Abstract
Breast cancer (BC) is the leading cause of cancer death in women. Adipokines, and other inflammation molecules linked to adiposity, are suspected to be involved in breast carcinogenesis, however prospective findings are inconclusive. In a prospective nested case-control study within the EPIC-Varese cohort, we used conditional logistic regression to estimate rate ratios (RRs) for BC, with 95% confidence intervals (CI), in relation to plasma levels of C-reactive protein (CRP), tumor necrosis factor-alpha (TNF-α), interleukin-6, leptin, and adiponectin, controlling for BC risk factors. After a median 14.9 years, 351 BC cases were identified and matched to 351 controls. No marker was significantly associated with BC risk overall. Significant interactions between menopausal status and CRP, leptin, and adiponectin were found. Among postmenopausal women, high CRP was significantly associated with increased BC risk, and high adiponectin with significantly reduced risk. Among premenopausal women, high TNF-α was associated with significantly increased risk, and high leptin with reduced risk; interleukin-6 was associated with increased risk only in a continuous model. These findings constitute further evidence that inflammation plays a role in breast cancer. Interventions to lower CRP, TNF-α, and interleukin-6 and increase adiponectin levels may contribute to preventing BC.
Similar content being viewed by others
Introduction
Breast cancer is the commonest cancer and leading cause of cancer death in women worldwide, with an estimated 1.7 million cases and over 520,000 deaths in 2012, accounting for 25% of all female cancers and 15% of all female cancer deaths1.
As long ago as 1863, Rudolf Virchow proposed that cancers originate at sites of chronic inflammation2. It is now clear that chronic inflammation is associated with several human cancers and that pro-inflammatory cytokines and other immunomodulatory molecules can be produced by cells in cancerous tissue to favor tumor growth, infiltration and metastasis3. C-reactive protein (CRP), an acute-phase protein of hepatic origin that is a sensitive yet nonspecific marker of the inflammatory response, has been associated with breast cancer risk in some4,5,6,7 but not all studies6. Several adipokines (immunomodulatory proteins produced by adipose and other tissues) are also suspected to play a role in breast carcinogenesis8. In particular, altered levels of tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), adiponectin, and leptin have important roles in promoting inflammation in obesity and chronic inflammatory diseases9, and may play a role in carcinogenesis8,10. However prospective studies on markers of inflammation and breast cancer risk have produced conflicting results11,12,13.
We carried out a case-control study to prospectively assess whether pre-diagnostic levels of CRP, TNF-α, IL-6, leptin, and adiponectin in plasma are associated with risk of developing breast cancer.
Results
Baseline characteristics of cases and controls, by tertiles of plasma level of inflammatory biomarkers, are shown in Table 1. Women in the highest tertiles of all biomarkers tended to be older and have higher BMI (lower BMI for high adiponectin). Alcohol intake decreased with increasing adiponectin levels. Women in the highest tertiles were also less educated (not for increasing levels of adiponectin), less likely to be smokers (not for increasing levels of IL-6) or sometime oral contraceptive users, and more likely to be postmenopausal. Age at menarche was higher for increasing levels of CRP and IL-6. Lastly, while women with highest CRP levels were less likely to be nulliparous, the opposite was the case for women with highest adiponectin levels.
Table 2 shows RRs of developing breast cancer by tertiles of plasma markers. None of the markers was significantly associated with risk. Table 3 shows results for postmenopausal and premenopausal women separately. Significant interactions between menopausal status and plasma levels were found for CRP (tertiles model), leptin (tertiles and continuous models), and adiponectin (tertiles model).
Among postmenopausal women, high levels (third tertile) of CRP were associated with significantly increased risk (RR 2.42; 95% CI: 1.17–5.00) compared to the first tertile, fully-adjusted model; while high levels (third tertile) of adiponectin were associated with significantly reduced risk (RR 0.37; 95% CI: 0.19–0.72) compared to the first tertile, fully-adjusted model. None of the other biomarkers was significantly associated with breast cancer risk in postmenopausal women.
Among premenopausal women, high TNF-α was associated with significantly increased breast cancer risk in the tertile model only (P trend = 0.017); and high IL-6 was associated with increased risk in the continuous model only (RR 1.58; 95% CI: 1.02–2.46). By contrast, high plasma leptin was associated with significantly reduced risk, both in the tertile-based model (RR 0.43; 95% CI: 0.20–0.89, third vs. first tertile) and for a 1 standard deviation increase in leptin (RR 0.71; 95% CI: 0.50–0.99). None of the other biomarkers was significantly associated with breast cancer risk premenopausal women.
Discussion
In this nested case-control study, none of the inflammatory biomarkers analyzed was associated with breast cancer risk in the overall population. However, there were significant interactions between menopausal status and levels of CRP, leptin, and adiponectin. Among postmenopausal women, high CRP was associated with increased breast cancer risk, and high adiponectin was associated with decreased risk. And among premenopausal women, high TNF-α and IL-6 were associated with increased risk, and high leptin was associated with decreased risk.
Our finding of a direct association between plasma CRP and risk of postmenopausal breast cancer is in line with the findings of two recently published meta-analyses4,14. The first4, which examined 12 prospective studies, found that risk increased significantly by 7% overall and by 6% in postmenopausal women, for each doubling of CRP concentration. The other study14 analyzed 15 cohort and case-control studies, and included premenopausal women, finding that risk increased by 16% for each natural log unit increase in CRP; however when postmenopausal and premenopausal women were analyzed separately, the risk increase was significant only in postmenopausal women.
CRP is an established systemic marker of inflammation, being produced by the liver in response to cytokines (including IL-6 and TNF-α) produced by cells in inflamed tissue15,16. The lack of association between CRP and breast cancer risk in premenopausal women suggests that inflammation plays little or no role in premenopausal breast cancer.
However this conclusion is opposed by our finding that high TNF-α was associated with increased breast cancer risk in premenopausal women. Our finding, in fact, contrasts with the results of the only four prospective studies we are aware of to have investigated TNF-α and breast cancer risk12,17,18: three found no significant association between TNF-α and breast cancer; while a fourth case-control study on postmenopausal women nested in the Malmö Diet and Cancer Cohort19 found an association between high TNF-α and reduced breast cancer risk.
TNF-α is a major mediator of inflammation: its induction, for example by tissue damage, induces a cascade of other inflammatory cytokines, chemokines, growth factors and endothelial adhesins which recruit and activate a range of cells at the site of tissue damage to promote healing20,21. However, when produced chronically, TNF-α seems to act as a tumor promoter, contributing to the tissue remodeling and stromal development necessary for tumor growth and spread20,21. Recent data suggest that TNF-α is involved in carcinogenesis at least in part because it activates nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) (reviewed in22), which is responsible for inducing the expression of genes associated with cell proliferation, apoptosis, inflammation, metastasis, and angiogenesis23. TNF-α can also stimulate the activity of the inducible nitric oxide synthase (iNOS), which is implicated in cellular changes leading to malignancy (transformation of normal cells, growth of transformed cells, angiogenesis and metastasis of malignant cells24).
Although our finding that TNF-α is associated with increased breast cancer risk in premenopausal women is not supported by previous studies, the association could be real since TNF-α has been found to stimulate the enzymes of estrogen synthesis25. High TNF-α could therefore promote breast cancer by this mechanism, which is likely to be more important in premenopause − before the fall in estrogen synthesis heralded by the menopause.
We found that plasma IL-6 was associated with increased breast cancer risk among premenopausal women, but only in the continuous model. IL-6 has been reported to activate Janus kinase (JAK) and signal transducer and activator of transcription 3 (STAT3) pathways22 to promote a cellular microenvironment that may promote cancer growth. However, no association between increased IL-6 levels and breast cancer risk has been reported in previous studies, specifically the case-cohort study nested within the Women’s Health Initiative Observational Study12, the British Women’s Heart and Health Study cohort study and Caerphilly Cohort26, and the Health Aging and Body Composition prospective cohort study17.
The inverse association we found between plasma leptin and breast cancer risk in premenopausal women is supported by the findings of a case-control study by Harris et al.27 on premenopausal women. By contrast the case-control study of Touvier et al.13 found no association between leptin and breast cancer risk. Other prospective studies that investigated plasma leptin and breast cancer mainly involved postmenopausal women, and found no association12,28 or a direct association11,29. Leptin is thought to be involved in promoting breast cancer in obese women by stimulating the conversion of aromatizable androgens (androstenedione and dehydroepiandrosterone) to estradiol. This occurs not only in adipose but also in breast epithelial cells, particularly when levels of circulating estrogens decline, as they do in postmenopausal women30,31. This mechanism might explain why high leptin was associated with non-significantly increased breast cancer risk in our postmenopausal women, even after adjusting for BMI. However, in premenopausal women, high leptin may lower breast cancer risk, since leptin is involved in the regulation of ovarian folliculogenesis32 and at high levels may reduce follicular estradiol secretion33. Very high leptin levels have been reported in women with chronic anovulation34, a condition that may be associated with reduced breast cancer risk35.
As regards adiponectin, we found decreased breast cancer risk with increasing levels in postmenopausal women, in agreement with the findings of a 2013 meta-analysis that examined 17 observational studies (4 nested case-control studies and 9 case-control studies)36, and found no association of adiponectin with breast cancer risk overall, but decreased risk in postmenopausal women. A 2014 meta-analysis37 which examined 15 observational studies (6 prospective and 9 case-control studies), found a 5% reduction in overall breast cancer risk for 3 μg/ml increments in adiponectin, but no significant associations in post- or premenopausal women examined separately. A 2015 case-cohort study on postmenopausal women found no association between plasma adiponectin and breast cancer risk12. A 2016 meta-analysis of 107 epidemiological studies38 found that circulating adiponectin levels were lower in patients with various cancers than controls. However, other studies have found that increased adiponectin levels correlate with cancer progression (reviewed in39); and in patients with viral infections or chronic inflammation, increased levels of adiponectin predict cancer development39. Obesity is protective against breast cancer in premenopause but increases breast cancer risk in postmenopause. Adiponectin levels are low in obesity, so a presumed cancer-promoting effect of low adiponectin in premenopause may be masked by concomitant and protective obesity. In postmenopause, obesity is not protective so low levels of adiponectin may be “freed” to exert a cancer promoting effect, possibly explaining our finding that high adiponectin was associated with lowered breast cancer risk in postmenopausal women only40.
Strengths of our study are its prospective design, relatively large sample size, and availability of detailed information on lifestyle that made it possible to control for confounding effects. A limitation is that we assessed variables at baseline only and do not know to what extent they may have changed subsequently. Limited data indicate that adipokine levels in a single blood sample are useful biomarkers of inflammation in population-based studies41.
Another limitation is that the relation between the circulating levels of the biomarkers we examined and their activity in breast or adipose is unknown, and it is possible that plasma levels may be a poor surrogate for local activity. For example leptin and adiponectin seem to function primarily in a paracrine manner, so circulating levels are unlikely to reflect biological activity in the breast42. Another possible limitation is that samples were collected, stored at −196 °C, and analyzed up to 20 years later. There may have been differential decay of the analytes over that period43,44. However, unless analyte decay varied with initial concentration (which seems unlikely), this will not bias analyte-risk associations.
To conclude, the findings of this case-control study nested in the EPIC-Varese cohort suggest that high levels of CRP and low levels of adiponectin may increase the risk of postmenopausal breast cancer, while high levels of TNF-α and IL-6, and low levels of leptin may increase breast cancer risk among premenopausal women. Further research is required to elucidate the mechanisms by which leptin can influence the etiology of premenopausal breast cancer; interventions to lower CRP and increase adiponectin levels might help reduce the risk of developing postmenopausal breast cancer, while interventions to lower TNF-α and IL-6 levels might help reduce the risk of developing premenopausal breast cancer.
Methods
Study population and data collection
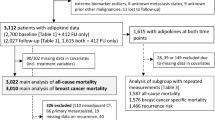
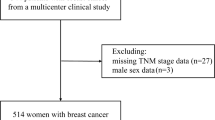
The case-control study was nested within the 9378 women, resident in Varese Province, northern Italy, who were recruited in 1992-1997 (age 35–69 years) to the European Prospective Investigation into Cancer and Nutrition (EPIC)-Varese study, and gave blood samples on recruitment.
At baseline, detailed information was collected on reproductive and medical history, physical activity, alcohol consumption, smoking, education, and socioeconomic variables, using a standardized lifestyle questionnaire. Diet over the previous year was investigated using a food frequency questionnaire specifically developed to capture local dietary habits. Weight, height, and blood pressure were measured, and a 30 mL fasting blood sample was collected. The blood samples were divided into 0.5 mL aliquots of plasma, serum, red blood cells, and buffy coat, on the day of collection, and stored in liquid nitrogen at −196 °C45.
Ethics Statement
The study protocol was approved by the ethics committee of the Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, Italy. At baseline, participants signed a written informed consent to use clinical data for research. Consent forms were stored with barcode ID for subject identification. The ethics committee approved this consent procedure. The study protocol and informed consent procedure met the requirements of Italian legislation and the Declaration of Helsinki of 1975, as revised in 2008.
Breast cancer cases and selection of control women
The women were followed-up to December 31, 2009 (median 14.9 years), through the Varese section of the Lombardy Cancer Registry, characterized by high data completeness and quality. A total of 362 new breast cancers was identified.
For each case, one matched control was chosen, using an incidence density sampling protocol, from appropriate risk sets consisting of cohort members alive and free of cancer at the time of diagnosis of the index case. Matching criteria were age at recruitment (±5 years), date of recruitment (±180 days), menopausal status (postmenopausal, premenopausal, and perimenopausal at baseline), and analysis of inflammatory markers in the same batch.
Analysis of plasma samples
Plasma samples were analyzed using Luminex multiplex technology, which determines multiple analytes in a single microwell plate, using antibody kits purchased from Bio-Rad (Bio-Plex, TNF-α, IL-6, leptin, and adiponectin) or Merck (CRP)46. All the analyses were performed in duplicated and results with a intra-assay %CV > 20% were discarded. The contents of each well were read by Bio-Plex 100 System array reader (Bio-Rad Laboratories, California, USA), which identifies and quantifies each analyte based on bead color and fluorescent signal intensity. Instrument calibration procedure was performed daily by Bio-Plex Calibration Kit (Bio-Rad) for optimal performance and reproducibility of results. The data were processed using Bio-Plex Manager software (version 6.1) using five-parametric curve fitting and converted to pg/ml.
All kits supplied lyophilized standards that were reconstituted and diluted at 7 serial concentrations following manufacturer’s instructions (standard curves). Standards included all recombinant proteins tested and were considered as positive controls for the procedure. Standard diluent buffers alone were used as negative controls.
Statistical methods
Plasma levels of inflammatory molecules were grouped into tertiles based on the distribution in controls. Baseline characteristics of cases and controls, according to tertiles of plasma inflammatory biomarkers, were summarized as means and standard deviations (continuous variables) or frequencies (categorical variables). Conditional logistic regression models were used to estimate rate ratios (RRs) for breast cancer with 95% confidence intervals (CIs), with lowest tertile as reference. The significance of linear trends was assessed by treating each tertile as a continuous variable in the model and performing the Wald test. RRs were also calculated for 1 standard deviation increments in plasma concentration as a continuous variable. We ran a minimally adjusted model, adjusted for age (continuous) and BMI (<25 kg/m2, 25- < 30 kg/m2, ≥30 kg/m2), and a fully-adjusted model, with the following additional covariates: age at menarche (<15 years, ≥15 years), parity (nulliparous, 1–2 children, >2 children), oral contraceptive use (never, sometime), education (≤8 years, >8 years), smoking status (never, former, current), and alcohol consumption (continuous).
We analyzed all women, and postmenopausal and premenopausal women separately. P values for interaction of inflammatory markers with menopausal status were estimated by adding the product of tertile of plasma concentrations and menopausal status to the model and applying the Wald test.
We excluded seven cases and their matched controls because a plasma sample was not available for the case or the control. We excluded four additional cases and controls because confounder variables were missing for the case or control. The analyses were therefore performed on 351 cases and 351 matched controls, total 702 women – 334 postmenopausal, 360 premenopausal, and 8 perimenopausal. All statistical tests were two-sided, differences were considered significant for P < 0.05. The analyses were performed with Stata version 14.0 (College Station, TX, USA).
Data availability
The data that support the findings of this study are held by the corresponding author, however their availability is restricted: for ethical reasons, the Ethical Committee does not allow open/public sharing of data pertaining to individuals. However aggregated data are available to other researchers, upon request.
References
Torre, L. A. et al. Global cancer statistics, 2012. CA Cancer J. Clin. 65, 87–108 (2015).
Coussens, L. M. & Werb, Z. Inflammation and cancer. Nature 420, 860–867 (2002).
Crusz, S. M. & Balkwill, F. R. Inflammation and cancer: advances and new agents. Nat. Rev. Clin. Oncol. 12, 584–596 (2015).
Chan, D. S., Bandera, E. V., Greenwood, D. C. & Norat, T. Circulating C-Reactive Protein and Breast Cancer Risk-Systematic Literature Review and Meta-analysis of Prospective Cohort Studies. Cancer Epidemiol. Biomarkers Prev. 24, 1439–1449 (2015).
Frydenberg, H. et al. Pre-diagnostic high-sensitive C-reactive protein and breast cancer risk, recurrence, and survival. Breast Cancer Res. Treat. 155, 345–354 (2016).
Wang, G. et al. A prospective follow-up study of the relationship between C-reactive protein and human cancer risk in the Chinese Kailuan Female Cohort. Cancer Epidemiol. Biomarkers Prev. 24, 459–465 (2015).
Wulaningsih, W. et al. Prediagnostic serum inflammatory markers in relation to breast cancer risk, severity at diagnosis and survival in breast cancer patients. Carcinogenesis 36, 1121–1128 (2015).
van Kruijsdijk, R. C., van der, W. E. & Visseren, F. L. Obesity and cancer: the role of dysfunctional adipose tissue. Cancer Epidemiol. Biomarkers Prev. 18, 2569–2578 (2009).
Fantuzzi, G. Adipose tissue, adipokines, and inflammation. J. Allergy Clin. Immunol. 115, 911–919 (2005).
Rose, D. P. & Vona-Davis, L. Biochemical and molecular mechanisms for the association between obesity, chronic inflammation, and breast cancer. Biofactors 40, 1–12 (2014).
Gross, A. L., Newschaffer, C. J., Hoffman-Bolton, J., Rifai, N. & Visvanathan, K. Adipocytokines, inflammation, and breast cancer risk in postmenopausal women: a prospective study. Cancer Epidemiol. Biomarkers Prev. 22, 1319–1324 (2013).
Gunter, M. J. et al. Circulating Adipokines and Inflammatory Markers and Postmenopausal Breast Cancer Risk. J. Natl. Cancer Inst. 107, (2015).
Touvier, M. et al. Association between prediagnostic biomarkers of inflammation and endothelial function and cancer risk: a nested case-control study. Am. J. Epidemiol. 177, 3–13 (2013).
Guo, L. et al. C-reactive protein and risk of breast cancer: A systematic review and meta-analysis. Sci. Rep. 5, 10508 (2015).
Volanakis, J. E. Human C-reactive protein: expression, structure, and function. Mol. Immunol. 38, 189–197 (2001).
Gauldie, J. et al. Interferon beta 2/B-cell stimulatory factor type 2 shares identity with monocyte-derived hepatocyte-stimulating factor and regulates the major acute phase protein response in liver cells. Proc. Natl. Acad. Sci. USA 84, 7251–7255 (1987).
Il'yasova, D. et al. Circulating levels of inflammatory markers and cancer risk in the health aging and body composition cohort. Cancer Epidemiol. Biomarkers Prev. 14, 2413–2418 (2005).
Krajcik, R. A., Massardo, S. & Orentreich, N. No association between serum levels of tumor necrosis factor-alpha (TNF-alpha) or the soluble receptors sTNFR1 and sTNFR2 and breast cancer risk. Cancer Epidemiol. Biomarkers Prev. 12, 945–946 (2003).
Dias, J. A. et al. Low-Grade Inflammation, Oxidative Stress and Risk of Invasive Post-Menopausal Breast Cancer - A Nested Case-Control Study from the Malmo Diet and Cancer Cohort. PLoS. One. 11, e0158959 (2016).
Balkwill, F. & Mantovani, A. Inflammation and cancer: back to Virchow? Lancet 357, 539–545 (2001).
Balkwill, F. Tumor necrosis factor or tumor promoting factor? Cytokine Growth Factor Rev. 13, 135–141 (2002).
Prieto-Hontoria, P. L. et al. Role of obesity-associated dysfunctional adipose tissue in cancer: a molecular nutrition approach. Biochim. Biophys. Acta 1807, 664–678 (2011).
Karin, M. Nuclear factor-kappaB in cancer development and progression. Nature 441, 431–436 (2006).
Geller, D. A. & Billiar, T. R. Molecular biology of nitric oxide synthases. Cancer Metastasis Rev. 17, 7–23 (1998).
Purohit, A., Newman, S. P. & Reed, M. J. The role of cytokines in regulating estrogen synthesis: implications for the etiology of breast cancer. Breast Cancer Res. 4, 65–69 (2002).
Heikkila, K. et al. Associations of circulating C-reactive protein and interleukin-6 with cancer risk: findings from two prospective cohorts and a meta-analysis. Cancer Causes Control 20, 15–26 (2009).
Harris, H. R., Tworoger, S. S., Hankinson, S. E., Rosner, B. A. & Michels, K. B. Plasma leptin levels and risk of breast cancer in premenopausal women. Cancer Prev. Res. (Phila) 4, 1449–1456 (2011).
Stattin, P. et al. Plasma leptin and breast cancer risk: a prospective study in northern Sweden. Breast Cancer Res. Treat. 86, 191–196 (2004).
Ollberding, N. J. et al. Prediagnostic leptin, adiponectin, C-reactive protein, and the risk of postmenopausal breast cancer. Cancer Prev. Res. (Phila) 6, 188–195 (2013).
Catalano, S. et al. Leptin enhances, via AP-1, expression of aromatase in the MCF-7 cell line. J. Biol. Chem. 278, 28668–28676 (2003).
Pasqualini, J. R. et al. Concentrations of estrone, estradiol, and estrone sulfate and evaluation of sulfatase and aromatase activities in pre- and postmenopausal breast cancer patients. J. Clin. Endocrinol. Metab 81, 1460–1464 (1996).
Brannian, J. D. & Hansen, K. A. Leptin and ovarian folliculogenesis: implications for ovulation induction and ART outcomes. Semin. Reprod. Med. 20, 103–112 (2002).
Falk, R. T. et al. Interrelationships between serum leptin, IGF-1, IGFBP3, C-peptide and prolactin and breast cancer risk in young women. Breast Cancer Res. Treat. 98, 157–165 (2006).
Brewer, C. J. & Balen, A. H. The adverse effects of obesity on conception and implantation. Reproduction. 140, 347–364 (2010).
Terry, K. L., Willett, W. C., Rich-Edwards, J. W. & Michels, K. B. A prospective study of infertility due to ovulatory disorders, ovulation induction, and incidence of breast cancer. Arch. Intern. Med. 166, 2484–2489 (2006).
Liu, L. Y. et al. The role of adiponectin in breast cancer: a meta-analysis. PLoS. One. 8, e73183 (2013).
Macis, D., Guerrieri-Gonzaga, A. & Gandini, S. Circulating adiponectin and breast cancer risk: a systematic review and meta-analysis. Int. J. Epidemiol. 43, 1226–1236 (2014).
Wei, T., Ye, P., Peng, X., Wu, L. L. & Yu, G. Y. Circulating adiponectin levels in various malignancies: an updated meta-analysis of 107 studies. Oncotarget (2016).
Hebbard, L. & Ranscht, B. Multifaceted roles of adiponectin in cancer. Best. Pract. Res. Clin. Endocrinol. Metab 28, 59–69 (2014).
Barb, D., Williams, C. J., Neuwirth, A. K. & Mantzoros, C. S. Adiponectin in relation to malignancies: a review of existing basic research and clinical evidence. Am. J. Clin. Nutr. 86, s858–s866 (2007).
Lee, S. A. et al. Intra-individual variation of plasma adipokine levels and utility of single measurement of these biomarkers in population-based studies. Cancer Epidemiol. Biomarkers Prev. 16, 2464–2470 (2007).
Vona-Davis, L. & Rose, D. P. Adipokines as endocrine, paracrine, and autocrine factors in breast cancer risk and progression. Endocr. Relat Cancer 14, 189–206 (2007).
de Jager, W., Bourcier, K., Rijkers, G. T., Prakken, B. J. & Seyfert-Margolis, V. Prerequisites for cytokine measurements in clinical trials with multiplex immunoassays. BMC. Immunol. 10, 52 (2009).
Flower, L., Ahuja, R. H., Humphries, S. E. & Mohamed-Ali, V. Effects of sample handling on the stability of interleukin 6, tumour necrosis factor-alpha and leptin. Cytokine 12, 1712–1716 (2000).
Palli, D. et al. A molecular epidemiology project on diet and cancer: the EPIC-Italy Prospective Study. Design and baseline characteristics of participants. Tumori 89, 586–593 (2003).
Allione, A. et al. Anticoagulants used in plasma collection affect adipokine multiplexed measurements. Cytokine 80, 43–47 (2016).
Acknowledgements
We thank A. Evangelista and D. Del Sette for technical support, and Don Ward for help with the English. The Italian Association for Cancer Research (AIRC) provided financial support for this study.
Author information
Authors and Affiliations
Contributions
C.A., S.S., and V.K. conceived and designed the experiments. C.A., S.S., V.K., S.G., A.A., and G.M. performed the experiments. C.D.G. and G.T. contributed analysis tools. C.A., S.S., V.K., and V.P. wrote the paper. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Agnoli, C., Grioni, S., Pala, V. et al. Biomarkers of inflammation and breast cancer risk: a case-control study nested in the EPIC-Varese cohort. Sci Rep 7, 12708 (2017). https://doi.org/10.1038/s41598-017-12703-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-12703-x
This article is cited by
-
Dietary Inflammatory Index and risk of breast cancer: evidence from a prospective cohort of 67,879 women followed for 20 years in France
European Journal of Nutrition (2023)
-
Associations of aspirin and other anti-inflammatory medications with breast cancer risk by the status of COX-2 expression
Breast Cancer Research (2022)
-
Prognostic significance of cachexia in advanced non-small cell lung cancer patients treated with pembrolizumab
Cancer Immunology, Immunotherapy (2022)
-
Circulating inflammatory biomarkers, adipokines and breast cancer risk—a case-control study nested within the EPIC cohort
BMC Medicine (2022)
-
Inflammatory biomarkers and risk of breast cancer among young women in Latin America: a case-control study
BMC Cancer (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.