Abstract
The current study was designed to explore the epidemiology of extremities chronic osteomyelitis, its prognosis and the complications of the treatment methods being used in southwest China. The data from osteomyelitis patients treated at the Department of Orthopaedics, Southwest Hospital, China between May 2011 and September 2016 were collected and analysed. The study comprised 503 admitted patients, of which 416 males and 87 were females, with an average age of 40.15 ± 5.64 years. Approximately 356 cases were followed for more than 18 months; the average bone union time was 6.24 ± 0.76 months in 94.1% (335) patients, and infections were almost controlled in 93.8% patients. The rate of infection control with the induced membrane technique was higher than with the I-stage free bone graft. Iliac infection was the main complication of the induced membrane technique, and impaired joint activity was the main complication of I-stage free bone grafts. In southwest China, the incidence of haematogenous osteomyelitis, caused mainly by Staphylococcus aureus, remains very high. The speed of bone defect repair and the rate of infection control with the induced membrane technique were superior to those of I-stage free bone grafts. Internal fixation should be given priority because it offers reduced complications with no increase in the recurrence of infection.
Similar content being viewed by others
Introduction
Osteomyelitis is a severe bone infection that results from various aetiologies and mechanisms1. With recent advancements in surgical techniques, the incidence of haematogenous osteomyelitis has decreased markedly, while the incidence of post-traumatic osteomyelitis has remained at higher levels. The incidence of osteomyelitis in the American population during the last decade (2000–2009) was twice that of 40 years ago2. Recent changes in the epidemiology, pathogenesis, diagnosis, treatment, and prognosis of this disease have varied according to population3,4. Clinical signs of osteomyelitis are diverse and are probably altered by geography, lifestyle and the quality of available medical services5,6,7. The phalanges bones are frequently affected8, particularly in African populations, but in many other countries, the most susceptible bones are the tibia or femur1,9,10. During a survey spanning 2005 to 2012, the incidence of acute haematogenous osteomyelitis (AHO) in southern Israel was 5.6:100,000, but in the Bedouin and Jewish populations, the incidences were 7.3 and 4.1:100,000, respectively10. Chronic bone infections are more often linked with diverse bacterial biofilms11.
China has a rich diversity of populations, climates, and lifestyles. Southwest China is underdeveloped in terms of economic growth compared with coastal China, and its very cloudy and humid climate offers a desirable niche for diverse microbial growth. In terms of osteomyelitis, southwest China is characterised by several features: i) the incidence of osteomyelitis is considerably higher than in other parts of China, ii) there is a shortage of well-trained physicians specialized in addressing bone infections, and iii) patients are forced to seek treatment in a few select hospitals. There are few prominent hospitals, which lack relevant reports and authentic data. In this context, we aimed to explore the clinical characteristics of osteomyelitis in southwest China and to observe the treatment and prognosis of this disease.
Methods
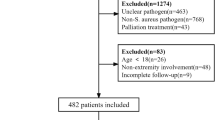
A retrospective analysis of 503 osteomyelitis patients admitted to the Department of Orthopaedics, Southwest Hospital, China, from May 2011 to September 2016 was performed. We followed patients who met the diagnosis of osteomyelitis through the electronic medical records system to collect their basic information, history, clinical manifestations, auxiliary examinations, treatment, prognosis and complications.
Inclusion criteria
patients diagnosed with osteomyelitis based on the following criteria: local bone pain and swelling on examination, draining fistula, imaging procedures, microbiological and histopathological examinations, and biochemical examinations.
Exclusion criteria
patients with acute osteomyelitis (less than 2 weeks); patients without surgical treatment; osteomyelitis in the spine, pelvis and skull; patients with incomplete data; and patients with diabetic foot infection who were not treated in our department. Finally, 503 patients were selected. Of these, 320 were treated with the induced membrane two-stage technique, and 183 were treated with I-stage free bone grafts (bone grafts after debridement); no other methods were used in this study. Intravenous antibiotic therapy was applied for approximately 2 weeks post operation, third-generation cephalosporin (ceftazidime or cefpiramide) was administered to patients with a negative culture, and no patient received oral antibiotic treatment. Standard follow-up was performed every three months to observe infection control, bone healing and complications. The Ethics Committee of Southwest Hospital, Third Military Medical University Chongqing, China, approved this study, and any related procedures were performed in accordance with relevant guidelines and regulations.
Ethics approval and informed consent
Ethics approval was obtained from the Southwest Hospital, Third Military Medical University Ethics Committee. All the participants gave their written informed consent.
Statistics
Numerative data (sites, sinus, complications) were compared using Pearson’s chi-square test or Fisher’s exact test, while measurement data (age, levels of inflammation markers, bone union time) were compared using the t test or rank-sum test. Relevant risk factors were analysed using logistic regression analysis; to compare the influence of fixators on prognosis, we used one-way ANOVA or the chi-square test. P values below 0.05 were considered significant.
Results
There were 503 patients, including 416 males and 87 females, with an average age of 40.15 ± 5.64 years. The average number of previous operations was 2.33 ± 0.22; 2.60 ± 0.27 times for those with post-traumatic osteomyelitis and1.14 ± 0.20 times for those with haematogenous osteomyelitis. The average duration of infection was 62.91 ± 11.38 months. The 503 patients experienced infections in 510 sites; the rate of sinus infection was 69.2% (353/510) and was higher among the post-traumatic osteomyelitis patients than among those with haematogenous osteomyelitis (P < 0.01). Forty-one patients had type 2 diabetes or other systemic adverse factors, 15 patients had varicose veins or other local adverse factors, and 169 patients had a history of smoking; the data are presented in Table 1. The use of contiguous seeding based on skin lesions, the number of cases was kept small enough to tabulate.
Infection site
Among the 496 cases with a single-site infection, there were 285 cases of tibia infection, 133 femur infections, 13 ulna and radius infections, 14 humerus infections, 11 fibula infections, 15 calcaneus infections, 7 clavicle infections, 6 metatarsal infections, 5 infections of the toes, 4 patella infections, and 3 phalanx infections. Seven patients had multiple ipsilateral infection sites. A total of 408 sites were infected in the post-traumatic osteomyelitis patients compared with 91 sites in the haematogenous osteomyelitis group. The right side accounted for 47.1% of the total infection sites, and the left side accounted for 52.9%.
Classification
According to the Waldvogel classification, there were 403 cases (80.1%) of post-traumatic osteomyelitis, 90 cases (17.9%) of haematogenous osteomyelitis and 10 (2%) contiguous seedings from skin lesion infections. Of the post-operative traumatic osteomyelitis cases, 244 (60.5%) infections resulted from open fractures, 148 (36.7%) were post-operative infections after a closed fracture, and the mechanism of injury was unknown in 11 cases. According to the Cierny-Mader classification for 496 cases of single-site infection, sixty-seven cases (13.5%) were classified as type I, 56 cases (11.3%) as type II, 129 cases (26.0%) as type III and 244 cases (49.2%) as type IV.
Laboratory test
Thirty-seven patients (7.4%) had a body temperature higher than 37.1 °C, 85 (16.9%) had a white blood cell count (WBC) greater than 10 000/μL, 218 (43.3%) had C-reactive protein (CRP) levels greater than 10 mg/L, and 209 (41.6%) had an erythrocyte sedimentation rate (ESR) greater than 20 mm/hr. Only 55 patients (10.9%) were positive for all three inflammation markers, and the positive rate was higher among the haematogenous osteomyelitis group than among the post-traumatic osteomyelitis group (Table 1). The positive rates for WBC and body temperature among patients without sinus infection were 26.0% and 11.3%, respectively, which were higher than for those with sinus infection (13% and 5.7%, respectively; P < 0.01 and P = 0.023), while the differences in ESR and CRP were not statistically significant.
Pathogenic microorganism
A total of 467 patients (92.8%) had a history of antibiotic therapy before admission, and 324 (64.4%) had a positive culture; 377 strains of microorganisms were cultivated, 39 of which were cultured with two strains and 7 of which were cultured with three strains. Staphylococcus aureus accounted for 42.2% (159 strains), including 38 strains of MRSA. Pseudomonas aeruginosa accounted for 49 strains (13.0%), Enterobacter cloacae for 35 strains (9.2%), E. coli for 33 strains (8.8%), fungi for 7 strains (1.9%), Acinetobacter baumannii for 17 strains (4.5%), and other microorganisms accounted for 77 strains (20.4%). The positive rate of sinus secretion cultures was 47.9% (169/353), and 55.0% (93/169) were in accordance with the deep tissue culture. The positive rate of deep tissue cultures from post-traumatic osteomyelitis patients was 66.9% (273/408), and the proportion of S. aureus was 38.4% (117/305), while the positive rate of cultures from haematogenous osteomyelitis patients was 54.9% (50/91), and S. aureus accounted for 64.4% (38/59). Eighty-three patients had to undergo debridement more than twice before bone grafting; of these, 41 (49.4%) had positive cultures, and S. aureus accounted for 48.8% (20/41) of the microorganism distribution according to body site, as shown in Table 2.
Treatments and consequences
All the patients had an average bone defect length of 6.8 ± 1.1 cm; 320 cases were treated with the induced membrane technique and 183 were treated with I-stage free bone grafts. No other surgical methods were used for osteomyelitis therapy. Additionally, 256 patients were fixed with internal fixation, 117 with temporary or long-term external fixation (locking compression plate, Synthes, Switzerland) and 130 patients did not undergo fixation. One hundred eight patients were treated with flaps or skin grafts.
A total of 356 patients (284 treated with the induced membrane technique and 72 treated with I-stage free bone graft) were followed for more than 18 months. The total infection control rate was 93.8% (334/356), and 94.1% (335) acquired bone union. The average union time was 6.24 ± 0.76 months. Twenty-two patients underwent repeated surgery or amputation because of recurrent infection, and 83 patients required debridement more than twice before bone grafting. The complication rate was 18.0% (64/356). There were 8 cases of nonunion, 14 cases of iliac infection, 14 cases of restricted joint activity, 7 cases of pin-track infection when external fixation was used, 5 cases of loosening fixations, and 16 cases of other complications. The infection control rate for the induced membrane technique was higher than for I-stage free bone graft. The main complication of the induced membrane technique was iliac infection, while the main complication of I-stage free bone graft was restricted joint activity. The various complications encountered in the study are tabulated in Table 3.
There were no significant differences in the rate of infection control or the healing time of the bone defect according to fixation method. However, the difference in the complication rate was statistically significant (external fixation group > internal fixation group > no fixation group). The main complication in the internal fixation group was iliac infection, while pin-track infection was the main complication in the external fixation group. The prognosis and complications are elaborated in Table 4.
Discussion
The incidence of osteomyelitis has changed significantly in recent decades. The aetiology and morbidity of osteomyelitis is linked to many factors, including ethnicity, lifestyle and economic conditions. In the United States, the rate of infection following fracture fixation was approximately 5%, of which 1/3 of cases transformed into refractory osteomyelitis12. A fracture of the tibia, age in the 50 s13, a BMI > 30 kg/m2, alcohol abuse, compartment fasciotomy, and the use of temporary external fixation are independent risk factors for bone infection. Jiang and colleagues reviewed the characteristics of osteomyelitis in southeast China5. China has a large population and diverse landscapes, climates and customs (lifestyles), which may contribute to the incidence and severity of disease. The current study focused on patients living in southwest China, where the humid climate and relatively poor medical facilities may contribute to higher morbidity. Our medical centre is one of few hospitals specializing in bone infection in the entire region. The study began in 2011, and it focused on the treatment and characterization of osteomyelitis. With approximately 200 million people living in the five provinces of southwest China, our data could provide regional representation of the overall situation.
The current findings suggest that post-traumatic osteomyelitis is the predominant type (80.1%), but haematogenous osteomyelitis is still present in large proportions, particularly with a childhood and adolescent onset14. The average age of the haematogenous osteomyelitis patients was 35.4 years due to chronic osteomyelitis that was ignored for a long time, while normal immunized adults (38.9%) were seen at first onset. The most common site of osteomyelitis infection was the tibia, and 28.6% of cultures from the tibia were positive10, while the most common site of haematogenous osteomyelitis was the femur, and the positive rate of microbial cultures from the femur was 54.9%. These findings show that the characteristics of osteomyelitis vary significantly in different regions and according to work and/or race.
The recommended standard for osteomyelitis diagnosis consists of biopsy and deep tissue culture15. Damaged bones and soft tissues may expose numerous proteins, such as collagen and fibronectin, which serve as a substrate for bacterial attachment and growth1. A bacterial culture shows positive growth and may be affected by culture time, culture conditions, antibiotics use before culture, and biofilm-associated bacterial strains16. In the present study, the positive rate of the cultures was 64.4% after a normal duration (5 days), which differs slightly from previous reports5. The conventional culture time is approximately 1 week but in case of partial cultures may take approximately 2 weeks5. In contrast, the types and phenotypes of the microorganism may change as the disease progresses. A very large number of patients (92.8%) had undergone heavy antibiotic treatment before admission to the hospital, which may have led to changes in drug resistance. For patients with sinus infection, the level of sinus infection secretion culture was limited; the positive culture rate was lower (47.9%) than the overall positive rate (64.4%) in the current study. The percentage of microbial species shared between sinus infection secretion cultures and deep tissue culture was only 44.0%.
Staphylococcus aureus is abundant in the skin microflora and in mucus and is a frequent cause of biofilm-associated infections17,18. A study by Arias4 examined 193 patients with S. aureus (28.7%), MRSA (9.3%), and polymicrobial strains (31%), but the current study found higher rates of S. aureus (37.3%), including an 11.7% MRSA rate and a14.2% rate of polymicrobial infection. Among the patients with monomicrobial infection, the proportion of S. aureus was considerably higher (76.2%) in the haematogenous osteomyelitis patients than in the post-traumatic osteomyelitis patients (43.6%), and the rates of Escherichia coli and Enterobacter cloacae colonies were gradually increased.
For typical osteomyelitis, diagnosis following a patient history and physical examination is not difficult. However, for some atypical cases, preoperative auxiliary examinations are needed to obtain a preliminary diagnosis, and the value of serum inflammation markers is limited by many factors (cold, pain, surgery and other factors). Positive rates of WBC (16.9%), CRP (43.3%) and ESR (41.6%) were found for only a small number of patients (10.9%), indicating that positive inflammatory markers have poor specificity. The trending levels of acute inflammatory markers is more significant and indicates the infection status following initiation of treatment19. The levels of inflammatory markers gradually ascend 2 weeks post operation, indicating the failure of infection control.
To treat osteomyelitis, surgical intervention, conservative treatments or a combination of both can be used depending on the physician’s viewpoint4. The results of the present study show that the average duration of post-traumatic osteomyelitis was 37.1 ± 9.05 months and the average number of operations was 2.6 ± 0.27, while for haematogenous osteomyelitis, the average duration was 174.9 ± 16.14 months and the average number of operations was 1.1 ± 0.20. This indicates that physicians prioritize surgical approaches for post-traumatic osteomyelitis, while conservative treatment is more often adopted for haematogenous osteomyelitis.
The prognosis of osteomyelitis is related to its classification and treatment and the patient’s socioeconomic status20. Conventional techniques, such as vascularized fibula autograft and Iliazarov bone transport, yield poor long-term outcomes, often due to graft resorption and revascularization by creeping substitution21,22. For patients with bone defects greater than 4-5 cm, bone grafting treatment may lead to absorption of the grafts. May et al.23 reported that for tibial infections requiring bone graft for structural support, the repair time for the bone defect was 3–6 months, while tibial defects > 6 cm and intact fibula reconstruction require 12–18 months. The average bone defect length for our patients was 6.8 ± 1.1 cm, and the average bone healing time was 6.24 ± 0.76 months. The speed of the bone defect repair and the infection control rate were superior with the induced membrane technique compared with I-stage free bone graft, and the incidence of complications was not significant.
The use of the induced membrane technique to repair bone defects has been widely adapted in recent years because of its simple operation and high healing rate24,25,26. The complications associated with this technique include infection recurrence, delayed stress fracture and nonunion of bones27,28. Our results indicated that the most common complication was iliac infection, which may relate to the improper handling of the bone supply area. There were no significant differences in the rate of infection control and the bone defect healing time according to fixation method. However, there was a significant difference in the complication rate, suggesting that the use of internal fixation may not necessarily increase the incidence of infection. In contrast, external fixation may increase the incidence of complications, particularly pin-track infection; therefore, we propose the use of internal fixation, particularly for infection control.
This study had certain limitations; for example, diabetic foot infection cases were not treated at our department, and we did not have complete follow-up data, which impacted the observation of the overall distribution of osteomyelitis. We applied logistic regression analysis with the aim of identifying risk factors (gender, age, smoking, sinus and other factors) for osteomyelitis and infection control, but the results did not permit any clear conclusions. We did not find any connection between risk factors and a reduced recurrence of infection.
Conclusion
In southwest China, post-traumatic osteomyelitis is the most common type of osteomyelitis, but the incidence of haematogenous osteomyelitis is still higher than developed regions in the country. S. aureus is the main bacterial strain for bone infections. The speed of bone defect repair and the infection control rate of the induced membrane technique was superior to that of I-stage free bone graft. Internal fixation should be given priority as it does not increase the rate of infection recurrence but reduces the risk of complications such as pin-track infection.
References
Parsons, B. & Strauss, E. Surgical management of chronic osteomyelitis. Am J Surg. 188, 57–66 (2004).
Kremers, H. M. et al. Trends in the epidemiology of osteomyelitis: a population-based study, 1969 to 2009. J Bone Joint Surg Am. 97, 837–845 (2015).
Conterno, L. O. & Turchi, M. D. Antibiotics for treating chronic osteomyelitis in adults. Cochrane Database Syst Rev. 9, CD004439 (2013).
Arias Arias, C. et al. Differences in the Clinical Outcome of Osteomyelitis by Treating Specialty: Orthopedics or Infectology. PloS one. 10, e0144736 (2015).
Jiang, N. et al. Clinical Characteristics and Treatment of Extremity Chronic Osteomyelitis in Southern China: A Retrospective Analysis of 394 Consecutive Patients. Medicine. 94, e1874 (2015).
Lazzarini, L., Mader, J. T. & Calhoun, J. H. Osteomyelitis in long bones. J Bone Joint Surg Am. 86, 2305–2318 (2004).
Wirbel, R. & Hermans, K. Surgical treatment of chronic osteomyelitis in children admitted from developing countries. Afr J Paediatr Surg. 11, 297–303 (2014).
Ibingira, C. B. Chronic osteomyelitis in a Ugandan rural setting. East Afr Med J. 80, 242–246 (2003).
Hwang, H. J., Jeong, W. K., Lee, D. H. & Lee, S. H. Acute Primary Hematogenous Osteomyelitis in the Epiphysis of the Distal Tibia: A Case Report With Review of the Literature. J Foot Ankle Surg. 55, 600–604 (2016).
Cohen, E., Lifshitz, K., Fruchtman, Y., Eidelman, M. & Leibovitz, E. Current data on acute haematogenous osteomyelitis in children in Southern Israel: epidemiology, microbiology, clinics and therapeutic consequences. Int Orthop. 40, 1987–1994 (2016).
Wilkins, M., Hall-Stoodley, L., Allan, R. N. & Faust, S. N. New approaches to the treatment of biofilm-related infections. J Infect. 69, S47–52 (2014).
Darouiche, R. O. Treatment of infections associated with surgical implants. N Engl J Med. 350, 1422–1429 (2004).
Parkkinen, M., Madanat, R., Lindahl, J. & Mäkinen, T. J. Risk Factors for Deep Infection Following Plate Fixation of Proximal Tibial Fractures. J Bone Joint Surg Am. 98, 1292–1297 (2016).
Rossaak, M. & Pitto, R. P. Osteomyelitis in Polynesian children. Int Orthop. 29, 55–58 (2005).
Mouzopoulos, G. et al. Management of bone infections in adults: the surgeon’s and microbiologist’s perspectives. Injury. 42, S18–23 (2011).
Zimmerli, W. Clinical presentation and treatment of orthopaedic implant-associated infection. J Intern Med. 276, 111–119 (2014).
Ceroni, D. et al. From prevention of pin-tract infection to treatment of osteomyelitis during paediatric external fixation. J Child Orthop. 10, 605–612 (2016).
Vuong, C. & Otto, M. Staphylococcus epidermidis infections. Microbes infect. 4, 481–489 (2002).
Sanders, J. & Mauffrey, C. Long bone osteomyelitis in adults: fundamental concepts and current techniques. Orthopedics. 36, 368–375 (2013).
Pollak, A. N., McCarthy, M. L. & Burgess, A. R. Short-term wound complications after application of flaps for coverage of traumatic soft-tissue defects about the tibia. The Lower Extremity Assessment Project (LEAP) Study Group. J Bone Joint Surg Am. 82, 1681–1691 (2000).
Hertel, R. et al. Cancellous bone graft for skeletal reconstruction. Muscular versus periosteal bed–preliminary report. Injury. 25, A59–70 (1994).
Chadayammuri, V., Hake, M. & Mauffrey, C. Innovative strategies for the management of long bone infection: a review of the Masquelet technique. Patient Saf Surg. 9, 32 (2015).
May, J. W. Jr., Jupiter, J. B. & Byrd, H. S. Clinical classification of post-traumatic tibial osteomyelitis. J Bone Joint Surg Am. 71, 1422–1428 (1989).
Woon, C. Y., Chong, K. W. & Wong, M. K. Induced membranes–a staged technique of bone-grafting for segmental bone loss: a report of two cases and a literature review. J Bone Joint Surg Am. 92, 196–201 (2010).
Masquelet, A. C., Fitoussi, F., Begue, T. & Muller, G. P. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet. 45, 346–353 (2000).
Ren, L., Kang, Y., Browne, C., Bishop, J. & Yang, Y. Fabrication, vascularization and osteogenic properties of a novel synthetic biomimetic induced membrane for the treatment of large bone defects. Bone. 64, 173–182 (2014).
Taylor, B. C., French, B. G., Fowler, T. T., Russell, J. & Poka, A. Induced membrane technique for reconstruction to manage bone loss. J Am Acad Orthop Surg. 20, 142–150 (2012).
Stafford, P. R. & Norris, B. L. Reamer-irrigator-aspirator bone graft and bi Masquelet technique for segmental bone defect nonunions: a review of 25 cases. Injury. 41, S72–77 (2010).
Acknowledgements
We thank YL for the statistics help.
Author information
Authors and Affiliations
Contributions
X.W. contributed to data collection and writing the paper and performed surgeries. S.Y. contributed to data collection and data analysis, performed surgeries, and wrote the paper. J.F. contributed to data collection. K.H. contributed to data collection. S.D. and S.W. contributed to patient follow-up. Z.X. contributed to overall planning and data analysis and performed surgeries.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, X., Yu, S., Sun, D. et al. Current data on extremities chronic osteomyelitis in southwest China: epidemiology, microbiology and therapeutic consequences. Sci Rep 7, 16251 (2017). https://doi.org/10.1038/s41598-017-16337-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-16337-x
This article is cited by
-
Clinical effects of early debridement, internal fixation, and Masquelet technique for childhood chronic haematogenous osteomyelitis of long bones
Journal of Orthopaedic Surgery and Research (2023)
-
Epidemiology and microbiology of fracture-related infection: a multicenter study in Northeast China
Journal of Orthopaedic Surgery and Research (2021)
-
Investigating clinical characteristics and prognostic factors in patients with chronic osteomyelitis of humerus
Burns & Trauma (2019)
-
Epidemiology, microbiology and therapeutic consequences of chronic osteomyelitis in northern China: A retrospective analysis of 255 Patients
Scientific Reports (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.