Abstract
We aimed to determine the prevalence and possible ethnic variations in strabismus and amblyopia among multiethnic school-aged children in rural China. A total of 9,263 children (4,347 Han, 3,352 Yi, 799 Dai and 765 Bai) aged 6 to 14 years were analyzed. Comprehensive eye examinations including monocular distance visual acuity, anterior segment examination, autorefraction, cover testing and ocular motility were conducted. Manifested strabismus was detected in 3.53% of the overall population. The prevalence of strabismus was 3.29% in Han, 4.12% in Yi, 2.25% in Dai, and 3.66% in Bai ethnic groups with marginally inter-ethnic differences (P = 0.046). There was an increasing trend in the prevalence of strabismus with increasing age (P < 0.001). Amblyopia affected 132 children (1.43%) overall, with no statistical differences in gender and age. The prevalence of amblyopia was highest in Dai ethnic group (2.00%) and lowest in ethnic Yi ethnic group (1.04%) with no significant difference being detected (P = 0.062). Refractive error and strabismus were the two major factors associated with amblyopia. No significant ethnic differences in strabismus and amblyopia among Chinese ethnic minorities were observed. Refractive error and strabismus were the major causes for amblyopia in rural Chinese children.
Similar content being viewed by others
Introduction
Amblyopia and strabismus are two major childhood-onset ocular disorders exerting persistent negative effects on visual and binocular function development. Strabismus manifests as a condition in which the eyes are improperly aligned. The condition is identified as a common cause of amblyopia in children, presenting significant psychosocial and psychosocial consequences followed by adverse effects on binocularity, stereopsis, and depth of perception1,2. Amblyopia refers to unilateral or bilateral reduction in best corrected visual acuity (BCVA) not directly attributable to structural abnormality of the eye or posterior visual pathways. Individuals with childhood-onset unilateral amblyopia have a greater lifetime risk of eventual bilateral visual impairment and age-related macular degeneration3. Nevertheless, amblyopia is potentially reversible, if properly treated. Earlier reports have indicated that the treatment of amblyopia is ineffective after 8 years old; yet, recent amblyopia treatment studies have shown that visual acuity can be improved in older children4.
Epidemiologic studies on strabismus and amblyopia in preschool and school-aged populations have been widely carried out in recent decades including the Multi-Ethnic Pediatric Eye Disease Study (MEPEDS)5,6; the Baltimore Pediatric Eye Disease Study7; the Strabismus, Amblyopia, and Refractive Error in Singaporean Children Study8; and the Vision In Preschoolers Study9,10. In these studies, racial/ethnic differences were observed including higher exotropia versus esotropia ratios as well as lower strabismus and amblyopia prevalence rates in the Asians compared with other ethnic groups.
China is one of the largest developing countries throughout the world with a multiethnic population including Han ethnicity and other 55 ethnic minorities. Han ethnicity is the major ethnic group which accounts for about 90% of the entire national population. There are few data addressing the epidemiology of strabismus and amblyopia among Chinese children of ethnic minorities. Yunnan Province is located on the border of southwestern China and has the largest number of ethnic minorities among all provinces in China, which provides us with a unique opportunity to look into the possible ethnic differences among various Chinese ethnic minorities. In this study, we compared the prevalence and subtypes of strabismus and amblyopia in school-based samples of different ethnic groups including Han, Yi, Dai and Bai Chinese children and adolescents aged 6 to 14 years in rural communities in Yunnan Province.
Methods
Study Population
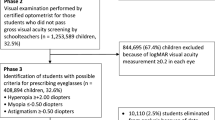
The Yunnan Minority Children Eye Study was a series of school-based studies conducted from 2014 to 2015 in Yangbi and Mangshi in Yunnan Province. The current study was conducted to compare the variations in the prevalence of strabismus and amblyopia among different ethnic groups aged 6 to 14 years in Yangbi and Mangshi located within Yunnan. All 13,738 students from 55 schools located in the study sites were invited to participate in the study, among whom, 10,244 had completed eye examinations and provided parents’ consent, with questionnaire data provided (74.6% response rate). There were no significant differences in terms of age (P = 0.23) and gender (P = 0.55) between responders and non-responders. The study sample included 4,347 Han (42.4%), 3352 Yi (32.7%), 799 Dai (7.8%), 765 Bai (7.5%) and 981 other ethnic minorities (9.6%), with each ethnic group having similar proportions of boys and girls (Table 1). Participants of different ethnicities resided together in the same communities. In the current analysis of the prevalence across ethnic groups, we only included the four major ethnic groups including Han, Yi, Dai and Bai. Some ethnic group such as Jingpo, Hui, Achang, Lisu and other unknown minorities was excluded from the analysis because of the complexity of ethnic composition and inadequate number in each ethnic group. Finally, 9,263 study participants were included in the current analysis. The subjects aged from 6 to 14 years, with a mean age of 9.55 ± 1.93 years, while sex was distributed equally in each of the four ethnic group (Table 1). Ethnicity of the offspring was identified according to the father’s ethnicity.
Written informed consent was obtained from at least one parent after the nature of the study was explained and verbal consent was obtained from each child before examination. All procedures were reviewed and approved by the Kunming Medical University institutional ethical review board in accordance with the Declaration of Helsinki. The study methods were carried out in accordance with the approved guidelines.
Questionnaire and Eye Examinations
Questionnaires were distributed to all enrolled children who were required to fill out the questionnaire under their parents’ supervision. Basic demographic information as well as medical history of amblyopia, strabismus, and any prior ophthalmic treatment was included in the questionnaire.
A comprehensive ophthalmologic examination including monocular distance visual acuity (VA), anterior segment, ocular alignment, and non-cycloplegic autorefraction was performed by two optometrists and two ophthalmologists who were trained and certified using standardized study protocols, as previously described in MEPEDS11. Post-cycloplegic refraction and fundus examination were also performed. The same study ophthalmologists (HZ and ZF) performed the ophthalmologic examinations in all schools.
Ocular alignment was assessed using the Hirschberg light reflex test, the unilateral cover (cover–uncover) test, and the alternate cover test. The cover test was conducted at both distances, namely, distant (6 m) and near (33 cm), by using fixation targets. Visual acuity with and without optical correction was examined if glasses were worn. Ocular movements (versions and ductions) were assessed in nine diagnostic positions of gaze with the head in a stationary position. If strabismus was suspected, a prism cover test was performed to detect the magnitude of the deviation.
Distance VA was measured with a logarithm of the minimum angle of resolution (LogMAR) visual acuity chart (Precision Vision, La Salle, IL, USA) at a distance of 4 m, with or without spectacles. For children with initial VA less than 20/25 in either eye (or 2-line interocular difference), cycloplegic refraction was performed. Subjective refraction was then performed to obtain BCVA. If glasses were worn, testing was performed with and without correction.
The refraction status of all participants was measured using an auto refractometer (NIDEK ARK-510A, NIDEK Corporation, Japan) under non-cycloplegic conditions. The average of three consecutive readings of sphero-cylindrical autorefraction was determined. Spherical refraction (SE) was calculated as the sum of the spherical and half of the cylindrical power. Any child with abnormal ocular alignment, ocular movement, or distance VA was further evaluated by post-cycloplegic refraction. For cycloplegic refraction, one drop of topical 1.0% cyclopentolate was administered to each eye twice with a 5-minute interval. Fifteen minutes later, a third drop was administered if the pupil size was less than 6 mm or if the pupillary light reflex was still present.
Definitions
Strabismus was defined as any tropia presented at distant or near fixations with or without spectacles. Constant heterotropia was considered as constant tropia at both near and distant fixation; otherwise, it was considered intermittent. Strabismus was defined as constant or intermittent heterotropia of any magnitude at distant or near fixation. Strabismus was classified by the primary direction (esotropia, exotropia, vertical) of the tropia. Microstrabimus is defined as a deviation of fewer than 10 prism diopters, in addition to binocular vision.
Unilateral amblyopia was defined if the participant had a BCVA ≤ 20/32 in the worse eye and a 2-line interocular difference or more in BCVA, without any underlying structural abnormality of the visual pathway and presenting at least one of the following risk factors in the affected eye: past or present strabismus; previous strabismus surgery; anisometropia consistent with the worse eye such as spherical equivalent (SE) difference of ≥3.00 diopters (D) in myopia, ≥1.00 D in hyperopia, or ≥1.50 D in astigmatism; and evidence of past or present visual axis obstruction (e.g., congenital cataract, intraocular lens, aphakia, corneal opacity, ptosis, or eyelid hemangioma). Bilateral amblyopia was defined as a condition of bilateral subnormal BCVA < 20/40, presenting amblyopia factors including bilateral high ametropia (myopia ≥ 6.00 D, hyperopia ≥ 4.00 D, or astigmatism ≥ 2.50 D) and evidence of past or present visual axis obstruction (see above). Children who met the unilateral and bilateral amblyopia criteria were classified as unilateral amblyopia, similar to that used in MEPDES5,6.
Statistical Analysis
Statistical analyses were performed using a commercially available statistical software package (SPSS for Windows, version 19.0, IBM–SPSS, China). The prevalence rates of strabismus and amblyopia were calculated by age and gender for each of the four ethnic groups. The chi-square test incorporating sampling weights with a 0.05 significance level was used to compare the prevalence rates for the four ethnic groups. Odds ratios (ORs) and 95% confidence intervals (CIs) were also presented.
Results
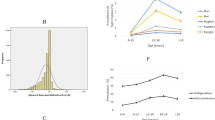
Table 2 shows the prevalence of strabismus by age and gender. On the basis of the comprehensive eye examinations of 9,263 subjects, manifest strabismus was detected in 327 children [3.53%, 95% Confidence Interval (CI), 3.15–3.91%], including 143 Han, 138 Yi, and 18 Dai and 28 Bai children, with corresponding prevalence rates of 3.29% (95% CI, 2.76–3.82%), 4.12% (95% CI, 3.44–4.79%), 2.25% (95% CI, 1.22–3.28%), and 3.66% (95% CI, 2.33–4.99%), respectively. Marginally significant ethnic differences in the prevalence of strabismus were indicated, with a P value of 0.046 (Table 2). The overall sample was divided into four three groups by age (6 to 8 years, 9 to 11 years, and 12 to 14 years). Higher prevalence of strabismus was found in older age groups, ranging from 2.47% to 4.96% (P < 0.001). Gender was not associated with the prevalence of strabismus (P = 0.49).
Table 3 demonstrates the distribution of strabismus subtypes. Among the 327 children with strabismus, 3 reported a history of strabismus surgery, 2 presented with normal ocular position, and 1 had residual exotropia. Among strabismic children in each ethnic group, the number of children with exotropia remarkably exceeded the number of those with esotropia, with exotropia versus esotropia ratios of 10.5:1 (115:11) in ethnic Han, 10.3:1 (113:11) in ethnic Yi, 7.5:1 (15:2) in ethnic Dai and 7:1 (21:4) in ethnic Bai.
Among the 9,263 children, 72 Han (1.66%), 35 Yi (1.04%), 16 Dai (2.00%), and 9 (1.18%) Bai children were found to be affected by amblyopia (Table 2). The overall prevalence of amblyopia in this study was 1.43% (95% CI, 1.18–1.67%). No differences were observed in the prevalence of amblyopia in gender (P = 0.192) or age (P = 0.704). Bilateral amblyopia was present in 8 (0.09%) children, whereas unilateral amblyopia was observed in 124 (1.34%) children.
The distribution of the types of amblyopia by ethnic groups is presented in Table 4. Refractive error was identified as the most frequent cause of unilateral amblyopia and was present in 103 cases (83.06%). Combined strabismic/anisometropic ranked the second and was observed in 16 cases (12.90%), followed by strabismus in 5 cases (4.03%). Therefore, 119 cases of all amblyopia cases were attributable to abnormal refractive error. Only 21 cases were attributable, even in part, to strabismus. On the basis of questionnaire information, 5 children were previously diagnosed with and treated for amblyopia, 2 of whom remained amblyopic upon our examination.
Discussion
This study provides new school-based data on the prevalence and ethnic variations in strabismus and amblyopia in multiethnic school-aged children in rural China. Overall, the ethnic differences in strabismus and amblyopia in Chinese ethnic minorities was not pronounced. Intermittent exotropia was the predominant form of strabismus in each ethnic group, whereas the extropia versus estropia ratios were high.
Our study filled the gap of knowledge on the epidemiology of major pediatric eye disorders in rural China. A detailed comparison of prevalence estimates between our study and previous ones is summarized in Table 5. The overall prevalence of strabismus in our study was higher compared with that in Turkey (2.4%; 6 to 14 years)12, Japan (1.3%; 6 to 12 years)13 and the RESC studies (5 to 15 years) which reported the prevalence of strabismus of 1.9% in southern China14, 1.3% in South Africa15, 1.9% in India16, 0.53% in New Delhi17, 2.3% in Chile18, and 2.1% in Nepal19. When age was restricted to the same range, the prevalence of strabismus in children aged 7 years was similar with that in the United Kingdom (2.68% versus 2.3%)20. Meanwhile, the prevalence in children aged 12 years to 13 years (4.93%) was similar with that in the Anyang Childhood Eye Study (5.0%)21 but higher than that reported in the Mexican (2.3%)22 and Sydney (2.8%)23. Considering the variations in methodological issues such as different age ranges of the study participants and definitions of diseases, whether Chinese children had a higher prevalence of strabismus remains unclear.
Exotropia is markedly more prevalent than esotropia in Chinese school-aged children. This finding is inconsistent with previous studies in white populations, with esotropia being much more prevalent in the Whites, though the age ranges of the participants were different5,6,7. Lower hyperopia rates in Asian populations may be partially responsible24. Interestingly, recent studies from both Asia13,25 and the West5,6,7 reported similar increases in the prevalence of exotropia. The increase trend in exotropia versus esotropia ratio could be attributable to the declining occurrence of accommodative esotropia as these populations became less hyperopic. Further studies are warranted to determine the reason for this tendency with genetic and ethnic differences being taken into consideration.
With regard to amblyopia, the prevalence in our multiethnic Chinese school children was 1.43%. Compared with school-aged children in other studies (Table 5), the prevalence was higher than the rates from the Refractive Error Studies in Children (RESC) except 2.3% in Chile and 1.43% in Nepal for 2-line intraocular difference in BCVA absent in the amblyopic diagnostic criteria, which would lead to an underestimation of the prevalence by approximately half12,13,14,15,16,17,18,19. Following the RESC, only 86 children (0.93%) in our study in accordance with the diagnostic criteria of amblyopia, which was similar with the results from Shunyi (0.97%)24 and Guangzhou (0.87%)14.The rate of amblyopia was also higher than that found in the Shandong Children Eye Study, even though the rate 1.66% pertained only to ethnic Han children in our study26. When age was restricted to the same range, the rates found in our study were higher than those in other studies, including the Anyang Childhood Eye Study (1.44% versus 1.0%, 6 to 9 years)21 and the Sydney Myopia Study (1.52% versus 1.1% in 6 years; 1.26% versus 0.9% in 12 years)23,27. However, the prevalence was 1.40% lower than 2.5% in the Anyang Childhood Eye Study of children aged 12 years to 13 years28. The observed differences may be attributable to the variations in the definitions used in these studies. In addition, availability of vision screening programs early in life was not mentioned in some of these studies; thus, cases of amblyopia that were previously diagnosed and treated could have been discounted. In this study population, previous diagnosis and treatment of amblyopia were uncommon. Only a small number of children had undergone vision screening, with 5 of them having been previously diagnosed with amblyopia. Other children, especially those from rural regions, rarely had any form of vision screening. Therefore, this prevalence estimate reflected the natural frequency of pathology in the absence of effective surveillance and intervention, indicating the full magnitude of public health challenge. The relatively higher prevalence of amblyopia could be attributable to a lack of awareness of regular eye check-ups and the importance of using spectacles. No difference in the prevalence of amblyopia between genders was found, which was consistent with the results in previous studies. Our study found that the most common cause of amblyopia was refractive error and followed by strabismus, which was similar to the observation in the previous studies28,29,30. However, some studies identified strabismus as the main cause23,27.
The strengths of the study included a large and multiethnic study sample, which initially provided sufficient statistical power in detecting the potential ethnic differences of ocular diseases we are interested in. Our study also had limitations. The major limitation was that the study design was school-based rather than population-based. Although the school attendance rate in rural China has been rapidly increased in recent years, some children still could not attend schools as they are unable to afford the expenses. Thus, being unable to include these children in the study might have distorted the prevalence estimates. In addition, the diagnostic criterion for amblyopia in this study might have underestimated the prevalence, especially among children with older age.
In conclusion, no significant ethnic differences in strabismus and amblyopia among Chinese ethnic minorities were observed. Our study enriched the epidemiologic research of pediatric ophthalmology and may help ophthalmologists and optometrists to better understand the patterns of strabismus and amblyopia and potentially inform planning for school-based vision screening programs.
References
Jackson, S., Harrad, R. A., Morris, M. & Rumsey, N. The psychosocial benefits of corrective surgery for adults with strabismus. Br J Ophthalmol 90, 883–888, https://doi.org/10.1136/bjo.2005.089516 (2006).
Jackson, S., Morris, M. & Gleeson, K. The long-term psychosocial impact of corrective surgery for adults with strabismus. Br J Ophthalmol 97, 419–422, https://doi.org/10.1136/bjophthalmol-2012-302983 (2013).
van Leeuwen, R. et al. Risk of bilateral visual impairment in individuals with amblyopia: the Rotterdam study. Br J Ophthalmol 91, 1450–1451, https://doi.org/10.1136/bjo.2006.113670 (2007).
Pediatric Eye Disease Investigator, G. A prospective, pilot study of treatment of amblyopia in children 10 to <18 years old. Am J Ophthalmol 137, 581–583, https://doi.org/10.1016/j.ajo.2003.08.043 (2004).
Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months the multi-ethnic pediatric eye disease study. Ophthalmology 115, 1229–1236 e1221, https://doi.org/10.1016/j.ophtha.2007.08.001 (2008).
McKean-Cowdin, R. et al. Prevalence of amblyopia or strabismus in asian and non-Hispanic white preschool children: multi-ethnic pediatric eye disease study. Ophthalmology 120, 2117–2124, https://doi.org/10.1016/j.ophtha.2013.03.001 (2013).
Friedman, D. S. et al. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71 months the Baltimore Pediatric Eye Disease Study. Ophthalmology 116(2128–2134), e2121–2122, https://doi.org/10.1016/j.ophtha.2009.04.034 (2009).
Chia, A. et al. Prevalence of amblyopia and strabismus in young singaporean chinese children. Invest Ophthalmol Vis Sci 51, 3411–3417, https://doi.org/10.1167/iovs.09-4461 (2010).
Pascual, M. et al. Risk factors for amblyopia in the vision in preschoolers study. Ophthalmology 121, 622–629 e621, https://doi.org/10.1016/j.ophtha.2013.08.040 (2014).
Ying, G. S. et al. Prevalence of vision disorders by racial and ethnic group among children participating in head start. Ophthalmology 121, 630–636, https://doi.org/10.1016/j.ophtha.2013.09.036 (2014).
Varma, R. et al. The multi-ethnic pediatric eye disease study: design and methods. Ophthalmic Epidemiol 13, 253–262, https://doi.org/10.1080/09286580600719055 (2006).
Caca, I. et al. Amblyopia and refractive errors among school-aged children with low socioeconomic status in southeastern Turkey. J Pediatr Ophthalmol Strabismus 50, 37–43, https://doi.org/10.3928/01913913-20120804-02 (2013).
Matsuo, T. & Matsuo, C. The prevalence of strabismus and amblyopia in Japanese elementary school children. Ophthalmic Epidemiol 12, 31–36, https://doi.org/10.1080/09286580490907805 (2005).
He, M. et al. Refractive error and visual impairment in urban children in southern china. Invest Ophthalmol Vis Sci 45, 793–799 (2004).
Naidoo, K. S. et al. Refractive error and visual impairment in African children in South Africa. Invest Ophthalmol Vis Sci 44, 3764–3770 (2003).
Dandona, R. et al. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci 43, 615–622 (2002).
Murthy, G. V. et al. Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci 43, 623–631 (2002).
Maul, E., Barroso, S., Munoz, S. R., Sperduto, R. D. & Ellwein, L. B. Refractive Error Study in Children: results from La Florida, Chile. Am J Ophthalmol 129, 445–454, doi:S0002939499004547 (2000).
Pokharel, G. P., Negrel, A. D., Munoz, S. R. & Ellwein, L. B. Refractive Error Study in Children: results from Mechi Zone, Nepal. Am J Ophthalmol 129, 436–444, doi:S0002939499004535 (2000).
Williams, C. et al. Prevalence and risk factors for common vision problems in children: data from the ALSPAC study. Br J Ophthalmol 92, 959–964, https://doi.org/10.1136/bjo.2007.134700 (2008).
Fu, J. et al. Prevalence of amblyopia and strabismus in a population of 7th-grade junior high school students in Central China: the Anyang Childhood Eye Study (ACES). Ophthalmic Epidemiol 21, 197–203, https://doi.org/10.3109/09286586.2014.904371 (2014).
Ohlsson, J. et al. Visual acuity, amblyopia, and ocular pathology in 12- to 13-year-old children in Northern Mexico. J AAPOS 7, 47–53, https://doi.org/10.1067/mpa.2003.S1091853102420113 (2003).
Robaei, D., Kifley, A. & Mitchell, P. Factors associated with a previous diagnosis of strabismus in a population-based sample of 12-year-old Australian children. Am J Ophthalmol 142, 1085–1088, https://doi.org/10.1016/j.ajo.2006.06.053 (2006).
Zhao, J. et al. Refractive Error Study in Children: results from Shunyi District, China. Am J Ophthalmol 129, 427–435, doi:S0002939499004523 (2000).
Yu, C. B., Fan, D. S., Wong, V. W., Wong, C. Y. & Lam, D. S. Changing patterns of strabismus: a decade of experience in Hong Kong. Br J Ophthalmol 86, 854–856 (2002).
Wu, J. F. et al. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS One 8, e82763, https://doi.org/10.1371/journal.pone.0082763 (2013).
Robaei, D. et al. Visual acuity and the causes of visual loss in a population-based sample of 6-year-old Australian children. Ophthalmology 112, 1275–1282, https://doi.org/10.1016/j.ophtha.2005.01.052 (2005).
Fu, J. et al. Prevalence of amblyopia and strabismus in a population of 7th-grade junior high school students in Central China: the Anyang Childhood Eye Study (ACES). Ophthalmic Epidemiol 21, 197–203, https://doi.org/10.3109/09286586.2014.904371 (2014).
Chen, X. et al. Prevalence of amblyopia and strabismus in Eastern China: results from screening of preschool children aged 36-72 months. Br J Ophthalmol 100, 515–519, https://doi.org/10.1136/bjophthalmol-2015-306999 (2016).
Fu, J. et al. Prevalence, causes and associations of amblyopia in year 1 students in Central China: The Anyang childhood eye study (ACES). Graefes Arch Clin Exp Ophthalmol 252, 137–143, https://doi.org/10.1007/s00417-013-2451-z (2014).
Acknowledgements
This work is supported by the National Natural Science Foundation of China (Grant No. 81400435 and No. 81560169). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Hu Liu conceived of and designed the study. Chen-Wei Pan, Xuejuan Chen, Hui Zhu, Zhujun Fu, Hua Zhong, Jun Li, Dan Huang and Hu Liu performed the experiments. Chen-Wei Pan and Xuejuan Chen analyzed the dataset. Chen-Wei Pan and Xuejuan Chen wrote the manuscript. Chen-Wei Pan, Xuejuan Chen, Hui Zhu, Zhujun Fu, Hua Zhong, Jun Li, Dan Huang and Hu Liu reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pan, CW., Chen, X., Zhu, H. et al. School-based assessment of amblyopia and strabismus among multiethnic children in rural China. Sci Rep 7, 13410 (2017). https://doi.org/10.1038/s41598-017-13926-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-13926-8
This article is cited by
-
Prevalence and associated risk factors for childhood strabismus in Lhasa, Tibet, China: a cross-sectional, school-based study
BMC Ophthalmology (2020)
-
Validation of dynamic random dot stereotests in pediatric vision screening
Graefe's Archive for Clinical and Experimental Ophthalmology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.