Abstract
The international staging system (ISS), based on serum beta-2 microglobulin and albumin, is used to predict survival in multiple myeloma, but its prognostic significance in diffuse large B-cell lymphoma (DLBCL) remains unknown. Herein, we retrospectively analyzed 215 de novo DLBCL patients. According to ISS, there were 90 of 215 (41.9%) patients in stage I, 98 of 215 (45.6%) in stage II and 27 of 215 (12.6%) in stage III group. Patients with ISS stage II/III showed shorter overall survival (OS) and event free survival (EFS) than those with stage I treated with R-CHOP (p = 0.012 and p = 0.043, respectively), but not those treated with CHOP regimen (p > 0.05). Multivariable analysis revealed that ISS, independent of IPI, indicated different survival in both OS (HR, 5.690; 95% CI, 1.270–25.495, p = 0.023) and EFS (HR, 2.116; 95% CI, 1.005–4.455, p = 0.049) in DLBCL patients treated with R-CHOP. ISS could identify patients with better outcome in intermediate-high/high IPI risk patients (p < 0.05). Our data suggests that advanced ISS stage is associated with inferior outcome in DLBCL patients treated with R-CHOP. ISS could identify a subgroup of DLBCL patients with superior outcome from high IPI risk patients, which may help to avoid intensive therapy.
Similar content being viewed by others
Introduction
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin’s lymphoma (NHL) with different clinical behaviors and response to treatment1. Although the addition of rituximab into CHOP regimen (cyclophosphamide, doxorubicinm vincristine and prednisone) has dramatically improved the survival of DLBCL patients2,3,4, about one third of patients with DLBCL succumbs to the disease eventually5,6. It is urgent to find new prognostic markers to identify those patients with very good or poor outcome and then give them more individualized therapy.
Based on the serum beta-2 microglobulin (Sβ2M) and serum albumin (SA) levels, the international staging system (ISS) has been used to evaluate the prognosis in multiple myeloma for many years7. However more and more evidence show that ISS is more related with the host features and immune system than multiple myeloma stage8. In this situation, ISS could also be used to predict outcome in the other hematological malignancies. Increasing studies show both Sβ2M and SA could predict outcome in DLBCLs9,10,11,12,13. However, to the best of our knowledge, the prognostic value of the combination of Sβ2M and SA in DLBCL has not been validated yet. Therefore, the purpose of the present study was to evaluate the prognostic significance of ISS in patients with DLBCL.
Methods
In the present study, a total of 215 patients consecutively diagnosed as de novo DLBCL from January, 2001 to February, 2013 in Nanfang Hospital were reviewed. Patients with immunodeficiency-associated tumors and various types of DLBCL, including primary mediastinal, central nervous system, intravascular, testicular lymphomas, transformed NHL and posttransplant lymphoproliferative disorder were excluded from the study. All patients treated with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) or R-CHOP (rituximab plus CHOP) chemotherapy. The disease stage was evaluated according to the Ann Arbor staging system. Performance status was assigned according to the Eastern Cooperative Oncology Group (ECOG) scale. According to the ISS, all patients were divided into three groups: stage I group: β2-microglobulin <3.5 mg/L and serum albumin ≥35 g/L, stage II group: not stage I or stage III, stage III group: β2-microglobulin >5.5 mg/L. Electronic medical records of patients were collected prospectively and reviewed retrospectively in this study. All patients had provided written informed consent themselves or their guardians prior to treatment allowing the use of their medical records for medical research. This study was approved by the Ethics Committee of Southern Medical University affiliated Nanfang Hospital. All methods were performed in accordance with relevant guidelines and regulations.
Mann-Whitney test was applied to compare the differences between groups. Overall survival (OS) was calculated from the date of diagnosis to death from any cause or the last follow-up. Event-free survival (EFS) was calculated from the date of diagnosis to the date of documented disease progression, relapse or death from any cause. OS and EFS were estimated using the method of Kaplan-Meier and the log-rank test. Multivariable analysis was conducted by Cox proportional hazard regression model. All p values were two-sided and the significance was defined as p < 0.05. Statistical analysis was done using the Statistical Package of Social Sciences version 13.0 for Windows.
Results
Patients’ characteristics
A total of 215 de novo DLBCL patients were retrospectively analyzed. The male-to-female ratio was 1.90: 1 and the median age of patients at diagnosis was 49 years (range 19–80 years), which was similar to three other recent studies of Chinese DLBCL patients14,15,16, but much younger than those reported for DLBCL populations in the Western countries17,18. Based on the IPI score, 58 patients (27.0%) were in the intermediate-high or high-risk groups. Seventy-two patients (33.5%) had B symptoms and 61.4% patients had a SA ≥35 g/L. At baseline, 71.6% patients had a β2-microglobulin <3.5 mg/L, 15.3% had a level from 3.5 mg/L to 5.5 mg/L and 13.0% had a level >5.5 mg/L. According to ISS, 90 patients were in stage I group, 98 patients in stage II group and 27 patients in stage III group. Patients with high ISS risk tended to present with B symptoms (p = 0.011), high LDH (p = 0.019) and high IPI score (p = 0.001). Seventy-eight patients were treated with CHOP and other 137 patients were treated with R-CHOP. Baseline clinical features at the time of diagnosis are listed in Table 1.
ISS predicted survival in DLBCL patients treated with R-CHOP
The median follow-up was 52 months. The 5-years overall survival (OS) and event-free survival (EFS) were 80.5% and 63.9% respectively for all DLCBL patients. With respective to treatment, 78 patients were treated with CHOP and other 137 patients were treated with R-CHOP. The 5-years OS and EFS were 66.2% and 51.9% in patients treated with CHOP and 87.9% and75.8% in patients treated with R-CHOP.
ISS showed no significant impact on OS and EFS in DLBCL patients treated with CHOP regimen (p = 0.906 and p = 0.972, respectively, Figure S1A–B). However, in the cases treated with R-CHOP, ISS could divide patients into different prognostic groups (p = 0.012, with 5-year OS of 96.4% versus 83.2% versus 75.8% for stage I, II and III respectively; p = 0.043, with 5-year EFS of 79.9% versus 60.8% versus 65.7% for stage I, II and III respectively, Figure S1C–D). Due to no significant differences were found between stage II and III groups, patients were re-divided into stage I and II/III groups with different prognosis (p = 0.012, with 5-year OS of 96.4% versus 81% for stage I, II/III respectively; p = 0.043, with 5-year EFS of 79.9% versus 61.8% for stage I, II/III respectively, Fig. 1) after incorporating stage II and stage III groups.
Multivariable analysis revealed that ISS, independent of IPI, indicated different survival in both OS (hazard ratio [HR] 5.690; 95% confidence interval [CI], 1.270–25.495, p = 0.023) and EFS (HR, 2.116; 95% CI, 1.005–4.455, p = 0.049) in DLBCL patients treated with R-CHOP. The multivariable survival analysis is shown in Table 2.
ISS improved the IPI risk stratification in DLBCL patients
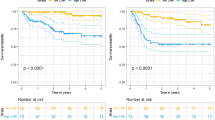
To further investigate whether ISS could improve the IPI risk stratification of DLBCL patients, we explored the prognostic value of ISS in low/low-intermediate and intermediate-high/high risk patients with DLBCL defined by IPI. ISS could identify a subgroup of patients with better outcome in intermediate-high/high risk patients (p = 0.042, with 5-year OS of 100% versus 78.0% for stage I and stage II/III, respectively; p = 0.029, with 5-year EFS of 90.9% versus 48.6% for stage I and stage II/III, respectively, Fig. 2A–B). However in low/low-intermediate risk patients, ISS could only identify patients with better overall survival (p = 0.036, with 5-year OS of 95.5% versus 82.9% for stage I and stage II/III, respectively), but not event-free survival (p = 0.293, with 5-year OS of 78.0% versus 70.5% for stage I and stage II/III, respectively, Fig. 2C–D).
Kaplan-Meier curve for overall survival (OS) and event-free survival (EFS) in DLBCL patients treated with R-CHOP according to ISS. OS (A) and EFS (B) for low/ low intermediate risk IPI DLBCL patients (IPI = 0–2) according to ISS. OS (C) and EFS (D) for high intermediate/high IPI risk DLBCL patients (IPI = 3–5) according to ISS.
Discussion
ISS, defined by two routine and inexpensive pieces: Sβ2M and SA levels, is the most important prognostic system for multiple myeloma in the past ten years7. Recently more and more studies show both Sβ2M and SA could be used to predict outcome in DLBCLs9,10,11,12,13. But none of those studies have evaluated the prognostic value of the combination of Sβ2M and SA in DLBCL. In the present study, we retrospectively evaluated the prognostic significance of ISS in newly diagnosed DLBCL patients. To the best of our knowledge, this is the first time to provide evidence that advanced ISS stage at diagnosis was strongly associated with high-risk clinical features and indicated dismal outcome in DLBCL patients receiving rituximab-contained immunochemotherapy.
The underlying mechanisms by which ISS predicts DLBCL outcome are unclear. Decreased SA may be caused by the cytokine release by tumor cells such as IL-6 and the intense inflammatory response to the tumor, which may be a surrogate for a more aggressive behavior19,20,21. In this study, we also found that DLBCL patients with low serum albumin tended to present with aggressive clinical behavior including elevated LDH, B symptoms, advanced Ann Arbor stage and subsequent unfavorable outcome, which was consistent with previous studies19.
Increasing studies shows that elevated Sβ2 M is associated with dismal outcome in patients with DLBCL12,13,22. However the mechanisms for Sβ2M and outcome in DLBCL remain largely unknown. β2M is a subunit of the light chain of the class I major histocompatibility complex (MHC) and is released from the complex during cell turnover23. Elevated Sβ2M also implies the abnormal of the light and heavy chains of MHC class molecules, which can help cancer cells change epitope expression to escape T cell recognition24,25. Thus, Sβ2M may indicate cell turnover rate, high tumor burden and immune disorder in patients with DLBCL which is associated with survival.
Our study also showed IPI independent impact of ISS on the survival of DLBCL patients treated with rituximab-contained immunochemotherapy. This observation supports the involvement of ISS in immune system mediating the effect of rituximab and may provide further information on the mechanism of effect of rituximab. Further analysis showed ISS was able to identify a subset of very good outcome patients in high IPI risk DLBCL patients and if confirmed in further series could further improve risk stratification to guide treatment in DLBCLs. It is interesting that another study showed albumin can improve the low-risk NCCNIPI definition, in partially agreement with our findings. The addition of low serum albumin as a risk factor into NCCN-IPI augmented NCCN-IPI identifies more patients as low risk and maintains the excellent prognosis for this group compared to the conventional NCCN-IPI risk definition26.
It should be noted that this is a retrospective study with a relatively small number of patients from a single medical center. Therefore, the choice of patients might have been biased. Nevertheless, we only enrolled patients with de novo DLBCL treated with standard first-line chemotherapy in this study, and all electronic medical records for patients were collected prospectively, which can reduce bias to the least. In addition, we suggest prospective study of larger cohorts in multi-centers to be performed in order to confirm our findings.
In conclusion, our retrospective study evaluated the prognostic value of ISS at diagnosis in an independent cohort of de novo DLBCL. Although need to be confirmed prospectively, our data suggests that advanced ISS stage is associated with an inferior outcome in DLBCL patients treated with R-CHOP. ISS could identify a subgroup of DLBCL patients with superior outcome from high IPI risk subgroup. If confirmed in prospective clinical trials, these findings will have immediate clinical value, which can help to avoid intensive therapy in the high IPI risk subgroup of DLBCL patients.
Change history
03 May 2019
A correction to this article has been published and is linked from the HTML and PDF versions of this paper. The error has been fixed in the paper.
References
Swerdlow, S. H., Campo, E. & Harris, N. L. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissue (4th Ed). Lyon, France: IARC (2008).
Coiffier, B. et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. The New England journal of medicine 346, 235–242, https://doi.org/10.1056/NEJMoa011795 (2002).
Habermann, T. M. et al. Rituximab-CHOP versus CHOP alone or with maintenance rituximab in older patients with diffuse large B-cell lymphoma. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 24, 3121–3127, https://doi.org/10.1200/jco.2005.05.1003 (2006).
Pfreundschuh, M. et al. CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large-B-cell lymphoma: a randomised controlled trial by the MabThera International Trial (MInT) Group. The Lancet. Oncology 7, 379–391, https://doi.org/10.1016/s1470-2045(06)70664-7 (2006).
Coiffier, B. & Sarkozy, C. Diffuse large B-cell lymphoma: R-CHOP failure-what to do? Hematology / the Education Program of the American Society of Hematology. American Society of Hematology. Education Program 2016, 366–378, https://doi.org/10.1182/asheducation-2016.1.366 (2016).
Muffly, L. S. & Smith, S. M. Prognosis in diffuse large B-cell lymphoma: the picture continues to come into focus. Cancer 119, 1129–1131, https://doi.org/10.1002/cncr.27860 (2013).
Greipp, P. R. et al. International staging system for multiple myeloma. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 23, 3412–3420, https://doi.org/10.1200/jco.2005.04.242 (2005).
Bataille, R., Annweiler, C. & Beauchet, O. Multiple Myeloma International Staging System: “Staging” or Simply “Aging” System? Clinical Lymphoma Myeloma and Leukemia 13, 635–637, https://doi.org/10.1016/j.clml.2013.07.003 (2013).
Bairey, O., Shacham-Abulafia, A., Shpilberg, O. & Gurion, R. Serum albumin level at diagnosis of diffuse large B-cell lymphoma: an important simple prognostic factor. Hematological oncology 34, 184–192, https://doi.org/10.1002/hon.2233 (2016).
Dalia, S. et al. Serum albumin retains independent prognostic significance in diffuse large B-cell lymphoma in the post-rituximab era. Annals of hematology 93, 1305–1312, https://doi.org/10.1007/s00277-014-2031-2 (2014).
Eatrides, J., Thompson, Z., Lee, J. H., Bello, C. & Dalia, S. Serum albumin as a stable predictor of prognosis during initial treatment in patients with diffuse large B cell lymphoma. Annals of hematology 94, 357–358, https://doi.org/10.1007/s00277-014-2150-9 (2015).
Miyashita, K. et al. Beta-2 microglobulin is a strong prognostic factor in patients with DLBCL receiving R-CHOP therapy. Leukemia research 39, 1187–1191, https://doi.org/10.1016/j.leukres.2015.08.016 (2015).
Seo, S. et al. Prognostic significance of serum beta-2 microglobulin in patients with diffuse large B-cell lymphoma in the rituximab era. Oncotarget 7, 76934–76943, https://doi.org/10.18632/oncotarget.12734 (2016).
Li, X. et al. The Glasgow Prognostic Score as a significant predictor of diffuse large B cell lymphoma treated with R-CHOP in China. Annals of hematology 94, 57–63, https://doi.org/10.1007/s00277-014-2167-0 (2015).
Jin, X. et al. Homozygous A polymorphism of the complement C1qA276 correlates with prolonged overall survival in patients with diffuse large B cell lymphoma treated with R-CHOP. Journal of hematology & oncology 5, 51, https://doi.org/10.1186/1756-8722-5-51 (2012).
Zhou, D. et al. Prognostic values of various clinical factors and genetic subtypes for diffuse large B-cell lymphoma patients: a retrospective analysis of 227 cases. Asian Pacific journal of cancer prevention: APJCP 14, 929–934 (2013).
Sehn, L. H. et al. Impact of concordant and discordant bone marrow involvement on outcome in diffuse large B-cell lymphoma treated with R-CHOP. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 29, 1452–1457, https://doi.org/10.1200/jco.2010.33.3419 (2011).
Iqbal, J. et al. BCL2 predicts survival in germinal center B-cell-like diffuse large B-cell lymphoma treated with CHOP-like therapy and rituximab. Clinical cancer research: an official journal of the American Association for Cancer Research 17, 7785–7795, https://doi.org/10.1158/1078-0432.ccr-11-0267 (2011).
Zhou, Q. et al. Low prognostic nutritional index predicts poor outcome in diffuse large B-cell lymphoma treated with R-CHOP. Int J Hematol 104, 485–490, https://doi.org/10.1007/s12185-016-2052-9 (2016).
McMillan, D. C. et al. Albumin concentrations are primarily determined by the body cell mass and the systemic inflammatory response in cancer patients with weight loss. Nutrition and cancer 39, 210–213, https://doi.org/10.1207/S15327914nc392_8 (2001).
Jacobson, J. L. et al. A new staging system for multiple myeloma patients based on the Southwest Oncology Group (SWOG) experience. British journal of haematology 122, 441–450 (2003).
Chen, Y. et al. Prognostic significance of baseline peripheral absolute neutrophil, monocyte and serum beta2-microglobulin level in patients with diffuse large b-cell lymphoma: a new prognostic model. British journal of haematology 175, 290–299, https://doi.org/10.1111/bjh.14237 (2016).
Shi, C., Zhu, Y., Su, Y., Chung, L. W. & Cheng, T. Beta2-microglobulin: emerging as a promising cancer therapeutic target. Drug discovery today 14, 25–30, https://doi.org/10.1016/j.drudis.2008.11.001 (2009).
Topfer, K. et al. Tumor evasion from T cell surveillance. Journal of biomedicine & biotechnology 2011, 918471, https://doi.org/10.1155/2011/918471 (2011).
Vinay, D. S. et al. Immune evasion in cancer: Mechanistic basis and therapeutic strategies. Seminars in cancer biology 35(Suppl), S185–198, https://doi.org/10.1016/j.semcancer.2015.03.004 (2015).
Melchardt, T. et al. A modified scoring of the NCCN-IPI is more accurate in the elderly and is improved by albumin and beta2 -microglobulin. British journal of haematology 168, 239–245, https://doi.org/10.1111/bjh.13116 (2015).
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant No. 81600165, 81670183), the Natural Science Foundation of Guangdong Province (Grant No. 2014A030313277).
Author information
Authors and Affiliations
Contributions
F.R. and W.X.L. designed the study, analyzed and interpreted the data. W.Y.Q., H.X.X., W.Q., Z.Y.K., H.W.M. and S.J.L. collected data. F.R., W.X.L. and Z.L.Z. analyzed data and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wei, X., Hao, X., Zhou, L. et al. The international staging system improves the IPI risk stratification in patients with diffuse large B-cell lymphoma treated with R-CHOP. Sci Rep 7, 13592 (2017). https://doi.org/10.1038/s41598-017-13254-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-13254-x
This article is cited by
-
Albumin improves stratification in the low IPI risk patients with diffuse large B-cell lymphoma
International Journal of Hematology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.