Abstract
Streptococcus agalactiae (GBS) is the leading cause worldwide of neonatal sepsis. We sought to assess to which extent HIV exposure of neonates is associated with GBS neonatal disease. Furthermore, we assessed to which extent HIV infection in women is associated with maternal rectovaginal GBS carriage, the single most important risk factor for GBS neonatal disease. We searched Pubmed, Embase, and Web of Science for studies assessing the association between neonatal GBS disease and HIV-status of the mother and studies that assessed the association between rectovaginal GBS colonization and HIV status in women. HIV-exposed uninfected neonates were more than twice as likely to have neonatal GBS disease compared to unexposed neonates. HIV-exposed neonates were not at increased risk for early-onset neonatal disease, but were 4.43 times more likely to have late-onset neonatal GBS disease. There was no significant association between HIV infection status and rectovaginal GBS carriage. Public health interventions preventing neonatal GBS disease are urgently needed for the increasing group of HIV-exposed neonates. A framework integrating and explaining our findings highlights opportunities for the clinical practice and global health policy to prevent disease. Well-designed studies should clarify the relation between HIV-status and GBS carriage.
Similar content being viewed by others
Introduction
One million children die each year in the first 4 weeks of life because of neonatal disease1. Early-onset neonatal disease (EOD), which occurs in the first week of life and most often within 24 hours after birth, is caused by bacteria that are transmitted from the genital tract of the mother before or during delivery2. Late-onset neonatal disease (LOD) occurs between the first week and the third month of life and may be caused by bacteria acquired vertically or horizontally3.
Streptococcus agalactiae (Group B Streptococcus (GBS)), present in the vagina and/or gastro-intestinal tract of 20 to 30% of pregnant women, is the most common infectious agent identified in case of EOD4 and an important pathogen in LOD5. Although vaginal carriage of GBS usually remains asymptomatic, it has been associated with chorioamnionitis6, spontaneous abortion7,8, premature labor9, premature delivery10, premature rupture of membranes11 and puerperal sepsis12,13, causing substantial neonatal and maternal morbidity and mortality1,2,14,15.
Infants born to HIV-infected mothers have increased rates of infectious morbidity and mortality compared to non-exposed infants, even if they remain HIV-uninfected16,17. Since the first study reporting an increased risk of GBS neonatal disease in HIV-exposed neonates17, evidence for this association has been accumulating.
A possible explanation for these observations might be higher rectovaginal GBS carriage rates in HIV-infected women, as rectovaginal GBS carriage is a major risk factor for GBS neonatal sepsis.
Indeed, HIV might influence the microbial composition of the vagina, rectum and colon18,19,20,21,22 and HIV infection in women has been associated with increased prevalence of vaginal candidiasis and sexually transmitted infections23,24. However, conflicting results have been reported for the association between HIV infection and rectovaginal carriage of GBS25,26.
The objectives of this systematic review and meta-analysis were to assess to which extent HIV exposure of neonates is associated with GBS neonatal disease and to clarify to which extent HIV infection of women is associated with rectovaginal GBS carriage, a major risk factor for GBS neonatal disease.
Research in context
Evidence before this study
Mother-to-child transmission of HIV is one of the great tragedies of the HIV pandemic. Although the number of HIV-infected infants is declining due to interventions for the elimination of pediatric HIV infection, the number of newborns that are HIV-uninfected but HIV-exposed through their HIV-infected mothers is on the rise. Interest in the health outcomes of these HIV-exposed infants has grown in the past decade, and several studies suggest increased mortality rates and increased infectious morbidity.
Neonatal sepsis causes one million neonatal deaths yearly, and Group B Streptococcus (GBS) is the leading cause. Since 2010, evidence has also been accumulating for an association between HIV-uninfected neonates born to HIV-infected mothers and neonatal sepsis caused by Group B Streptococcus (GBS). Regarding the association between maternal vaginal GBS carriage – the single most important risk factor, if not, a prerequisite, for GBS neonatal sepsis – and HIV-infection in mothers, conflicting results have been reported.
Added value of this study
To our knowledge, this systematic review and meta-analysis is the first to examine the association between HIV-exposure of neonates and the risk for neonatal disease caused by GBS. We performed subgroup analysis to further clarify the risk for the early-onset form of GBS neonatal sepsis, and the late-onset form. Furthermore, we performed a meta-analysis to assess the risk for maternal vaginal GBS carriage in HIV-infected compared to uninfected women. We present a pathogenic framework, explaining our findings regarding the associations between neonatal HIV-exposure and early-and late-onset neonatal sepsis. This framework offers opportunities for the clinical practice and global health policy to reduce HIV-related neonatal morbidity and mortality rates.
Implications of all the available evidence
Neonates born to HIV-infected mothers, but themselves uninfected, are at increased risk for GBS neonatal sepsis. Subgroup analysis showed that these neonates were four times more likely to have the GBS late-onset form, but were not at increased risk for the early-onset form. We found no association between maternal vaginal GBS carriage and HIV-infection, but included studies suffered from major limitations.
The health needs of HIV-exposed, uninfected infants should be prioritized further. Particularly in sub-Saharan Africa, were 90% of new HIV infections occurs and the burden of neonatal mortality is the highest, public health interventions reducing neonatal mortality rates are urgently needed. Feeding strategies should be explored to reduce LOD in infants born to HIV-infected mothers.
Methods
Protocol and registration
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines27 for carrying out and reporting this systematic review and meta-analysis, using an a priori defined protocol. This systematic review and meta-analysis has been registered in PROSPERO under registration number CRD42016033414.
Eligibility criteria
We included studies that assessed the association between neonatal GBS disease and HIV-status of the mother and studies that assessed the association between rectovaginal GBS colonization and HIV status in adult women. We only included studies that reported a sample size and a measure of effect for the associations assessed or provided the data to calculate the latter. There were no restrictions in terms of study design, manuscript language, or date of publication. We included papers that were published up to 1 November 2015.
Reviews, conference abstracts, comments, guidelines, case reports or case series, unpublished articles, multiple reports of the same data and in vitro and animal studies were not considered for inclusion. We excluded studies that had no clear description of the assessment of the HIV status of the women, of the HIV exposure of the neonates, or of the laboratory methodology to assess rectovaginal GBS carriage. GBS neonatal disease was defined as the presence of GBS as assessed by molecular methods, culture from blood, cerebrospinal fluid or another normally sterile site, or by latex agglutination in cerebrospinal fluid, in neonates below 90 days of age.
Search strategy
We searched the MEDLINE (through PubMed), Web of Science, and EMBASE databases for bibliographic references. We used the combination of all of the following search terms (Streptococcus agalactiae, S. agalactiae, GBS, Group B Streptococcus, Group B streptococci, early-onset disease, early-onset sepsis, late-onset disease, late-onset sepsis, neonatal sepsis, neonatal septicemia, neonatal pneumonia or neonatal meningitis) with all of the following search terms (human immunodeficiency virus, HIV, HIV-1, or AIDS).
The bibliographic references of the studies that were considered eligible were also hand searched.
Study selection
Studies were selected in a two-stage process (Fig. 1). First, all bibliographic references were screened to identify studies for full text evaluation by one reviewer (PC), on the basis of only the information present in the title and abstract. Subsequently, the full texts of those articles not excluded in the screening process were assessed for eligibility, using the aforementioned criteria, by two authors independently (PC and MV). Reasons for inclusion or exclusion were recorded and categorized, and disagreements were resolved by consensus (Supplementary Table 1).
Selected studies were divided into two categories, i.e. studies reporting an association between HIV-exposure and GBS invasive neonatal disease in infants (or providing data to calculate this), and studies reporting an association between HIV infection and rectovaginal GBS carriage in adult women (or providing data to calculate this).
Data collection process
A predefined data extraction form was pilot-tested and used for data extraction. From each individual study, information was collected on authors, year of publication, journal, country where the study had been carried out, study design, sample collection period, study population, age of the participants, total number of study participants, total number of samples included in the analysis, HIV assessment and prevalence, GBS neonatal disease assessment and incidence, rectovaginal GBS carriage assessment and prevalence, relevant measures of effects, statistics, correction for confounding, and epidemiological strengths and weaknesses.
This procedure was performed for each article independently by two authors (PC, and TC, VJ, ES, JVDW or MV) and disagreements were resolved by discussion between both authors. Further information or clarification from manuscript authors was sought by PC on seven occasions.
Risk of bias in individual studies
To assess the quality and risk of bias of the included studies, we developed a quality appraisal tool (Supplementary Table 2), based on the Newcastle-Ottawa Scale28. This scale is a bias assessment tool for observational studies, recommended by the Cochrane Collaboration29. We adapted this tool to the content of the meta-analysis. For example, consideration was given to the methodology used to assess rectovaginal GBS carriage.
Stars were assigned by PC for three broad criteria (representativeness of the study groups, comparability of the study groups, and quality of the outcome assessment) in order to provide a measure of their quality. In this context, good representativeness is defined as those exposed/unexposed being similar to others in the community they come from, and good comparability is defined as the exposed and unexposed being similar in all respects other than their HIV or HIV exposure status.
Studies that scored none or one, two or three, or four stars for representativeness were classified as having respectively a high, medium or low risk of bias for this criterion. Studies assigned none, one, or two stars for comparability or outcome were considered to have respectively a high, medium or low risk of bias for comparability and outcome.
Data analysis
First, an odds ratio (OR) was calculated for studies that did not present them. We compared the odds of neonatal GBS disease in neonates born to HIV-infected mothers versus infants born to HIV-uninfected mothers, and the odds of rectovaginal GBS carriage in HIV-positive versus HIV-negative women, using unadjusted counts. All neonates born from HIV-positive women were considered as HIV-exposed, regardless of their infection status. Rectovaginal GBS carriage was defined as GBS detected in the vagina and/or rectum and/or (peri)anal region by culture. While our protocol also included detection of rectovaginal and neonatal GBS by molecular testing, none of the eligible studies used molecular testing, and the results reported in this manuscript are based on culture and latex agglutination results only.
We reported the results of the meta-analyses obtained after pooling individual study estimates with random effects model as ORs with 95% confidence interval (CI). The degree of heterogeneity between the studies was assessed using the I2 index, with percentages of 30–50%, 50–75% and 75–100% being indicative of moderate, substantial and considerable heterogeneity, respectively30.
A priori planned subanalyses were performed for GBS neonatal disease by considering early-onset and late-onset neonatal GBS disease separately, relying on the authors’ own classification into these two groups.
To assess publication bias, funnel plots were created by plotting the natural logarithm of the ORs against the inverse of the standard error. The asymmetry of the funnel plots was visually inspected and statistically checked using Egger’s regression test and Begg and Mazumdar’s rank correlation test31,32. All statistical analyses were carried out using the Comprehensive Meta-Analysis software package v3 (Biostat Inc., Englewood, NJ).
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Manuscript and study selection
A total of 546 unduplicated citations were identified, we selected 81 abstracts for full text evaluation (Fig. 1). Of these, 32 manuscripts did not report results on GBS disease or carriage or HIV exposure, seven were reviews, book chapters or letter to editors, nine did not include an HIV-negative or GBS-negative group, 11 did not present measures of effect or the data to calculate these, four reported already published data, and one paper could not be found (Supplementary Table 1).
Seventeen manuscripts reporting on 19 studies met the inclusion criteria. These included four studies reporting on neonatal GBS disease only, 11 studies reporting on rectovaginal carriage only, and two studies reporting both (Fig. 1). A list of these studies and a digest of the extracted information is presented in the Supplementary Tables 3 and 4.
Description of selected studies
Six studies, reporting a total of 252,051 births, reported cases of infants with GBS neonatal disease born to HIV-infected mothers compared to infants with GBS neonatal disease born to HIV-uninfected mothers17,33,34,35,36,37. Five of these studies were conducted in South Africa33,34,35,36,37 and one was performed in Belgium17. All infants included were born in a hospital. For the laboratory diagnosis of GBS neonatal disease, all studies used the BacT/ALERT microbial detection system to detect bacteria in blood and/or cerebrospinal fluid samples. Positive samples were subcultured on blood agar plates and identification was subsequently performed using standard identification methods.
For the second category, thirteen studies, representing a total of 10,105 women, provided rectovaginal GBS carriage ratios of HIV-infected versus HIV-uninfected women7,25,26,34,35,38,39,40,41,42,43,44,45. Eleven of these studies were conducted in low-or-middle income countries, i.e. three studies in South Africa34,35,43, two studies in Tanzania39,41, and one study in Burkina Faso, Brazil, Democratic Republic Congo, Kenya, Malawi, and Zimbabwe7,25,26,38,40,42 and two in a high-income country namely Spain and the US44,45. All these studies recruited pregnant women in a hospital setting, except for the study of Djigma and coworkers in Burkina Faso (2011), who recruited non-pregnant women, and the study of Ulla and coworkers in Spain (1993), who recruited female sex workers attending a family planning center.
Rectovaginal GBS carriage was assessed by culture in all studies: five studies performed rectovaginal sampling and culturing with the use of an enrichment broth, as recommended by the Centers for Disease Control and Prevention (CDC) guidelines26,40,41,42,44, two studies only sampled vaginally with cultures performed according to the CDC guidelines34,35 and the remaining six studies did not culture according to CDC guidelines or did not report the exact culture methods used7,25,38,39,43,45.
Of the 19 studies described of the 17 manuscripts, three were retrospective17,37,44, fourteen were cross-sectional7,25,26,33,34,35,36,39,40,41,42,43 and none were prospective.
One study reported two different analyses for rectovaginal GBS carriage in HIV-infected versus uninfected women, i.e. using the total cohort versus matched subsets35. The analysis least prone to bias (i.e. the matched subsets) was used for this meta-analysis. The same study analyzed matched subsets for the association of HIV exposure of neonates and GBS neonatal disease and early-onset GBS neonatal disease, but not for late-onset GBS neonatal disease. Therefore, we used the total cohort analysis for these associations.
Risk of bias within studies
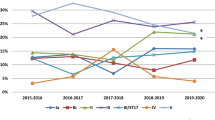
The results of the critical appraisals of the included studies are shown in Fig. 2 and Supplementary Table 5. All six studies addressing the relationship between HIV exposure of neonates and GBS neonatal disease were assessed as having a low risk of bias for representativeness17,33,34,35,36,37. Two out of the six studies had a low risk of bias for comparability33,35, two had a medium risk34,36 and two had a high risk17,37. For the GBS disease outcome assessment, four studies were assessed as having a low risk of bias33,35,36,37 and two had a medium risk17,34.
Quality assessment using an adapted Newcastle-Ottawa Scale for risk of bias of studies included in the systematic review. Left, studies (n = 13) reporting an association between HIV infection and rectovaginal GBS carriage. Right, studies (n = 6) reporting an association between neonatal HIV exposure and neonatal GBS disease. The absolute numbers of studies are shown in the boxes.
Of the studies on HIV infection and maternal GBS carriage only two out of the thirteen studies were assessed as having a low risk of bias for representativeness35,40, nine studies a medium risk7,25,26,34,39,41,42,43,45 and two studies a high risk38,44.
Three out of the thirteen studies were assessed as having a low risk of bias for comparability35,40,44, four a medium risk34,39,41,43, and six a high risk7,25,26,38,42,45. The risk of bias for outcome assessment was low in five out of the thirteen studies26,40,41,42,44; medium in two studies34,35 and high in six studies7,25,38,39,43,45.
Association of maternal HIV status with GBS neonatal disease
The meta-analysis of the association between HIV exposure of neonates and GBS neonatal disease showed that HIV-exposed neonates were more than twice as likely to have neonatal GBS disease compared to unexposed neonates (OR, 2.39; CI, 1.31–4.38; p = 0.005) (Fig. 3). The crude OR in the individual studies ranged from 1.72 to 19.86, with three of the six individual studies showing a statistically significant association. The subanalyses showed that HIV-exposed neonates were not at increased risk for early-onset neonatal disease (OR, 1.31; 95% CI, 0.84–2.04; p = 0.240), but were 4.43 times more likely to have late-onset neonatal disease (95% CI, 1.81–10.85; p = 0.001).
Forest plot of estimates of association between HIV exposure and GBS neonatal disease. Studies are plotted alphabetically according to the last name of the first author and followed by the publication year. Each study is represented by a black square and a horizontal line, which corresponds to the OR and 95% CI, respectively. The areas of the black squares reflect the weight of the study (determined by random effects analysis) in the meta-analysis. The vertical line in the middle corresponds to an OR of 1.0. The diamonds represents the overall summary estimate for EOD, LOD and total GBS disease, respectively, with the 95% CIs given by the width. In the columns on the right, the number of cases on the total number of HIV-positive and of HIV-negative mothers is given, respectively, for each study. aDangor, 2015, JID; bDangor, 2015, PONE; CI, confidence interval; OR, odds ratio; //95% CI line exceeding OR 100.
As recommended by Sterne and co-workers (2011)46 to only create funnel plots when the number of studies is ten or more, we did not create a funnel plot for this meta-analysis.
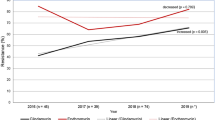
Association of HIV infection and rectovaginal GBS carriage
In our meta-analysis of the association between HIV infection and rectovaginal GBS carriage, we found no significant association between HIV infection status and rectovaginal GBS carriage (OR 1.09; 95% CI 0.82–1.44; p = 0.55) (Fig. 4). The crude ORs in the individual studies ranged from 0.26 to 4.22, with only three studies reporting a statistically significant association7,25,35. Two of these studies found a significantly higher rectovaginal carriage rate in HIV-positive women7,25, whereas one study found a significantly lower rate35.
Forest plot of estimates of association between HIV infection and rectovaginal GBS carriage. Studies are plotted alphabetically according to the last name of the first author and followed by the publication year. Each study is represented by a square and a horizontal line, which corresponds to the OR and the 95% CI, respectively. The magnitude of the squares reflects the weight of the study (determined by random effects analysis) in the meta-analysis. The vertical line in the middle indicates the OR 1.0. The diamond at the bottom represents the summary estimate, with its width indicating the 95% CI. The two columns on the right document the number of GBS cases on the total of HIV-positive and of HIV-negative women, respectively, for each study. aDangor, 2015, JID; CI, confidence interval; OR, odds ratio; bold, p < 0.05.
The heterogeneity among these studies is substantial (I2 = 68.7%). Visual inspection of the funnel plot shows an asymmetrical distribution of studies, suggesting publication bias (Fig. 5), which is marginally supported by Egger’s regression intercept (0.94; 95% CI −0.48–2.37; p = 0.09), but not by the Begg and Mazumdar’s rank correlation test (Kendall’s tau = −0.10, one-tailed p-value = 0.313). Two studies7,25 fall outside the pseudo 95% confidence interval, providing further evidence of heterogeneity and bias.
Funnel plot to assess publication bias among studies evaluating the association between HIV infection and rectovaginal GBS carriage. The circles represent the estimates of the 11 included studies of association between HIV infection and rectovaginal GBS carriage. The log of the odds ratio is plotted on the horizontal axis, against the inverse of the standard error of the odds ratio on the vertical axis. The vertical line in the funnel plot indicates the fixed-effects summary estimate and the sloping lines indicate the expected 95% confidence intervals for a given standard error.
Discussion
Group B streptococci (GBS) are a major cause of neonatal sepsis, which results in one million neonatal deaths every year1. Also, studies have repeatedly shown that HIV-negative neonates that had been exposed to HIV during pregnancy are at increased risk for infectious morbidity and mortality (reviewed in47). In this systematic review and meta-analysis, we assessed the risk for GBS neonatal disease in HIV-exposed neonates. We also assessed the risk for rectovaginal GBS carriage in HIV-infected women, as rectovaginal carriage is a major risk factor for neonatal GBS disease.
We found convincing evidence that HIV-exposed neonates were at higher risk for GBS neonatal disease. When analyzing cases of early-onset GBS and late-onset GBS disease separately, we found that this increased risk pertains to late-onset disease only.
There are several factors associated with HIV infection in pregnant women or mothers that might explain why infants born to HIV-infected mothers are at increased risk for late-onset, but not early-onset GBS disease. In the case of early-onset GBS disease, the factors that increase or decrease the risk for early-onset GBS disease might be well-balanced, while in the case of late-onset GBS disease, the net result may be an enhanced risk (Fig. 6).
Framework explaining a higher prevalence of LOD (but not of EOD) in HIV-uninfected infants born to HIV + mothers compared to HIV- mothers. (1): lower concentrations of anti-GBS antibodies and cytokines in the circulation of HIV + mothers compared to HIV- mothers (↑EOD,↑LOD); (2): reduced transplacental transfer rate (symbolized by the narrower arrow) of anti-GBS antibodies and cytokines in HIV + mothers leading to reduced fetal immunity (↑EOD,↑LOD); (3): antiretrovirals in circulation of HIV + mothers might cause neonatal immune dysfunction (↑EOD,↑LOD); (4): higher rates of caesarean section in HIV + women compared to HIV- women (symbolized by the broader arrow), leading to a lower risk of GBS transmission during vaginal birth but also leading to neonatal gut dysbiosis (↓EOD,↑LOD); (5): antibiotic prophylaxis in HIV + women reduces vaginal carriages rates of GBS and hence risk GBS transmission during vaginal birth but is a contributor of neonatal gut dysbiosis (↓EOD,↑LOD); (6): lower prevalence of breastfeeding (symbolized by the narrower arrow) in HIV + mothers compared to HIV- mothers leading to a reduced passive immunity in their newborns and to neonatal gut dysbiosis (↑LOD); (7): neonatal gut dysbiosis leading to a reduced gut immunity and bacterial translocation (↑LOD); (8): HIV-infected women are at higher risk of having al low birth weight infant or a preterm delivery, both risk factors for EOD and LOD (↑EOD,↑LOD). ↓ = lower risk of, ↑ = higher risk of.
Factors that might decrease early-onset GBS disease rates in HIV-exposed neonates
Antibiotic prophylaxis
HIV-infected pregnant women widely use antibiotic prophylaxis (co-trimoxazole), as recommended by the World Health Organization (WHO)48. Co-trimoxazole, largely effective against GBS41, is likely to be responsible for lower GBS rectovaginal carriage rates in HIV-infected pregnant women. For instance, we previously showed, using GBS-specific quantitative PCR (qPCR), that none of 30 Rwandan HIV-infected women, of which 93.3% were on antibiotic prohylaxis, carried GBS49. Seale and coworkers found that the rectovaginal GBS carriage rate was significantly less in 161 HIV-positive women on co-trimoxazole prophylaxis (n = 161, 3.1% GBS positive) compared to HIV-positive women not on prophylaxis (n = 239, 8.4% GBS positive) and compared to HIV-negative women (n = 7285, 12.1% GBS positive)50. As in GBS EOD, GBS is thought to be transmitted to the neonate from the vagina during passage through the birth channel or, more commonly, to the fetus in utero after breaking of the membranes by an ascending infection from the vagina, reduction of vaginal GBS carriage rates might reduce the risk for the early-onset form, but not for the late-onset form, where GBS is considered to be more frequently community- or hospital-acquired, or acquired through gut translocation. Antibiotic prophylaxis might also lead to neonatal gut dysbiosis: see further.
Caesarean delivery
The prevalence of EOD might be reduced by the practice of elective caesarean section. Elective caesarean section, i.e. caesarean delivery before labor and before rupture of membranes, has been shown to reduce the risk of mother-to-child transmission of HIV by 80% (60% to 70% of mother-to-child transmissions occur during labor and vaginal delivery51,52. This has led to dramatically increased ECS rates in HIV-infected women in some countries52. Because of the modes of transmission of GBS in EOD and LOD (see ‘antibiotic prophylaxis’), ECS might reduce the risk for EOD but not for LOD. Interestingly, Wu and coworkers found that of the 28 EOD cases, significantly more were born by vaginal delivery compared to cesarean delivery (64.3 versus 35.7%, respectively). Mehar and coworkers studied 141 cases of neonatal sepsis (61.3% EOD and 39.7% LOD). Of the neonates born by vaginal delivery, 38.1% became septic compared to 21.2% who were delivered by cesarean section53. Hook and colleagues54 compared pregnancy outcomes among 497 women undergoing elective repeat cesarean delivery to 492 who attempted trial of labor and 989 women with routine vaginal delivery. They found that rates of suspected and confirmed neonatal sepsis were significantly lower in the elective repeat cesarean delivery group, although absolute numbers of cases were very small (9, 26 and 26 cases of suspected sepsis in elective repeat cesarean delivery, trial of labor and vaginal delivery, respectively; and 0, 4 and 1 cases of confirmed sepsis in elective repeat cesarean delivery, trial of labor and vaginal delivery, respectively). Caesarean delivery might also lead to neonatal gut dysbiosis: see further.
Factors that might increase late-onset GBS disease rates in HIV-exposed neonates
Formula feeding
Since 2009, the WHO recommends HIV-positive mothers to practice exclusive breastfeeding for their infants in combination with antiretroviral therapy (ART) for mother or infant. However, compared to HIV-negative women, HIV-positive women have been shown to preferentially choose exclusive replacement feeding or mixed feeding, or stop breastfeeding early, because of fear of HIV transmission through breast milk. This is a consequence of previous WHO guidelines recommending total avoidance of breastfeeding and/or because many advocates of programs for prevention of mother-to-child transmission recommend early weaning55,56,57,58,59,60,61. Lack of breastfeeding might hamper passive protection of the neonate against GBS neonatal disease as GBS specific IgA, present in breast milk, could offer GBS-specific protection62. Furthermore, HIV-infected mothers might have reduced IgA in breast milk, as has been shown to be the case for saliva63. These altered infant feeding practices are likely to have more effect on the incidence of LOD, considering the fact that most infants with EOD are already septic at birth or become septic shortly after birth.
Many other bioactive factors in breastmilk, such as growth factors and prebiotics, may contribute to a better immune response and development and these children are likely more resistant to infectious diseases64. This has been exemplified by some trials, where breastfed children born to HIV-positive mothers has significantly lower mortality rates compared to formula-fed children65,66. Formula feeding might also lead to neonatal gut dysbiosis: see below.
Neonatal gut dysbiosis
The human gut microbiome is involved in many aspects of health and disease by exerting metabolic, nutritional, and immunological effects on the host67. In healthy, vaginally delivered and term newborns, pioneering bacteria from the mother are encountered, tolerated and regulated by the naïve neonatal gut immune system. In turn, this emerging microbiome sculpts the gut immune, metabolic and barrier function67,68. This dynamic process is readily disrupted. Such disruption, termed dysbiosis, appears to be pivotal in development of LOS67,69,70. Neonatal gut dysbiosis compromises the integrity of the intestinal barrier and the development of the immune system, leading to an increased risk for bacterial gut translocation into the bloodstream of the neonates69,71,72.
The most important disturbing factors of the neonatal gut microbiome appear to be (i) C-section delivery, (ii) perinatal maternal and/or neonatal antibiotic use, and (iii) formula feeding73.
-
(i)
The gut microbiome differences between neonates born by vaginal delivery and caesarean section are striking. A landmark study by Dominquez-Bello and coworkers found that the former harbored a gut microbiome closely resembling their mother’s vaginal bacteria (e.g. lactobacilli), while the latter harbored a gut microbiome resembling that of the maternal skin (e.g. Staphylococcus, Corynebacterium, Propionibacterium spp.)74. Other studies have confirmed that neonates born by caesarean section have disturbed gut microbiomes compared to neonates born by vaginal delivery (reviewed in75).
-
(ii)
Multiple studies have shown that peripartum antibiotics disrupt the natural neonatal microbiome assembly73. For example, intrapartum antibiotics to prevent neonatal GBS disease has been associated with decreased bacterial diversity of the meconium76 and lower abundance of lactobacilli and bifidobacteria in the neonatal gut73. Administration of antibiotics to the neonate directly after birth has been associated with gut dysbiosis73 and with LOS77.
-
(iii)
Formula feeding can cause perturbations of the neonatal gut microbiome compared to breast milk, even if given in small amounts during breastfeeding73. Breast milk contains a mix of nutrients, bacteria, antimicrobial proteins and secretory IgA that affects the shaping of the normal neonatal gut microbiome. Formula milk has for example been associated with a decreased prevalence of bifidobacteria78, thought to suppress the growth of potentially pathogenic bacteria79. Clinical studies have shown that lack of breastfeeding is a risk factor for neonatal LOD and meningitis80,81,82, and it is tempting to hypothesize that the mechanistic pathway explaining these findings is a combination of the above-discussed consequences of formula feeding/lack of breastfeeding, ie. a reduced passive immunity and a dysbiotic gut microbiome.
The risk of bacterial translocation causing LOS is exacerbated in preterms and neonates with (very)-low birth weight: these are not only at higher risk of the above-mentioned risk factors leading to gut microbiome dysbiosis, but also have an increased intestinal permeability and an immature immune system79.
Factors that might increase EOD and LOD GBS disease rates in HIV-exposed neonates
Compromised immunity
Low maternal GBS-specific antibody concentrations have been shown to be correlated with susceptibility of neonates for GBS EOD and LOD83,84,85. Some important observations show that these protective antibodies are reduced in HIV-exposed neonates and HIV-infected mothers. Significantly lower GBS-specific antibody concentrations were measured in maternal/cord blood from HIV-infected mothers and neonates born from HIV-infected mothers34,86. Furthermore, a reduced transplacental transfer of GBS-specific antibodies has been shown in HIV-infected mothers34,86. In addition, the neonatal anti-GBS antibodies remained significantly lower at 16 weeks86. Le Doare and co-workers demonstrated a significantly lower antibody-mediated C3b/iC3b deposition on all investigated GBS serotypes (Ia, Ib, II, III and V) in HIV-infected women and neonates born to HIV-infected women, suggesting a reduced opsonophagocytotic immune effector function86. A recent phase 2 GBS vaccination trial (with a trivalent vaccine consisting of conjugated capsular polysaccharides of GBS serotypes Ia, Ib and III) in African HIV-positive and HIV-negative pregnant women showed that the vaccine was less immunogenic in HIV-infected women, irrespective of their CD4 count87.
Other perturbations of the immune system of HIV-infected women (even in the absence of overt immune dysfunction) might also play an important role. HIV-infected women were shown to have reduced transplacental transfer of hematopoietic cytokines. This may result in lower thymic output of CD4+ cells in their infants and a delay in immune cell maturation17. Furthermore, intrauterine exposure to HIV or its soluble products appears to cause a disturbed thymic function in HIV-uninfected newborns88.
Anti-retroviral therapy (ART)
ART, used to prevent mother-to-child transmission of HIV, might play a role as well. Nucleoside reverse transcriptase inhibitors (NRTIs) crossing the placenta could cause mitochondrial dysfunction in HIV-exposed uninfected infants, explaining a decrease in neutrophils, total lymphocytes, CD4+ and CD8+ cells counts17.
Prematurity and (very)-low birth weight
Prematurity and (very)-low birth weight are more prevalent in neonates born to HIV-infected mothers (reviewed in89) and both are risk factors for GBS EOD and GBS LOD90,91,92,93,94,95.
Factors that might increase or decrease early-onset GBS disease rates in HIV-exposed neonates: meta-analysis of the risk for rectovaginal GBS carriage in HIV-infected women
Because rectovaginal GBS carriage is a major risk factor for early-onset neonatal GBS disease, we also assessed the risk for rectovaginal GBS carriage in HIV-infected women.
Our meta-analysis, based on 13 studies, did not show an association between HIV infection and rectovaginal GBS carriage, but most of the studies suffered from major limitations and we consider the currently available evidence weak and call for further study.
Few studies had adequate statistical power and few were designed to assess the association between HIV infection and rectovaginal GBS carriage. Most studies were at medium or high risk of bias related to representativeness of study groups, comparability of study groups, and/or outcome assessment.
Heterogeneity was considerable. Technical biases, such as the specimen collection and culture methods are likely to contribute substantially to this heterogeneity. For example, rectovaginal sampling has been shown to yield significantly higher recovery rates compared to vaginal sampling alone96,97. Furthermore, the use of a selective enrichment broth has been shown to improve GBS detection substantially96,98. However, rectovaginal sampling and the use of a selective enrichment broth, both recommended by the CDC, were used by only five studies. Also, the different study populations and eligibility criteria are likely to contribute to the observed heterogeneity.
Some important possible confounding factors were not taken into account. First, as described above, the use of antibiotic prophylaxis in HIV positive women, recommended by the WHO48, might be responsible for lower GBS rectovaginal carriage rates in HIV-infected pregnant women but was only taken into account in few studies. Secondly, none of the studies corrected for bacterial vaginosis (BV), a disturbance of the vaginal microbiome characterised by the deprivation of lactobacilli and the presence of anaerobes such as Gardnerella vaginalis and Atopobium vaginae. BV has been shown to be a risk factor for the acquisition of HIV99 but also to be negatively associated with vaginal GBS carriage49,100. Although speculatively, this might mask an association between HIV and GBS.
Finally, risk factors for early-onset GBS disease such as urinary tract infections and intrapartum fever have been reported to be more prevalent in HIV-infected women but were considered only by Cutland et al.35.
As the risk for EOD increases with heavier vaginal GBS colonization at the onset of labor or rupture of membranes101, future studies should also include quantitative molecular tests such as GBS-specific qPCR to determine the vaginal GBS load in relation to the HIV status. Furthermore, including the assessment of GBS serotype/genotype distribution in HIV-positive and –negative women will document whether more virulent GBS strains are present in HIV-positive women.
In conclusion, the evidence that HIV-exposed infants are at increased risk for late-onset GBS neonatal disease is accumulating. A compromised immune system, a neonatal gut microbiome dysbiosis, a lesser tendency to breastfeed but higher tendency for cesarean section and the use of prophylactic antibiotics in HIV-positive women might partly explain these findings. Public health interventions to prevent LOD are urgently needed in neonates born to HIV-infected mothers, even if themselves uninfected, and promoting feeding strategies such as breastfeeding or the use of probiotics and prebiotics have been shown to be exciting options to prevent69,81,82,102.
While we did not find evidence for an increased risk of rectovaginal GBS colonization in HIV-infected women, most studies conducted to date suffered major limitations. Further well-designed studies incorporating sensitive, quantitative (and serotype specific) GBS detection methods may further clarify the relation between HIV-positivity and GBS carriage.
References
Lawn, J. E., Cousens, S., Zupan, J. & Lancet Neonatal Survival Steering, T. 4 million neonatal deaths: when? Where? Why? Lancet 365, 891–900, https://doi.org/10.1016/S0140-6736(05)71048-5 (2005).
Hornik, C. P. et al. Early and late onset sepsis in very-low-birth-weight infants from a large group of neonatal intensive care units. Early Hum Dev 88(Suppl 2), S69–74, https://doi.org/10.1016/S0378-3782(12)70019-1 (2012).
Schuchat, A. Epidemiology of group B streptococcal disease in the United States: shifting paradigms. Clin Microbiol Rev 11, 497–513 (1998).
Stoll, B. J. et al. Early onset neonatal sepsis: the burden of group B Streptococcal and E. coli disease continues. Pediatrics 127, 817–826, https://doi.org/10.1542/peds.2010-2217 (2011).
Dillon, H. C. Jr, Khare, S. & Gray, B. M. Group B streptococcal carriage and disease: a 6-year prospective study. J Pediatr 110, 31–36 (1987).
Yancey, M. K. et al. Peripartum infection associated with vaginal group B streptococcal colonization. Obstet Gynecol 84, 816–819 (1994).
Temmerman, M. et al. The role of maternal syphilis, gonorrhoea and HIV-1 infections in spontaneous abortion. Int J STD AIDS 3, 418–422 (1992).
McDonald, H. M. & Chambers, H. M. Intrauterine infection and spontaneous midgestation abortion: is the spectrum of microorganisms similar to that in preterm labor? Infect Dis Obstet Gynecol 8, 220–227, https://doi.org/10.1155/S1064744900000314 (2000).
Allen, U. et al. Relationship between antenatal group B streptococcal vaginal colonization and premature labour. Paediatr Child Health 4, 465–469 (1999).
Regan, J. A. et al. Colonization with group B streptococci in pregnancy and adverse outcome. VIP Study Group. Am J Obstet Gynecol 174, 1354–1360 (1996).
Matorras, R. et al. Group B streptococcus and premature rupture of membranes and preterm delivery. Gynecol Obstet Invest 27, 14–18 (1989).
Acosta, C. D. et al. Severe maternal sepsis in the UK, 2011–2012: a national case-control study. PLoS Med 11, e1001672, https://doi.org/10.1371/journal.pmed.1001672 (2014).
Koenig, J. M. & Keenan, W. J. Group B streptococcus and early-onset sepsis in the era of maternal prophylaxis. Pediatr Clin North Am 56, 689–708, Table of Contents, https://doi.org/10.1016/j.pcl.2009.04.003 (2009).
Beck, S. et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ 88, 31–38, https://doi.org/10.2471/BLT.08.062554 (2010).
Khan, K. S., Wojdyla, D., Say, L., Gulmezoglu, A. M. & Van Look, P. F. WHO analysis of causes of maternal death: a systematic review. Lancet 367, 1066–1074, https://doi.org/10.1016/S0140-6736(06)68397-9 (2006).
Madhi, S. A. et al. Primary isoniazid prophylaxis against tuberculosis in HIV-exposed children. N Engl J Med 365, 21–31, https://doi.org/10.1056/NEJMoa1011214 (2011).
Epalza, C. et al. High incidence of invasive group B streptococcal infections in HIV-exposed uninfected infants. Pediatrics 126, e631–638, https://doi.org/10.1542/peds.2010-0183 (2010).
Spear, G. T. et al. Comparison of the diversity of the vaginal microbiota in HIV-infected and HIV-uninfected women with or without bacterial vaginosis. J Infect Dis 198, 1131–1140, https://doi.org/10.1086/591942 (2008).
Schellenberg, J. J. et al. Molecular definition of vaginal microbiota in East African commercial sex workers. Appl Environ Microbiol 77, 4066–4074, https://doi.org/10.1128/AEM.02943-10 (2011).
Jespers, V. et al. The significance of Lactobacillus crispatus and L. vaginalis for vaginal health and the negative effect of recent sex: a cross-sectional descriptive study across groups of African women. BMC Infect Dis 15, 115, https://doi.org/10.1186/s12879-015-0825-z (2015).
McHardy, I. H. et al. HIV Infection is associated with compositional and functional shifts in the rectal mucosal microbiota. Microbiome 1, 26, https://doi.org/10.1186/2049-2618-1-26 (2013).
Dillon, S. M. et al. An altered intestinal mucosal microbiome in HIV-1 infection is associated with mucosal and systemic immune activation and endotoxemia. Mucosal Immunol 7, 983–994, https://doi.org/10.1038/mi.2013.116 (2014).
Weiss, H. A. et al. The epidemiology of HSV-2 infection and its association with HIV infection in four urban African populations. AIDS 15(Suppl 4), S97–108 (2001).
Vandepitte, J. et al. Prevalence and correlates of Mycoplasma genitalium infection among female sex workers in Kampala, Uganda. J Infect Dis 205, 289–296, https://doi.org/10.1093/infdis/jir733 (2012).
Mitima, K. T. et al. Prevalence of colonization by Streptococcus agalactiae among pregnant women in Bukavu, Democratic Republic of the Congo. J Infect Dev Ctries 8, 1195–1200, https://doi.org/10.3855/jidc.5030 (2014).
El Beitune, P. et al. Group B Streptococcus carriers among HIV-1 infected pregnant women: Prevalence and risk factors. European Journal of Obstetrics Gynecology and Reproductive Biology 128, 54–58 (2006).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6, e1000097, https://doi.org/10.1371/journal.pmed.1000097 (2009).
Wells, G. A. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. (2013).
Higgins, J. P. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928, https://doi.org/10.1136/bmj.d5928 (2011).
Higgins, J. P. T. & Green, S. Cochrane handbook for systematic reviews of interventions version. (2011).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–1101 (1994).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 (1997).
Dangor, Z. et al. Burden of invasive group B Streptococcus disease and early neurological sequelae in South African infants. PLoS One 10, e0123014, https://doi.org/10.1371/journal.pone.0123014 (2015).
Dangor, Z. et al. HIV-1 Is Associated With Lower Group B Streptococcus Capsular and Surface-Protein IgG Antibody Levels and Reduced Transplacental Antibody Transfer in Pregnant Women. J Infect Dis 212, 453–462, https://doi.org/10.1093/infdis/jiv064 (2015).
Cutland, C. L. et al. Maternal HIV infection and vertical transmission of pathogenic bacteria. Pediatrics 130, e581–590, https://doi.org/10.1542/peds.2011-1548 (2012).
Cutland, C. L. et al. Increased Risk for Group B Streptococcus Sepsis in Young Infants Exposed to HIV, Soweto, South Africa, 2004-2008. Emerging Infectious Diseases 21, 638–645, https://doi.org/10.3201/eid2104.141562 (2015).
Frigati, L. et al. A retrospective review of group B streptococcal infection in the Metro East area of the Western Cape province: 2010 to 2011. Southern African Journal of Epidemiology and Infection 29, 33–36 (2014).
Djigma, F. et al. HIV-infected women of Burkina Faso: a “reservoir” of mycoplasma infection. Journal of Infection in Developing Countries 5, 176–181 (2011).
Ernest, A. I. et al. Maternal vaginorectal colonization by Group B Streptococcus and Listeria monocytogenes and its risk factors among pregnant women attending tertiary hospital in Mwanza, Tanzania. Tanzania Journal of Health Research 17 (2015).
Gray, K. J. et al. Group B Streptococcus and HIV infection in pregnant women, Malawi, 2008–2010. Emerg Infect Dis 17, 1932–1935, https://doi.org/10.3201/eid1710.102008 (2011).
Joachim, A. et al. Maternal and neonatal colonisation of group B streptococcus at Muhimbili National Hospital in Dar es Salaam, Tanzania: prevalence, risk factors and antimicrobial resistance. BMC Public Health 9, 437, https://doi.org/10.1186/1471-2458-9-437 (2009).
Mavenyengwa, R. T., Moyo, S. R. & Nordbø, S. A. Streptococcus agalactiae colonization and correlation with HIV-1 and HBV seroprevalence in pregnant women from Zimbabwe. European Journal of Obstetrics Gynecology and Reproductive Biology 150, 34–38 (2010).
Sebitloane, H. M., Moodley, J. & Esterhuizen, T. M. Pathogenic lower genital tract organisms in HIV-infected and uninfected women, and their association with postpartum infectious morbidity. S Afr Med J 101, 466–469 (2011).
Shah, M., Aziz, N., Leva, N. & Cohan, D. Group B Streptococcus colonization by HIV status in pregnant women: prevalence and risk factors. J Womens Health (Larchmt) 20, 1737–1741, https://doi.org/10.1089/jwh.2011.2888 (2011).
Ulla, M. et al. Sexually transmitted diseases in a high risk subpopulation from the province of Soria. Enferm Infecc Microbiol Clin 11, 299–303 (1993).
Sterne, J. A. et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343, d4002, https://doi.org/10.1136/bmj.d4002 (2011).
Afran, L. et al. HIV-exposed uninfected children: a growing population with a vulnerable immune system? Clin Exp Immunol 176, 11–22, https://doi.org/10.1111/cei.12251 (2014).
WHO. Guidelines on co-trimoxazole prophylaxis for HIV-related infections among children, adolescents and adults in resource-limited settings. (2006).
Cools, P. et al. A Multi-Country Cross-Sectional Study of Vaginal Carriage of Group B Streptococci (GBS) and Escherichia coli in Resource-Poor Settings: Prevalences and Risk Factors. PLoS One 11, e0148052, https://doi.org/10.1371/journal.pone.0148052 (2016).
Seale, A. C. et al. Maternal colonization with Streptococcus agalactiae and associated stillbirth and neonatal disease in coastal Kenya. Nat Microbiol 1, 16067, https://doi.org/10.1038/nmicrobiol.2016.67 (2016).
Chama, C. M. & Morrupa, J. Y. The safety of elective caesarean section for the prevention of mother-to-child transmission of HIV-1. J Obstet Gynaecol 28, 194–197, https://doi.org/10.1080/01443610801912295 (2008).
Jamieson, D. J. et al. Cesarean delivery for HIV-infected women: recommendations and controversies. Am J Obstet Gynecol 197, S96–100, https://doi.org/10.1016/j.ajog.2007.02.034 (2007).
Veerendra Mehar, S. A., Singh, R., Agarwal, A., Agrawal, N. & Majethia, A. Relationship between gestational age and mode of delivery with neonatal septicemia. International Journal of Contemporary Pediatrics 3, 891–895 (2016).
Hook, B., Kiwi, R., Amini, S. B., Fanaroff, A. & Hack, M. Neonatal morbidity after elective repeat cesarean section and trial of labor. Pediatrics 100, 348–353 (1997).
Aishat, U., Olufunmilayo, F., David, D. & Gidado, S. Factors Influencing Infant Feeding Choices of HIV Positive Mothers in Southwestern, Nigeria. American Journal of Public Health Research 3, 72–79 (2015).
Lunney, K. M. et al. HIV-positive poor women may stop breast-feeding early to protect their infants from HIV infection although available replacement diets are grossly inadequate. J Nutr 138, 351–357 (2008).
Kuhn, L. et al. Elevations in mortality associated with weaning persist into the second year of life among uninfected children born to HIV-infected mothers. Clin Infect Dis 50, 437–444, https://doi.org/10.1086/649886 (2010).
Slater, M., Stringer, E. M. & Stringer, J. S. Breastfeeding in HIV-positive women: What can be recommended? Paediatr Drugs 12, 1–9, https://doi.org/10.2165/11316130-000000000-00000 (2010).
Haile, D. S. T. & Biadgilign, S. Adherence to WHO breastfeeding guidelines among HIV positive mothers in Southern Ethiopia. Pediatric Health, Medicine and Therapeutics 6, 87–92 (2015).
Sadoh, W. E., Sadoh, A. E., Adeniran, K. A. & Abhulimhen-Iyoha, B. I. Infant-feeding practices among HIV-infected mothers in an HIV-treatment programme. J Health Popul Nutr 26, 463–467 (2008).
Adejuyigbe, E., Orji, E., Onayade, A., Makinde, N. & Anyabolu, H. Infant feeding intentions and practices of HIV-positive mothers in southwestern Nigeria. J Hum Lact 24, 303–310, https://doi.org/10.1177/0890334408317765 (2008).
Weisman, L. E. & Dobson, F. M. The potential impact of group B streptococcal antibodies in breast milk. Adv Exp Med Biol 310, 345–351 (1991).
Challacombe, S. J. & Sweet, S. P. Salivary and mucosal immune responses to HIV and its co-pathogens. Oral Dis 3(Suppl 1), S79–84 (1997).
Pacheco, A. R., Barile, D., Underwood, M. A. & Mills, D. A. The impact of the milk glycobiome on the neonate gut microbiota. Annu Rev Anim Biosci 3, 419–445, https://doi.org/10.1146/annurev-animal-022114-111112 (2015).
Thior, I. et al. Breastfeeding plus infant zidovudine prophylaxis for 6 months vs formula feeding plus infant zidovudine for 1 month to reduce mother-to-child HIV transmission in Botswana: a randomized trial: the Mashi Study. JAMA 296, 794–805, https://doi.org/10.1001/jama.296.7.794 (2006).
Alvarez-Uria, G., Midde, M., Pakam, R., Bachu, L. & Naik, P. K. Effect of Formula Feeding and Breastfeeding on Child Growth, Infant Mortality, and HIV Transmission in Children Born to HIV-Infected Pregnant Women Who Received Triple Antiretroviral Therapy in a Resource-Limited Setting: Data from an HIV Cohort Study in India. ISRN Pediatr 2012, 763591, https://doi.org/10.5402/2012/763591 (2012).
Berrington, J. E., Stewart, C. J., Cummings, S. P. & Embleton, N. D. The neonatal bowel microbiome in health and infection. Curr Opin Infect Dis 27, 236–243, https://doi.org/10.1097/QCO.0000000000000061 (2014).
Wardwell, L. H., Huttenhower, C. & Garrett, W. S. Current concepts of the intestinal microbiota and the pathogenesis of infection. Curr Infect Dis Rep 13, 28–34, https://doi.org/10.1007/s11908-010-0147-7 (2011).
Sherman, M. P. New concepts of microbial translocation in the neonatal intestine: mechanisms and prevention. Clin Perinatol 37, 565–579, https://doi.org/10.1016/j.clp.2010.05.006 (2010).
Groer, M. W. et al. Development of the preterm infant gut microbiome: a research priority. Microbiome 2, 38, https://doi.org/10.1186/2049-2618-2-38 (2014).
Carl, M. A. et al. Sepsis from the gut: the enteric habitat of bacteria that cause late-onset neonatal bloodstream infections. Clin Infect Dis 58, 1211–1218, https://doi.org/10.1093/cid/ciu084 (2014).
Madan, J. C. et al. Gut microbial colonisation in premature neonates predicts neonatal sepsis. Arch Dis Child Fetal Neonatal Ed 97, F456–462, https://doi.org/10.1136/fetalneonatal-2011-301373 (2012).
Mueller, N. T., Bakacs, E., Combellick, J., Grigoryan, Z. & Dominguez-Bello, M. G. The infant microbiome development: mom matters. Trends Mol Med 21, 109–117, https://doi.org/10.1016/j.molmed.2014.12.002 (2015).
Dominguez-Bello, M. G. et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci USA 107, 11971–11975, https://doi.org/10.1073/pnas.1002601107 (2010).
Rutayisire, E., Huang, K., Liu, Y. & Tao, F. The mode of delivery affects the diversity and colonization pattern of the gut microbiota during the first year of infants’ life: a systematic review. BMC Gastroenterol 16, 86, https://doi.org/10.1186/s12876-016-0498-0 (2016).
Jaureguy, F. et al. Effects of intrapartum penicillin prophylaxis on intestinal bacterial colonization in infants. J Clin Microbiol 42, 5184–5188, https://doi.org/10.1128/JCM.42.11.5184-5188.2004 (2004).
Kuppala, V. S., Meinzen-Derr, J., Morrow, A. L. & Schibler, K. R. Prolonged initial empirical antibiotic treatment is associated with adverse outcomes in premature infants. J Pediatr 159, 720–725, https://doi.org/10.1016/j.jpeds.2011.05.033 (2011).
Bezirtzoglou, E., Tsiotsias, A. & Welling, G. W. Microbiota profile in feces of breast- and formula-fed newborns by using fluorescence in situ hybridization (FISH). Anaerobe 17, 478–482, https://doi.org/10.1016/j.anaerobe.2011.03.009 (2011).
Westerbeek, E. A. et al. The intestinal bacterial colonisation in preterm infants: a review of the literature. Clin Nutr 25, 361–368, https://doi.org/10.1016/j.clnu.2006.03.002 (2006).
Schanler, R. J., Lau, C., Hurst, N. M. & Smith, E. O. Randomized trial of donor human milk versus preterm formula as substitutes for mothers’ own milk in the feeding of extremely premature infants. Pediatrics 116, 400–406, https://doi.org/10.1542/peds.2004-1974 (2005).
Schanler, R. J., Shulman, R. J. & Lau, C. Feeding strategies for premature infants: beneficial outcomes of feeding fortified human milk versus preterm formula. Pediatrics 103, 1150–1157 (1999).
Hylander, M. A., Strobino, D. M. & Dhanireddy, R. Human milk feedings and infection among very low birth weight infants. Pediatrics 102, E38 (1998).
Baker, C. J. & Kasper, D. L. Correlation of maternal antibody deficiency with susceptibility to neonatal group B streptococcal infection. N Engl J Med 294, 753–756, https://doi.org/10.1056/NEJM197604012941404 (1976).
Baker, C. J., Edwards, M. S. & Kasper, D. L. Role of antibody to native type III polysaccharide of group B Streptococcus in infant infection. Pediatrics 68, 544–549 (1981).
Baker, C. J. et al. Maternal antibody at delivery protects neonates from early onset group B streptococcal disease. J Infect Dis 209, 781–788, https://doi.org/10.1093/infdis/jit549 (2014).
Le Doare, K. et al. Anti-group B Streptococcus antibody in infants born to mothers with human immunodeficiency virus (HIV) infection. Vaccine 33, 621–627, https://doi.org/10.1016/j.vaccine.2014.12.025 (2015).
Heyderman, R. S. et al. Group B streptococcus vaccination in pregnant women with or without HIV in Africa: a non-randomised phase 2, open-label, multicentre trial. Lancet Infect Dis 16, 546–555, https://doi.org/10.1016/S1473-3099(15)00484-3 (2016).
Clerici, M. et al. T-lymphocyte maturation abnormalities in uninfected newborns and children with vertical exposure to HIV. Blood 96, 3866–3871 (2000).
Xiao, P. L. et al. Association between maternal HIV infection and low birth weight and prematurity: a meta-analysis of cohort studies. BMC Pregnancy Childbirth 15, 246, https://doi.org/10.1186/s12884-015-0684-z (2015).
Adair, C. E. et al. Risk factors for early-onset group B streptococcal disease in neonates: a population-based case-control study. CMAJ 169, 198–203 (2003).
Lin, F. Y., Weisman, L. E., Troendle, J. & Adams, K. Prematurity is the major risk factor for late-onset group B streptococcus disease. J Infect Dis 188, 267–271, https://doi.org/10.1086/376457 (2003).
Benitz, W. E., Gould, J. B. & Druzin, M. L. Risk factors for early-onset group B streptococcal sepsis: estimation of odds ratios by critical literature review. Pediatrics 103, e77 (1999).
Stoll, B. J. et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 110, 285–291 (2002).
Berardi, A. et al. Group B streptococcus late-onset disease: 2003–2010. Pediatrics 131, e361–368, https://doi.org/10.1542/peds.2012-1231 (2013).
Shane, A. L. & Stoll, B. J. Neonatal sepsis: progress towards improved outcomes. J Infect 68(Suppl 1), S24–32, https://doi.org/10.1016/j.jinf.2013.09.011 (2014).
El Aila, N. A. et al. Comparison of different sampling techniques and of different culture methods for detection of group B streptococcus carriage in pregnant women. BMC Infect Dis 10, 285, https://doi.org/10.1186/1471-2334-10-285 (2010).
Dillon, H. C. Jr., Gray, E., Pass, M. A. & Gray, B. M. Anorectal and vaginal carriage of group B streptococci during pregnancy. J Infect Dis 145, 794–799 (1982).
Baker, C. J. et al. Vaginal colonization with group B streptococcus: a study in college women. J Infect Dis 135, 392–397 (1977).
Atashili, J., Poole, C., Ndumbe, P. M., Adimora, A. A. & Smith, J. S. Bacterial vaginosis and HIV acquisition: a meta-analysis of published studies. AIDS 22, 1493–1501, https://doi.org/10.1097/QAD.0b013e3283021a37 (2008).
Hillier, S. L., Krohn, M. A., Nugent, R. P. & Gibbs, R. S. Characteristics of three vaginal flora patterns assessed by gram stain among pregnant women. Vaginal Infections and Prematurity Study Group. Am J Obstet Gynecol 166, 938–944 (1992).
Verani, J. R. & Schrag, S. J. Group B streptococcal disease in infants: progress in prevention and continued challenges. Clin Perinatol 37, 375–392, https://doi.org/10.1016/j.clp.2010.02.002 (2010).
Aceti, A. et al. Probiotics Prevent Late-Onset Sepsis in Human Milk-Fed, Very Low Birth Weight Preterm Infants: Systematic Review and Meta-Analysis. Nutrients 9, https://doi.org/10.3390/nu9080904 (2017).
Acknowledgements
Piet Cools is supported by the Ghent University. Ghent University
Author information
Authors and Affiliations
Contributions
Designed the study protocol: P.C., T.C., V.J., E.S., J.V.D.W., M.V.; Performed the literature search: P.C.; Selection of papers: P.C., M.V.; Data extraction: P.C., T.C., V.J., E.S., J.V.D.W., M.V.; Performed the meta-analysis: J.V.D.W., P.C., V.J., T.C.; Quality assessment of studies: P.C., J.V.D.W., H.V.; Wrote the paper: P.C., T.C., V.J., E.S., J.V.D.W., H.V., M.V.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cools, P., van de Wijgert, J.H.H.M., Jespers, V. et al. Role of HIV exposure and infection in relation to neonatal GBS disease and rectovaginal GBS carriage: a systematic review and meta-analysis. Sci Rep 7, 13820 (2017). https://doi.org/10.1038/s41598-017-13218-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-13218-1
This article is cited by
-
The effects of exposure to HIV in neonates at a referral hospital in South Africa
BMC Pediatrics (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.