Abstract
The prognosis of patients after thoracic endovascular aortic repair (TEVAR) is affected by several clinical characteristics. This study aimed to evaluate whether thyroid hormones predicts early (30 days) and mid-term (12 months) aorta-related adverse events (ARAE) and readmissions (ARAR) in patients after TEVAR. A total of 338 continuous patients who underwent TEVAR were included and stratified based on quartile of free thyroxine (FT4) levels examined before surgery. The relationship of FT4 levels with early or mid-term ARAE and ARAR were assessed using univariate and multiple logistic regression analysis. The incidence of ARAE and ARAR were 2.7% and 4.1% within 30 days, and 8.9% and 13.5% within 12 months, respectively. After adjusting for confounders, the lowest FT4 quartile group were noted to be at significantly greater risk than the highest FT4 quartile group in early (OR 10.105, 95% CI 1.103 to 92.615, P = 0.041) and mid-term (OR 5.687, 95% CI 1.708 to 18.935, P = 0.005) ARAR, but not significantly different in early (OR 2.097, 95% CI 0.228 to 19.307, P = 0.513) and mid-term (OR 0.695, 95% CI 0.207 to 2.332, P = 0.556) ARAE. Thus, patients with low-normal FT4 levels after TEVAR are at greater risk of ARAR, but not ARAE, in both the early and the mid-term follow-up periods.
Similar content being viewed by others
Introduction
Thoracic endovascular aortic repair (TEVAR) has been increasingly applied to treat a variety of aortic diseases1,2. Nevertheless, it is still a young technology with several unknowns, including the risk factors for the prognosis of patients after TEVAR. Thyroid hormones play important roles in the development and functioning of the circulatory system. Several studies have demonstrated that overt thyroid disorders, or even subclinical dysfunction, are associated with cardiovascular disease3,4,5,6,7. Blood pressure and heart rate, which can be affected by thyroid hormones, are associated with the prognosis of patients after TEVAR3,4,8,9.
It is unclear whether thyroid hormone levels are related to aortic diseases and whether thyroid hormones could provide valuable predictive information for patients after TEVAR. The aim of this study was to investigate the influence of thyroid hormones on aorta-related adverse events (ARAE) and readmissions (ARAR) during the early (30 days) and mid-term (12 months) follow-up periods after TEVAR.
Methods
Study population
A retrospective study was conducted on prospectively collected data of aortic disease patients undergoing TEVAR from January 2004 to December 2015 at Wuhan Asia Heart Hospital. Participants who had a medical history of aortic disease, Marfan syndrome or other connective tissue disease, cancer, renal insufficiency, and clinical hyperthyroidism or hypothyroidism were excluded. Participants who were scheduled to have or who underwent surgical procedures within 30 days of study enrolment were also excluded.
The methods in the study were in accordance with relevant guidelines and the Declaration of Helsinki. Written informed consent was obtained from all participants. All procedures were approved by the Ethics Committee of Wuhan Asia Heart Hospital and the Ethics Committee of The First Affiliated Hospital of Shantou University Medical College.
Procedures
All subjects routinely received a contrast-enhanced computed tomography (CT) scan before a TEVAR procedure. The indications for the TEVAR procedure were aortic dissection (AD), intramural hematoma (IMH), aortic aneurysm (AA), penetrating aortic ulcer (PAU), and traumatic aortic lesions10,11. Successful procedures were defined as technically accurate placement of the stent graft at the intended target location without endoleak11.
Subjects were classified into the acute group (≤14 days), the sub-acute group (15–90 days), and the chronic group (>90 days), based on the time interval from symptom onset date to procedure date10,11.
Diagnostic criteria
Concentrations of serum free triiodothyronine (FT3), free thyroxine (FT4) and thyroid-stimulating hormone (TSH) were measured on fasting, morning samples using 2 different assays. Hyperthyroidism and hypothyroidism were defined as serum TSH < 0.45 μU/L and TSH > 19.9 μU/L respectively5. All participants were stratified by quartiles based on of FT4 levels.
Persistent or unrelenting pain despite having received maximal medical therapy was considered as refractory pain12. Refractory hypertension was defined as persistent hypertension despite having received ≥3 different classes of antihypertensive therapies at best recommended or maximum tolerated doses12,13. Rupture or impending rupture was defined as extravasation of fresh blood outside the thoracic aorta or concomitant hemothorax documented by preoperative CT14.
Follow-up
All subjects were followed up by 3 clinical cardiologists at 30 days, 3 months, 6 months, and 12 months from the completion of the TEVAR procedure. Symptoms, medications, laboratory measurements, electrocardiogram and imaging tests (ultrasonic cardiogram and contrast-enhanced CT, depending on medical criteria) were collected by electronic data capture and telephone interviews. Early (30 days) and mid-term (12 months) ARAE and ARAR were the primary outcomes of our study.
ARAE was defined as aorta-related death, progression of aortic disease, organ failure or lower limb ischemia, aortic expansion of >5 mm, or endoleak. ARAR was defined as readmissions associated with any aorta-related complications, such as progression of aortic disease, organ failure or lower limb ischemia, surgical requirement, or occurrence of similar symptoms upon aortic disease onset without other diseases identified by a comprehensive clinical examination.
Statistical analysis
Continuous variables were presented as means ± standard deviations or medians (quartile 1 to quartile 3 [Q1–Q3]). Categorical variables were shown as counts and percentages. Analysis of variance, Kruskal-Wallis test, and Chi-square test were used to compare the difference in normal continuous variables, non-normal continuous variables and categorical variables, respectively. The relationship between thyroid hormones and 30-day or 12-month ARAE and ARAR were assessed using univariate and multiple logistic regression analysis. Candidate covariates for multivariable modelling were selected based on p-value (P) < 0.1 in univariate logistic regression analysis. Odds ratios (ORs) were presented with 95% confidence interval, and a two-tailed P < 0.05 was considered statistically significant. All data analyses were performed using the statistical software Statistical Product and Service Solution (SPSS 19.0 for Windows, Chicago, Illinois, USA).
Data availability statement
All raw data and analysis code are available from the corresponding author on reasonable request.
Results
Demographics
Three hundred and thirty-eight subjects (mean age 56.5 years, 276 males, 62 females) were included: 221 patients with AD, 78 patients with IMH, 32 patients with AA, and 7 patients with PAU. There were 182 subjects in the acute phase, 85 subjects in the sub-acute phase, and 71 subjects in the chronic phase.
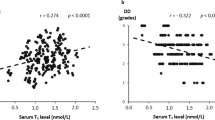
The clinical and operative procedure characteristics of subjects stratified by FT4 levels are shown in Table 1 and Table 2, respectively. None of the parameters were significantly different among the 4 levels. The medians (Q1–Q3, ng/dl) of the FT4 quartiles were 0.82 (0.76–0.86), 0.95 (0.92–0.98), 1.12 (1.07–1.17), and 1.35 (1.28–1.49), respectively.
Univariate analysis and multiple logistic regression analysis at early follow-up
All 338 patients completed 30 days of follow-up, and the incidence of patients with ARAR was 4.1%. The univariate analysis indicated that there were 3 variables (other than thyroid hormones) associated with early ARAR, including glomerular filtration rate (GFR), cerebrovascular diseases (CVD), and operative procedure. Multiple logistic regression showed that, FT4 levels (OR 0.079, 95% CI 0.004 to 1.074, P = 0.105) were not associated with 30-day ARAR when FT4 was analyzed as a continuous variable. When all participants were stratified into quartiles based on FT4 levels, the lowest FT4 quartile group were at significantly greater risk of 30-day ARAR (OR 10.105, 95% CI 1.103 to 92.615, P = 0.041) compared to the highest FT4 quartile group. There was no significant association between 30-day ARAR and neither FT3 (OR 3.288, 95% CI 0.780 to 13.859, P = 0.105) nor TSH OR 0.508, 95% CI 0.242 to 1.064, P = 0.073). Besides FT4, GFR (OR 0.972, 95% CI 0.946 to 0.999, P = 0.044) was another multivariable predictor of ARAR. The results of multivariable logistic analyses for ARAR within 30 days are shown in Table 3.
The incidence of patients with early ARAE was 2.7%. Operative procedure and blood transfused were variables significantly associated with ARAE on univariate analysis. The results of multiple logistic regression analysis showed that FT4 (OR 0.543, 95% CI 0.022 to 13.697, P = 0.711) was not associated with 30-day ARAE when FT4 was analyzed as a continuous variable. When all participants were stratified by quartiles of FT4, no significant associations were noted between 30-day ARAE and the lowest FT4 quartile group (OR 2.097, 95% CI 0.228 to 19.307, P = 0.513), FT3 (OR 3.168, 95% CI 0.688 to 14.587, P = 0.139), and TSH (OR 1.016, 95% CI 0.692 to 1.491, P = 0.937).
Univariate analysis and multiple logistic regression analysis at mid-term follow up
A total of 288 patients (85.2%) were followed-up with regard to 12-month ARAR; the percentage of patients that encountered ARAR was 13.5%. Potential risk factors for mid-term ARAR identified by univariate analysis were gender, tobacco abuse, peripheral arterial disease (PAD), CVD, GFR, and stage of aortic diseases. After adjustment for these factors, FT4 (OR 0.114, 95% CI 0.018 to 0.705, P = 0.019) was noted to be significantly associated with 12-month ARAR when FT4 was analyzed as a continuous variable. When all participants were stratified by quartiles of FT4, the risk of ARAR in subjects at the lowest FT4 quartile (OR 5.687, 95% CI 1.708 to 18.935, P = 0.005) and the 2nd quartile (OR 3.635, 95% CI 1.102 to 11.990, P = 0.034) was significantly greater than those subjects at the highest quartile. FT3 and TSH were not significantly associated with 12-month ARAR (OR 0.563, 95% CI 0.231 to 1.369, P = 0.205; OR 0.914, 95% CI 0.744 to 1.123, P = 0.393). Other multivariable predictors of ARAR were CVD (OR 3.161, 95% CI 1.392 to 7.177, P = 0.006) and chronicity (OR 3.177, 95% CI 1.247 to 7.790, P = 0.015) (Table 4).
Meanwhile, a total of 292 patients (86.4%) were followed-up with regard to 12-month ARAE; the incidence of 12-month ARAE was 8.9%. The results of univariate analysis showed that variables that were significantly associated with mid-term ARAE included gender, hypertension, and transfusion. Multiple logistic analysis revealed that FT4 (OR 1.015, 95% CI 0.640 to 1.608, P = 0.950) was not significantly associated with 12-month ARAE when FT4 was analyzed as a continuous variable. When all participants were stratified by quartiles of FT4, no significant associations were noted between 12-month ARAE and the lowest FT4 quartile group (OR 0.695, 95% CI 0.207 to 2.332, P = 0.556), FT3 (OR 1.108, 95% CI 0.449 to 2.733, P = 0.824), and TSH (OR 0.998, 95% CI 0.803 to 1.239, P = 0.983).
Discussion
This study showed that among subjects who underwent TEVAR, those who had low-normal levels of FT4 were at increased risk of ARAR compared to those with high-normal levels of FT4 in both early and mid-term follow-up.
The entire circulatory system and thyroid are closely linked by their embryological anlage. The metabolic functions and the effects of thyroid hormones on the heart and vasculature have been discussed in several studies. Thyroid hormones function in the maintenance of normal vascular remodeling. When the secretion of thyroid hormones is disordered, the altered blood coagulability and endothelial dysfunction will affect the remodeling of the damaged aorta, resulting in increased risk in developing aorta-related clinical symptoms and possible readmission15.
In spite of this, the relationship between subclinical hypothyroidism and cardiovascular diseases has not been fully elucidated. One of the most common cardiovascular manifestations of hypothyroidism is hypertension, which results from increasing systemic vascular resistance. Hypertension can be aggravated by hypothyroidism4. At the same time, hypertension can also lead to poor prognosis for patients after TEVAR10,16. Therefore, lower levels of thyroid hormones may cause patients to be at a higher risk of readmission.
Lower levels of FT4, even within the normal range, can influence increased arterial stiffness, coronary artery calcification, atherosclerosis, cardiac pump performance, and C-reactive protein4,17,18,19,20. These clinical characteristics are also predictive factors of the adverse outcomes in patients after TEVAR21,22,23. Owing to the aforementioned effects of thyroid hormones on the overall vascular system, it is reasonable to find an association between low-normal levels of FT4 and increased risk of ARAR in patients after TEVAR.
In addition to reflection of the negative feedback of T4 and T3, TSH also embodies other influences, such as drugs and non-thyroidal disease24. FT3 and FT4 levels are differentially associated with some cardiovascular risk markers in euthyroid subjects25. Therefore, it is plausible that the levels of FT4 reflect a more sensitive index of cardiac “thyroid status”. This could explain why in this study, FT4, but not TSH and FT3, was an independent predictor of aortic readmission. Similar findings on the relationship of thyroid hormones and cardiovascular diseases were also reported in previous studies9,25.
Monitoring both ARAE and ARAR could provide additional information than monitoring only one of these parameters. Some researchers have found an inverse relationship between the risk of adverse events and the risk of readmission. In other words, patients who are at higher risk of readmission are at lower risk of adverse events or mortality26,27,28. For patients after TEVAR, several studies focused on adverse events and ignored readmissions. However, the risk of readmission partially embodies the quality of health and hospital services. Therefore, those two endpoints were collected to obtain more information about the prognosis of patients after TEVAR. In this study, FT4 was associated with ARAR instead of adverse events. These findings are also consistent with studies on other predictors of adverse events and readmission. Factors that are weak predictors of readmission tend to be strong predictors of adverse events, and vice versa29,30. As a rationale for our study, there might be no relationships between readmissions and adverse events. The detailed relationship should be assessed in future studies.
There are several limitations in this study. Firstly, it was a retrospective, single-center study. Some variables that affect thyroid hormones were also not considered in our study. In subsequent researches, we will consider more variables that affect thyroid hormones. Secondly, the predictive value of overt thyroid disorders in patients after TEVAR was not analyzed because the number of patients with overt thyroid disorders was too small for the analysis to be effective. This should be assessed in future studies as well.
Conclusions
This study showed that, in comparison to patients with high-normal FT4 levels, patients with low-normal FT4 levels had greater risk of experiencing ARAR after TEVAR during the early and mid-term follow-up periods. In contrast, risk of ARAE was not significantly different in patients with differing FT4 levels. These findings need to be further verified in larger clinical studies before they can provide remarkable contributions to the prognostic assessment of patients after TEVAR.
References
Bicknell, C. & Powell, J. T. Aortic disease: thoracic endovascular aortic repair. Heart 101, 586–591, https://doi.org/10.1136/heartjnl-2014-306690 (2015).
Qin, Y. L. et al. Endovascular Repair Compared With Medical Management of Patients With Uncomplicated Type B Acute Aortic Dissection. Journal of the American College of Cardiology 67, 2835–2842, https://doi.org/10.1016/j.jacc.2016.03.578 (2016).
Collet, T. H. et al. Subclinical hyperthyroidism and the risk of coronary heart disease and mortality. Arch Intern Med 172, 799–809, https://doi.org/10.1001/archinternmed.2012.402 (2012).
Grais, I. M. & Sowers, J. R. Thyroid and the heart. Am J Med 127, 691–698, https://doi.org/10.1016/j.amjmed.2014.03.009 (2014).
Kim, E. J. et al. Relation of hypothyroidism and incident atrial fibrillation (from the Framingham Heart Study). Am Heart J 167, 123–126, https://doi.org/10.1016/j.ahj.2013.10.012 (2014).
Biondi, B. & Klein, I. Hypothyroidism as a risk factor for cardiovascular disease. Endocrine 24, 1–13, https://doi.org/10.1385/endo:24:1:001 (2004).
Razvi, S., Weaver, J. U., Butler, T. J. & Pearce, S. H. Levothyroxine treatment of subclinical hypothyroidism, fatal and nonfatal cardiovascular events, and mortality. Arch Intern Med 172, 811–817, https://doi.org/10.1001/archinternmed.2012.1159 (2012).
Razvi, S. W. J., Butler, T. J. & Pearce, S. H. Levothyroxine treatment of subclinical hypothyroidism, fatal and nonfatal cardiovascular events and mortality. Arch Intern Med 172, 811–817 (2012).
Sousa, P. A. et al. Impact of Free Thyroxine on the Outcomes of Left Atrial Ablation Procedures. The American journal of cardiology 116, 1863–1868, https://doi.org/10.1016/j.amjcard.2015.09.028 (2015).
Erbel, R. et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). European heart journal 35, 2873–2926, https://doi.org/10.1093/eurheartj/ehu281 (2014).
Hiratzka, L. F. et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the diagnosis and management of patients with thoracic aortic disease. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology,American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons,and Society for Vascular Medicine. Journal of the American College of Cardiology 55, e27–e129, https://doi.org/10.1016/j.jacc.2010.02.015 (2010).
Trimarchi, S. et al. Importance of refractory pain and hypertension in acute type B aortic dissection: insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation 122, 1283–1289, https://doi.org/10.1161/CIRCULATIONAHA.109.929422 (2010).
Fattori, R. et al. Interdisciplinary expert consensus document on management of type B aortic dissection. Journal of the American College of Cardiology 61, 1661–1678, https://doi.org/10.1016/j.jacc.2012.11.072 (2013).
Faure, E. M., Canaud, L., Marty-Ane, C., Becquemin, J. P. & Alric, P. Endovascular management of rupture in acute type B aortic dissections. Eur J Vasc Endovasc Surg 49, 655–660, https://doi.org/10.1016/j.ejvs.2015.01.025 (2015).
Squizzato, A., Romualdi, E., Buller, H. R. & Gerdes, V. E. Clinical review: Thyroid dysfunction and effects on coagulation and fibrinolysis: a systematic review. J Clin Endocrinol Metab 92, 2415–2420, https://doi.org/10.1210/jc.2007-0199 (2007).
Melby, S. J., Zierer, A., Damiano, R. J. Jr & Moon, M. R. Importance of blood pressure control after repair of acute type a aortic dissection: 25-year follow-up in 252 patients. J Clin Hypertens (Greenwich) 15, 63–68, https://doi.org/10.1111/jch.12024 (2013).
Klein, B. B. a. I. Hypothyroidism as a Risk Factor for Cardiovascular Disease. Endocrine June, 1–13 (2004).
Klein Irwin, O. K. Thyroid hormone and the cardiovascular system. N Engl J Med Feb 15, 501–509, https://doi.org/10.1056/NEJM200102153440707 (N Engl J Med).
Kim, E. S. et al. Association between low serum free thyroxine concentrations and coronary artery calcification in healthy euthyroid subjects. Thyroid 22, 870–876, https://doi.org/10.1089/thy.2011.0366 (2012).
Wang, J. et al. Low serum free thyroxine concentrations associate with increased arterial stiffness in euthyroid subjects: a population-based cross-sectional study. Endocrine 50, 465–473, https://doi.org/10.1007/s12020-015-0602-1 (2015).
Sakakura, K. et al. Peak C-reactive protein level predicts long-term outcomes in type B acute aortic dissection. Hypertension 55, 422–429, https://doi.org/10.1161/HYPERTENSIONAHA.109.143131 (2010).
Okina, N. et al. Utility of measuring C-reactive protein for prediction of in-hospital events in patients with acute aortic dissection. Heart Vessels 28, 330–335, https://doi.org/10.1007/s00380-012-0257-2 (2013).
Wen, D., Du, X., Dong, J. Z., Zhou, X. L. & Ma, C. S. Value of D-dimer and C reactive protein in predicting inhospital death in acute aortic dissection. Heart 99, 1192–1197, https://doi.org/10.1136/heartjnl-2013-304158 (2013).
Surks, M. I. & Sievert, R. Drugs and thyroid function. N Engl J Med 333, 1688–1694, https://doi.org/10.1056/nejm199512213332507 (1995).
Roef, G. L. et al. Triiodothyronine and free thyroxine levels are differentially associated with metabolic profile and adiposity-related cardiovascular risk markers in euthyroid middle-aged subjects. Thyroid 24, 223–231, https://doi.org/10.1089/thy.2013.0314 (2014).
Gorodeski, E. Z. & Blackstone, S. R. E. H. Are All Readmissions Bad Readmissions? N Engl J Med 15, 297–298, https://doi.org/10.1056/NEJMc1001882 (2010).
Heidenreich, P. A., Sahay, A., Kapoor, J. R., Pham, M. X. & Massie, B. Divergent trends in survival and readmission following a hospitalization for heart failure in the Veterans Affairs health care system 2002 to 2006. Journal of the American College of Cardiology 56, 362–368, https://doi.org/10.1016/j.jacc.2010.02.053 (2010).
Ong, M. K. et al. Looking Forward, Looking Back: Assessing Variations in Hospital Resource Use and Outcomes for Elderly Patients with Heart Failure. Circ Cardiovasc Qual Outcomes 2(6), 548–557, https://doi.org/10.1161/CIRCOUTCOMES (2009).
Lindenauer P. K. et al. The performance of US hospitals as reflected in risk-standardized 30-day mortality and readmission rates for medicare beneficiaries with pneumonia. J Hosp Med Jul-Aug, E12–18, https://doi.org/10.1002/jhm.822 (2010).
Harlan, M. et al. An Administrative Claims Measure Suitable for Profiling Hospital Performance Based on 30-Day All-Cause Readmission Rates Among Patients With Acute Myocardial Infarction. Circ Cardiovasc Qual Outcomes March, 243–252, https://doi.org/10.1161/CIRCOUTCOMES (2011).
Acknowledgements
This work was supported by National Natural Science Foundation of China (No. 81473063).
Author information
Authors and Affiliations
Contributions
N.L. contributed to the conception, design, data analysis and writing. Z.Q.H., T.X., X.J.M. and X.R.T. contributed to conception and design, X.C. and X.F.C. contributed to acquisition of data. All authors reviewed this manuscript and approved the final version to be published.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lu, N., He, Z., Xu, T. et al. Association of Thyroid Function with Early/Mid-term Aorta-Related Adverse Events and Readmissions after Thoracic Endovascular Aortic Repair. Sci Rep 7, 14730 (2017). https://doi.org/10.1038/s41598-017-15370-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-15370-0
This article is cited by
-
Non-O blood group is associated with lower risk of in-hospital mortality in non-surgically managed patients with type A aortic dissection
BMC Cardiovascular Disorders (2020)
-
Optimal blood pressure control for patients after thoracic endovascular aortic repair of type B aortic dissection
BMC Cardiovascular Disorders (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.