Abstract
Physical activity, screen viewing, sleep, and homework among children have been independently linked to health outcomes. However, few studies have assessed the independent associations between time spent in daily activities and children’s physical and mental health. This study describes time spent in four activities among primary school students in Shanghai, and examines the relationship between daily time-use patterns and obesity and mental health. The representative sample consists of 17,318 children aged 6–11 years in Shanghai. Time spent in moderate to vigorous physical activities (MVPA), screen viewing, sleep, and homework was measured by validated questionnaires. Logistic regressions were performed. We also fitted generalized additive models (GAM) and performed two-objective optimization to minimize the probability of poor mental health and obesity. In 2014, 33.7% of children spent ˂1 hour/day on MVPA, 15.6% spent ≥ 2 hours/day on screen viewing, 12.4% spent ˂ 9 hours/day on sleep, and 27.2% spent ≥ 2 hours/day on homework. The optimization results suggest that considering the 24-hour time limit, children face trade-offs when allocating time. A priority should be given to the duration of sleep and MVPA. Screen exposure should be minimized to save more time for sleep and other beneficial activities.
Similar content being viewed by others
Introduction
A burgeoning literature has linked moderate to vigorous physical activity (MVPA) to improved health outcomes in children and adolescents1,2,3. MVPA generates more energy expenditure, reduces children’s cardio-metabolic risk factors, and improves mood, attention, cognition and academic performance3,4,5,6,7,8. In contrast, sedentary behaviors such as television viewing, video-game playing, computer use, and in some cases, excessive time spent on homework have been shown to be related to adverse health outcomes9,10,11, potentially offsetting the beneficial effects of MVPA on health12. One can be both active and sedentary. Vice-versa, one can also be inactive but not sedentary. These two dimensions have been independently related to health outcomes13. In addition to inadequate MVPA and sedentary lifestyles, evidence also supports a relationship between short sleep duration and increased risk of childhood obesity14,15, as well as behavioral and depressive symptoms16. Although evidence linking behaviors and health is strong, most studies to date have focused on the relationship between time spent in a single activity and health outcomes. Guidelines about children’s time use have been proposed separately for each behavior without the benefit of analyses controlling for time spent in multiple activities. Specifically, the World Health Organization recommends at least 60 minutes of MVPA daily for children aged 5–17 years17, the American Academy of Pediatrics (AAP) recommends less than 2 hours of screen viewing for children and adolescents18, the United States (US) National Sleep Foundation recommends a 9–11 hour sleep duration for school-aged children19, and the US National Education Association recommends 10 to 50 minutes of homework per day for students in grades 1 through 520. Yet, time use is determined across several categories such that greater time use in one activity may mean less time use in another activity. It is important, therefore, to obtain estimates of the associations between time use in multiple activities and health outcomes and to further examine the combined associations. Previous studies have examined the combination of behaviors associated with children’s health21,22. However, those studies were limited because they defined daily activities based on energy expenditure rather than time allocation to specific behaviors.
For school children, time allocation during school is relatively fixed by the curriculum. Children’s major activities after school include MVPA, screen viewing, homework and sleep, all of which have been related to health outcomes. While Shanghai’s education model has drawn global attention for its top ranking in the Program for International Student Assessment (PISA)23, concerns about declining physical fitness and overall health in children have increased. The obesity prevalence of Shanghai’s primary school students was almost as high as that of children in developed countries24. Studies have also reported that Chinese students experienced high levels of academic stress25. It is therefore warranted to evaluate lifestyles, behaviors, and health status in these children. Using a population-based survey conducted among primary school students in Shanghai, this study aims to (1) assess the distribution of children’s daily time spent in MVPA, screen viewing, homework, and sleep; (2) evaluate the combined associations between daily time use in several activities and obesity and poor mental health, two most pressing public health issues affecting child development in Chinese children.
Methods
Study design and data collection
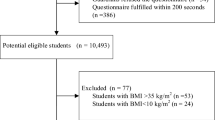
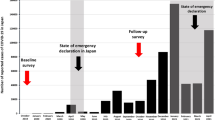
We conducted the Shanghai Children’s Health, Education and Lifestyle Evaluation (SCHEDULE) study in July, 2014. The SCHEDULE was designed to represent children aged 6 to 11 years (grades 1 to 5) in Shanghai’s primary schools. We excluded students with special needs or at international schools. The SCHEDULE investigated a broad range of questions including socio-demographic characteristics, health behaviors (i.e., physical activity, sleep duration, and sedentary behaviors), health status (i.e., body mass index (BMI), self-reported health problems, mental health status), and academic performances.
We selected study participants using a multistage cluster sampling approach. There are 16 districts and 1 county in Shanghai. Six districts and 1 county were randomly selected to represent the entire city. Second, we randomly selected 26 public primary schools, the primary sampling units (PSUs), from the 7 districts/county in proportion to population size. Third, we stratified the sampled schools by school size. All students from grades 1 to 5 were selected if a school had less than 1000 students, and half of the students in a school were selected if the number of students was above 1000, with random selection of class numbers. Finally, we conducted interviews among the sampled students as well as one of their parents and the head teacher of their classes. The initial sample consisted of 17,624 participants, and 17,318 of them answered the questionnaires. Sampling weights were computed using inverse probability weighting, which represented the inverse of the combined selection probability for each stage, including the non-response rate (1.74%). Details of the sampling procedures and quality control strategies were presented in Appendix 1.
The study was approved by the institutional review board of the Shanghai Children’s Medical Center (SCMC), Shanghai Jiao Tong University (SCMCIRB-K2014033). All methods were performed in accordance with the relevant guidelines and regulations. All parents and teachers of the children who participated in the study gave written informed consent.
Measurements
Time spent in MVPA, screen viewing, and homework during weekdays and weekends was measured using the Chinese version of the International Children’s Leisure Activities Study Survey Questionnaire (CLASS-C) which was validated in Hongkong population26. CLASS-C is a 7-day recall questionnaire used to measure MVPA and sedentary behaviors among school-aged children and adolescents26. Studies found that the CLASS-C had good test-retest reliability and acceptable criterion validity when compared with accelerometer-measured MVPA26. Screen viewing included watching television, playing video games, and using computers. Homework included assignments from both schools and extracurricular studies. We first derived the average time spent in MVPA, screen viewing, and homework per day, then categorized the variables as ˂1 hour, 1–2 hours, and ≥2 based on the current guidelines and their distributions in the population.
For sleep duration, children’s bedtimes and waking times on weekdays and weekends during the past month were collected from parental report (e.g., ‘what was the usual bedtime on weekdays during the past month? What was the usual bedtime on weekends during the past month?’). The average sleep duration was calculated using the formula: ([weekday sleep duration × 5] + [weekend sleep duration × 2])/7. This sleep questionnaire produces estimates reasonably consistent with objectively-measured sleep duration by actigraphy (r = 0.59–0.74)27.
Anthropometric data including height and weight were measured three times by the same group of medical staff from the SCMC. The average measures were used to compute the BMI by dividing the weight in kilograms by the square of the height in meters. Obesity status was determined based on sex specific BMI-for-age cutoff standard for Chinese children28.
Children’s mental health status was ascertained with 25 questions in the Chinese version of the parent-reported Strengths and Difficulties Questionnaire (SDQ), a brief behavioral and psychosocial wellbeing screening questionnaire for children aged 3 to 16 years29,30. Previous studies confirmed the questionnaire’s reliability and validity among primary school children in China31,32. Poor mental health was defined based on the cutoff scores of the total difficulties (SDQ ≥ 17)33.
Controlled variables associated with obesity and poor mental health included children’s age (<8, 8–10, ≥10 years), gender and health status (parent-reported having any chronic health problems such as asthma, rhinitis and etc.), household income (<30,000 Renmingbi (RMB), 30,000–100,000 RMB, ≥100,000 RMB) and parents’ highest educational attainment (middle school and below, high school, college and above).
For the model using obesity as an outcome, paternal and maternal BMI and children’s dietary patterns were further controlled. Children’s dietary patterns were evaluated with a modified food frequency questionnaire (FFQ) with nine food items34. Parents were asked to estimate the frequency with which their children consumed these foods during the past month by selecting one of three responses: 0–2 times a week, 3–5 times a week, or 6 or more times a week. Factor analysis was used to derive two main factors describing the dietary patterns: “healthy dietary factor score” and “unhealthy dietary factor score.”35 Details about the FFQ analysis were presented in Appendix 2.
Data analysis
Descriptive analyses were initially conducted to assess the percentage of missing values in all variables. We performed multiple imputations five times with a chained approach and separate regression model for each variable (missing value patterns and imputation process were presented in Appendix 1). Using the multiply imputed sample, we first described the average time spent in MVPA, screen viewing, homework, and sleep per day, the distributions of these four time variables, and the categorical demographic variables by the two health outcomes. We applied sampling weights in all analyses. Next, survey-weighted logistic regressions were used to estimate the simultaneous associations between the time spent in each activity and obesity and poor mental health after adjusting for age, gender, annual household income, parents’ highest educational attainment, and the presence of health problems. In the regression with obesity as the outcome, dietary patterns and parents’ BMI were further added as covariates. Finally, we fitted generalized additive models (GAM) using the same covariates as in the logistic regression models and performed two-objective optimization to minimize the probability of poor mental health and obesity. We chose GAM because it extends logistic regression to allow for non-linear association and serves as useful tools for finding the optimal time allocation strategies. In the optimization procedure, we gave equal weights to the two probabilities and minimize the sum of the two as we viewed the two outcomes equally important. We also considered the trade-off between activities that the increased time in one activity necessarily decreases the time spent in other activities, and therefore we set the sum of the four time variables (sleep, MVPA, screen, and homework) as fixed and searched for the optimal time allocation strategy. Further, because the total time of the four variables ranges between 10 to 15 hours in 90% of our data, we performed optimization under the sum constraint at 10, 11,…, 15 hours respectively and provided the optimal time allocation strategy under each time constraint. Details about the optimization analysis were presented in Appendix 3. Descriptive and regression analyses were performed using STATA 14.2 (StataCorp LP, College Station, TX). Odds ratios (ORs) with 95% confidence intervals (CIs) were reported. Sampling weights were used in all analyses to ensure representativeness. Two-objective optimization was performed in R (version 3.3.2) and R package mgcv was used36.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Results
The prevalence of obesity in Shanghai’s primary school students was 10.3% (Table 1). For children who were obese, the distribution of MVPA time did not vary significantly by weight status. However, ≥2 hours of screen time was more prevalent among those who were obese (19.8% vs. 15.1%, p = 0.001). Also, the percentage of children who had sleep duration of < 9 hour was significantly higher in those who were obese (16.5% vs. 12.0%, p < 0.001) and so was the percentage of children spent ≥ 2 hours on homework (31.2% vs. 26.8%, p < 0.05). Boys, children with health problems, children whose parents had higher BMI and children with higher unhealthy dietary scores were more likely to be obese (p < 0.05).
Table 2 presents the association between time-use categories and obesity, after adjusting for related covariates. The odds ratio of time spent in each activity compared with the current guideline-recommended time (MVPA: 1–2 hours; screen time:<1 hour; sleep duration:≥10 hours; homework:<1 hour) shows that among time spent in the four lifestyle behaviors, insufficient sleep had the largest magnitudes of association with both obesity and poor mental health. In the obesity model, screen viewing for over 2 hours per day was associated with higher odds of obesity (OR = 1.38, 95% CI: 1.14, 1.66). Less than 9 hours of sleep predicted higher odds of being obese (OR = 1.91, 95% CI: 1.50, 2.43). However, time spent in MVPA and homework was not associated with the odds of obesity.
The prevalence of poor mental health in Shanghai’s primary school students was 11.3% (Table 1). Among children who had poor mental health, we observed that a higher percentage of children spent ˂ 1 hour on MVPA (44.7% vs. 32.3%, p < 0.001). Also, compared to children with good mental health, more children with poor mental health had ≥ 2 hours of screen time (18.2% vs. 15.3%, p = 0.011) and had sleep duration of ˂9 hours (18.4% vs 11.7%, p < 0.001). Boys, children at younger age, children with health problems, children whose parents had a lower educational level and those from families with lower household income were more likely to have poor mental health (p < 0.001).
In the logistic regression model for mental health, compared with 1–2 hours of MVPA, less than 1 hour of MVPA was associated with significantly higher odds of poor mental health (OR = 1.37, 95% CI: 1.15, 1.64). Same was found for over 2 hours of screen viewing (OR = 1.28, 95% CI: 1.05, 1.55) and less than 9 hours of sleep duration (OR = 2.17, 95% CI: 1.71, 2.76). Doing homework for 1–2 hours per day was significantly associated with lower odds of poor mental health compared with ˂ 1 hour of homework (OR = 0.70, 95% CI: 0.57, 0.85) (Table 2).
Figure 1(a) shows the GAM fitted smooth functions for the association between the four time variables and obesity. As the GAM analysis suggests, obesity was strongly associated with screen exposure and duration of sleep but not with MVPA and homework. An increase in the time of screen exposure led to an increase in the probability of obesity. As the duration of sleep increased from 7 to around 11 hours, the probability of obesity decreased.
The GAM fitted smooth functions for the association between the four time variables and the two outcomes respectively. Solid line - the estimated smooth function on the scale of the linear predictor. Dotted line - the 95% confidence interval for the estimated function. Bottom - rug plot showing the distribution of the covariate.
Figure 1(b) shows the GAM fitted smooth functions for the association between the four time variables and mental health, and poor mental health was significantly associated with all four variables. MVPA and sleep were both negatively associated with poor mental health, but the strength of association varied over different values of the time variables. Increasing the time spent in MVPA from 0 to 2 hours and increasing the duration of sleep from 8 to 10 hours led to a decrease in the probability of having mental health problems. However, a further increase in time spent in either activity would not be as effective in decreasing the probability, as the estimated function suggested a smaller slope and a weaker effect. For screen exposure, its association with poor mental health was moderately significant (p-value 0.025). If the time of screen exposure increased from 0 to 2 hours, the probability of having mental health problems increased. Spending too little time and spending too much time on homework were both not beneficial for mental health. Allocating 1 to 2 hours to homework led to a relatively low probability of poor mental health.
Therefore, in the two-objective optimization based on GAM, as the total time increased, the extra time was first allocated to the duration of sleep to ensure enough sleep (Table 3). The extra time was further added to MVPA and homework. After enough sleep was guaranteed, allocating the extra time to MVPA was preferred. Screen exposure should be minimized at all times to save more time for sleep and other beneficial activities.
Discussion
Using a representative sample, our study found primary school students in Shanghai spent on average 1.69 hours on MVPA, 1.10 hours viewing screen, 1.27 hours doing homework, and 9.60 hours sleeping per day. Children who spent more time in screen viewing and less time in sleep have higher odds to be obese and those who spent less time in MVPA, sleep and more time in in screen viewing are more likely to have suboptimal mental health. Among all the activities, the magnitudes of sleep associated with both outcomes are the largest.
Using CLASS, a study in Australia reported that children aged 9–12 spent on average 2.14 hours daily on MVPA37. Another study in Hong Kong reported that children aged 9–14 spent 1.24 hours daily on MVPA38. As for screen viewing, Shanghai students spent more time than US students aged 6–11 (1.10 vs. 0.89 hours)39.
However, Shanghai students spent less time on sleep. A study comparing the sleep durations of primary school students showed that the sleep duration of Chinese children was 1 hour shorter than that of US children (9.25 vs. 10.15 hours)40. They also had a shorter sleep duration than British students (9.82 hours)41, but a longer sleep duration than their Hong Kong counterparts (8.79 hours)42. Overall, inadequate sleep has been a major concern among primary school students in Shanghai.
Extensive literature has linked each of the health behaviors we studied and health outcomes43,44,45,46,47,48. However, considering the 24-hour time limit, children face trade-offs when allocating their time. Longer screen time often implies shorter sleep duration or reduced homework time24,49, while more time doing homework may be linked to a later bedtime and shorter sleep duration50. The competing nature of these behaviors hinders our understanding of whether the association was resulted from the behavior itself or the displacement of another behavior. It is often difficult to disentangle the potential mechanisms behind the associations, which could be meaningful for developing effective interventions. To address this issue, several studies have investigated screen exposure and physical activity simultaneously. Studies have found that, compared with MVPA, screen time has a stronger association with BMI51,52. But long screen time and insufficient MVPA both independently predicted depressive and anxiety symptoms and school life dissatisfaction53. Sleep duration was also linked to obesity as strongly as sitting time and even more strongly than physical activity54. In our study, inadequate sleep was associated with the greatest odds for both obesity and poor mental health, which may reflect the problem of insufficient sleep among students in Shanghai. In fact, a local policy has been implemented in 2005 to delay school start times. This policy has increased students’ sleep duration from 9.35 hours per day in 200555. However, the problem has not yet been fully addressed. More efforts from parents, schools, and communities are needed.
To better understand the associations between different time-use patterns and obesity and mental health, we performed an optimization analysis with total time constraints of the four activities ranging from 10 to 15 hours. It is noteworthy that, even though the current guidelines suggest that screen time should not exceed 2 hours per day, the increased time allocated to screen viewing would decrease the time spent in other beneficial activities. Based on the optimization results, screen time should be minimized to ensure enough sleep and allow for more time in healthy activities such as MVPA. This is also consistent with the latest AAP recommendations for children’s media use, which suggested that for children aged 6 and older, parents should place consistent limits on the time spent on screens, and make sure that screen time did not take the place of sleep, physical activity, or other behaviors beneficial for health56.
To our knowledge, this was the first study to report the combined association between MVPA, screen exposure, sleep, homework and BMI and mental health in primary school children. Many countries, including the US and UK, have shown increasing interest in understanding whether the top-ranked Shanghai education model also benefits students’ health23. The current study showed that certain time use patterns in Shanghai’s students were not optimal for health.
There were several limitations in this study. First, for sleep and MVPA, it would be more accurate to use objective measurement such as accelerometers. Self-reported information using questionnaires can suffer from social desirability bias, such as overestimating MVPA. And for screen exposure, CLASS-C did not include time that children spent with tablets and smartphones. The total screen time may be underestimated. Second, we chose BMI and mental health as the study outcomes and did not examine other issues that may also be of interest to the development of school-aged children, such as scholastic performance. Future studies are needed to evaluate the overall development of children. Third, the cross-sectional nature of the study restricted our potential to identify a causal link between daily time use and children’s health and did not rule out the possibility of reverse causality between the health behaviors and outcomes under study. Intervention studies would be warranted to clarify the causal pathways and illustrate the mechanisms between time use patterns and obesity and mental health.
The findings from this study suggested that students’ daily time allocation was related to their physical and mental health. Insufficient sleep and too much screen time were two major concerns among primary school students in Shanghai. Guidelines for school-aged children should consider the overall time use pattern to promote children’s health.
References
Biddle, S. J. & Asare, M. Physical activity and mental health in children and adolescents: a review of reviews. British journal of sports medicine, bjsports90185 (2011).
Strong, W. B. et al. Evidence based physical activity for school-age youth. The Journal of pediatrics 146, 732–737 (2005).
Willis, E. A. et al. Length of moderate-to-vigorous physical activity bouts and cardio-metabolic risk factors in elementary school children. Preventive medicine 73, 76–80 (2015).
Puyau, M. R., Adolph, A. L., Vohra, F. A., Zakeri, I. & Butte, N. F. Prediction of activity energy expenditure using accelerometers in children. Medicine and science in sports and exercise 36, 1625–1631 (2004).
Tomporowski, P. D. Cognitive and behavioral responses to acute exercise in youths: A review. Pediatric Exercise Science 15, 348–359 (2003).
Ahamed, Y. et al. School-based physical activity does not compromise children’s academic performance. Medicine and Science in Sports and Exercise 39, 371 (2007).
Control, C.f.D. & Prevention The association between school based physical activity, including physical education, and academic performance. Atlanta, GA : US Department of Health and Human Services 500, 5–32 (2010).
Zhang, Y. et al. Association between physical activity and teacher-reported academic performance among fifth-graders in Shanghai: a quantile regression. PloS one 10, e0115483 (2015).
Mendoza, J. A., Zimmerman, F. J. & Christakis, D. A. Television viewing, computer use, obesity, and adiposity in US preschool children. International Journal of Behavioral Nutrition and Physical Activity 4, 44 (2007).
Wake, M., Hesketh, K. & Waters, E. Television, computer use and body mass index in Australian primary school children. Journal of paediatrics and child health 39, 130–134 (2003).
Cooper, H. & Valentine, J. C. Using research to answer practical questions about homework. Educational Psychologist 36, 143–153 (2001).
Dunstan, D. W., Thorp, A. A. & Healy, G. N. Prolonged sitting: is it a distinct coronary heart disease risk factor? Current opinion in cardiology 26, 412–419 (2011).
Ekelund, U. et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 388, 1302 (2016).
Cappuccio, F.P. et al. Meta-analysis of short sleep duration and obesity in children and adults. SLEEP-NEW YORK THEN WESTCHESTER - 31, 619 (2008).
Chen, X., Beydoun, M. A. & Wang, Y. Is sleep duration associated with childhood obesity? A systematic review and meta‐analysis. Obesity 16, 265–274 (2008).
Paavonen, E. J. et al. Short sleep duration and behavioral symptoms of attention-deficit/hyperactivity disorder in healthy 7-to 8-year-old children. Pediatrics 123, e857–e864 (2009).
Organization, W.H. Global recommendations on physical activity for health. (2010).
Gentile, D. A. et al. Well-child visits in the video age: pediatricians and the American Academy of Pediatrics’ guidelines for children’s media use. Pediatrics 114, 1235–1241 (2004).
Hirshkowitz, M. et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health 1, 40–43 (2015).
Cooper, H. The battle over homework: Common ground for administrators, teachers, and parents. (Corwin Press, 2006).
Carson, V., Tremblay, M. S., Chaput, J. P. & Chastin, S. F. Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Applied physiology, nutrition, and metabolism=Physiologie appliquee, nutrition et metabolisme 41, S294–302 (2016).
Chastin, S. F., Palarea-Albaladejo, J., Dontje, M. L. & Skelton, D. A. Combined Effects of Time Spent in Physical Activity, Sedentary Behaviors and Sleep on Obesity and Cardio-Metabolic Health Markers: A Novel Compositional Data Analysis Approach. PLoS One 10, e0139984 (2015).
Sellar, S. & Lingard, B. Looking East: Shanghai, PISA 2009 and the reconstitution of reference societies in the global education policy field. Comparative Education 49, 464–485 (2013).
Hale, L. & Guan, S. Screen time and sleep among school-aged children and adolescents: A systematic literature review. Sleep medicine reviews 21, 50–58 (2015).
Zhao, X., Selman, R. L. & Haste, H. Academic stress in Chinese schools and a proposed preventive intervention program. Cogent Education 2, 1000477 (2015).
Huang, Y., Wong, S. H. & Salmon, J. Reliability and validity of the modified Chinese version of the Children’s Leisure Activities Study Survey (CLASS) questionnaire in assessing physical activity among Hong Kong children. Pediatric exercise science 21, 339 (2009).
Chen, W. J. et al. Comparative study of children’s sleep evaluation methods. Zhonghua Er Ke Za Zhi 50, 293 (2012).
Cole, T. & Lobstein, T. Extended international (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatric obesity 7, 284–294 (2012).
Goodman, R. Psychometric Properties of the Strengths and Difficulties Questionnaire. Journal of the American Academy of Child & Adolescent Psychiatry 40, 1337–1345 (2001).
Goodman, R., Ford, T., Simmons, H., Gatward, R. & Meltzer, H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. The British Journal of Psychiatry 177, 534–539 (2000).
Du, Y., Kou, J. & Coghill, D. The validity, reliability and normative scores of the parent, teacher and self report versions of the Strengths and Difficulties Questionnaire in China. Child and Adolescent Psychiatry and Mental Health 2, 8 (2008).
Lai, K. Y. et al. Validation of the Chinese version of the strengths and difficulties questionnaire in Hong Kong. Social psychiatry and psychiatric epidemiology 45, 1179–1186 (2010).
Qin, Q. et al. Using the strengths and difficulties questionnaire to screen for child mental health in the twins and the only-child. Int J Clin Exp Med 9, 8749–8754 (2016).
Popkin, B. The nutritional status and dietary pattern of Chinese adolescents, 1991 and 1993. European Journal of Clinical Nutrition 52, 908–916 (1999).
Newby, P. K. & Tucker, K. L. Empirically derived eating patterns using factor or cluster analysis: a review. Nutrition Reviews 62, 177 (2004).
Wood, S. N. Fast stable restricted maximum likelihood and marginal likelihood estimation of semiparametric generalized linear models. Journal of the Royal Statistical Society 73, 3–36 (2011).
Hume, C. et al. Are children’s perceptions of neighbourhood social environments associated with their walking and physical activity? Journal of Science and Medicine in Sport 12, 637–641 (2009).
Huang, Y. J., Wong, S. H., Salmon, J. & Hui, S. S. Reliability and validity of psychosocial and environmental correlates measures of physical activity and screen-based behaviors among Chinese children in Hong Kong. International Journal of Behavioral Nutrition and Physical Activity 8, 1–9 (2011).
Fakhouri, T. H., Hughes, J. P., Brody, D. J., Kit, B. K. & Ogden, C. L. Physical activity and screen-time viewing among elementary school–aged children in the United States from 2009 to 2010. Jama Pediatrics 167, 223–229 (2013).
Liu, X., Liu, L., Owens, J. A. & Kaplan, D. L. Sleep patterns and sleep problems among schoolchildren in the United States and China. Pediatrics 115, 241–249 (2005).
Blair, P. S. et al. Childhood sleep duration and associated demographic characteristics in an English cohort. Sleep 35, 353–360 (2012).
Ng, D. K. et al. Prevalence of sleep problems in Hong Kong primary school children: a community-based telephone survey. CHEST Journal 128, 1315–1323 (2005).
PrenticeDunn, H. & PrenticeDunn, S. Physical activity, sedentary behavior, and childhood obesity: A review of cross-sectional studies. Psychology Health & Medicine 17, 255–273 (2012).
Mitchell, J. A., Daniel, R., Schmitz, K. H. & Janet, A. M. Greater screen time is associated with adolescent obesity: a longitudinal study of the BMI distribution from ages 14 to 18. Obesity 21, 572 (2013).
Fatima, Y., Doi, S. A. & Mamun, A. A. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obesity Reviews 16, 137 (2015).
Matamura, M. et al. Associations between sleep habits and mental health status and suicidality in a longitudinal survey of monozygotic twin adolescents. Journal of Sleep Research 23, 290–294 (2014).
Michaud, I., Chaput, J. P., O’Loughlin, J., Tremblay, A. & Mathieu, M. E. Long duration of stressful homework as a potential obesogenic factor in children: A QUALITY study. Obesity 23, 815–822 (2015).
Mchale, S. M. et al. The Role of Daily Activities in Youths’ Stress Physiology. Journal of Adolescent Health Official Publication of the Society for Adolescent Medicine 51, 623–628 (2012).
Vandewater, E. A., Bickham, D. S. & Lee, J. H. Time well spent? Relating television use to children’s free-time activities. Pediatrics 117, 181–191 (2006).
Sun, W. Q. et al. The relation among sleep duration, homework burden, and sleep hygiene in chinese school-aged children. Behavioral sleep medicine 12, 398–411 (2014).
Eisenmann, J. C., Bartee, R. T., Smith, D. T., Welk, G. J. & Fu, Q. Combined influence of physical activity and television viewing on the risk of overweight in US youth. International journal of obesity (2005) 32, 613–618 (2008).
Maher, C., Olds, T. S., Eisenmann, J. C. & Dollman, J. Screen time is more strongly associated than physical activity with overweight and obesity in 9- to 16-year-old Australians. Acta Paediatrica 101, 1170–1174 (2012).
Cao, H. et al. Screen time, physical activity and mental health among urban adolescents in China. Preventive medicine 53, 316–320 (2011).
Kong, I. G., Lee, H. J., Kim, S. Y., Sim, S. & Choi, H. G. Physical Activity, Study Sitting Time, Leisure Sitting Time, and Sleep Time Are Differently Associated With Obesity in Korean Adolescents: A Population-Based Study. Medicine 94, e1965 (2015).
Li, S. et al. Bed- and room-sharing in Chinese school-aged children: prevalence and association with sleep behaviors. Sleep Med 9, 555–563 (2008).
Media, C.O.C.A. Media and Young Minds. Pediatrics 138 (2016).
Acknowledgements
The study was supported by The fourth round of Three-Year Public Health Action Plan (2015–2017) (GWIV-36); Chinese National Natural Science Foundation (81602870, 81422040); Shanghai Municipal Education Commission (D1502); Ministry of Education New Century Excellent Talents (NCET-13–0362),Shanghai Science and Technology Commission (14441904004).
Author information
Authors and Affiliations
Contributions
Yunting Zhang designed the survey protocol, supervised data collection process, and drafted the initial manuscript; Donglan Zhang wrote the statistical analysis plan, analyzed the data, and drafted the initial manuscript for the method and result part; Xinyue Li analyzed data for the optimization calculation, and wrote the related part of the manuscript; Patrick Ip and Frederick Ho designed the survey protocol in major measurement tools and revised manuscript; Yanrui Jiang and Wanqi Sun took the leading role in implementing the onsite survey; Qi Zhu supervised survey data entry and created survey dataset; Weiming Zhu designed the sampling protocol of the survey and calculated sampling weight; Jun Zhang and Xiaoming Shen conceptualized, designed the study and revised the manuscript; Hongyu Zhao supervised the statistical analysis process and revised the manuscript; Guanghai Wang revised the manuscript; Fan Jiang obtained funding, initiated and supervised the survey, conceptualized the design of this study and revised the final version of the manuscript; All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Y., Zhang, D., Li, X. et al. Daily Time-Use Patterns and Obesity and Mental Health among Primary School Students in Shanghai: A Population-Based Cross-Sectional Study. Sci Rep 7, 16200 (2017). https://doi.org/10.1038/s41598-017-15102-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-15102-4
This article is cited by
-
Children’s Daily Activity Patterns and the Influence of Multilevel Ecological Factors
Child & Youth Care Forum (2024)
-
Children’s Daily Activities and Well-being during the COVID-19 Lockdown: Associations with Child and Family Characteristics
Current Psychology (2024)
-
The impact of school life and family involvement on Western China junior high school students’ wellbeing at multidimensional levels
Archives of Public Health (2022)
-
School-related sedentary behaviours and indicators of health and well-being among children and youth: a systematic review
International Journal of Behavioral Nutrition and Physical Activity (2022)
-
Associations between socioprovincial factors and self-reported mental disorders among students from grade 4 to 8 in rural China
Archives of Public Health (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.