Abstract
During wound healing, the migration of keratinocytes onto newly restored extracellular matrix aims to reestablish continuity of the epidermis. The application of amniotic membrane (AM) to chronic, deep traumatic, non-healing wounds has proven successful at stimulating re-epithelialization. When applied on epithelial cell cultures, AM activates extracellular signal-regulated kinases 1/2 (ERK1/2) and c-Jun N-terminal kinases 1/2 (JNK1/2), with the overexpression and phosphorylation of c-Jun along the wound edge. The effect of AM on the migration of cells was investigated by studying critical proteins involved in the focal adhesions turn-over: Focal Adhesion Kinase (FAK), Paxillin and Vinculin. In Mv1Lu and HaCaT cells, validated models for cell migration and wound healing, AM affected the expression and activation of Paxillin, but did not affect Vinculin expression, both factors which integrate into focal adhesions. Moreover, AM regulation also affected FAK activity through phosphorylation. Finally, we have determined that AM regulation of focal adhesions involves both JNK and MEK MAP kinase signaling pathways. This data provides a molecular background to understand how AM regulates critical cell and molecular aspects of cell migration, organizing and directing the movement of cells by the continuous formation, maturation, and turnover of focal adhesion structures at the migration leading edge.
Similar content being viewed by others
Introduction
During wound healing, skin integrity is restored by the actions of numerous cell types. Upon skin disruption, molecular events culminate in the formation of a fibrin clot which stops bleeding, while also serving as a provisional matrix for inflammatory cell migration. These are attracted by cytokines, including TGF-ß and other factors released by damaged tissue and platelets1. At the end of wound healing, the migration of keratinocytes onto the restored extracellular matrix, which accumulates around the newly formed granulation tissue, culminates this process and so reestablishes the continuity of the epidermis2. For the case of deep-traumatic and chronic non-healing wounds, the application of amniotic membrane (AM) has proven to successfully encourage re-epithelialization, resulting in a suitable therapeutic alternative to avoid autologous skin transplantation3,4. These properties derive from the ability of the AM to provide immuno-modulatory effects5 and to supply helpful growth factors including EGF or TGF-ß, among others6,7,8. In our lab we have shown how, when applied in vitro, the presence of AM promotes the activation of R-Smads8 and affects the expression profile of several TGF-ß dependent genes in epithelial cultured-cells9,10. Moreover, AM induces the activation of extracellular signal-regulated kinases 1/2 (ERK1/2) and c-Jun N-terminal kinases 1/2 (JNK1/2), along with the overexpression of c-Jun on the wound edge3,8,9. On top of that, the presence of AM is able to induce the phosphorylation of c-Jun specifically at the migrating front edge of Mv1Lu and HaCaT cells on wound healing assays8. In this context, the activation of JNK and MEK signaling, at the edge of healing wounds, is required for the phosphorylation of c-Jun8.
Cell migration is a coordinated process that requires the organized and directional movement of cell bodies. This is achieved by rapid changes in the dynamics of actin filaments together with the formation and disassembly of cell adhesion sites11,12. The continuous formation of focal complexes (FCs) that mature into focal adhesions (FAs), both containing ready-to-attach proteins13, is observed at the actively migrating leading edge of epithelia14. Together with protrusion extension and cell body retraction, the adhesion to substrates via the attachment of specific proteins is considered an essential step for cell migration15. FCs assembled at cell front undergo either rapid turnover or maturation in response to contractile forces and the feedback from extracellular components13,14. Many proteins are involved in the assembly, maturation and disassembly of FAs11,16. Among them, Paxillin and Vinculin can be considered fundamental components for FAs functioning, as once incorporated, the first is able to integrate multiple signaling cascades to coordinate the process16, while the latter has a broader role related to cytoskeletal dynamics16. Moreover, Paxillin acts as a key scaffold protein in the formation of FAs, whose assembly and disassembly is so critical during cellular migration17. On top of these proteins, the Focal Adhesion Kinase (FAK) acts as a master regulator11 of the process since it can modulate FAs assembly and disassembly through phosphorylation of different players, including Paxillin13.
In this paper, we applied the wound scratch assay method along with specific inhibitors for MEK-1 and JNK signaling pathways to study in situ the effect of AM on focal structures, either FCs or FAs, dynamism during the migration of two well established migration and wound healing cellular models, the Mink Lung Epithelial (Mv1Lu) cells and the spontaneously immortalized human keratinocyte (HaCaT) cells. By paying attention to focal structures and the proteins involved in this biological phenomenon, we describe the ability of AM treatment to stimulate the dynamics and turnover of focal structures contributing to enhanced migration of cells at the front edge of wounds.
Results
AM treatment induces the expression of Paxillin in Mv1Lu cells
Non-malignant mink lung epithelial cells, Mv1Lu, are recognized as a good epithelial model for the study of cell motility due to their ability to migrate and stop proliferation by means of cell-to-cell contact inhibition after confluence18,19,20,21. A closer view of the migration edge of artificial wound assays performed on Mv1Lu cells8,9 revealed the ability of AM to stimulate protrusion generation at the migrating edge of wounds (Fig. 1a). The presence of SP600125 or PD98059, inhibitors for JNK and MEK (JNKi and MEKi) respectively, produced an apparent decrease in the number of protrusions at the edge of migrating cells (Fig. 1a). These variations in the number of protrusions accompany variations in cell motility and are regarded as an indicator for increased cytoskeletal dynamics, in which Paxillin is usually involved14. When we studied Paxillin expression by performing WB on total protein extracts obtained from sub-confluent Mv1Lu cells, so that they would behave like a migratory edge8, we detected that AM treatment resulted in increased Paxillin levels (Fig. 1b and c). Paxillin activities are regulated through posttranslational modification, including phosphorylation and ubiquitination22. JNK and MEK MAP kinases had been shown to take part in the mediation of some of the effects triggered by AM stimulation8,9. The presence of either JNKi or MEKi promoted the accumulation of Paxillin after 24 hours in Mv1Lu sub-confluent cells. Interestingly, neither JNKi nor MEKi presence affected Paxillin induction by AM stimulus, which promoted its accumulation in a similar fashion independently of the presence of inhibitors (Fig. 1b and c). In this line, we also studied Vinculin total levels, as a concurrent factor incorporating to FAs. In that case, the expression levels of Vinculin showed not to be affected either by AM stimulus or by the presence of JNKi or MEKi (Fig. 1b and c).
Amniotic membrane (AM) promotes cell protrusion generation and Paxillin expression in migrating Mv1Lu cells. (a) Detailed pictures of the migrating edge of artificial wound assays treated with AM in combination with inhibitors. Scale Bar 50 µm. (b) Western Blot of total protein extracts from sub-confluent Mv1Lu cells cultured in the presence of AM and/or inhibitors and collected after 24 hours. The dashed grey lines indicate that two distant parts of the very same blot were put together. ß-actin was used as loading control. (‡) Unspecific bands. (c) Relative protein level plots generated from Western Blot quantification. C: serum starvation; JNKi: SP600125; MEKi: PD98059. Asterisks denote statistically significant differences between conditions according to ANOVA statistical analysis: (***) p < 0.001; (ns) not significant. All experiments were repeated at least three times. Representative pictures and results are shown.
These results would suggest the ability of AM treatment to promote cytoskeletal changes specifically involving the modulation of Paxillin protein levels in Mv1Lu cells. Moreover, our results would indicate that within the context of AM stimulation, this modulation would be influenced by MAP kinase activities.
Increased Paxillin levels correspond with enhanced focal complex dynamics in migrating Mv1Lu cells
When studying cells at the leading edge of wound assays by means of confocal microscopy, the cells migratory status could be determined by paying attention to the conformation of actin filaments: actively migrating cells show a rather diffuse structure; less mobile cells usually depict a profuse filament network23 (Fig. 2a). In our case, immuno-labelling of Paxillin on Mv1Lu cells also revealed distinct patterns for this protein. While unstimulated cells showed well defined focal structures corresponding to consolidated FAs, AM-stimulated cells depicted abundant but less conspicuous labelling at the migrating membrane, probably corresponding with the conformation of FCs (Fig. 2a). Both JNKi and MEKi are known to hamper AM induction of migration and wound closure in scratch assays8,9. When we studied the effects of these inhibitors on the cytoskeletal organization of unstimulated Mv1Lu cells no alteration was observed. However, in the case of AM-treatment, the cells lining the wound gap showed a consistent filament network in the presence of inhibitors, contrasting with the diffuse cytoskeleton labelling observed in their absence (Fig. 2a). For the case of Paxillin immuno-labelling, clear changes were observable upon AM stimulation in the presence of inhibitors (Fig. 2a and b). It is worth to note how AM stimulation alone increased the number of focal structures detected at the leading edge of migrating fronts. However, the presence of both JNKi and MEKi inhibitors when AM was added, restrained the increase of observable focal structures at that area (Fig. 2c). Interestingly, both AM stimulation or the presence of JNKi resulted in a reduction of the average size of the detected focal structures, while MEKi did not reduce significantly this parameter (Fig. 2c).
Amniotic membrane (AM) treatment alters Paxillin distribution and focal structures arrangement in migrating Mv1Lu cells. (a) Confocal microscopy images of Mv1Lu cells at the migrating edge of artificial wound assays. Scale Bar 50 µm. Juxtaposed field images were taken to show migration front from a wider perspective. (b) 2.5x magnified detail from merged pictures in (a). Scale Bar 10 µm. (c) Plots for average number and size of focal structures detected at the migrating leading edge. Asterisks denote statistically significant differences between conditions according to ANOVA statistical analysis: (*) p < 0.05, (**) p < 0.005 and (***) p < 0.001; (ns) not significant. Paxillin: green; Actin: red; Nuclei: blue; C: serum starvation; JNKi: SP600125; MEKi: PD98059; FS: focal structures. All the experiments were repeated at least three times. Representative pictures are shown.
Altogether, these observations would corroborate the ability of AM to promote the migration of Mv1Lu cells by encouraging the integration of Paxillin into focal structures, also involving changes to the conformation of actin filaments. Moreover, our results suggest that this phenomenon would be overwatched by MAP kinase activities.
AM treatment promotes Paxillin activation in migrating HaCaT cells
Spontaneously immortalized human keratinocyte cells, HaCaT, are highly valued as a human skin and epithelial wound healing model. HaCaT cells have a non-malignant origin and exhibit the ability to stop proliferation upon cell-to-cell contact inhibition. Finally, they also retain normal keratinization and migratory capacities upon confluence disruption8,9,24, also showing a considerable response in terms of wound closure to AM treatment8,9. A closer look at the migrating leading edge of sub-confluent HaCaT cells also revealed increased extension in protrusions of cells exposed to AM (Fig. 3a). When we studied Paxillin expression by WB, we detected that AM treatment resulted in an increase of Paxillin levels, which accumulated considerably after 24 hours (Fig. 3b and c). Interestingly, the presence of either JNKi or MEKi alone increased Paxillin levels (data not shown), nevertheless AM stimulation along with inhibitors resulted in anticipated augmented Paxillin levels (Fig. 3b and c). To further understand the underlying mechanism, we tried to assess Paxillin activation status by researching into its phosphorylated form. Phospho-Paxillin levels increased steadily upon AM treatment, showing its highest at the end of the 24-hour period. Interestingly, while the presence of JNKi initially promoted a substantial activation of Paxillin up to 3 hours, the presence of either JNKi or MEKi hampered the ability of AM to promote such activation at longer incubation times (Fig. 3b and c). Lastly, in a similar fashion to Mv1Lu cells, total expression levels of Vinculin remained steady, independently of either AM stimulation or JNKi and MEKi co-treatment.
Amniotic membrane (AM) promotes cell protrusion generation and Paxillin phosphorilation in migrating HaCaT cells. (a) Migrating HaCaT cells, protrusions are indicated by arrows. Scale Bar 50 µm. (b) Western Blot of total protein extracts from sub-confluent HaCaT cells cultured in the presence of AM and/or inhibitors and collected after 24 hours. ß-actin was used as loading control. (‡) Unspecific bands. (c) Relative protein level plots generated from Western Blot quantification data. C: serum starvation; JNKi: SP600125; MEKi: PD98059. Asterisks denote statistically significant differences between conditions according to ANOVA statistical analysis: (***) p < 0.001; (ns) not significant. All experiments were repeated at least three times. Representative pictures and results are shown.
These results suggest that upon AM stimulation, similar mechanisms would operate both in HaCaT and Mv1Lu cells for the promotion of the cytoskeletal changes required for cell migration and wound restoration.
AM induced Paxillin dynamics are associated with cytoskeletal filament conformation in migrating HaCaT cells
Confocal microscopy studies of artificial wounds on HaCaT cells showed a highly coherent monolayer an orderly cell disposition at the wound edge. Interestingly, when studying actin filaments, we found that cells treated with either JNKi or MEKi, regardless of AM presence or not, showed intense labelling corresponding with a well-developed filament network at the protruding cellular pole of cells bordering the wound gap. In contrast, control or AM-treated cells portrayed weaker labelling intensity at the migrating edge compared with areas distant from the wound gap (Fig. 4). When focusing on Paxillin immuno-labelling, HaCaT cells showed a diffuse pattern, in which focal structures were mainly appreciable at the edge of the migrating front (Fig. 4a and b). Interestingly, the treatment with AM promoted an increase in the number of detectable focal structures, which was abrogated by the presence of any of the inhibitors used (Fig. 4c). However, in contrast to what was observed for Mv1Lu cells, the stimulation of wounded HaCaT cells with AM did not result in a significant increase of the focal structures average size of at the leading edge of the migrating front (Fig. 4c). Moreover, while JNKi presence seemingly had no effect on the evolution of the average size of these focal structures, the presence of MEKi promoted a noticeable increase on it, which was further contributed by AM stimulus (Fig. 4c).
Amniotic membrane (AM) treatment increases the detection focal structures in migrating HaCaT cells. (a) Confocal microscopy images of HaCaT cells at the migrating edge of artificial wound assays. Scale Bar 50 µm. (b) 2.5x magnified detail from merged pictures in (a). (c) Plots for average number and size of focal structures detected at the migrating leading edge. Asterisks denote statistically significant differences between conditions according to ANOVA statistical analysis: (*) p < 0.05, (**) p < 0.005 and (***) p < 0.001; (ns) not significant. Paxillin: green; Actin: red; Nuclei: blue; C: serum starvation; JNKi: SP600125; MEKi: PD98059; FS: focal structures. All the experiments were repeated at least three times. Representative pictures are shown.
Altogether, these observations would sustain the ability of AM treatment to promote Paxillin dynamism and cytoskeletal remodeling for the promotion of HaCaT cells migration.
MA-induced Paxillin dynamics correlate with increased Focal Adhesion Kinase activation at the migrating edge of HaCaT cells
FAK is another relevant factor in modulating focal structures assembly, as well as in cytoskeletal remodeling and in the promotion of directional cell movement. When we studied FAK behavior on cells lining artificial wounds by means of immuno-labelling of phosphorylated tyrosine residues25, consolidated staining was detectable on the leading edge of unstimulated cells (Fig. 5a). Interestingly, AM stimulation resulted in increased immuno-labelling of migrating HaCaT cells. It is worth noting, as showed by pseudo-color analysis, that the labelling signal highly condensates at the membrane leading edge, especially in the cases of AM stimulated cells (Fig. 5a and b). Strikingly, immuno-labelling of cells treated with AM and either JNKi or MEKi depicted weaker, although some increase in fluorescence signal was recorded in cells co-exposed to AM and MEKi inhibitor (Fig. 5a and b). To further validate the previous observations, we performed WB on total protein extracts obtained from sub-confluent HaCaT cells and studied phospho-tyrosine detection as an optimal readout for FAK activation25. Coherently, AM stimulation resulted in a clear increase in phospho-tyrosine detection, which was sustained for the first 6 hours of treatment, retaining considerable induction after 24 hours (Fig. 5c). Consistently, despite AM inoculation, the presence of JNKi restrained phospho-tyrosine levels similar to those registered for control cells along the 24-hour time course (Fig. 5c). However, when MEKi and AM were used, although an increase in phospho-tyrosine detection was recorded, this time it was much weaker than in samples stimulated just with AM (Fig. 5c).
Amniotic membrane (AM) promotes FAK activation and detection at focal structures in migrating HaCaT cells. (a) HaCaT cells at the migrating edge of artificial wound assays show increased p-tyr-100 immune-staining when AM was present. P-tyr-100 immune-staining signal was converted into pseudo-color rainbow scale to display fluorescence-intensity variations. Fluorescent signal was converted using Rainbow feature from ZEN software, on a linear mode and covering the full range of the data. Co-staining with phalloidin and Hoechst-33258 was used to show the cell structure and nuclei, respectively. P-tyr-100: pseudo-color; p-tyr-100: green; Actin: red; Nuclei: blue. Scale Bar 25 µm. (b) Relative fluorescence level plot generated from average p-tyr-100 signal intensity data obtained at the migrating leading edge. (c) Western Blot of total protein extracts from sub-confluent HaCaT cells cultured in the presence of AM and/or different inhibitors collected for a 24 hours time course. ß-actin was used a loading control. Relative protein level plots were generated from Western Blot quantification data. C: serum starvation; JNKi: SP600125; MEKi: PD98059. Asterisks denote statistically significant differences between conditions according to ANOVA statistical analysis: (***) p < 0.001; (ns) not significant. All the experiments were repeated at least three times. Representative pictures and results are shown.
In conclusion, these data show evidence of the participation of FAK in the dynamism affecting FAs in migrating HaCaT cells after AM stimulation, through a process which involves the modulation of FAK activities by means of its phosphorylation status.
Discussion
In this paper, using two validated cell models for studying migration and wound healing, we have shown how the ability of AM to promote migration is sustained in the reorganization of cell focal structures, with the particular implication of Paxillin and FAK. AM treatment clearly induced the accumulation of Paxillin in both Mv1Lu and HaCaT cells. In both cases, the effect of AM on Paxillin protein levels was not blocked in the presence of either MEKi or JNKi. When we looked at Vinculin, another protein participating focal structures, AM did not exert relevant regulation on its protein levels. Notably, AM treatment induced the phosphorylation of Paxillin in HaCaT cells; in that case however, the presence of MEKi or JNKi prevented Paxillin phosphorylation. Moreover, AM caused a net remodeling of the FAs clearly noticeable by the alteration in size and number of focal structures detected at the protruding pole of cells at the migrating edge. This re-arrangement was disturbed by the presence of JNKi and MEKi, coherently with their well-known capacity to inhibit AM-induced cell migration8,9. Additionally, we have shown the ability of AM treatment to trigger the enrichment of active FAK to the migrating cells protruding pole, a phenomenon that was again affected by the presence of MEKi and JNKi.
In artificial wound assays, a close look at the wound migrating edge of epithelial cells shows evident morphological differences in those cells actively migrating compared with less motile cells. These morphological differences generally correspond with the development of cytoplasmic protrusions such as filopodia and ruffles14, which as we show in this paper, increase when cells are stimulated with AM. These differences could be swiftly related to divergent behavior involving focal as well as cytoskeletal structures. Directional cell movement requires the continuous formation of focal complexes (FCs), maturation into focal adhesions (FAs), and turnover at the rear of the leading-edge migrating cells13,14. FCs assembled at cell front undergo either rapid turnover or maturation in response to contractile forces and the feedback from extracellular components13,14. In this process, Paxillin acts as a key scaffold protein for the assembly, maturation into FAs and disassembly26. By providing a structural framework, Paxillin facilitates the concurrent binding of different protein components, particularly signaling molecules. This feeds an efficient crosstalk between different pathways, affecting many fundamental processes including gene transcription27. Coherently, alterations in Paxillin expression levels can affect migratory performance, as shown by different classic reports linking its expression with cancer metastatic potential28,29,30. Here, we show how AM treatment increased Paxillin expression in migrating Mv1Lu and HaCaT cells, in a process which was not affected when JNK or MEK-1 signaling was inhibited. Interestingly, although knowledge on the mechanisms affecting Paxillin expression is scarce, it has been noted that TGF-ß1 signaling promotes its accumulation through a transcription-independent mechanism31. As TGF-ß1 is considered among the factors released by AM, here levels of Paxillin may be regulated by transcription as well as by protein stabilization in response to this kind of signaling. Vinculin, another important component incorporating to FAs, has the main function of anchoring actin filaments and integrins16. Interestingly, and in contrast to Paxillin, Vinculin was not transcriptionally regulated by the presence of AM. Although both proteins co-localize at FAs, they openly diverge in their ability to transduce signals, as the stimuli conducted through Vinculin fundamentally influence cytoskeletal mechanical properties, such as contractibility, adhesion strength and stiffness16,32. The ability of the AM treatment to induce this differential expression, further suggests its ability to accurately activate chosen components of the migration machinery.
Activation of JNK is usually correlated with increased cell migration in a mechanism involving the phosphorylation of known substrates. This process results in the transcriptomic modulation of key genes required for migration such as c-JUN 33. Indeed, on top of the ability of AM to induce JNK signaling3, we have described in the past the increased expression of c-Jun9 and the occurrence of its phosphorylation specifically at the leading edge of migrating Mv1Lu and HaCaT cells when they were stimulated with AM8. However, a more dynamic role for JNK in regulating cell migration involves the direct phosphorylation of cytosolic substrates. Paxillin exhibits several phosphorylation sites whose modifications modulate its behavior, already been identified as a substrate for JNK34. In this context, Paxillin interaction with activated JNK seems critical, as the resulting phosphorylation at Ser-178 residue appears to be essential to allow migration22,35. As we have shown here, AM treatment resulted in an obvious rise in Paxillin Ser-178 residue phosphorylated levels in HaCaT cells. More importantly, the presence of JNKi not only altered AM-induced Paxillin phosphorylation but also abrogated its incorporation into nascent FCs despite increasing Paxillin levels. Indeed, this was evidenced by the lower number of focal structures detected at the wound’s leading edge cells. It is worth noting that it has been shown that different extracellular signals regulate spreading and cell migration through this JNK/Paxillin system13. The fact that such observations were not as dramatic when using MEKi, which merely contributes to JNK activation8,9, would further point to activated JNK as a key element channeling the effects of AM on FAs dynamics and HaCaT cell migration.
It has been described that phosphorylation of Paxillin by JNK further promotes its association with FAK22,35. FAK operates as the cell master controller for FAs remodeling at the migration leading edge, consequently driving directional cell movement11,13. Increased FAK localization at these areas has been connected to FAs increased turnover at the protrusion front13. We have observed a clear change in the number and size of focal structures in cells stimulated with AM when compared to unstimulated control cells, both by studying Paxillin and phospho-tyrosine FAK. Paxillin is phosphorylated at residues Tyr-31 and Tyr-118 by FAK27,35. Phosphorylation at these sites generates two functional binding elements for members of the Crk family of SH2-SH3 adaptor proteins, which further coordinate integrin-mediated cell motility and consolidation of FCs into FAs27. This process is crucial, as mature FAs enable the cell contractibility necessary to pull the cell forward13. Additionally, FAK integrates growth-factor and integrin signals to promote cell migration11,36. Coherently, FAK-null fibroblasts show larger, more stable focal adhesions and lose random migration capacity37. Here we have shown the ability of AM to promote a strong stimulation of FAK, as evidenced by immunostaining at the leading edge. This would agree with the idea of the emergence of numerous dynamic FCs in cells stimulated with AM, compared to those left alone which show a rather static behavior as could be related to the reduced number and size of focal structures. Indeed, in every case, the structure of actin microfilaments was also suggestive for the migratory status of the conditions assayed14,38. Although the best characterized activation mechanism for FAK involves its auto-phosphorylation at Tyr-397 induced by interaction with Extra Cellular Matrix (ECM) components and members of the integrin family11,16, here we evidenced the ability of both JNKi and MEKi to prevent further FAK activation by AM. Whether this phenomenon is the consequence of higher ECM feedback linked to increased migration, or the result of additional endogenous or exogenous receptor activation by AM, perhaps also involving JNK, is something that will be the object of further research.
Migrating cells require for the spatiotemporal integration of many signals regulating essential activities responsible for cell movement. Continuous assembly/disassembly of cell adhesion sites, together with cytoskeleton dynamics are coordinated by those signals12. By regulating critical and intimate mechanisms inherent to these processes, AM is able to consistently stimulate cell migration. Precisely, using two distant but relevant epithelial models for the study of cell migration and wound healing such as Mv1Lu and HaCaT cells, here we showed evidence of the involving of MAP kinases activities for the promotion of FAs remodeling, a fundamental phenomenon for cell migration. Understanding this regulation and its potential implications for different cell types involved may help explain some of the wonderful properties shown by AM for the epithelialization of clinical non-healing wounds, providing a real opportunity for the development of improved therapies and procedures.
Materials and Methods
This study was approved by the local ethics committee (University Clinical Hospital Virgen de la Arrixaca, Murcia, Spain) and the Spanish Agency for Drugs (AEMPS). Appropriate written informed consent was obtained from AM donors. Additionally, all methods were performed in accordance with the relevant guidelines and regulations.
Cells and AM processing
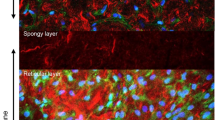
Mink Lung Epithelial cells (Mv1Lu)18,20,21, a kind gift from Dr. Inman, were grown in Eagle’s Minimum Essential Medium (EMEM) and spontaneously immortalized human keratinocyte (HaCaT) cells, obtained from ATCC, were cultured in Dulbecco’s Modified Eagle Medium (DMEM) high-glucose (Biowest, Nuaillé, France). Both cell lines media were supplemented with 10% Fetal Bovine Serum (FBS) (Thermo Fisher Scientific, Waltham, MA USA), 1000 units/ml Penicillin/1000 µg/ml Streptomycin (Sigma-Aldrich, St Louis, MO, USA), and 1% L-glutamine (Biowest, Nuaillé, France) at 37 °C in a 7.5% CO2 incubator. Amniotic membrane was prepared as described elsewhere9. Briefly, term placenta from healthy donor mothers was obtained from uncomplicated caesarean section. The fetal membranes were washed in Physiological Saline Solution (PSS) (B.Braun, Barcelona, Spain) supplemented with 50 µg/ml Amphotericin (Bristol-MyersSquibb, Madrid, Spain), 48 µg/ml Clotrymazol (Almirall-Prodesfarma, Barcelona, Spain), 50 µg/ml Tobramycin (Laboratorios Normon, Madrid, Spain) and 50 µg/ml Vancomycin (Laboratorios Hospira, Madrid, Spain) and rapidly transferred to the laboratory in sterile conditions. Under a laminar flow cabinet, the amnion was mechanically peeled from the chorion, washed three to four times with 200 ml of PBS (Biowest, Nuaillé, France) and flattened onto sterile nitrocellulose paper (Pierce, Thermo Fisher Scientific, Waltham, MA USA) with the amniotic epithelium surface up, and the spongy layer facing and sticking to the nitrocellulose paper. Then, paper with adhered membrane was cut into 1 cm × 1 cm fragments. Freshly cut AM fragments were separated from paper pieces and placed in a sterile vial containing a freezing solution made of 10% Dimethyl Sulfoxide (DMSO) (Sigma-Aldrich, St Louis, MO, USA), 4% human albumin (Grifols, Bercelona, Spain) in DMEM (Biowest, Nuaillé, France) medium and then frozen at −80 °C and later preserved in liquid nitrogen until further use. The day of wound application, AM pieces were thawed at 37 °C, then pieces were washed three times with DMEM and placed at 37 °C in a 7.5% CO2 incubator for two hours for the re-vitalisation of the amniotic membrane cells. The pieces now were used for the desired experiment. When the JNK inhibitor SP600125 (15 µM; JNKi) or MEK inhibitor PD98059 (50 µM; MEKi) (all Sigma-Aldrich, St Louis, MO, USA) were used, these were added at the beginning (T0) alone or with pieces of AM. In all cases, similar concentrations of DMSO (inhibitor’s carrier) or PBS were used for control samples.
Western blot
Mv1Lu or HaCaT cells were seeded to reach 50% confluence on day two in 6-cm diameter plates using a medium containing 10% FBS. At this point, culture medium was substituted for a FBS-free medium and cells were cultured on it for an additional 24-hour period. The treatment with AM was done as previously described9. Briefly, 5 pieces of 1cm2 AM per plate were placed floating on the medium of the samples indicated with AM in the figures. At T0, incubation with AM, inhibitors alone, or combination of both began. After 24 hours incubation, AM was removed and cells were lysed using lysis buffer: 20 mM TRIS pH 7.5, 150 mM NaCl, 1 mM EDTA, 1.2 mM MgCl2, 0.5% Nonidet P-40, 1 mM DTT, 25 mM NaF and 25 mM ß-glycerolphosphate (all from Sigma-Aldrich, St Louis, MO, USA) supplemented with phosphatase inhibitors (I and II) and protease inhibitors (all from Sigma-Aldrich, St Louis, MO, USA). Protein extracts were analyzed by SDS-PAGE followed by western blot using the appropriate antibodies: anti-Paxillin39 (Abcam, Cambridge, UK), anti-phospho-Paxillin40 (Life Technologies Corporation, Carlsbad, CA, USA), anti-phospho-tyr-10025 (New England Biolabs, Frankfurt, Germany), anti-vinculin41 and anti-β-actin42 (Sigma-Aldrich, St Louis, MO, USA). Secondary antibodies were anti-rabbit IgG Horseradish peroxidase linked F(ab’)2 I fragment (from donkey) (GE Healthcare, GE, Little Chalfont, United Kingdom) and Horseradish peroxidase linked Rat anti-mouse IgG1 (BD Pharmingen, Beckton Dickinson, Franklin Lakes, NJ, USA). WBs were developed using Horseradish peroxidase substrate (ECL) (GE Healthcare, GE, Little Chalfont, United Kingdom) and images were taken with a Chemidoc XRS® (Bio-Rad, Hercules, Ca, USA).
Immunocytochemistry and analysis in wound healing assay
Mv1Lu or HaCaT cells were grown to confluence over round glass-coverslips using medium containing 10% FBS (Thermo Fisher Scientific, Waltham, MA USA). Prior to the assays (24 hours), cells were washed and medium was exchanged for FBS-free medium. Then, the epithelium was wounded using a razor blade, which was immediately dragged to create a space large enough to allow migration. At T0, fresh FBS-free medium was placed and incubation began in a 6-well plate containing five coverslips and four 1 cm2 piece of AM floating on the medium. When used, inhibitors were added at T0. After 24 hours of incubation, AM was removed and the coverslips were fixed in 4% formaldehyde (Applichem GmbH, Darmstadt, Germany) in PBS (Biowest, Nuaillé, France). Subsequently, cells were permeabilized with 0.3% Triton X-100 (Sigma-Aldrich, St Louis, MO, USA) in PBS (Biowest, Nuaillé, France). Immunostaining was performed by blocking buffer [0.3% Bovine Serum Albumin (BSA) (Santa Cruz Biotechnology, Heidelberg, Germany), 10% FBS (Thermo Fisher Scientific, Waltham, MA USA), 0.1% Triton X-100 (Sigma-Aldrich, St Louis, MO, USA) in PBS (Biowest, Nuaillé, France)] supplemented with 5% skimmed milk (Beckton Dickinson, Franklin Lakes, NJ, USA), at room temperature for 1 hour of incubation with either: anti-Paxillin (Abcam, Cambridge, UK) or anti-phospho-tyr-100 (Cell Signaling Technology, Danvers, MA, USA) performed in blocking buffer. After staining with the primary antibody, samples were stained with the appropriate fluorescent-labelled secondary antibodies together with Alexa Fluor 594-conjugated phalloidin (Molecular Probes, Thermo Fisher Scientific, Waltham, MA USA), where indicated, and Hoechst 33258 (Fluka, Biochemika, Sigma-Aldrich, St Louis, MO, USA) for half an hour at room temperature to reveal actin and nuclei respectively. Control samples without primary antibody were done, showing in all cases a negative signal, to test the specificity of secondary antibody (data not shown). Finally, samples were examined and images were taken with a confocal microscope (LSM 510 META from ZEISS, Jena, Germany) using Zeiss Efficient Navigation (ZEN) interface software. For the acquisition of images, a Plan-neofluar 40x/1.30 oil DIC lens was used. Fields were scanned with the appropriate laser and fluorescent signal was collected with the scanning laser confocal module Meta, Zeiss. When a wider view of the migration front was required (indicated in the figure), two juxtaposed fields were acquired utilizing the “Tile scan” feature of ZEN. For clarity of some images, fluorescent signal was converted on a linear mode and covering the full data range using Rainbow feature from ZEN software.
Quantitative image processing and statistical analysis
Delimitation of regions of interest and quantification of structures was performed using built in tools included in Image J 1.8.0 image processing software. In all cases, we used Prism’s Graph Pad software for data calculation and representation. Statistical analysis shown in figures represent data mean ± SEM, analyzed using one way ANOVA statistical analysis applying Newman-Keuls multiple comparison test. At the figure legends, asterisks denote statistically significant differences between treatments (*p < 0.05, **p < 0.005 and ***p < 0.001, ****p < 0.0001).
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
References
Barrientos, S., Stojadinovic, O., Golinko, M. S., Brem, H. & Tomic-Canic, M. Growth factors and cytokines in wound healing. Wound repair and regeneration: official publication of the Wound Healing Society [and] the European Tissue Repair Society 16, 585–601, https://doi.org/10.1111/j.1524-475X.2008.00410.x (2008).
Singer, A. J. & Clark, R. A. Cutaneous wound healing. N Engl J Med 341, 738–746, https://doi.org/10.1056/NEJM199909023411006 (1999).
Insausti, C. L. et al. Amniotic membrane induces epithelialization in massive posttraumatic wounds. Wound Repair Regen 18, 368–377, https://doi.org/10.1111/j.1524-475X.2010.00604.x (2010).
Castellanos, G., Bernabe-Garcia, A., Moraleda, J. M. & Nicolas, F. J. Amniotic membrane application for the healing of chronic wounds and ulcers. Placenta, https://doi.org/10.1016/j.placenta.2017.04.005 (2017).
Manuelpillai, U., Moodley, Y., Borlongan, C. V. & Parolini, O. Amniotic membrane and amniotic cells: potential therapeutic tools to combat tissue inflammation and fibrosis? Placenta 32(Suppl 4), S320–325, https://doi.org/10.1016/j.placenta.2011.04.010 (2011).
Insausti, C. L. et al. The amniotic membrane as a source of stem cells. Histol Histopathol 25, 91–98 (2010).
Koizumi, N. J. et al. Growth factor mRNA and protein in preserved human amniotic membrane. Curr Eye Res 20, 173–177 (2000).
Ruiz-Canada, C. et al. Amniotic membrane stimulates cell migration by modulating Transforming Growth Factor-beta signaling. J Tissue Eng Regen Med, https://doi.org/10.1002/term.2501 (2017).
Alcaraz, A. et al. Amniotic Membrane Modifies the Genetic Program Induced by TGFss, Stimulating Keratinocyte Proliferation and Migration in Chronic Wounds. PLoS One 10, e0135324, https://doi.org/10.1371/journal.pone.0135324 (2015).
Insausti, C. L., Moraleda, J. M., Castellanos, G. & Nicolas, F. J. In Placenta The Tree of Life Gene and Cell Therapy (eds Ornella Parolini & Antonietta R. Silini) Ch. 4, 49–68 (CRC Press, 2016).
Mitra, S. K., Hanson, D. A. & Schlaepfer, D. D. Focal adhesion kinase: in command and control of cell motility. Nat Rev Mol Cell Biol 6, 56–68, https://doi.org/10.1038/nrm1549 (2005).
Brakebusch, C. & Fassler, R. The integrin-actin connection, an eternal love affair. EMBO J 22, 2324–2333, https://doi.org/10.1093/emboj/cdg245 (2003).
Hu, Y. L. et al. FAK and paxillin dynamics at focal adhesions in the protrusions of migrating cells. Scientific reports 4, 6024, https://doi.org/10.1038/srep06024 (2014).
Mayor, R. & Etienne-Manneville, S. The front and rear of collective cell migration. Nat Rev Mol Cell Biol 17, 97–109, https://doi.org/10.1038/nrm.2015.14 (2016).
Paluch, E. K., Aspalter, I. M. & Sixt, M. Focal Adhesion-Independent Cell Migration. Annu Rev Cell Dev Biol 32, 469–490, https://doi.org/10.1146/annurev-cellbio-111315-125341 (2016).
Lopez-Colome, A. M., Lee-Rivera, I., Benavides-Hidalgo, R. & Lopez, E. Paxillin: a crossroad in pathological cell migration. J Hematol Oncol 10, 50, https://doi.org/10.1186/s13045-017-0418-y (2017).
Turner, C. E. Paxillin and focal adhesion signalling. Nat Cell Biol 2, E231–236, https://doi.org/10.1038/35046659 (2000).
Demetriou, M., Nabi, I. R., Coppolino, M., Dedhar, S. & Dennis, J. W. Reduced Contact-Inhibition and Substratum Adhesion in Epithelial Cells Expressing GlcNAc-Transferase V. The Journal of Cell Biology 130, 383–392 (1995).
Wu, F. et al. Cell cycle arrest in G0/G1 phase by contact inhibition and TGF-beta 1 in mink Mv1Lu lung epithelial cells. Am J Physiol 270, L879–888 (1996).
Rahimi, N., Hung, W., Tremblay, E., Saulnier, R. & Elliott, B. c-Src Kinase Activity Is Required for Hepatocyte Growth Factor-induced Motility and Anchorage-independent Growth of Mammary Carcinoma Cells. Journal of Biological Chemistry 273, 33714–33721 (1998).
Zou, Y. Serine/Threonine Kinase Mirk/Dyrk1B Is an Inhibitor of Epithelial Cell Migration and Is Negatively Regulated by the Met Adaptor Ran-binding Protein M. Journal of Biological Chemistry 278, 49573–49581, https://doi.org/10.1074/jbc.M307556200 (2003).
Huang, C., Rajfur, Z., Borchers, C., Schaller, M. D. & Jacobson, K. JNK phosphorylates paxillin and regulates cell migration. Nature 424, 219–223, https://doi.org/10.1038/nature01745 (2003).
Murayama, A. et al. Epigenetic control of rDNA loci in response to intracellular energy status. Cell 133, 627–639, https://doi.org/10.1016/j.cell.2008.03.030 (2008).
Boukamp, P. et al. Normal keratinization in a spontaneously immortalized aneuploid human keratinocyte cell line. J Cell Biol 106, 761–771 (1988).
Graness, A., Cicha, I. & Goppelt-Struebe, M. Contribution of Src-FAK signaling to the induction of connective tissue growth factor in renal fibroblasts. Kidney Int 69, 1341–1349, https://doi.org/10.1038/sj.ki.5000296 (2006).
Ishibe, S., Joly, D., Zhu, X. & Cantley, L. G. Phosphorylation-dependent paxillin-ERK association mediates hepatocyte growth factor-stimulated epithelial morphogenesis. Molecular cell 12, 1275–1285, doi:S1097276503004064 (2003).
Petit, V. et al. Phosphorylation of tyrosine residues 31 and 118 on paxillin regulates cell migration through an association with CRK in NBT-II cells. J Cell Biol 148, 957–970 (2000).
Salgia, R. et al. Expression of the focal adhesion protein paxillin in lung cancer and its relation to cell motility. Oncogene 18, 67–77, https://doi.org/10.1038/sj.onc.1202273 (1999).
Vadlamudi, R., Adam, L., Tseng, B., Costa, L. & Kumar, R. Transcriptional up-regulation of paxillin expression by heregulin in human breast cancer cells. Cancer Res 59, 2843–2846 (1999).
Velasco-Velazquez, M. A., Salinas-Jazmin, N., Mendoza-Patino, N. & Mandoki, J. J. Reduced paxillin expression contributes to the antimetastatic effect of 4-hydroxycoumarin on B16-F10 melanoma cells. Cancer Cell Int 8, 8, https://doi.org/10.1186/1475-2867-8-8 (2008).
Han, X. et al. TGF-beta1 up-regulates paxillin protein expression in malignant astrocytoma cells: requirement for a fibronectin substrate. Oncogene 20, 7976–7986, https://doi.org/10.1038/sj.onc.1204996 (2001).
Goldmann, W. H., Auernheimer, V., Thievessen, I. & Fabry, B. Vinculin, cell mechanics and tumour cell invasion. Cell Biol Int 37, 397–405, https://doi.org/10.1002/cbin.10064 (2013).
Huang, C., Jacobson, K. & Schaller, M. D. A Role for JNK-Paxillin Signaling in Cell Migration. Cell Cycle 3, 4–6 (2004).
Schaller, M. D. Paxillin: a focal adhesion-associated adaptor protein. Oncogene 20, 6459–6472, https://doi.org/10.1038/sj.onc.1204786 (2001).
Huang, Z., Yan, D. P. & Ge, B. X. JNK regulates cell migration through promotion of tyrosine phosphorylation of paxillin. Cell Signal 20, 2002–2012, https://doi.org/10.1016/j.cellsig.2008.07.014 (2008).
Sieg, D. J. et al. FAK integrates growth-factor and integrin signals to promote cell migration. Nat Cell Biol 2, 249–256, https://doi.org/10.1038/35010517 (2000).
Ilic, D. et al. Reduced cell motility and enhanced focal adhesion contact formation in cells from FAK-deficient mice. Nature 377, 539–544, https://doi.org/10.1038/377539a0 (1995).
Kimura, K., Teranishi, S., Yamauchi, J. & Nishida, T. Role of JNK-dependent serine phosphorylation of paxillin in migration of corneal epithelial cells during wound closure. Invest Ophthalmol Vis Sci 49, 125–132, https://doi.org/10.1167/iovs.07-0725 (2008).
Vandenberghe, M. et al. ORAI1 calcium channel orchestrates skin homeostasis. Proc Natl Acad Sci USA 110, E4839–4848, https://doi.org/10.1073/pnas.1310394110 (2013).
Tezuka, Y. et al. Regulation of neurite growth by inorganic pyrophosphatase 1 via JNK dephosphorylation. PLoS One 8, e61649, https://doi.org/10.1371/journal.pone.0061649 (2013).
Rubashkin, M. G. et al. Force engages vinculin and promotes tumor progression by enhancing PI3K activation of phosphatidylinositol (3,4,5)-triphosphate. Cancer Res 74, 4597–4611, https://doi.org/10.1158/0008-5472.CAN-13-3698 (2014).
Radhakrishnan, S. K. et al. Constitutive expression of E2F-1 leads to p21-dependent cell cycle arrest in S phase of the cell cycle. Oncogene 23, 4173–4176, https://doi.org/10.1038/sj.onc.1207571 (2004).
Acknowledgements
We thank Mónica Rodriguez Valiente, Ester García and Ángela Filiu who prepared AM. ABG was supported with funds from the University Clinical Hospital Virgen de la Arrixaca. We are grateful to Catalina Ruiz who envisioned the participation of Paxillin regulation in the process of cell migration induced by AM. We are indebted to the University Clinical Virgen de la Arrixaca for strongly supporting this research. Instituto de Salud Carlos III, Fondo de Investigaciones Sanitarias. Plan Estatal I + D + I and Instituto de Salud Carlos III-Subdirección General de Evaluación y Fomento de la Investigación (Grant no.: PI13/00794); Red TerCel grants RD/0019/0001 and RD16/0011/0001. http://www.isciii.es/. Fondos FEDER (EDRF) “Una manera de hacer Europa” A way of making Europe. Also, we thank IMIB-Arrixaca and FFIS for technical support and assistance.
Author information
Authors and Affiliations
Contributions
A.B. performed the experiments. G.C. and J.M.M. supplied Amniotic membrane. A.B. and S.L. did the image analysis and quantification. S.L. performed statistical analysis. A.B., S.L. and F.J.N. prepared Figures 1–5. S.L. and F.J.N. wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bernabé-García, Á., Liarte, S., Moraleda, J.M. et al. Amniotic membrane promotes focal adhesion remodeling to stimulate cell migration. Sci Rep 7, 15262 (2017). https://doi.org/10.1038/s41598-017-15509-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-15509-z
This article is cited by
-
Comparison of the effects of preservation methods on structural, biological, and mechanical properties of the human amniotic membrane for medical applications
Cell and Tissue Banking (2024)
-
Human amniotic membrane inhibits migration and invasion of muscle-invasive bladder cancer urothelial cells by downregulating the FAK/PI3K/Akt/mTOR signalling pathway
Scientific Reports (2023)
-
Novel six-gene prognostic signature based on colon adenocarcinoma immune-related genes
BMC Bioinformatics (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.