Abstract
Acute primary angle closure glaucoma (APACG) is an ophthalmic emergency that may lead to irreversible blindness. Although efforts were made to control intraocular pressure, disease progression still existed. Anterior segment optical coherence tomography (AS OCT) may provide a new insight into mechanism of APACG. In order to seek out associated factors by AS OCT, We compared anterior segment parameters between 74 APACG and 48 normal eyes. Analysis of variance, principle component analysis and logistic regression were used. APACG group had more women (75.7% vs 47.9%, p = 0.002), smaller anterior chamber (anterior chamber depth, ACD; anterior chamber area, ACA; all p = 0.001), narrower angle (AOD500, AOD750, angle opening distance at 500um and 750um; TISA500, TISA750, trabecular-iris space area at 500um and 750um; ARA500, ARA750, angle recess area at 500um and 750um; all p < 0.001), thinner iris (iris thickness at 750um, IT750; maximum of iris thickness, ITMAX; all p < 0.001), larger iris area (IA, p < 0.001) and lens vault (LV, p = 0.005). Principle component extracted were AOD500, AOD750, TISA500, TISA750, ARA500, ARA750, IA, PD (pupillary diameter), ACD, ACA and IT750. After adjusting for confounding factors, AOD750 (b = 12.40 ± 2.56, p < 0.001), IT750 (b = 10.50 ± 3.45, p = 0.002) and IA (b = −1.56 ± 0.77, p = 0.044) were significantly associated with occurrence of APACG.
Similar content being viewed by others
Introduction
APACG is characterized by a suddenly increased intraocular pressure (IOP) caused by acute angle closure, If not treated urgently and effectively, it may lead to permanent vision loss. Asian people, female sex, narrow periphery angle, thick lens, anterior lens location and short axial length were known risk factors for APACG1. However, even with treatments to eliminate pupillary block, to widen angle or to reduce angle synechia, there remained a significant number of patients requiring medical treatment or secondary operation2.
A previous study in White Caucasian individuals found that in a period of 27 ± 14 months, 15% of APACG eyes developed to chronic or late stages, 6% were blinded, and 10% were visually impairment3. Another study of APACG in Hong Kong Chinese indicated that at 4 years after attack, 50% had abnormal IOP, 31% had non-improved vision and 11% were blinded4. It is imperative to take a new insight into mechanism of APACG, and advance of AS OCT in recent years provides an opportunity to expand our knowledge about APACG.
Moghimi et al.5 reported that 37.5% of acute angle closure eyes had pupillary block, 50% of them had exaggerated LV, in comparison with fellow eyes and primary angle closure suspect, APACG eyes had the shallowest ACD, least iris curvature and greatest LV. Guzman et al.6 noted that LV, TISA750 and IT750 were major determinants of APACG. Other studies showed that AS OCT parameters changed differently in normal and angle closure eyes: angle became wider after pharmacological mydriasis in normal individuals7, less loss of IA with pupil dilation was verified in APACG, angle closure and primary angle suspect8,9,10, lens vault loss and anterior chamber dimension loss remained smaller in angle closure eyes8.
Although several anatomical and dynamic factors of APACG were newly identified by AS OCT, exact parameters that lead to APACG were still uncertain. Mid-dilated pupil was one of the most important feature of APACG11, and narrower angle width was the only parameter identified for a significant IOP increase after pupil dilation12. This was different from normal individuals, in which angle width widened and 68.9% of IOP decreased in pupil dilated situation7,13. Discrepancy between APACG and normal individual in dilated condition hinted that structural or re-distributional difference of anterior segment may exist. While most studies about APACG used fellow eyes of APACG, primary angle closure suspect or primary angle closure as controls, advantages of using normal individuals were as follows: (1) comparison between angle closure and normal open angles may hint new information about angle closure mechanism8,14,15; (2) normal eyes can provide a normal reference to both APACG and fellow eyes and screened important parameters associated with APACG16,17,18; (3) fellow eye or primary angle suspect had a risk of inducing high intro-ocular pressure in pupil dilated condition, the risk in normal people was relative low, so normal controls were more frequently used in dynamics of anterior segment19,20. Therefore, the purpose of this study was to compare AS OCT parameters between APACG and normal dilated eyes and identify associated factors of APACG in Chinese people.
Methods
This prospective study was approved by the Ethnics Committee of Joint Shantou International Eye Center of Shantou University and the Chinese University of Hong Kong. The study was conducted in accordance with the principles of the Declaration of Helsinki and the Good Clinical Practice Guidelines. We included 74 APACG eyes and 48 normal eyes between July 2015 and March 2016 at the Joint Shantou International Eye Center of Shantou University and the Chinese University of Hong Kong. Informed consent was obtained from all participants. APACG was defined as21: (1) at least two of the symptoms-ocular pain or headache, nausea and/or vomiting; (2) IOP at least 30 mmHg; (3) at least three of the following signs: Conjunctival injection, corneal epithelial edema, fixed mild-dilated pupil, closed/narrow angle, and shallow anterior chamber. Inclusion of normal controls were based on: (1) no history of glaucoma or ocular surgery that may influence anterior segment construction; (2) IOP < 21 mmHg without medication; (3) open angle on gonioscopy; (4) absence of glaucomatous optic nerve damage or visual field damage. After attack, all APACG eyes accepted anti-glaucoma drugs, which included beta-blockers, alpha-2 angonists, topical/systemic carbonic anhydrase inhibitors and miotics. If IOP was higher than 40 mmHg, 250 ml of minnitol was intravenously given. ASOCT images were captured thereafter. To mimic dilated pupil in APACG, pupils were dilated by 0.5% tropic-amide in normal controls before ASOCT images were captured (Fig. 1). Uncooperative individuals or individuals with unclear corneal were excluded. Data of age, sex, laterality and AS OCT measurements were collected in both groups.
All ASOCT (Visante; Carl Zeiss Meditec, Dublin, CA) examinations were done by a single operator, masked to the results of clinical findings. Scans were taken along the horizontal axis using the enhanced anterior segment single protocol in a room without windows, with door closed and the only lighting with the AS OCT screen (<1 lux)5,22. After capturing several images, the one with the best quality was chosen for analysis. Images were processed using customized software, the Anterior Segment Analysis Program (ASAP; National University Hospital, Singapore)8 by a single experienced observer who was masked to clinical data. The only observer input was to determine the location of the scleral spurs. The algorithm then automatically calculated the anterior segment parameters23: AOD500, AOD750, TISA500, TISA750, ARA500, ARA750, IT500, IT 750, ITMAX, IA, PD, ACD, ACW, ACA and LV.
ANOVA and Student’s t-test were used for analysis of continuous variables. Chi-square testing was used for analysis of categorical variables. Principle component analysis was applied to mitigate multicollinearity among anterior segment parameters and identify primary predictors24. Binary logistic regression with forward method was used to detect the associated factors for APACG. The level of significance was defined as p-value less than 0.05. All the statistical analyses were performed with using SPSS software version 19.0 (SPSS Inc, Chicago, IL).
Results
The characteristics of patients in two groups were listed in Table 1. Mean age in APACG (n = 74) and normal group (n = 48) was not statistically different (64.15 ± 7.23 years vs 66.77 ± 11.92 years, p = 0.175). There were more women in APACG group (75.7% vs 47.9%, p = 0.002). Laterality between the two groups was not statistically significant (p = 0.098).
Table 2 revealed that nasal and temporal parameters were not statistically different in both normal and APACG group (all p > 0.05). We used temporal data in both groups as representatives in logistic regression. Except for ACW and IT500, all other AS OCT parameters were statistically different between normal and APACG group (all p < 0.05) (Table 3).
Linear regression indicated significant multicollinearity among AS OCT parameters, which was judged by the threshold of VIF25 (variance of inflation factors) ≧ 10 (Table 4). Principle component analysis with varimax rotation was used to eliminate multicollinearity and extract predominant variables. Principle component (PC) with eigenvalue ≧ 1 was considered as statistically significant26. The first four principle components accounted for 79.24% of total variance. PC1 accounted for 48.28% of total variance, and loaded heavily on angle parameters (AOD500, AOD750, TISA500, TISA750, ARA500, ARA750). PC2 accounted for 14.47% of total variance, which indicated the importance of iris area and pupil diameter. PC3 loaded heavily on anterior chamber parameters (ACD, ACW, ACA), explaining 8.90% of total variance. PC4 was contributed by iris thickness (IT500, IT750), and accounted for 7.58% of total variance (Tables 5 and 6).
ACW and IT500 were not statistically different between APACG and normal group, so we included Sex, AOD500, AOD750, TISA500, TISA750/ARA500/ARA750/ACD (one at a time to avoid collinearity), IA, PD, ACA and IT750 in Logistic regression analysis, results revealed that after adjusting for sex, AOD500, TISA500, TISA750, ARA500, ARA750, PD, ACD and ACA, AOD750, IT750 and IA were significantly associated with occurrence of APACG (Table 7).
Discussion
Known risk factors of APACG has discovered by A-ultrasound, gonioscopy and ultrasound bio-microscopy for a long time. Shallow anterior chamber, narrow peripheral angle, thick lens, anterior lens position and short axial length were popular reported ones1. Although traditional tools helped us to understand basic pathogenesis of APACG, limitations of contact, dis-automated, subjective, time-consuming, un-quantitative were obvious. AS OCT became popular recently for its advantage of sitting positioned, non-contact, fast, semi-automated, objective, high-resolutional, quantitative, high repeatability and reproducibility27.
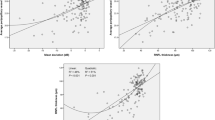
In this study, we found that all AS OCT parameters in APACG group were smaller than normal group except for IA and LV. This was similar to results reported by others. Seager et al.8 confirmed that IA was significantly larger in angle closure group compared with normal and open angle glaucoma group, and less loss of IA on dilation may contribute to AAC attack. Wang et al.28 reported that larger IA was significantly associated with narrow angles. Previous studies suggested that greater LV was the prominent feature of APAC affected eyes compared with fellow eyes29, primary angle closure suspect5, primary angel closure or primary angle closure glaucoma6. We guess that zonular laxity, forward movement of lens and iris pushed by posterior chamber pressure, choroidal volume expansion may be the reason for greater LV. Larger LV led to smaller ACD, IA may had an effect on narrower angle, and both of which explained a smaller ACA. This was partly confirmed by our study, data showed that in our study, ACD was negatively correlated with LV (R2 = −0.828, P < 0.001), IA was negatively correlated with AOD750 (R2 = −0.284, P = 0.002) and TISA750 (R2 = −0.18, P = 0.047), correlation between IA and other AS OCT parameters was not statistically significant (all P > 0.05). Furthermore, there was another interesting find-out, IA was negatively correlated with PD (R2 = −0.286, P = 0.001). So we speculated that larger IA in APACG led to a narrower angle. According to report by Nongpiur30, IA in our study was only medium, this means that smaller or larger IA was relative to its contrast, and a threshold associated with occurrence of APAC may exist. This assumption needs confirmation by others in the future.
However, in Logistic regression analysis, LV was not an independent risk factor for APACG. The first parameter included in forward regression was AOD750. This was also confirmed by other reports. Narayanaswamy et al.31 assessed the diagnostic performance of angle parameters in 1465 participants, they confirmed that AOD750 was the most significant angle measurement for identifying narrow angles in gradable AS-OCT images: areas under the receiver operating characteristic curves were highest for AOD750 in the nasal (0.90, 95% confidence interval, 0.89–0.92) and temporal (0.90, 95% confidence interval, 0.89–0.92). Nongpiur et al.32 identified the association between baseline ASOCT parameters and the development of gonioscopic angle closure, findings suggested that smaller AOD750 and larger LV explained 38% of gonioscopic angle closure, for every 0.1 mm decrease in AOD750, the odds ratio of developing gonioscopic angle closure was 3.27 (95% confidence interval, 1.87–5.69). Besides this, several studies have used AOD750 as an index to assess treatment outcomes of APACG33,34. The importance of AOD750 in assessment of angle width was also verified by our study: AOD750 was positively correlated with most of angle parameters (AOD500, R2 = 0.784, P < 0.001; TISA500, R2 = 0.674, P < 0.001; TISA750, R2 = 0.903, P < 0.001; ARA500, R2 = 0.616, P < 0.001; ARA750, R2 = 0.865, P < 0.001; ACW, R2 = 0.282, P = 0.002; ACD, R2 = 0.474, P < 0.001; ACA, R2 = 0.509, P < 0.001), and negatively correlated with LV (R2 = −0.356, P < 0.001) and IA (R2 = −0.284, P = 0.002).
The second parameter in logistic regression was IT750. Iris and its dynamics was a newly reported parameter in recent studies. Lee and his colleagues observed narrow angles in different ethnics, results hinted that IT750 was both a significant predictor of AOD750 in Whites and Africans and a predictor of TISA750 in Whites22. Atalay reported that IT750 was predictive of AOD750 in both APACG affected and fellow eyes35. Effect of IT750 on anterior segment was not clear, it made sense that mild-dilated pupil in APACG attack led to thicker peripheral IT and thus narrower angle. This was proved by previous studies. Guzman identified risk factors for APACG, comparison showed that thicker IT750 was a major determinant of APACG6. Other reports also pointed out that thinner IT750 was associated with greater increase in angle width after laser peripheral iridotomy36. These all indicated that thicker IT750 was detrimental to APACG. However, it cannot be verified by our study. IT750 in our study was thinner than normal controls and previous reported APAC eyes. Although IT750 was positively correlated with AOD750 (R2 = 0.224, p = 0.013), the correlation between IT750 and other AS OCT parameters was not statistically significant (all p > 0.05).
The third parameter in logistic regression was IA. It was not frequently reported in studies of APACG. Sng and colleagues described ASOCT parameters in APACG and fellow eyes, they found that IA was smaller in APACG eyes, but it was not an dependent risk factor associated with APAC attack37. Nevertheless, IA was verified as a factor associated with occludable angle in Chinese38, it was one of six variables that explained variability of TISA750 and AOD75039, and it was negatively correlated with change of AOD750 after laser peripheral iridotomy40.
We seeked out three associated factors for APACG by ASOCT, but there were still limitations in this study. Firstly, the sample size was not big enough. For logistic regression, the more the variables, the more the sample size. In our study, the variables were 16, so sample size would at least be 80 in both APACG and normal group. Secondly, gender was not balanced between APACG and control group. Although the ratio of female in APACG group (75.4%) was similar to other studies (Male:female = 1:3.3, female ratio, 76%)3,4, the female:male ratio in control group was smaller (about 1:1), and data in our study showed that some of angle parameters was statistically different between men and women (ARA500, P = 0.035, IT500, P = 0.044 in APACG group; AOD500, P = 0.043, AOD750, P = 0.039 in control group), this may induce bias, because AOD750 entered into logistic regression. Thirdly, ASOCT images were captured after treatment, so it would not be the real situation of APACG, especially if mitotic drug was used that can affect angle parameters. Nevertheless, APACG was an ophthalmic emergency, images before treatment were not practical and unethical. Pretreatment anterior segment imaging during acute primary angle closure was only reported by two studies34,37. AOD750 was smaller than ours (0.002 and 0.002 mm VS 0.05 ± 0.09 mm), IT750 (0.34 and 0.33 mm VS 0.34 ± 0.10 mm) and IA (1.55 and 1.43 mm2 VS 1.55 ± 0.38 mm2) was similar to ours. Difference may due to sample diversity or drug-induced bias. According to results reported by Sng37, before and after medical treatment (same protocol to ours), difference in AOD750, IT750 and IA was 0.02 mm (−0.03 to 0.06), −0.01 mm (−0.05 to 0.02) and 0.27 mm2 (0.18 to 0.37) respectively. Therefore, bias induced by anti-glaucoma drugs was 3.03% (0.01/0.33) for IT750 and 18.89% (0.27/1.43) for IA in their study. The bias for AOD750 can not be calculated (0.02/0). Besides, not all patients subsided after treatment, so images may differ between severe and subside patients, further sub-groups should be divided. Fourthly, Pupil were dilated in normal group, the anterior segment especially the angle parameters may not represent the normal controls. The potential bias has been observed by previous studies. Zhang et al.41 analyzed anterior segment changes induced by tropic-amide in normal Chinese, outcome indicated that AOD500 changed from baseline 0.322 mm to 0.386 mm (19.88% of baseline), IA changed from 2.70 mm2 to 1.77 mm2 (−34.4% of baseline). Guo et al 42 compared anterior segment changes before and after mydriasis in normal people, results showed that ∆AOD500, ∆IT750, ∆IA was −0.074 ± 0.111 mm (P = 0.009), −0.09 ± 0.034 mm (P < 0.001), and 0.523 ± 0.162 mm (P < 0.001) respectively. An interesting point was that anterior chamber became wider after mydriasis in normal subjects43, which was very different from APACG eyes. This may indirectly verified that iris dynamics in open and angle eyes was different in conditions of pupil dilation, and loss of iris area was smaller in angle closure eyes: loss of IA per mm of PD increase was 0.145 mm2 in primary angle closure glaucoma, 0.161 mm2 in fellow eyes and 0.165 mm2 in normal controls44. According to previous results, the corrected IA of normal group in our study should be 1.67 mm2 (1.35 + 0.165*(5.89–3.96)) if we take pupil diameter into account. So the difference in pupil diameter between two groups may induce bias. Although pupil diameter has an effect on other AS OCT parameters: in our study, PD was positively correlated with angle width (AOD750, R2 = 0.271, P = 0.003; TISA750, R2 = 0.195, P = 0.031; ARA750, R2 = 0.182, P = 0.045; ACW, R2 = 0.246, P = 0.006; ACD, R2 = 0.46, P < 0.001; ACA, R2 = 0.553, P < 0.001), and negatively correlated with LV and IA (LV, R2 = −0.395, P < 0.001; IA, R2 = −0.286, P = 0.001), it did not enter into model in Logistic regression. Lastly, all images were captured at one time-point, dynamic changes of anterior segment were not observed. All of these deficiency should be overcame in further studies.
In conclusion, in this study, APACG eyes had smaller anterior anterior chamber and narrower angle but greater IA and LV than normal controls. Greater LV had an effect on smaller ACD, but effect of IA on angle parameter was controversial. AOD750, IT750 and IA were independent associated factors for APACG. Effect of AOD750 was easily understood and confirmed by other studies, IT750 was positively correlated with AOD750, and less loss of IA in pupil dilated situation may be detrimental to angle closure. Further studies with precise design and detailed accomplishment will be needed in the future.
References
Zhang, X. et al. Why does acute primary angle closure happen? Potential risk factors for acute primary angle closure. Survey of ophthalmology Apr 17 (2017).
Tan, A. M., Loon, S. C. & Chew, P. T. Outcomes following acute primary angle closure in an Asian population. Clinical & experimental ophthalmology 37, 467–472 (2009).
Andreatta, W., Elaroud, I., Nightingale, P. & Nessim, M. Long-term outcomes after acute primary angle closure in a White Caucasian population. BMC ophthalmology 15, 108 (2015).
Lee, J. W. et al. Primary acute angle closure: long-term clinical outcomes over a 10-year period in the Chinese population. International ophthalmology 34, 165–169 (2014).
Moghimi, S. et al. Acute angle closure: qualitative and quantitative evaluation of the anterior segment using anterior segment optical coherence tomography. Clinical & experimental ophthalmology 42, 615–622 (2014).
Guzman, C. P. et al. Anterior segment optical coherence tomography parameters in subtypes of primary angle closure. Investigative ophthalmology & visual science 54, 5281–5286 (2013).
Dastiridou, A. I. et al. Comparison of Physiologic versus Pharmacologic Mydriasis on Anterior Chamber Angle Measurements Using Spectral Domain Optical Coherence Tomography. Journal of ophthalmology 2015, 845643 (2015).
Seager, F. E., Jefferys, J. L. & Quigley, H. A. Comparison of dynamic changes in anterior ocular structures examined with anterior segment optical coherence tomography in a cohort of various origins. Investigative ophthalmology & visual science 55, 1672–1683 (2014).
Zhang, Y. et al. Quantitative analysis of iris changes following mydriasis in subjects with different mechanisms of angle closure. Investigative ophthalmology & visual science 56, 563–570 (2015).
Quigley, H. A. et al. Iris cross-sectional area decreases with pupil dilation and its dynamic behavior is a risk factor in angle closure. Journal of glaucoma 18, 173–179 (2009).
Khazaeni, B. & Khazaeni, L. In StatPearls (2017).
Lavanya, R. et al. Risk of acute angle closure and changes in intraocular pressure after pupillary dilation in Asian subjects with narrow angles. Ophthalmology 119, 474–480 (2012).
Qian, C. X., Duperre, J., Hassanaly, S. & Harissi-Dagher, M. Pre- versus post-dilation changes in intraocular pressure: their clinical significance. Canadian journal of ophthalmology. Journal canadien d’ophtalmologie 47, 448–452 (2012).
Nongpiur, M. E. et al. Lens vault, thickness, and position in Chinese subjects with angle closure. Ophthalmology 118, 474–479 (2011).
Wang, B. S. et al. Increased iris thickness and association with primary angle closure glaucoma. The British journal of ophthalmology 95, 46–50 (2011).
Wang, Z., Chung, C., Lin, J., Xu, J. & Huang, J. Quantitative Measurements of the Ciliary Body in Eyes With Acute Primary-Angle Closure. Investigative ophthalmology & visual science 57, 3299–3305 (2016).
Bian, J. J., Dai, W. J. & Liu, D. C. Morphological monitoring indexes in anterior segment with primary acute angle closure glaucoma. [Zhonghua yan ke za zhi] Chinese journal of ophthalmology 48, 502–506 (2012).
Zhang, H. T., Xu, L., Cao, W. F., Wang, Y. X. & Jonas, J. B. Anterior segment optical coherence tomography of acute primary angle closure. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie 248, 825–831 (2010).
Aptel, F., Chiquet, C., Beccat, S. & Denis, P. Biometric evaluation of anterior chamber changes after physiologic pupil dilation using Pentacam and anterior segment optical coherence tomography. Investigative ophthalmology & visual science 53, 4005–4010 (2012).
Aptel, F. & Denis, P. Optical coherence tomography quantitative analysis of iris volume changes after pharmacologic mydriasis. Ophthalmology 117, 3–10 (2010).
Moghimi, S., Chen, R., Hamzeh, N., Khatibi, N. & Lin, S. C. Qualitative evaluation of anterior segment in angle closure disease using anterior segment optical coherence tomography. Journal of current ophthalmology 28, 170–175 (2016).
Lee, R. Y., Chon, B. H., Lin, S. C., He, M. & Lin, S. C. Association of ocular conditions with narrow angles in different ethnicities. Am J Ophthalmol 160, 506–515 (2015).
Moghimi, S., Ramezani, F., He, M., Coleman, A. L. & Lin, S. C. Comparison of Anterior Segment-Optical Coherence Tomography Parameters in Phacomorphic Angle Closure and Acute Angle Closure Eyes. Investigative ophthalmology & visual science 56, 7611–7617 (2015).
Liu, J., Li, Q., Dong, J., Chen, J. & Gu, G. Multivariate modeling of aging in bottled lager beer by principal component analysis and multiple regression methods. J Agric Food Chem 56, 7106–7112 (2008).
Hossain, M. G., Saw, A., Alam, R., Ohtsuki, F. & Kamarul, T. Multiple regression analysis of anthropometric measurements influencing the cephalic index of male Japanese university students. Singapore medical journal 54, 516–520 (2013).
Almkvist, O., Bosnes, O., Bosnes, I. & Stordal, E. Selective impact of disease on short-term and long-term components of self-reported memory: a population-based HUNT study. BMJ open 7, e013586 (2017).
Maslin, J. S., Barkana, Y. & Dorairaj, S. K. Anterior segment imaging in glaucoma: An updated review. Indian J Ophthalmol 63, 630–640 (2015).
Wang, B. et al. Quantitative iris parameters and association with narrow angles. Ophthalmology 117, 11–17 (2010).
Lee, J. R., Sung, K. R. & Han, S. Comparison of anterior segment parameters between the acute primary angle closure eye and the fellow eye. Investigative ophthalmology & visual science 55, 3646–3650 (2014).
Nongpiur, M. E. et al. Anterior segment imaging-based subdivision of subjects with primary angle-closure glaucoma. Eye (Lond), (2016).
Narayanaswamy, A. et al. Diagnostic performance of anterior chamber angle measurements for detecting eyes with narrow angles: an anterior segment OCT study. Archives of ophthalmology 128, 1321–1327 (2010).
Nongpiur, M. E. et al. Association of Baseline Anterior Segment Parameters With the Development of Incident Gonioscopic Angle Closure. JAMA Ophthalmol 135, 252–258 (2017).
Moghimi, S. et al. Changes in Anterior Segment Morphology After Laser Peripheral Iridotomy in Acute Primary Angle Closure. Am J Ophthalmol 166, 133–140 (2016).
Sng, C. C. et al. Anterior segment morphology after acute primary angle closure treatment: a randomised study comparing iridoplasty and medical therapy. The British journal of ophthalmology 100, 542–548 (2016).
Atalay, E. et al. Biometric Factors Associated With Acute Primary Angle Closure: Comparison of the Affected and Fellow Eye. Investigative ophthalmology & visual science 57, 5320–5325 (2016).
Lee, R. Y. et al. Association between baseline iris thickness and prophylactic laser peripheral iridotomy outcomes in primary angle-closure suspects. Ophthalmology 121, 1194–1202 (2014).
Sng, C. C. et al. Pretreatment anterior segment imaging during acute primary angle closure: insights into angle closure mechanisms in the acute phase. Ophthalmology 121, 119–125 (2014).
Wang, Y. E., Li, Y., Wang, D., He, M. & Lin, S. Comparison of factors associated with occludable angle between american Caucasians and ethnic Chinese. Investigative ophthalmology & visual science 54, 7717–7723 (2013).
Foo, L. L. et al. Determinants of angle width in Chinese Singaporeans. Ophthalmology 119, 278–282 (2012).
Huang, G. et al. Anatomic predictors for anterior chamber angle opening after laser peripheral iridotomy in narrow angle eyes. Current eye research 37, 575–582 (2012).
Zhang, Y. et al. Quantitative analysis of iris changes after physiologic and pharmacologic mydriasis in a rural Chinese population. Investigative ophthalmology & visual science 55, 4405–4412 (2014).
Guo, J. M., Li, M., Xu, X. L., Zhang, H. & Wang, J. M. Anterior segment changes after pharmacologic mydriasis using Pentacam and optical coherence tomography in angle closure suspects. International journal of ophthalmology 8, 980–984 (2015).
Kim, J. M. et al. Changes in intraocular pressure after pharmacologic pupil dilation. BMC ophthalmology 12, 53 (2012).
Lin, J. et al. Dynamic changes of anterior segment in patients with different stages of primary angle-closure in both eyes and normal subjects. PloS one 12, e0177769 (2017).
Acknowledgements
This study was supported by the National Natural Science Foundation of China (81371010), Medical Scientific Research Project of Guangdong Province, China (A2015355), Foundation for Distinguished Young Talents in Higher Education of Guangdong, China (2014KQNCX075), and Clinical Research Funds of Shantou University Medical College.
Author information
Authors and Affiliations
Contributions
M.Z. and C.Z. designed the study. C.H. and G.W. collected patients’ information. X.L. captured AS OCT images. D.M. and W.Z. analyzed data. L.L. wrote the main manuscript text. G.W. and C.Z. revised the manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, L., Liu, X., Huang, C. et al. Associated factors of acute primary angle closure glaucoma in a sub-group of Chinese people: comparison between attack eyes and normal controls. Sci Rep 7, 14885 (2017). https://doi.org/10.1038/s41598-017-14685-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-14685-2
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.