper method using the R package tsinterp 26. For each CD time-series, a cubic spline was fitted to model the association between year and air pollutant concentration. Then, the ratio between the year of the original modeled data (i.e., NO2: 2006, O3: mean of 2002 to 2009) and all years of follow-up was determined. For each year of follow-up, residence locations for cohort members were matched to the closest CD in Geographic Information Systems (ArcGIS v.10, ESRI 2010), and the corresponding time adjustment ratio was used to adjust data for annual differences in concentration. All air pollution exposures were assigned using 3-year moving averages with a 1-year lag time (and updated for residential mobility).
Finally, the combined oxidant capacity (Ox) of O3 and NO2 at each residential location was calculated as a weighted average with weights equivalent to their respective redox potentials (i.e. Ox = [(1.07 × NO2) + (2.075 × O3)]/3.145)27.
Statistical Analyses
Standard Cox proportional hazards models were used to estimate hazard ratios (HR) and 95% confidence intervals (95% CI) describing the relationship between outdoor air pollutants and nonaccidental (ICD-10: A to R), cardiovascular (ICD-10: I10-69 and E10-E14 (diabetes)), and respiratory mortality (ICD-10: J00-J99). All models were stratified by age (5-year categories), sex, airshed, and population centre size, and adjusted for individual-level covariates including visible minority status, Aboriginal status, marital status, educational attainment, income quintile, and labour force status. In addition, several neighbourhood-level covariates were included in the models including percent unemployed (aged 25 and older), percent not graduated from high school (aged 25 and older), and percent low income status within census divisions as well as population density (per km2) within dissemination areas (Table 1). All hazard ratios for individual pollutants are expressed for intervals equivalent to the difference between the mean and the 5th percentile of each pollutant. Hazard ratios for the product of PM2.5 and Ox are expressed per 100 ppb*µg/m3.
A series of models were examined to evaluate how oxidant gases may modify the relationship between PM2.5 and mortality. First, single pollutant models were examined using linear terms for PM2.5, NO2, O3, and Ox (as defined above). Hazard ratios for PM2.5 were then calculated across tertiles of Ox to evaluate trends in PM2.5-mortality associations at increasing concentrations of oxidant gases; the entire range of PM2.5 concentrations (i.e. 1–20 µg/m3) was available within each tertile of Ox. Three-dimensional plots were also examined for hazard ratios across tertiles of Ox and PM2.5.
Next, two pollutant models including both PM2.5 and Ox were examined to evaluate potential confounding by Ox in PM2.5-mortality associations followed by: 1) models including only the product of PM2.5 and Ox (i.e. PM2.5*Ox); 2) models including PM2.5 and the product of PM2.5 and Ox (i.e. PM2.5 + PM2.5*Ox); and 3) models including PM2.5, Ox, and product of PM2.5 and Ox (i.e. PM2.5 + Ox + PM2.5*Ox). Our primary aim in evaluating this series of models was to examine how Ox may modify the relationship between PM2.5 and mortality using linear terms for individual pollutants both excluding and including the main effect of Ox. Following the above analyses, we considered non-linear model forms to characterize potential effect modification due to Ox on PM2.5-mortality associations as outlined below.
The traditional relative risk function used to relate PM2.5 concentrations to mortality is: \(R(P{M}_{2.5})=\) \(\exp \{\theta \times P{M}_{2.5}\}\) with θ representing the logarithm of the relative risk for a unit change in PM2.5, assuming a linear relationship between PM2.5 and the logarithm of the relative risk. This model has been extended to include non-linear model specifications of the form: \(R(P{M}_{2.5})=\exp \{\theta \times T(P{M}_{2.5})\}\),where T(PM 2.5) is a monotonic transformation of PM2.5 28,29. Here, θ represents the logarithm of the relative risk for a unit change in T(PM 2.5). Setting \(T(P{M}_{2.5})=\mathrm{log}(\Im (P{M}_{2.5}))/1+\exp (-(P{M}_{2.5}-\mu )/\pi )\), where \(\Im (z)={e}^{z}\) or \(\Im (z)=1+z\), specifies a family of shapes taking supra-linear, near-linear, sub-linear and sigmodal forms depending on \((\Im ,\mu ,\pi )\).
In this study, we examined how mortality risks due to PM2.5 exposures may be affected by co-occurring exposure to Ox. To do this, we introduced the notion that the parameter θ can vary with concentrations of Ox by defining a joint relative risk function of the form: \(R(P{M}_{2.5},{O}_{x})=\exp \{\theta ({O}_{x})\times T(P{M}_{2.5})\}\). We additionally postulated that there exists a concentration of Ox, ω, below which, Ox does not modify the risk of death due to PM2.5 exposure and above that concentration there exists a linear association. That is: \(\theta ({O}_{x})=\eta +\lambda \times {({O}_{x}-\omega )}_{+}\), such that \({({O}_{x}-\omega )}_{+}=0\) if O x < ω and \({({O}_{x}-\omega )}_{+}=({O}_{x}-\omega )\) if \({O}_{x}\ge \omega \), for concentration ω. It is important to note that this model does not directly evaluate the impact of Ox on mortality; rather, it redistributes PM2.5 risk according to concentrations of Ox. Methods to estimate the unknown parameters and their uncertainty are presented in the Supplemental Material.
All statistical analyses were conducted using R version 3.2.4 and SAS version 9.3. Map Figures were created in ArcGIS 10.0 (ESRI, 2010). NO2 and O3 surfaces were created using interpolation (i.e. inverse distance weighted) from nationally representative NO2 and O3 point estimates, and raster algebra was used to calculate OX and the product of OX and PM2.5 using published PM2.5 surfaces19. All data are available through the Statistics Canada Research Data Centers located across Canada conditional on the necessary institutional approvals from Statistics Canada including security screening.
Institutional Approvals
The Canadian Census Health and Environment Cohort (CanCHEC) was approved by the Statistics Canada Policy Committee (reference number 012-2001) after consultation with the Statistics Canada Confidentiality and Legislation Committee, Data Access and Control Services Division, and the Federal Privacy Commissioner. This approval is equivalent to that of standard research ethics boards.
References
GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1659–724 (2016).
Crouse, D. L. et al. Ambient PM2.5, O3, and NO2 exposures and associations with mortality over 16 years of follow-up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ. Health Perspect. 123, 1180–1186 (2015).
Lakey, P. S. J. et al. Chemical exposure-response relationship between air pollutants and reactive oxygen species in the human respiratory tract. Sci Rep 6, 32916 (2016).
Broeckaert, F. et al. Serum clara cell protein: a sensitive biomarker of increased lung epithelium permeability caused by ambient ozone. Environ. Health Perspect. 108, 533–537 (2000).
Blomberg, A. et al. Clara cell protein as a biomarker for ozone-induced lung injury in humans. Eur. Respir. J. 22, 883–888 (2003).
Ciencewicki, J., Trivedi, S. & Kleeberger, S. R. Oxidants and the pathogenesis of lung diseases. J. Allergy Clin. Immunol. 122, 456–468 (2008).
Georas, S. N. & Rezaee, F. Epithelial barrier function: at the front line of asthma immunology and allergic airway inflammation. J. Allergy Clin. Immunol. 134, 509–520 (2014).
Weichenthal, S., Lavigne, E., Evans, G., Pollitt, K. & Burnett, R. T. Ambient PM2.5 and risk of emergency room visits for myocardial infarction: impact of regional PM2.5 oxidative potential: a case-crossover study. Environ Health 15, 46 (2016).
Williams, M. L., Atkinson, R. W., Anderson, H. R. & Kelly, F. J. Associations between daily mortality in London and combined oxidant capacity, ozone and nitrogen dioxide. Air Qual. Atmos. Health 7, 407–414 (2014).
Crobeddu, B., Aragao-Santiago, L., Bui, L. C., Boland, S. & Squiban, A. B. Oxidative potential of particulate matter 2.5 as predictive indicator of cellular stress. Environ. Pollut. 230, 125–133 (2017).
Kienast, K., Knorst, M., Lubjuhb, S., Muller-Quernheim, J. & Ferlinz, R. Nitrogen dioxide-induced reactive oxygen intermediates production by human alveolar macrophages and peripheral blood mononuclear cells. Arch. Environ. Health 49, 246–250 (1994).
Rattanavaraha, W. et al. The reactive oxidant potential of different types of aged atmospheric particles: an outdoor chamber study. Atmos Environ 45, 3848–3855 (2011).
Saffari, A., Daher, N., Shafer, M. M., Schauer, J. J. & Sioutas, C. Global perspective on the oxidative potential of airborne particulate matter: a synthesis of research findings. Environ. Sci. Technol. 48, 7576–7583 (2014).
Pinault, L., Finès, P., Labrecque-Synnott, F., Saidi, A. & Tjepkema, M. The Canadian Census-Tax-Mortality cohort: a 10-year follow-up. Statistics Canada. Anal. Stud. Meth. Ref. No. 11-633-X. no. 003 (2016).
Statistics Canada. 2001 Census Dictionary. Statistics Canada. Cat No. 92–378-XIE (2003).
Fellegi, I. P. & Sunter, A. B. A theory for record linkage. J. Am. Stat. Assoc. 64, 1183–1210 (1969).
Statistics Canada. Postal CodeOM Conversion File Plus (PCCF+) Version 6C, Reference Guide. Statistics Canada, Cat no. 82-F0086-XDB (2016).
Finès, P., Pinault, L. & Tjepkema, M. Imputing postal codes to analyze ecological variables in longitudinal cohorts: exposure to particulate matter in the Canadian Census Health and Environment Cohort Database. Statistics Canada. Anal. Stud. Meth. Ref. Cat. 11-633-X (2017).
van Donkelaar, A., Martin, R. V., Spurr, R. J. D. & Burnett, R. T. High resolution satellite-derived PM2.5 from optical estimation and geographically weighted regression over North America. Environ. Sci. Technol. 49, 10482–10491 (2015).
Boys, B. L. et al. Fifteen-year global time series of satellite-derived fine particulate matter. Environ. Sci. Technol. 48, 11109–11118 (2014).
Hystad, P. et al. Creating national air pollution models for population exposure assessment in Canada. Environ. Health Perspect. 119, 1123–1129 (2011).
Lamsal, L. et al. Ground-level nitrogen dioxide concentrations inferred from the satellite-borne ozone monitoring instrument. J. Geophys. Res. 113, D15308 (2008).
Robichaud, A. & Ménard, R. Multi-year objective analyses of warm season ground-level ozone and PM2.5 over North America using real-time observations and the Canadian operational air quality models. Atmosph. Chem. Phys. 14, 1769–1800 (2014).
Pudykiewicz, J. A., Kallaur, A. & Smolarkiewicz, P. K. Semi-Lagrangian modelling of tropospheric ozone. Tellus. B. Chem. Phys. Meteorol. 49, 231–248 (1997).
Shin, H. H., Stieb, D., Burnett, R., Takahara, G. & Jessiman, B. Tracking national and regional spatial-temporal mortality risk associated with NO2 concentrations in Canada: a Bayesian hierarchical two-level model. Risk. Anal. 32, 513–530 (2012).
Burr, W. Tsinterp: A time series interpolation package for R (v0.2-0). Available online: (http://github.com/wesleyburr/tsinterp) (2015).
Bratsch, S. G. Standard electrode potentials and temperature coefficients in water at 298.15 K. Vol. 18, No.1, 1–21. Available https://www.nist.gov/sites/default/files/documents/srd/jpcrd355.pdf (1989).
Nasari, M. et al. A Class of Non-Linear Exposure-Response Models Suitable for Health Impact Assessment Applicable to Large Cohort Studies of Ambient Air Pollution. Air Qual. Atmos. Health 9, 961–972 (2016).
Pinault, L. L. et al. Associations between fine particulate matter and mortality in the 2001 Canadian Census Health and Environment Cohort. Environ. Res. 159, 406–415 (2017).
Acknowledgements
We would like to acknowledge Drs. Randall Martin, Aaron van Donkelaar, Jeff Brook, and Perry Hystad for developing the exposure models used in estimate ambient air pollution concentrations in our analyses and Dr. Hwashin Shin for preparing the dataset used to year-adjusted O3 and NO2 data. We would also like to thank Drs. Eric Lavigne and Dave Stieb for their comments in reviewing the manuscript. Dr. Weichenthal received support from a GRePEC salary award funded by the Cancer Research Society, the Quebec Ministry of Economy, Science and Innovation, and FRQS (Fonds de Recherche du Québec- Santé).
Author information
Authors and Affiliations
Contributions
S.W. was the lead author and wrote the main manuscript text and prepared Fig. 1. L.P. and R.B. conducted all statistical analyses and contributed to writing the methods section of the manuscript. L.P. prepared Figs 2, 3, and 5 and Supplemental Figures S1–S4. R.B. prepared Fig. 4.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weichenthal, S., Pinault, L.L. & Burnett, R.T. Impact of Oxidant Gases on the Relationship between Outdoor Fine Particulate Air Pollution and Nonaccidental, Cardiovascular, and Respiratory Mortality. Sci Rep 7, 16401 (2017). https://doi.org/10.1038/s41598-017-16770-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-16770-y
This article is cited by
-
Air pollution and retinal vessel diameter and blood pressure in school-aged children in a region impacted by residential biomass burning
Scientific Reports (2021)
-
Road proximity, air pollution, noise, green space and neurologic disease incidence: a population-based cohort study
Environmental Health (2020)
-
Acute cardiovascular health effects in a panel study of personal exposure to traffic-related air pollutants and noise in Toronto, Canada
Scientific Reports (2020)
-
Low concentrations of fine particle air pollution and mortality in the Canadian Community Health Survey cohort
Environmental Health (2019)
-
Low Levels of Air Pollution and Health: Effect Estimates, Methodological Challenges, and Future Directions
Current Environmental Health Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.