Abstract
The objective was to explore the effectiveness of glenohumeral joint distension for the treatment of frozen shoulder. We searched electronic data sources including PubMed, Scopus, and Embase from the earliest records available to February 2017. Eleven randomized controlled trials including at least one pair of comparisons between capsular distension and a reference treatment were included, comprising 747 participants. Patients’ characteristics, details of reference treatments, aspects of capsular distension therapy, and outcome measurement were evaluated at three points in time: baseline, early following intervention, and at the trial’s end. The primary and secondary outcomes were the between-group standardized mean differences of changes in shoulder function and range of motion, respectively. Regarding the long-term primary outcome, the superiority of capsular distension to reference treatments was not identified. One secondary outcome (external rotation limitation) showed a probable early positive response to capsular distension when compared to intra-articular corticosteroid injection. Aspects of approaches, imaging guiding techniques and doses of distension were not found to modify treatment effectiveness. In conclusion, distension of the glenohumeral joint provides a similar long-term efficacy to all reference treatments. A single dose of a corticosteroid-contained regimen introduced through the ultrasound-guided posterior approach is a preferable practice of capsular distension for the management of frozen shoulder.
Similar content being viewed by others
Introduction
Frozen shoulder, also known as adhesive capsulitis, has a prevalence of 2–5% in the general population and is considered to be one of the most serious painful conditions involving the musculoskeletal system1. The histopathology involves inflamed glenohumeral and subacromial synovium, hypertrophy of the coracohumeral ligament and fibrosis of the joint capsule2. Intra-articular fluid infusion has been reported to invoke capsular stiffness and a steeply rising pressure, indicating poor compliance of the joint capsule; this is recognized as the predominant feature of frozen shoulder3. Several experimental studies have indicated that hydrodilatation of the glenohumeral joint with normal saline and corticosteroid decreased intra-articular pressure and increased the shoulder volume capacity4, 5. Due to the potential physiological benefits of distending contracted shoulder joints, capsular distension has long been used as a treatment for frozen shoulder6. However, there are numerous other therapeutic options for frozen shoulder, including oral medication, manual manipulation, injection therapy and/or surgical capsular release7. Although the latest Cochrane review suggested that arthrographic distension with saline or steroid provides short-term benefits in pain when compared with placebo but a comparison with alternative interventions was uncertain8, sufficient evidence to back this theory from a quantitative analysis of high-quality trials is still lacking. Therefore, the present meta-analysis aimed to investigate the effectiveness of capsular distension for frozen shoulder in function improvement and mobility recovery from high-quality trials and explore factors that might modify its treatment outcome.
Methods
Search Strategy and Criteria
We performed a literature search primarily in PubMed from the earliest record to February 2017. Scopus, Embase and Google Scholar were used as secondary database sources for the purpose of retrieving relevant studies not indexed in PubMed9, 10. A systematic review and meta-analysis of associated topics, the Cochrane Collaboration Central Register of Controlled Clinical Trials and Cochrane Systematic Reviews, was also examined to confirm that all pertinent trials were enrolled. There was no restriction of language for literature search. The key terms were chosen and combined for literature search as follows: [“adhesive capsulitis” or “frozen shoulder” or “shoulder pain”] and [“hydrodilatation” or “hydrodistension” or “distension”].
Inclusion and Exclusion
In this study, we included randomized controlled trials (RCTs) that investigated the effectiveness of capsular distension for treating frozen shoulder. All of the selected trials were required to include at least a treatment arm employing the technique of capsular distension, defined as injection of a substantial amount of fluid into the glenohumeral recess to expand the joint capsule. There was no limitation for the therapy conducted in the control group, which could be injection of corticosteroid or the use of oral medication, physical therapy or manipulation under anesthesia. The target population was patients with a clinical diagnosis of frozen shoulder. Those with shoulder pain or subacromial impingement syndrome but without limited glenohumeral joint mobility were not included in the scope of this review. Case reports, case series, and/or single-arm longitudinal follow-up studies were excluded from our meta-analysis. To minimize selection bias, quasi-experimental comparative studies were not included, either.
Data Collection and Abstraction
Two authors independently scrutinized the titles and abstracts of the searched articles and determined which of them should be included in this study following discussion with each other. The following were extracted from each of the chosen studies: author name, year of publication, study type, demography of the participants, definition of frozen shoulder, allocation of the recruits, in formation on the randomization process used, dose and regimen for capsular distension, information on the imaging modality used for guiding injections, details of the controlled treatment and outcome measurements taken before and after interventions.
Assessment of Study Quality
The quality of each selected study was assessed using the Cochrane Collaboration tool for assessing risk of bias, which evaluates random sequence generation, allocation concealment, blinding of the participants, blinding of the outcome assessment, completeness of outcome data, reporting selectiveness and other bias11. All of these items were judged as either a high, low, or unclear risk of bias of the study’s design. In compliance with the process of data collection and abstraction, all the seven aspects were reviewed by two authors independently, and any discrepancy in opinions was solved through discussion11.
Meta-analysis Methodology
The primary and secondary outcomes were the between-group standardized mean differences (SMDs) of changes in shoulder function and range of motion, respectively. The visual analogue scale of pain or the numeric pain scale would be used as the surrogate if a shoulder function or disability scale was not available. The data for quantitative analysis was extracted from three time points: before the treatment, at the first visit following intervention and at the end of the trial. Regarding the studies that only measured the outcome once, the measurements were analyzed as data obtained early following intervention. The effect sizes were then pooled using the random effect (i.e., Dersimonian and Laird) model12, 13. When dealing with the paired data, we assumed 0.5 as the value of pre-post correlation13. The analysis was executed in accordance with the intention to treat principle. Heterogeneity among studies was assessed by employing the Chi-squared test and the I 2 statistic and was graded as low, moderate, or high by using 0–25%, 25–75% and/or 75–100% as the cut-off ranges14. To investigate the possible cause of heterogeneity, a subgroup analysis was performed based on the differences in treatment techniques and regimens. Differences between subgroups were defined by non-overlapping of their 95% confidence intervals (CIs) of pooled effect sizes. Publication bias was assessed using a funnel plot (for examination of plot asymmetry) and the Egger’s test (for determination of statistical significance)14. All of the calculations were conducted using Comprehensive Meta-analysis Software version 3 (Biostat, Englewood, NJ, USA), with p < 0.05 considered to be of statistical significance.
Results
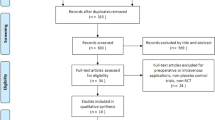
Study identification and selection
The initial search identified 255 citations, with a total of 127 left following removal of the duplicates. We later screened the titles and abstracts of the remaining literature and retained 21 articles for full text evaluation (Fig. 1). Ten studies were further excluded because one was a pilot research aiming at determining the maximal volume of hydrodilatation before capsule rupturing15; one was an experimental study comparing the effectiveness of hydrodilatation with capsule preservation and that with capsule rupturing5; three were case studies investigating pain reduction before and after hydrodilatation6, 16, 17; two were non-randomized comparative studies comparing arthrography with intra-articular corticosteroid and with or without capsular distension18, 19; one was an RCT comparing hydrodilatation by using two different guiding techniques20; one was an RCT investigating the effects of physical therapy after manipulation and hydrodilatation21; and one was an RCT that explored the difference between hypertonic saline wand normal saline as the regimen for hydrodilatation22. The final meta-analysis included 11 articles, representing a total of 747 participants.
Study characteristics and study quality
In the 11 enrolled trials, five double-armed RCTs compared hydrodilatation with corticosteroid injection to the glenohumeral joint23,24,25,26,27; one double-armed RCT compared hydrodilatation with placebo injection to the shoulder joint (arthrogram only)28, 28; one double-armed RCT compared hydrodilatation with manipulation29; one triple-armed RCT compared two methods of hydrodilatation (with or without corticosteroid in the distension regimen) with intra-articular corticosteroid injection30; one triple-armed RCT compared hydrodilatation with intra-articular corticosteroid injection and the usual care31; one triple-armed RCT compared hydrodilatation with intra-articular and subacromial corticosteroid injections32; and one four-armed trial compared hydrodilatation with and without intensive manipulation, manipulation alone and general physical therapy33. Regarding shoulder function measurements for calculation of the primary outcome, the Shoulder Pain and Disability Index was available in six RCTs24, 26,27,28, 31, 33, while the Constant Shoulder Scale was used in three RCTs25, 29, 32 and the visual analogue scale of pain was employed as the surrogate in one RCT23. Only the study conducted by Jacobs et al. lacked measurements of shoulder function30. A mixture of corticosteroid, local anesthetics, and normal saline was the most common regimen for hydrodilatation, and only one study employed the combination of hyaluronic acid and lidocaine24. The volume for hydrodilatation varied among studies, ranging from 20 mL to 90 mL. The majority employed a single dose of hydrodilatation, although two of the enrolled RCTs chose to incorporate multiple doses31. Ultrasound and fluoroscopy were the two most-frequently used guiding tools, and only two studies utilized the landmark-based injection technique30, 31. The details of the included studies are listed in Table 1 and the results of quality assessment are shown in Fig. 2.
Outcomes
In the evaluated studies, intra-articular corticosteroid injection was the most commonly used reference treatment, while subacromial corticosteroid injection32, placebo (arthrogram)28, intensive manipulation33, general physical therapy33 and treatment as usual (i.e., physical therapy and oral medication)31 all accounted for only one treatment arm, respectively. In the comparison with intra-articular corticosteroid injection, one treatment arm using local anesthetics with air30 and the other using hyaluronic acid24 for capsular dilatation were analyzed separately from those using corticosteroid in the distention regimen.
In terms of shoulder function, there was no significant benefit of capsular distension over intra-articular corticosteroid injection early following intervention (SMD, 0.51; 95% CI, −0.13 to 1.15) and at the end of the trial (SMD, 0.21; 95% CI, −011 to 0.52) (Fig. 3). With respect to shoulder range of motion improvement, hydrodilatation seemed to be better than corticosteroid intra-articular injection in external rotation early after treatment (SMD, 0.39; 95% CI, 0.18 to 0.59), although the advantage diminished in the long-term (SMD, 0.05; 95% CI, −0.19 to 0.29) (Fig. 4). Because the description of the use of corticosteroids was ambiguous in one study29, a sensitivity analysis was performed by removing it and the effect size remained similar for early external rotation improvement (SMD, 0.50; 95% CI, 0.07 to 0.93).
Forest plot of standardized mean differences of shoulder function improvement comparing hydrodilatation and intra-articular corticosteroid injection early following intervention (A) and at the trial’s end (B). Abbreviations: hydrodilatation, HD; intra-articular, IA. *denotes the regimen using hyaluronic acid instead of corticosteroid.
Forest plot of standardized mean differences of improvements in external rotation with use of hydrodilatation or an intra-articular corticosteroid injection early following intervention (A) and at the trial’s end (B). Abbreviations: hydrodilatation, HD; intra-articular, IA. *denotes the distension fluid that used hyaluronic acid instead of corticosteroid; #denotes the distension fluid that did not contain corticosteroid.
There was no between-group difference in abduction, forward flexion, or internal rotation at both time points (Supplement Figs 1–3). The treatment arm injecting hyaluronic acid in only one study24 demonstrated a similar trend along with the group using corticosteroid-mixed regimen and was superior to administration of intra-articular corticosteroid injection in early relief of external rotation limitation (SMD, 0.74; 95% CI, 0.32 to 1.17). Only one study used the arm employing local anesthetics with air for capsular distension which was shown to be inferior to the use of an intra-articular corticosteroid injection in all directions of shoulder movement improvement30 (Fig. 4, Supplement Figs 1 and 2). Regarding the studies without using intra-articular corticosteroid injection as controls, since each pair of comparison included a different controlled group, the pooled effect sizes were merely shown in the forest plots for reference (Figs 5 and 6 and Supplement Figs 4–6).
Forest plot of standardized mean differences of improvements in shoulder function comparing the use of hydrodilatation and various reference treatments early following intervention (A) and at the trial’s end (B). Abbreviations: hydrodilatation, HD; Placebo, PLA; IM, intensive manipulation; GPT, general physical therapy; TAU, treatment as usual; SAI, subacromial injection.
As part of this study, we performed subgroup analyses and tests for potential publication bias regarding the treatment pairs comparing capsular distension and corticosteroid intra-articular injections (Table 2). No differences were identified among the groups using either anterior or posterior needle approaches, single or multiple doses of injections and/or various guiding techniques like landmark, ultrasound, or fluoroscopy. In terms of publication bias, we only identified an unsymmetrical funnel plot with a p value of less than 0.05 through use of the Egger’s test in evaluating the effect sizes of early improvement in external rotation limitation.
Discussion
The present meta-analysis incorporated high-quality RCTs and investigated the effectiveness of capsular distension for frozen shoulder with respect to shoulder function and movement at different time points. Most of the evidence gathered resulted from the comparisons between hydrodilatation and corticosteroid intra-articular injection. We found that no significant differences in shoulder function were uncovered between hydrodilatation and all of the reference treatments evaluated. The use of hydrodilatation only led to a transient improvement in the limitations in external rotation of shoulder range of motion.
Corticosteroid injection has been recognized as an effective treatment for adhesive capsulitis and has provided a short-term benefit in pain reduction and restoration of range of motion compared with physical therapy34 and oral medication35. Although the subacromial bursa and rotator interval have also been reported as plausible regions for injection, injection into the glenohumeral joints is still the most frequently-used location considering capsular constriction is the primary pathology of the adhesive capsulitis. While corticosteroid administration is recognized as a chemical moderator that intervenes with intra-articluar inflammation, hydrodilatation may serve as a physical facilitator to synergistically expand the contracted joint cavity. In 2008, Buchbinder et al. conducted a Cochrane systematic review that included five RCTs and controlled trials that comparing arthroscopic distension with placebo or other interventions8. Among the five evaluated studies, only one RCT showed low risk of bias, demonstrating that hydrodilatation with corticosteroid and saline was better than a placebo in pain reduction and improvement in range of motion28. In the review article, there was no evidence to support that hydrodilatation was superior to other management methods such as corticosteroid intra-articular injection. Therefore, with a growing number of studies investigating various therapeutic options for adhesive capsulitis7, 36, we felt that it was necessary to integrate a high quality of evidence to validate the effectiveness of capsular distension for patients with frozen shoulder.
Awareness of the clinical course of adhesive capsulitis is crucial in determining the efficacy of a certain treatment. Although it has been described as a self-limiting disorder that resolves spontaneously within one to three years, a certain percentage (between 20% to 50%) of patients suffer long-term shoulder functional deficit36. Therefore, an intervention that provides early improvement and/or reduces long-term disability is of clinical significance, which served as the main reason for why we extracted participants’ data at three time points. In our research, the primary outcome was a change in shoulder function or disability scales, nearly all of which incorporated an evaluation of pain and functional limitation and were believed to be the best indicator of therapeutic effects. Based the comparison between hydrodilatation and treatments other than intra-articular corticosteroid injections, we were aware that hydrodilatation might be better than certain conservative management methods like medication and physical therapy early following intervention. Our study also indicated that hydrodilatation achieved similar efficacy as compared with intra-articular corticosteroid injection for the improvement of shoulder function.
The analysis of changes in range of motion shed light on a potential advantage of the use of hydrodilatation over intra-articular corticosteroid injection. However, the benefit was only seen in early recovery of external rotation limitation but not in internal rotation, abduction, or forward flexion. Many experimental and clinical studies have indicated that a predominant pathology of adhesive capsulitis is contracture of the coracohumeral ligament at the rotator interval37, 38. Extendibility of the structures near the anterior glenohumeral joint has been shown to associate the degrees of external rotation39. When performing hydrodilatation with arthrogram, leakage of contrast agents into the subscapularis bursa is usually indicative of capsule rupture40. This phenomenon implies that the anterior capsule is less resilient to stretching force from infused fluid than the posterior capsule, and might be the possible reason why hydrodilatation resulted in a reduction of the limitations on external rotation more than other directions. However, in our study, we also found an unsymmetrical funnel plot with a p value of less than 0.05 through use of the Egger’s test in evaluating the effect sizes of early improvement in external rotation limitation. The finding suggested a notable difference in methods of outcome assessment and treatment arms (i.e. volume used for capsular distension). Whether capsular distension benefits early recovery of range of motion needs more evidence derived from future studies using a standardized treatment protocol.
Regarding the regimen for dilatation, we found that the treatment arm that incorporated local anesthetics with air for dilatation had a significantly inferior outcome compared with those that employed corticosteroid intra-articular injection30. Hydrodilatation exerts physical stress on the constricted joint capsule, which may cause inflammation due to stretching injury. The addition of corticosteroid into the distension fluid appears to be imperative and may effectively divert the glenohumeral joint from a long-term inflammatory cascade41. Furthermore, a recent systematic review that included four RCTs pointed out that hyaluronic acid was not superior to corticosteroid injection or physical therapy for the treatment of adhesive capsulitis42. Since hyaluronic acid was only used in one of our selected trials, the evidence of hyaluronic acid used as an equivalent or a superior replacement for corticosteroid-containing regimens remains weak.
Regarding the comparison of hydrodilatation with non-invasive treatments, we noticed that hydrodilatation without manipulation was less effective than the use of intensive manipulation alone in one study33. Since patients’ post-intervention exercise regimen varied across the included studies, the influence of concomitant physical therapy on the effects of hydrodilatation was difficult to quantify.
The subgroup analysis provided certain insights of clinical application of hydrodilatation. First, no difference in effectiveness was recognized among the various aspects of approaches and/or guiding techniques. We suggested the use of the posterior approach through ultrasound guidance due to its provision of easy visualization of the joint capsule for needle advancement and freedom from radiation exposure. Second, multiple doses of hydrodilatation were not superior to a single dose of application, although a case series indicated repeated capsular distension with normal saline and corticosteroid could change the biomechanical properties of the glenohumeral joint4. Therefore, a single dose of hydrodilatation with corticosteroid and sufficient distension fluid appeared to be the preferable regimen. Another important point is that the clinicians need to weight up the adverse effect of hydrodilatation like severe pain after rupture of the joint capture with only a transient improvement in mobility in external rotation identified.
Study limitations
Several limitations do need to be acknowledged. First, the amount of distension fluid varied across the different studies considered and sometimes even in individual trials. As such, we were unable to determine the influence of injectate amount on treatment effectiveness using either a subgroup analysis or meta-regression. Second, the causes of frozen shoulder in our study population were multifactorial: some of them were idiopathic, while the remaining causes were secondary to diabetes mellitus, painful rotator cuff disorders, or other conditions. None of our enrolled RCTs probed a specific patient group, the effects of hydrodilatation on which need future additional research to validate. Third, most of distension fluid contained corticosteroid, but the dosage in the hydrodilatation group was usually identical to that in the intra-articular injection group. Therefore, the optimal dose of corticosteroid added in the hydrodilatation regimen also requires future investigation. Fourth, since our primary outcome was changes in shoulder function, the included studies might have low statistical power to detect changes in mobility, which was treated as the secondary outcome in this meta-analysis. In addition, the methods of evaluating shoulder range of motion differed among studies which made detection of a small improvement more difficult. Fifth, our secondary outcome employed multiple aspects of shoulder range of motion, which possessed the risk of false positive findings. Therefore, any positive result of the secondary outcome should be interpreted carefully and requires future studies to prove.
Conclusion
Evidence from aggregated published RCTs showed that the effectiveness of glenohumeral joint distension was similar to that of intra-articular corticosteroid injection, as well as that of most of the current conservative management methods. Corticosteroid plays a significant role in the early improvement of movement in frozen shoulder and capsular distension is not associated with significant changes in the long term outcome.
References
Zreik, N. H., Malik, R. A. & Charalambous, C. P. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles, ligaments and tendons journal 6, 26–34, doi:10.11138/mltj/2016.6.1.026 (2016).
Tamai, K., Akutsu, M. & Yano, Y. Primary frozen shoulder: brief review of pathology and imaging abnormalities. Journal of orthopaedic science: official journal of the Japanese Orthopaedic Association 19, 1–5, doi:10.1007/s00776-013-0495-x (2014).
Chung, S. G., Lee, K. J., Kim, H. C., Seo, K. S. & Lee, Y. T. Intra-articular pressure profiles of painful stiff shoulders compared with those of other conditions. PM & R: the journal of injury, function, and rehabilitation 1, 297–307, doi:10.1016/j.pmrj.2009.01.024 (2009).
Koh, E. S., Chung, S. G., Kim, T. U. & Kim, H. C. Changes in biomechanical properties of glenohumeral joint capsules with adhesive capsulitis by repeated capsule-preserving hydraulic distensions with saline solution and corticosteroid. PM & R: the journal of injury, function, and rehabilitation 4, 976–984, doi:10.1016/j.pmrj.2012.06.006 (2012).
Kim, K. et al. Capsule preservation improves short-term outcome of hydraulic distension in painful stiff shoulder. Journal of orthopaedic research: official publication of the Orthopaedic Research Society 29, 1688–1694, doi:10.1002/jor.21446 (2011).
Andren, L. & Lundberg, B. J. Treatment of Rigid Shoulders by Joint Distension during Arthrography. Acta Orthop Scand 36, 45–53 (1965).
Uppal, H. S., Evans, J. P. & Smith, C. Frozen shoulder: A systematic review of therapeutic options. World journal of orthopedics 6, 263–268, doi:10.5312/wjo.v6.i2.263 (2015).
Buchbinder, R., Green, S., Youd, J. M., Johnston, R. V. & Cumpston, M. Arthrographic distension for adhesive capsulitis (frozen shoulder). The Cochrane database of systematic reviews CD007005, doi:10.1002/14651858.CD007005 (2008).
Hung, C. Y., Hsiao, M. Y., Chang, K. V., Han, D. S. & Wang, T. G. Comparative effectiveness of dextrose prolotherapy versus control injections and exercise in the management of osteoarthritis pain: a systematic review and meta-analysis. Journal of pain research 9, 847–857, doi:10.2147/JPR.S118669 (2016).
Chang, K. V. et al. Comparative Effectiveness of Suprascapular Nerve Block in the Relief of Acute Post-Operative Shoulder Pain: A Systematic Review and Meta-analysis. Pain physician 19, 445–456 (2016).
Chang, K. V. et al. Early Versus Delayed Passive Range of Motion Exercise for Arthroscopic Rotator Cuff Repair: A Meta-analysis of Randomized Controlled Trials. The American journal of sports medicine 43, 1265–1273, doi:10.1177/0363546514544698 (2015).
Fleiss, J. L. The statistical basis of meta-analysis. Statistical methods in medical research 2, 121–145, doi:10.1177/096228029300200202 (1993).
Chang, K. V. et al. Comparison of the Effectiveness of Suprascapular Nerve Block With Physical Therapy, Placebo, and Intra-Articular Injection in Management of Chronic Shoulder Pain: A Meta-Analysis of Randomized Controlled Trials. Archives of physical medicine and rehabilitation 97, 1366–1380, doi:10.1016/j.apmr.2015.11.009 (2016).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. Bmj 327, 557–560, doi:10.1136/bmj.327.7414.557 (2003).
Lee, K. J., Lee, H. D. & Chung, S. G. Real-time pressure monitoring of intraarticular hydraulic distension for painful stiff shoulders. Journal of orthopaedic research: official publication of the Orthopaedic Research Society 26, 965–970, doi:10.1002/jor.20535 (2008).
Vad, V. B., Sakalkale, D. & Warren, R. F. The role of capsular distention in adhesive capsulitis. Archives of physical medicine and rehabilitation 84, 1290–1292 (2003).
Ibrahim, T., Rahbi, H., Beiri, A., Jeyapalan, K. & Taylor, G. J. Adhesive capsulitis of the shoulder: the rate of manipulation following distension arthrogram. Rheumatology international 27, 7–9, doi:10.1007/s00296-006-0160-1 (2006).
Corbeil, V., Dussault, R. G., Leduc, B. E. & Fleury, J. [Adhesive capsulitis of the shoulder: a comparative study of arthrography with intra-articular corticotherapy and with or without capsular distension]. Canadian Association of Radiologists journal = Journal l’Association canadienne des radiologistes 43, 127–130 (1992).
Ahn, J. K. et al. Effects of Ultrasound-guided intra-articular ketorolac injection with capsular distension. Journal of back and musculoskeletal rehabilitation 28, 497–503, doi:10.3233/BMR-140546 (2015).
Park, K. D. et al. Comparison of Sono-guided Capsular Distension with Fluoroscopically Capsular Distension in Adhesive Capsulitis of Shoulder. Annals of rehabilitation medicine 36, 88–97, doi:10.5535/arm.2012.36.1.88 (2012).
Buchbinder, R. et al. Efficacy and cost-effectiveness of physiotherapy following glenohumeral joint distension for adhesive capsulitis: a randomized trial. Arthritis and rheumatism 57, 1027–1037, doi:10.1002/art.22892 (2007).
Lee, J. H., Kim, S. B., Lee, K. W., Lee, S. J. & Lee, J. U. Effect of Hypertonic Saline in Intra-Articular Hydraulic Distension for Adhesive Capsulitis. PM & R: the journal of injury, function, and rehabilitation 7, 721–726, doi:10.1016/j.pmrj.2015.04.013 (2015).
Gam, A. N., Schydlowsky, P., Rossel, I., Remvig, L. & Jensen, E. M. Treatment of “frozen shoulder” with distension and glucorticoid compared with glucorticoid alone. A randomised controlled trial. Scandinavian journal of rheumatology 27, 425–430 (1998).
Park, K. D., Nam, H. S., Lee, J. K., Kim, Y. J. & Park, Y. Treatment effects of ultrasound-guided capsular distension with hyaluronic acid in adhesive capsulitis of the shoulder. Archives of physical medicine and rehabilitation 94, 264–270, doi:10.1016/j.apmr.2012.10.002 (2013).
Mun, S. W. & Baek, C. H. Clinical efficacy of hydrodistention with joint manipulation under interscalene block compared with intra-articular corticosteroid injection for frozen shoulder: a prospective randomized controlled study. Journal of shoulder and elbow surgery 25, 1937–1943, doi:10.1016/j.jse.2016.09.021 (2016).
Lee, D. H., Yoon, S. H., Lee, M. Y., Kwack, K. S. & Rah, U. W. Capsule-preserving hydrodilatation with corticosteroid versus corticosteroid injection alone in refractory adhesive capsulitis of shoulder: a randomized controlled trial. Archives of physical medicine and rehabilitation, doi:10.1016/j.apmr.2016.10.012 (2016).
Tveita, E. K., Tariq, R., Sesseng, S., Juel, N. G. & Bautz-Holter, E. Hydrodilatation, corticosteroids and adhesive capsulitis: a randomized controlled trial. BMC musculoskeletal disorders 9, 53, doi:10.1186/1471-2474-9-53 (2008).
Buchbinder, R., Green, S., Forbes, A., Hall, S. & Lawler, G. Arthrographic joint distension with saline and steroid improves function and reduces pain in patients with painful stiff shoulder: results of a randomised, double blind, placebo controlled trial. Annals of the rheumatic diseases 63, 302–309 (2004).
Quraishi, N. A., Johnston, P., Bayer, J., Crowe, M. & Chakrabarti, A. J. Thawing the frozen shoulder. A randomised trial comparing manipulation under anaesthesia with hydrodilatation. The Journal of bone and joint surgery. British volume 89, 1197–1200, doi:10.1302/0301-620X.89B9.18863 (2007).
Jacobs, L. G. et al. Intra-articular distension and steroids in the management of capsulitis of the shoulder. Bmj 302, 1498–1501 (1991).
Sharma, S. P., Baerheim, A., Moe-Nilssen, R. & Kvale, A. Adhesive capsulitis of the shoulder, treatment with corticosteroid, corticosteroid with distension or treatment-as-usual; a randomised controlled trial in primary care. BMC musculoskeletal disorders 17, 232, doi:10.1186/s12891-016-1081-0 (2016).
Yoon, J. P. et al. Intra-articular injection, subacromial injection, and hydrodilatation for primary frozen shoulder: a randomized clinical trial. Journal of shoulder and elbow surgery 25, 376–383, doi:10.1016/j.jse.2015.11.009 (2016).
Park, S. W., Lee, H. S. & Kim, J. H. The effectiveness of intensive mobilization techniques combined with capsular distension for adhesive capsulitis of the shoulder. Journal of physical therapy science 26, 1767–1770, doi:10.1589/jpts.26.1767 (2014).
Blanchard, V., Barr, S. & Cerisola, F. L. The effectiveness of corticosteroid injections compared with physiotherapeutic interventions for adhesive capsulitis: a systematic review. Physiotherapy 96, 95–107, doi:10.1016/j.physio.2009.09.003 (2010).
Ranalletta, M. et al. Corticosteroid Injections Accelerate Pain Relief and Recovery of Function Compared With Oral NSAIDs in Patients With Adhesive Capsulitis: A Randomized Controlled Trial. The American journal of sports medicine 44, 474–481, doi:10.1177/0363546515616238 (2016).
Manske, R. C. & Prohaska, D. Diagnosis and management of adhesive capsulitis. Current reviews in musculoskeletal medicine 1, 180–189, doi:10.1007/s12178-008-9031-6 (2008).
Ozaki, J., Nakagawa, Y., Sakurai, G. & Tamai, S. Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. The Journal of bone and joint surgery. American volume 71, 1511–1515 (1989).
Neer, C. S. 2nd, Satterlee, C. C., Dalsey, R. M. & Flatow, E. L. The anatomy and potential effects of contracture of the coracohumeral ligament. Clinical orthopaedics and related research, 182–185 (1992).
Harryman, D. T. 2nd, Sidles, J. A., Harris, S. L. & Matsen, F. A. 3rd The role of the rotator interval capsule in passive motion and stability of the shoulder. The Journal of bone and joint surgery. American volume 74, 53–66 (1992).
Bell, S., Coghlan, J. & Richardson, M. Hydrodilatation in the management of shoulder capsulitis. Australasian radiology 47, 247–251 (2003).
Song, A., Higgins, L. D., Newman, J. & Jain, N. B. Glenohumeral corticosteroid injections in adhesive capsulitis: a systematic search and review. PM & R: the journal of injury, function, and rehabilitation 6, 1143–1156, doi:10.1016/j.pmrj.2014.06.015 (2014).
Lee, L. C., Lieu, F. K., Lee, H. L. & Tung, T. H. Effectiveness of hyaluronic acid administration in treating adhesive capsulitis of the shoulder: a systematic review of randomized controlled trials. BioMed research international 2015, 314120, doi:10.1155/2015/314120 (2015).
Acknowledgements
This work was supported by grants from MOST 105-2314-B-002-008, MOST 106-2314-B-002-180 and National Taiwan University Hospital, Bei-Hu branch.
Author information
Authors and Affiliations
Contributions
W.T.W., and K.V.C. designed and wrote the paper. D.S.H., C.H.C., F.S.Y., and C.P.L. edited the paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, WT., Chang, KV., Han, DS. et al. Effectiveness of Glenohumeral Joint Dilatation for Treatment of Frozen Shoulder: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Sci Rep 7, 10507 (2017). https://doi.org/10.1038/s41598-017-10895-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-10895-w
This article is cited by
-
Ultrasound-guided hydrodilatation for adhesive capsulitis: capsule-preserving versus capsule-rupturing technique
Skeletal Radiology (2024)
-
Current concepts in the diagnosis and treatment of adhesive capsulitis: role of diagnostic imaging and ultrasound-guided interventional procedures
La radiologia medica (2022)
-
Hydrodilatation with corticosteroids is the most effective conservative management for frozen shoulder
Knee Surgery, Sports Traumatology, Arthroscopy (2021)
-
Intra-articular steroid for adhesive capsulitis: does hydrodilatation give any additional benefit? A randomized control trial
Skeletal Radiology (2020)
-
Konservative Therapie der „frozen shoulder“
Der Unfallchirurg (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.