Abstract
The individual response of patients to propofol results from the influence of genetic factors. However, the state of knowledge in this matter still remains insufficient. The aim of our study was to determine genetic predictors of variable pharmacokinetics and pharmacodynamics of propofol within selected 9 genes coding for propofol biotransformation enzymes, receptors and transporters. Our studies are the first extensive pharmaocgenetics research of propofol using high throughput sequencing technology. After the design and optimization of long range PCR-based next-generation sequencing experiment, we screened promoter and coding sequences of all genes analyzed among 87 Polish patients undergoing general anaesthesia with propofol. Initially we found that two variants, c.516 G > T in the CYP2B6 gene and c.2677 T > G in the ABCB1 gene, significantly correlate with propofol’s metabolic profile, however after Bonferroni correction the P-values were not statistically significant. Our results suggest, that variants within the CYP2B6 and ABCB1 genes correlate stronger with propofol’s metabolic profile compared to other 7 genes. CYP2B6 and ABCB1 variants can play a potentially important role in response to this anaesthetic and they are promising object for further studies.
Similar content being viewed by others
Introduction
Propofol (2,6-diisopropylphenol)‘s favorable pharmacological properties make it one of the safest and most widely used anaesthetics for intravenous general anaesthesia. However, a large interindividual variability of its pharmacodynamics (PD) and pharmacokinetics (PK) has been reported, which may lead to unexpected side effects1. It is known that the biotransformation pathway of propofol includes the action of numerous enzymes, whose polymorphic character may contribute to the individual response of patients to this anaesthetic2,3. Moreover, propofol transporting and receptor protein changes, which have a genetic background, could modify propofol action4,5. So far, the significance of only few variants of single genes in the propofol biotransformation rate and its dosage has been investigated6,7,8. Unfortunately, these data are often inconclusive. In addition, there are no studies on polygenic analysis in the context of variable PK and PD of propofol. Next-generation sequencing (NGS) technology has become currently an essential tool in extensive pharmacogenetic research, giving the possibility for in-depth analysis of targeted genes’ panel of interest.
The greatest contribution to propofol’s individual response is seen in the variants of the CYP2C9, CYP2B6, UGT1A9, SULT1A1, NQO1 genes, involved in the biotransformation pathway of the anaesthestic and also of transporting proteins: especially P-glycoprotein and serum albumin, encoded by the ABCB1 and ALB genes, as well as the receptor genes GABRA1 and ADRA1A 4,9,10. The crucial role can be probably played by three of the genes mentioned above: CYP2B6 (OMIM123930), CYP2C9 (OMIM601130) and UGT1A9 (OMIM606434), coding for metabolizing enzymes: cytochromes P-450 2B6 and 2C9, and UDP-glucuronosyltransferase 1A9, acting mainly in the liver.
The first step in propofol biotransformation is the hydroxylation process conducted mainly by CYP2B6 and CYP2C9 cytochromes, encoded by genes the CYP2B6 and CYP2C9, whose highly polymorphic character contributes to the variable expression level of these proteins and metabolism efficiency in the liver. For instance, two common allelic variants p.Q172H and p.K262R in the CYP2B6 gene are linked with decreased and increased expression, respectively11. For the CYP2C9 gene, two non-synonymous changes p.R144C (CYP2C9*2) and p.I359L (CYP2C9*3) associated with poor metabolizing phenotypes are a crucial subject of global pharmacogenetic studies12. Also the polymorphic gene UGT1A9 is described as an important pharmacogene due to the involvement in glucuronidation process of many important drugs besides propofol, for example, irinotecan and flavopiridol13. Genetic variants of the UGT1A9 gene lead to decreased (p.M33T, p.D256N), increased (c.399 C > T) or to absent (p.Y242X) enzyme activity4. The presence of these changes has been described with different frequencies in Polish and other populations14. The substitution p.M33T was proved to determine the pharmacokinetic profile of propofol and the reduced catalytic efficiency of the enzyme15.
Sulfotransferase 1A1 (SULT1A1) and NAD(P)H quinone dehydrogenase 1 (NQO1) play a role in the second phase of propofol metabolism. Among the many polymorphic changes in SULT1A1 (OMIM171150) and NQO1 (OMIM125860) genes, two alleles have been subjected to particularly intense investigation: NQO1*2 (p.P187S) and SULT1A1*2 (p.R213H), both leading to decreased expression16,17.
Long-term studies on the P-glycoprotein 1 encoded by the ABCB1 gene (OMIM171050), known as multidrug-resistance-protein 1, indicate the involvement of genetic polymorphism in the expression and activity of P-gp, which may affect the bioavailability, efficacy, and toxicity of drugs that are the substrates. Variants located in positions c.3435 and c.2677 of the ABCB1 gene have been analyzed in the context of opioid pharmacokinetics. Potentially, they could also affect the PK of propofol18.
Investigations demonstrate, that variants of the serum albumin gene ALB (OMIM103600), may considerably affect the transport of certain drugs by albumin. The change located in exon 7, c.725 G > C (p.R218P) or c.725 G > A (p.R218H) causes decreased binding of warfarin to the albumin, altering the pharmacokinetics of the drug19. Moreover, disturbed binding of drugs to this protein also cause variations c.1011 G > T (p.K313N) and c.1165 G > C (p.D365H)20.
Because the mechanism of propofol action is based on its interaction with an ionotropic receptor GABAA, which inhibits the transfer of nerve impulses between neurons in the central nervous system, sequence changes of the GABRA1 gene (OMIM 137160) may influence the effect of anaesthesia21. Stewart et al. proved the correlation between mutation p.M236W in the GABRA1 gene and the influence of etomidat anaesthetic on the receptor22. Moreover, studies have shown that polymorphism of the adrenergic receptor gene (ADRA1A, OMIM104221) influences the expression of these proteins, the post-translational processes and pharmacological response by the receptor interfering with the signal transduction, what may change the regulation of a number of relevant parameters in anaesthesia9.
The aim of our study was to identify the genetic determinants of diverse pharmacokinetics and pharmacodynamics of propofol, using deep sequencing of 9 candidate genes including: CYP2C9, CYP2B6, UGT1A9, SULT1A1, NQO1, ABCB1, ALB, GABRA1 and ADRA1A.
Results
Long range amplification and NGS
We optimized all twenty-seven LR-PCRs using three sets of polymerases and successfully amplified over 226 kb of the DNA for 87 patients anaesthetized with propofol (Fig. 1 ). Full-length gels are presented in Figure S1.
Results of 27 LR-PCR amplifications for one patient. Line 1 - ladder λ DNA HindIII; 2 - GABRA1 (17533 bp), 3 - ABCB1 (16809 bp); 4 - ABCB1 (17000 bp); 5 - NQO1 (11767 bp); 6 - ABCB1 (14483 bp); 7- ABCB1 (15827 bp); 8 - GABRA1 (10134 bp); 9 - ALB (11245 bp); 10 - CYP2C9 (17670 bp); 11 - CYP2C9 (10723 bp); 12 – ladder 100 bp; 13 - UGT1A9 (972 bp); 14 - ADRA1A (1183 bp); 15 - UGT1A9 (2303 bp); 16 - SULT1A1 (2760 bp); 17 - CYP2C9 (2761 bp); 18 - CYP2B6 (3312 bp); 19 - SULT1A1 (3219 bp); 20 - ABCB1 (3518 bp); 21 - CYP2B6 (3113 bp); 22 - ADRA1A (6818 bp); 23 - CYP2B6 (9280 bp); 24 - GABRA1 (9190 bp); 25 - ABCB1 (5967 bp); 26 - ALB (8571 bp); 27 - NQO1 (8998 bp); 28 - UGT1A9 (6700 bp); 29 - SULT1A1 (6497 bp); 30 – ladder 1 kbp;. Lines 1–11, 0.5% agarose gel; lines 12–14, 1.5% agarose gel; lines 15–30, 1.0% agarose gel. The gel images were obtained by trimming and colour adjusting of the full-length gels in the IrfanView 4.44 program.
All 87 DNA libraries with a mean fragment length between 300–500 bp were successfully sequenced on the Illumina MiSeq platform. On average 77.2% of the reads were aligned to the target regions. The mean depth of the reads was 166 (between 19–399) (Fig. 2). Four amplicons (numbered 7, 9, 10, 21) showed a considerable lower reads depth (<30-fold) among an average of 66% of the patient group analyzed and were excluded from further analyses. Moreover, amplicon number 11 showed insufficient coverage of approximately 25% of patients. Finally, only those variants of which the locus was read minimum 30 times in all patients, were included in the further analysis.
We detected 1513 different sequence variations in total. They were annotated and filtered using SNP-nexus and Variant Studio (Illumina). From the whole amount of the variants detected we selected only those described in the Human Genome Mutation Database (HGMD®Professional 2015.4) and nonsynonymous changes (Table 1). These changes were randomly verified with Sanger sequencing.
Pharmacokinetics and pharmacodynamics of propofol
The mean value of MRT was 82.5 min and the range was 8.0–504.1 min (SD = 107 min). Based on a percentile rank we determined three pharmacokinetic profiles of the propofol metabolism rate in our group of patients: rapid (MRT ≤ 30 min), intermediate (100 ≥ MRT > 30 min) and poor (MRT > 100 min) metabolizers, who constitute 27%, 48% and 22% of the group, respectively.
To specify the differences in the biotransformation pathway of propofol we analyzed the formation profile of two main metabolites: 4-hydroxypropofol (4-OHP) and propofol glucuronide (PG). Using a k-means clustering, we determined three significantly different (P = 0.00) groups of patients due to the formation of PG and 4-OHP (Fig. 3).
Profile 1 of PG formation was observed in 13 of patients, profile 2 and 3 in 23 and 44 individuals, respectively. Clearly, 4-OHP was produced to a minor extent, relative to PG, the second metabolite. Profile 1 of 4-OHP formation was reported in 14 of patients, profile 2 in 13 of the subjects and profile 3 was presented by 53 individuals (Fig. 3).
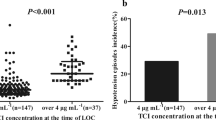
The pharmacodynamics of the anaesthetic were described by the awakening time of the patients after propofol anaesthesia. The mean awakening time was 12 min, the range was 0.5–45 min (SD = 7.8 min).
Correlation of genetic variants with PK and PD of propofol
The impact of genetic background on the pharmacokinetics of propofol was proved by correlation analysis of genetic changes found in genes coding for metabolizing and in transporting proteins of propofol with MRT and formation profiles of PG and 4-OHP. The statistical significance of distribution differences of selected variants in rapid, intermediate and poor metabolizers is shown in Table 2.
Two genetic changes initially have shown a correlation with the propofol metabolic profile, c.516 G > T (p.Q172H) in CYP2B6 gene and c.2677 T > G (p.S893A) in ABCB1 gene. Homozygotes c.516 T/T were more often (P = 0.046) presented in the group of rapid metabolizers, while heterozygotes c.2677 T/G were more frequently (P = 0.032) observed in patients presenting an intermediate and poor metabolism rate of the anaesthetic. However, using Bonferroni correction, the P-values were not statistically significant (P = 0.14, P = 0.1 for c.516 G > T and c.2677 T > G, respectively).
Moreover, we found that mutation p.S400N (c.1199 C > T) in the ABCB1 gene has a substantial impact on the profile of PG formation in our anaesthetized patient group. Homozygotes c.1199 C/C determined the profile 2 of the PG formation rate. However, none of variants analyzed affected the rate of 4-OHP formation.
The pharmacodynamics of propofol was correlated with genetic changes located in gene coding for the adrenergic receptor. The statistical significance of the influence of ADRA1A gene variants for the recovery time after anaesthesia is presented in Table 3. These analyses revealed no correlation between the pharmacodynamics of propofol and selected variants in the ADRA1A gene.
Discussion
Personalized anaesthesia with propofol still remains a challenge for pharmacogenomics. Global studies indicate in particular the contribution of CYP2B6, CYP2C9 and UGT1A9 gene polymorphism to the variability of propofol pharmacokinetics and pharmacodynamics6,7,8,23. Considering the complexity of the propofol biotransformation pathway, transport and interactions with receptors, in this study we presented deep sequence analysis of 9 gene panels, including those coding for receptors (GABRA1, ADRA1A), transporters (ALB, ABCB1) and liver enzymes (UGT1A9, CYP2B6, CYP2C9, NQO1, SULT1A1) in the context of anaesthetic metabolism rate, recovery time and searching for genetic determinants of individual propofol response.
Our investigations softly suggested that of the all genes analyzed, CYP2B6 and ABCB1 polymorphism may possibly influence propofol pharmacokinetics in this Polish patients group, what should be an object of further investigation. This finding confirms global reports and our previous results, proving the importance of variant p.Q172H (c.516 G > T; CM130453) in CYP2B6 gene for the propofol metabolism rate24. In our study homozygous c.516 T/T was identified more often in the rapid metabolizers of propofol, but no statistically significant correlation was found, in the contrast to Kansaku et al.7 and Mastrogianni et al.8, whose observations proved an association of a surprisingly higher propofol concentration in the serum with allele T7,8. On the other hand, Loryan et al.23 and Khan et al.25 did not find any correlation between polymorphism p.Q172H and the plasma concentration of propofol or its metabolites23,25. We also cannot share Murao et al.‘s (2015) conclusions that allele T decreased the total required dose of propofol6. The results of these different studies are contradictory, however, they do confirm the importance of a particular gene and a defined locus.
Moreover, we observed that heterozygotes c.2677 T/G of substitution p.S893A (c.2677 T > G; CM033585) located in exon 21 of the ABCB1 gene were more frequent (but not significantly) in the group of intermediate- and poor- propofol metabolizers. So far, there has been a lack of investigations that would analyse changes in the ABCB1 gene in the context of the reaction and the biotransformation rate of propofol. Nevertheless, the ABCB1 gene is considered to be one of the most important pharmacogenes and the impact of polymorphic variability is widely examined in the context of a number of therapies, especially of lymphocytic leukemia26. The change p.S893A resides in an important region between the membrane and the cytosolic N-terminal NBD in the part of TM10 of the ABCB1 protein27.
As evidence of the variable biotransformation process of propofol, in our experimental group we identified considerable interindividual differences in the formation of propofol metabolites, both PG and 4-OHP. Interestingly, as a causal genetic factor linked to interpatient variability in the formation rate of PG, we found the mutation p.S400N (c.1199 C > T) in the ABCB1 gene. Homozygous individuals c.1199 C/C revealed the profile 2 (“middle homogeneous”) of the glucuronidation rate. This mutation (CM045736) is known as disruptive of the ABCB1 protein transport activity and therefore it can probably influence propofol disposition and anaesthesia efficiency28.
The concept for molecular analysis in our investigations consisted of applying an approach combining LR-PCR with NGS, which enabled us to conduct an in-depth analysis of over 20 Mb of the sequence in a single run. A great advantage of using amplicon libraries and such methodology, compared to commercial sets of probes, is the easy and inexpensive modification of targeted genetic fragments through changes at the stage of designing long-range PCR. So far, only a few studies exist worldwide, which used a similar solution successfully29,30,31. On the other hand, we are of course aware of the limitations of our study, such as the number of patients, possible interactions between propofol with other drugs and the analysis of NGS data. It was crucial for us to obtain sufficient coverage for the genomic regions analyzed, which we unfortunately failed to achieve for a few amplicons, therefore 4 of them, covering exons 3–6 of the SULT1A1 gene, promoter and exons 1–8 of the GABRA1 gene and exons 6–15 of the ALB gene, were excluded from the final analysis. We suspect that they also can contain important changes for propofol action. To improve the experiment, perhaps the LR-PCR products of these 4 fragments should be added to the library in higher quantitative ratios in relation to other fragments.
Because we obtained a large amount of NGS data as detected variants, we decided to limit our analysis in the first stage only to the genetic changes recognized as most important from the pharmacogenetic point of view (mutations described in the HGMD database and as yet unknown amino acid changes). Nevertheless, our investigations are the first such a wide genetic analysis of the pharmacokinetics and pharmacodynamics of propofol in the world and may potentially allow genes to be identified that may play an important role in the interindividual variability of its anaesthetic action.
Materials and Methods
Patients and samples
Eighty-seven Polish patients (34 female and 53 men), Caucasians undergoing general anaesthesia with propofol (10 mg/mL propofol injectable emulsion, Diprivan; AstraZeneca, Macclesfield, UK) before minor laryngological surgery at the Regional Hospital in Poznan, Poland, were enrolled in this study. All participants provided written informed consent. The study was approved by the local Ethics Committee of the University of Medical Sciences in Poznan, Poland (resolution no. 653/09) and all experiments were performed in accordance with relevant guidelines and regulations of this Committee. Detailed information about the patients: age, weight, height, dose of propofol, infusion time, awakening time and adverse effects were collected (Table 4). All patients represented I or II class on The American Society of Anesthesiologists (ASA) scale. Perioperative monitoring includes heart rate, blood pressure and saturation. Anaesthesia was induced with propofol (2 mg/kg) followed by continuous infusion at a rate of 8 mg/kg/h, as described previously23. From each patient, 5 mL of peripheral blood for molecular analysis and 2 mL of blood samples were taken at 5 time points as follows: at the end of anaesthesia, 5, 10, 20 and 30 minutes after. These samples were collected for pharmacokinetic study.
LR-PCR amplification
The genomic DNA of each patient was isolated from the peripheral blood samples using the method with guanidine isothiocyanate (GTC). Detection of genetic variants in the coding sequence, including splice junctions and promoter regions of nine genes: UGT1A9, CYP2B6, CYP2C9, SULT1A1, NQO1, GABRA1, ADRA1A, ALB and ABCB1 was performed by NGS on MiSeq® System (Illumina, San Diego, USA). Amplicon libraries for NGS analysis were prepared based on twenty-seven LR-PCR fragments. Pairs of primer sets were designed in reference to the human genomic sequence (GRCh37/hg19) using Primer Blast and Primer 3 Plus software. In total, over 226 kb of the DNA of each patient were amplified in fragments ranging between 1 and 18 kbp (Table S1).
After optimization, LR-PCR reactions were carried out on an Applied Biosystems 2720 Thermal Cycler (Applied Biosystems, Foster City, CA) with the use of one of three polymerase sets: GoTaq® Long PCR Master Mix (Promega, Madison, USA), Long & High Fidelity PCR Enzyme Mix (BiotechRabbit, Hennigsdorf, Germany), Fire Pol®DNA Polymerase (Solis BioDyne, Tartu, Estonia) on the total volume of 30 μL, according to the manufacturer’s instructions (Table 5). Generally, most of the fragments were amplified using the GoTaq® Long PCR Master Mix (Promega) polymerase in accordance with the standard 2-step or 3-step PCR program.
NGS Library Preparation
After visualization on the agarose gel, the LR-PCR fragments obtained were purified with Exo-Sap (Affymetrix, Santa Clara, USA) before they were quantified using Qubit dsDNA BR Assay System (Invitrogen, Carlsbad, USA) on the Qubit® 2.0 Fluorometer (Thermo Fisher, Waltham, USA).
In the next step, 27 amplicons of each patient were pooled in equimolar ratios. According to the manufacturer’s protocol, 1 ng of the pooled DNA fragments was subjected to the Nextera XT procedure (Illumina) using transposome technology. Finally, using Nextera XT DNA Sample Preparation Kit (Illumina) and Nextera® XT Index Kit (96) (Illumina), we obtained eighty-seven both-side indexed DNA libraries ready for high-throughput sequencing. Quality control of the libraries was performed on TapeStation 2200 Instrument (Agilent, Santa Clara, USA) using an HS D1000 ScreenTape (Agilent). Normalization of all libraries was carried out with magnetic beads, according to the Nextera XT procedure.
Sequencing and bioinformatic analysis
Sequencing on the Illumina MiSeq System was performed as paired-end targeted resequencing using a MiSeq Reagent Kit v2 (300 cycle) (Illumina). Obtained reads were mapped to the reference DNA sequence (GRCh37/hg19) by a Burrows-Wheeler Aligner (BWA, version v0.7.10-r789) algorithm with default settings. Then, variants located in regions involved in the manifest were inspected using IGV (Integrative Genomics Viewer, version v2.3.59). The changes detected were then filtered using a set of criteria: GQX (genotyping quality) ≥ 30, read depth ≥ 30 and heterozygous read ratio ≥ 35%. Variants with potential pharmacokinetic significance included in Table 1 were randomly confirmed using Sanger sequencing. Amplicons were purified using shrimp alkaline phosphatase and exonuclease I, following manufacturer’s instructions. Direct sequencing was performed using BigDye Terminator v3.1 Cycle Sequencing Kit (Thermo Fisher Scientific) on the Applied Biosystems 3500 and Series Genetic Analyzers. Primer sequences and PCR conditions are available upon request.
HPLC measurements
The propofol concentration, as described previously24, as well as its two main metabolites: 4-hydroxypropofol and propofol glucuronide (Fluorochem Ltd., UK) in plasma retrieved from patients at five different time points was measured using the HPLC/UV (P580A, Dionex, Germany) system coupled to a fluorescence (RF2000, Dionex) detector. Plasma samples (150 μL) were mixed with 150 μL of 2 M trichloroacetic acid (TCA) and certifugated at 10,000 g for 10 min. An aliquot of the supernatant was injected onto an analytical C18 reversed-phase column (Hypersil GOLD, 250 mm × 4.6 mm × 5 µm, Thermo Fisher Scientific, USA) maintained at 30 °C. The mobile phase constituted 0.6% (v/v) orthophosphoric (V) acid and acetonitrile (50:50) at a flow rate of 1.0 ml/min. The elution profiles of propofol and 4-hydroxypropofol were monitored fluorometrically at an excitation wavelength of 270 nm and an emission wavelength of 310 nm and propofol glucuronide by HPLC/UV at wavelength of 260 nm. The plasma concentrations of propofol and its metabolites were determined by Chromeleon software version 6.80 (Dionex). For each analysis the percentage of relative standard deviation (RSD) was calculated and for the HPLC/UV and fluorescence method was below 2.5%. All samples were analyzed in duplicate.
Pharmacokinetic and pharmacodynamic parameters of propofol
The pharmacokinetics of propofol was characterized by the mean removal time (MRT), determined using a PKSolver tool based on HPLC measurements of the propofol concentration, dose of anaesthetic and infusion time32. Moreover, for both metabolites (propofol glucuronide and 4-hydroxypropofol) different profiles of the formation rate were defined by clustering analysis using k-means. Awakening time, characterized as the mean time of eye opening, first breath and orientation were used as pharmacodynamic parameter of propofol anaesthesia.
Statistical analysis
Analysis of the correlation between DNA sequence variants, MRT results, metabolites profiles and awakening time values was performed using Chi2 with Fisher’s test corrections. For multiple testing Bonferroni corrections were used. For all calculations STATISTICA 12.0 software (Stat Soft, 2014) was used. A P-value lower than 0.05 was considered statistically significant.
References
Pasin, L. et al. Propofol and survival: a meta-analysis of randomized clinical trials. Acta Anaesthesiol Scand. 59, 17–24 (2015).
Kübler, A. Postępy anestezjologii i intensywnej terapii w 2004 roku. Medycyna Praktyczna http://www.mp. pl/artykuly/27216 (2005).
Mikstacki, A. et al. The impact of genetic factors on response to anaesthetics. Adv Med Sci. 58, 9–14 (2013).
Restrepo, J. G., Garcia-Martín, E., Martínez, C. & Agúndez, J. A. Polymorphic drug metabolism in anaesthesia. Curr Drug Metab. 10, 236–46 (2009).
Landau, R., Bollag, L. A. & Kraft, J. C. Pharmacogenetics and anaesthesia: the value of genetic profiling. Anaesthesia 67, 165–79 (2012).
Mourão, A. L., de Abreu, F. G. & Fiegenbaum, M. Impact of the Cytochrome P450 2B6 (CYP2B6) Gene Polymorphism c.516G > T (rs3745274) on Propofol Dose Variability. Eur J Drug Metab Pharmacokinet. 41, 511–5 (2016).
Kansaku, F. et al. Individual differences in pharmacokinetics and pharmacodynamics of anesthetic agent propofol with regard to CYP2B6 and UGT1A9 genotype and patient age. Drug Metab Pharmacokinet. 26, 532–7 (2011).
Mastrogianni, O. et al. Association of the CYP2B6 c.516G > T polymorphism with high blood propofol concentrations in women from northern Greece. Drug Metab Pharmacokinet. 29, 215–8 (2014).
Landau, R. Pharmacogenetics: implications for obstetric anesthesia. Int J Obstet Anesth. 14, 316–23 (2005).
Schywalsky, M., Ihmsen, H., Knoll, R. & Schwilden, H. Binding of propofol to human serum albumin. Arzneimittelforschung 55, 303–6 (2005).
Zanger, U. M. et al. Polymorphic CYP2B6: molecular mechanisms and emerging clinical significance. Pharmacogenomics 8, 743–59 (2007).
Van Booven, D. et al. Cytochrome P450 2C9-CYP2C9. Pharmacogenet Genomics 20, 277–81 (2010).
Martignoni, E. et al. Two patients with COMT inhibitor-induced hepatic dysfunction and UGT1A9 genetic polymorphism. Neurology 65, 1820–1822 (2005).
Zakerska, O. et al. Genotype and allele frequencies of polymorphic UGT1A9 in the Polish population. Eur J Drug Met Pharm. 38, 217–21 (2013).
Korprasertthaworn, P. et al. Effects of amino acid substitutions at positions 33 and 37 on UDP-glucuronosyltransferase 1A9 (UGT1A9) activity and substrate selectivity. Biochem Pharmacol. 84, 1511–21 (2012).
Raftogianis, R. B., Wood, T. C., Otterness, D. M., Van Loon, J. A. & Weinshilboum, R. M. Phenol sulfotransferase pharmacogenetics in humans: association of common SULT1A1 alleles with TS PST phenotype. Biochem Biophys Res Commun. 239, 298–304 (1997).
Traver, R. D. et al. Characterization of a polymorphism in NAD(P)H: quinone oxidoreductase (DTdiaphorase). Br J Cancer. 75, 69–75 (1997).
Coulbault, L. et al. Environmental and genetic factors associated with morphine response in the postoperative period. Clin Pharmacol Ther. 79, 316–24 (2006).
Petersen, C. E., Ha, C. E., Harohalli, K., Park, D. S. & Bhagavan, N. V. Familial dysalbuminemic hyperthyroxinemia may result in altered warfarin pharmacokinetics. Chem. Biol. Interact. 124, 161–172 (2000).
Kragh-Hansen, U., Brennan, S. O., Galliano, M. & Sugita, O. Binding of warfarin, salicylate, and diazepam to genetic variants of human serum albumin with known mutations. Mol. Pharmacol. 37, 238–242 (1990).
Franks, N. P. Molecular targets underlying general anaesthesia. Br J Pharmacol. 147, 72–81 (2006).
Stewart, D., Desai, R., Cheng, Q., Liu, A. & Forman, S. A. Tryptophan mutations at azi-etomidate photo-incorporation sites on alpha1 or beta2 subunits enhance GABAA receptor gating and reduce etomidate modulation. Mol Pharmacol. 74, 1687–95 (2008).
Loryan, I. et al. Influence of sex on propofol metabolism, a pilot study: implications for propofol anesthesia. Eur J Clin Pharmacol 68, 397–406 (2012).
Mikstacki, A. et al. The effect of UGT1A9, CYP2B6 and CYP2C9 genes polymorphism on individual differences in propofol pharmacokinetics among Polish patients undergoing general anaesthesia. J Appl Genet. 8, https://doi.org/10.1007/s13353-016-0373-2 (2016).
Khan, M. S. et al. Pharmacogenetics, plasma concentrations, clinical signs and EEG during propofol treatment. Basic Clin Pharmacol Toxicol. 115, 565–70 (2014).
Svirnovski, A. I. et al. ABCB1 and ABCG2 proteins, their functional activity and gene expression in concert with drug sensitivity of leukemia cells. Hematology. 14, 204–12 (2009).
Wolf, S. J. et al. An update on ABCB1 pharmacogenetics: insights from a 3D model into the location and evolutionary conservation of residues corresponding to SNPs associated with drug pharmacokinetics. Pharmacogenomics J. 11, 315–25 (2011).
Woodahl, E. L., Crouthamel, M. H., Bui, T., Shen, D. D. & Ho, R. J. MDR1 (ABCB1) G1199A (Ser400Asn) polymorphism alters transepithelial permeability and sensitivity to anticancer agents. Cancer Chemother Pharmacol. 64, 183–8 (2009).
de Sousa Dias, M. et al. Detection of novel mutations that cause autosomal dominant retinitis pigmentosa in candidate genes by long-range PCR amplification and next-generation sequencing. Mol Vis. 19, 654–64 (2013).
Hernan, I. et al. Detection of genomic variations in BRCA1 and BRCA2 genes by long-range PCR and next-generation sequencing. J Mol Diagn. 14, 286–93 (2012).
Jia, H., Guo, Y., Zhao, W. & Wang, K. Long-range PCR in next-generation sequencing: comparison of six enzymes and evaluation on the MiSeq sequencer. Sci Rep. 4, 5737 (2014).
Zhang, Y., Huo, M., Zhou, J. & Xie, S. PKSolver: An add-in program for pharmacokinetic and pharmacodynamic data analysis in Microsoft Excel. Computer Methods and Programs in Biomedicine 99, 306–314 (2010).
Acknowledgements
This study was supported by grant from the Ministry of Science and Higher Education in Poland (grant number: N401 037 838), European Regional Development Fund-ERDF, European Fund for Innovative Economy and Foundation for Polish Science. I declare that I am a scholarship holder within the project “Scholarship support for PH.D. students specializing in majors strategic for Wielkopolska’s development”, Sub-measure 8.2.2 Human Capital Operational Programme, co-financed by European Union under the European Social Fund.
Author information
Authors and Affiliations
Contributions
Zakerska-Banaszak O.: performed research (molecular part), analyzed data and wrote the paper; Skrzypczak-Zielinska M.: designed the study and analyzed molecular data; Tamowicz B.: performed anaesthesia, collected and analyzed clinical data; Mikstacki A.: classified patients, collected and analyzed clinical data, Walczak M.: participated in NGS libraries preparation; Prendecki M.: performed research concerning pharmacokinetic part of the study; Dorszewska J.: established the pharmacokinetic research and analyzed data; Pollak A.: participated in NGS analysis; Lechowicz U.: performed the final quality control of NGS libraries; Oldak M.: supervised the NGS analysis; Huminska-Lisowska K.: participated in NGS data analysis; Molinska-Glura M.: performed statistical analyses of obtained results; Szalata M.: participated in the bioinformatic analysis; Slomski R.: supervised the study design, revised critical the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zakerska-Banaszak, O., Skrzypczak-Zielinska, M., Tamowicz, B. et al. Longrange PCR-based next-generation sequencing in pharmacokinetics and pharmacodynamics study of propofol among patients under general anaesthesia. Sci Rep 7, 15399 (2017). https://doi.org/10.1038/s41598-017-15657-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-15657-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.