Abstract
Systemic infusion of bone marrow stromal cells (BMSCs), a major type of multipotent stromal cells, produces pain relief (antihyperalgesia) that lasts for months. However, studies have shown that the majority of BMSCs are trapped in the lungs immediately after intravenous infusion and their survival time in the host is inconsistent with their lengthy antihyperalgesia. Here we show that long-lasting antihyperalgesia produced by BMSCs required their chemotactic factors such as CCL4 and CCR2, the integrations with the monocytes/macrophages population, and BMSC-induced monocyte CXCL1. The activation of central mu-opioid receptors related to CXCL1-CXCR2 signaling plays an important role in BMSC-produced antihyperalgesia. Our findings suggest that the maintenance of antihypergesia can be achieved by immune regulation without actual engraftment of BMSCs. In the capacity of therapeutic use of BMSCs other than structural repair and replacement, more attention should be directed to their role as immune modulators and subsequent alterations in the immune system.
Similar content being viewed by others
Introduction
Multipotent stromal cells have shown their therapeutic potential in a variety of clinical conditions1,2,3. Transplantation of bone marrow stromal cells (BMSCs), a major type of multipotent stromal cells, produces pain-relief or antihyperalgesia that lasts up to months and apparently involves activation of endogenous opioids in preclinical pain models4,5,6,7,8. Clinical studies also show promising long-term pain relief with multipotent stromal cells9, 10.
Considering the long-lasting beneficial effects of MSCs, there is a paradox. MSCs are often administered systemically. However, the majority of MSCs are trapped in the lungs immediately after intravenous infusion11,12,13. Only a very small percentage (<1%) of systemic MSCs can migrate to the injured brain/spinal site12, 14,15,16. Even direct arterial infusion that bypasses the pulmonary first-pass effect only leads to a transient recruitment of the cells to the brain17. Further, systemic MSCs only stay in the body for a matter of days to a few weeks12, 13, 18. MSCs survived better after intrathecal delivery. A portion of intrathecally injected MSCs migrated to the dorsal root ganglion and survived there for up to 84 days4. Nevertheless, about 50% of the survived cells were lost in about 14 days, while the antihyperalgesia of MSCs remained at the same level for at least 38 days.
Recent MSC medicine appreciate that there are sophisticated interactions between implanted cells and the host immune system19, 20. Intravenously infused MSCs would first encounter circulating immune cells and embolized cells in the lungs also interact with the host13, 21, 22. MSCs express a variety of immune mediators and receptors23, 24. The interactions between the immune and nervous system affect pain25. Thus, infused MSCs may interact with host immune cells, followed by release of immune mediators, leading to activation of the endogenous analgesic system and long-lasting pain relief. We have conducted a series of experiments to test this hypothesis.
Results
BMSC induced upregulation of opioid receptors
We have used a model of chronic orofacial pain with ligation injury of the masseter muscle tendon (TL) to assess BMSC-produced antihyperalgesia5. Notably, the pain-attenuating effect of BMSCs was consistently observed in other persistent pain models in both males and females with multiple measures of nociception, including thermal and mechanical pain sensitivity and pain-related conditioned place avoidance26. We showed previously that the BMSC-produced antihyperalgesia was attenuated, or pain hypersensitivity rekindled, by naloxone, an opioid receptors antagonist5; and that N-methyl-D-aspartate receptor-mediated trigeminal nociceptive neuronal hyperexcitability was attenuated by BMSCs, an effect also reversed by naloxone26. As naloxone may act as an inverse agonist to block opioid receptor constitutive activity, leading to increased pain27, we further verified this effect with a neutral opioid receptor antagonist 6-β-naltrexol. Similarly, the BMSC-produced antihyperalgesia was attenuated by 6-β-naltrexol (Supplementary Fig. 1a,b). These results suggest that the antihyperalgesia by BMSCs involves the endogenous opioid system.
Since RNAi of μ-opioid receptors (MOR) in the rostral ventromedial medulla (RVM), a major opioid-containing brainstem site for pain modulation, attenuated BMSC-produced antihyperalgesia5, we first examined whether there was a long-term effect of BMSCs on opioid receptor expression in the RVM (Fig. 1a). At 1w and 8w after infusion of primary BMSC, RT-qPCR showed that MOR, but not δ- and κ-opioid receptor mRNAs was upregulated (Fig. 1b) and western blot confirmed upregulation of MOR proteins in RVM (Fig. 1c). We have found that BMSCs after multiple passages (≥20 P) lost their antihyperalgesic property5 and can be used as a control. 20P-BMSCs did not affect MOR expression at 1w but only slightly increased MOR at 8w after infusion (Fig. 1c). Compared to 20P-BMSC-treated rats, the MOR protein levels were significantly higher at both 1 and 8 w after treatment with primary BMSCs (Fig. 1c). Consistently, increased immunostaining against MOR in RVM was observed (Supplementary Fig. 1c–f). This phenomenon was not limited to tissue injury pain models. In rats with L5 spinal nerve ligation injury, a model of neuropathic pain, infusion of human BMSCs selectively upregulated MOR mRNA in RVM (Supplementary Fig. 1h). These observations indicate that BMSC-produced antihyperalgesia involves long-lasting activation of the endogenous opioid system.
BMSC-induced selective upregulation of MOR and differential gene expression profiles between PRI and 20P-BMSCs. (a) The transverse section of the brainstem at 11.30 mm posterior to the Bregma illustrating the site where rostral ventromedial medulla (RVM) tissues were punched out for analysis (circle). py, pyramidal tract; 7n, facial nucleus; sp5, spinal trigeminal complex. (b) Bar graph shows relative levels of opioid receptor mRNAs in RVM. *p < 0.05 vs. medium. MOR, DOR, KOR: mu-, delta-, and kappa-opioid receptors, respectively. N = 3/group. (c) TL rats received primary (PRI) or 20-passage (20 P) BMSCs (20P-BMSC do not produce antihyperalgesia and was used as a control) at 7d post injury. β-actin was a loading control. *p < 0.05, **p < 0.01, ***p < 0.001, vs. Naïve; #p < 0.05, ##p < 0.01, vs. respective 20 P. n = 6/group. Cropped gel images are shown. See Supplementary Figure 9 for full-length blots. (d) Immunostaining against CD90 in PRI and 20 P BMSCs. Scale = 10 μm. (e) The treatment with PRI-, but not 20P-BMSCs, upregulated MOR gene expression in RVM. *p < 0.05, vs. naïve, medium and 20 P, n = 3. For (b,c,e), statistical comparisons were made by One-way ANOVA followed by post-hoc comparisons with Bonferroni corrections. (f) Heat map of gene-expression analysis. Total RNAs from PRI- and 20P-BMSCs were characterized using The Rat Inflammatory Cytokines & Receptors RT2 ProfilerTM PCR Array. Each column shows a separate sample. (g) The relative expression levels of each gene (open circles) in the PRI and 20 P samples are plotted against each other. Red, genes shown higher expression levels in PRI-BMSCs (>2-fold); Green, genes expressed lower (>2-fold) in PRI-cells and Black, no change (≤2-fold). The two dashed lines indicate the 2-fold changes from the middle diagonal line. Crosses represent control genes. (h) Bar graph illustrating fold changes in gene expression between PRI and 20P-BMSCs. Dashed line represents equal expression between PRI- and 20P-BMSCs.
Differential gene expression in primary and 20P-BMSCs
The lasting upregulation of MOR and antihyperalgesia apparently contradicts the kinetics of infused BMSCs in the body. Most intravenously infused MSCs are trapped in the lungs and removed from the system within a few weeks12, 13. Utilizing BMSCs isolated from GFP transgenic S-D rats [SD-Tg(GFP)Bal]28, we have verified this phenomenon. BMSCs were infused into the rat at 7d after TL. GFP-positive BMSCs were accumulated in the lungs at 6 h and 1d after infusion and very few GFP cells were observed at 7d after infusion (Supplementary Fig. 2). Few GFP cells were seen at the injured site and none was observed in the brainstem. Considering long-lasting effect of BMSCs on MOR and persistent pain, we reasoned that mechanisms other than a direct effect or engraftment of BMSCs underlie their antihyperalgesia.
Previous studies indicate that primary, but not 20P-BMSCs, produced pain relief5, suggesting altered BMSC genotype during culturing. Primary and 20P-BMSCs exhibited similar staining intensity for CD90.1 (Fig. 1d), indicating that BMSC markers maintained their expression in high-passage BMSCs29. However, at 8w after BMSC infusion, primary, but not 20P-BMSCs, upregulated MOR gene expression in RVM (Fig. 1e), consistent with a lack of antihyperalgesic effect by 20P-BMSCs5. Taking advantage of this phenomenon, we compared gene expression of primary and 20P-BMSCs. Utilizing the Inflammatory Cytokines & Receptors PCR Array, we observed differential expression profiles of major cytokines/chemokines and receptors between the primary and 20P-BMSCs (Fig. 1f–h). Among the 84 genes examined, 50 in primary BMSCs were expressed at a higher level in all 3 samples (≥2-fold) and 26 of them showed greater than 100-fold differences over the 20P-cells. Six genes expressed lower (>2-fold) in primary BMSCs (Fig. 1h). Genes for ribosomal proteins (Rpl13a and Rplp1), lactate dehydrogenase A and housekeeping protein β-actin (Actb) do not show differential expressions, suggesting normal biochemical activity remained in 20P-BMSCs. Control genes did not show greater than 2-fold differences between primary and 20P-BMSCs (Fig. 1g, crosses). Higher expression of some genes was further verified with RT-qPCR (Supplementary Fig. 3)
A repertoire of genes for immune mediators and receptors exhibited higher levels of expression in primary BMSCs compared to 20P-BMSCs (Table 1 4, 22, 30,31,32,33,34,35,36,37,38,39,40,41,42,43,44), including genes for chemotaxis-inducing chemokines and their receptors (Cxcl4, Ccl2, Ccl3, Ccl4, Cxcl12 (Sdf-1), Ccr2, Ccr5), anti-inflammatory cytokines and receptors (Tgfb1, Il10, Il10-ra, Il13RA1), proinflammatory cytokines and receptors (Tnf, Il1b, Il18, Tnfrsf1b), and components of the complement pathways (C3, C5). Interestingly, genes for CXCR2 and its ligands (Cxcl1, Cxcl2, Cxcl5, Cxcr2) that are involved in opioid release from immune cells30 showed higher expression in primary BMSCs. There was simultaneous higher mRNA expression of some receptors and their ligands in primary BMSCs (e.g., Ccl3/4/5-Ccr5, Cxcl1/2-Cxcr2, Ccl5-Ccr1, Il10-Il10ra, Tnf-Tnfrsf1b, Cxcl1/2/5-Cxcr2), suggesting reciprocal interactions with the host immune cells and autocrine signaling of BMSCs. TGFβ1, which was a critical mediator of BMSCs’ antihyperalgesia after intrathecal administration4, expressed higher in primary BMSCs (Fig. 1h, Supplementary Fig. 3). While higher expression of the anti-inflammatory cytokines and receptors is consistent with antihypergesia, genes of proinflammatory cytokines and complement components may contribute to the effect of BMSCs by promoting chemotactive interactions with immune cells21.
BMSC-derived Chemokines as mediators of antihyperalgesia
Differential gene expressions between antihyperalgesic primary and ineffective 20P-BMSCs suggest a role of BMSC-derived chemokines in BMSC-produced antihyperalgesia. We next chose to evaluate a role of CCL4 since it’s mRNA was not detectable in 2 of 3 20P-BMSC samples (Ct over the cut-off in one) and its expression showed the second highest fold change over 20P-BMSCs (Fig. 1h, Table 1). Western blot confirmed very low level of CCL4 in 20P-BMSCs, compared to primary BMSCs (Fig. 2a). We then employed a subtraction strategy to assess the role of CCL4 in BMSC-produced antihyperalgesia. Before transplantation, primary BMSCs were transduced with Ccl4 shRNA lentivirus. Figure 2b,c show the successful transduction of BMSCs and knock-down of Ccl4. Mechanical nociception of the rat was assessed with von Frey filaments45. EF50 (Effective Force50), the derived von Frey filament force (g) that produces a 50% response, was used as a measure of mechanical sensitivity5. In TL rats receiving infusion of transduced BMSCs, BMSC-induced increase in EF50 was significantly reduced, compared to that receiving control shRNA (Fig. 2d), and the increased MOR expression in RVM was also significantly reduced (Fig. 2g). These results indicate that BMSC-derived CCL4 contributed to their antihyperalgesic effect.
Attenuation of BMSC-induced antihyperalgesia after subtraction of Ccl4 and blocking CCR2. (a) CCL4 protein levels were reduced in P20 BMSCs. *p < 0.05, vs. P1 BMSCs, n = 4. (b) Primary BMSCs were transducted with Ccl4-shRNA plasmids containing GFP. Immunofluorescence staining of BMSC with GFP confirmed successful gene transfer. Scale = 10 μm. (c) Ccl4 mRNA expression was reduced in BMSCs transduced with Ccl4 shRNA lentivirus compared to Ctrl shRNA-treated cells (n = 3, RT-qPCR). *p < 0.05, vs. ctrl shRNA. (d) Attenuation of BMSC-induced antihyperalgesia by pretreatment of BMSCs with RNAi of Ccl4. Compared to Ctrl shRNA, Ccl4 shRNA pretreatment attenuated BMSC-produced antihyperalgesia in TL rats, as indicated by a reduction in EF50. Dashed lines connect data points not shown with the scale of the abscissa. Ipsi, ipsilateral to injury; Con, contralateral non-injured. (e) CCR2 protein levels were reduced in P20 BMSCs. *p < 0.05, vs. P1 BMSCs, n = 4. (f) Pretreatment of BMSC with RS 102895 (10 μM for 24 h), a CCR2b antagonist attenuated BMSC-produced antihyperalgesia. ##p < 0.01, ###p < 0.001; vs. Ctrl shRNA (C) and vs. Veh (D). (g) Pretreatment of BMSC with shRNA against Ccl4 (-Ccl4) or CCR2b antagonist RS 102895 (-CCR2) reduced BMSC-induced MOR upregulation in RVM in TL rats. *p < 0.05, vs. veh. Error bars in (a,c,e, and g) are S.E.M. and in (d and f) (n = 6–8) are 95% confidence intervals. Statistics: (a,c,e) Unpaired, Two-tailed Student’s t-test; (d,f) Two-way ANOVA followed by post-hoc comparisons with Bonferroni corrections; (g) One-way ANOVA followed by post-hoc comparisons with Bonferroni corrections. Cropped gel images are shown in 2a, e.g. See Supplementary Figure 9 for full-length blots.
We then examined the role CCL2-CCR2 signaling, the most studied chemoattractant for monocytes, T cells and other immune cells46. Both CCL2 and CCR2 genes showed higher expression in primary BMSCs (Fig. 1h, Supplementary Fig. 3). In contrast to primary BMSCs, CCR2 proteins in 20P-BMSCs was almost undetectable (Fig. 2e). In the next experiment, primary BMSCs were pretreated with a CCR2 receptor antagonist RS102895 (10 μM for 24 h) before infusion. In TL rats receiving infusion of RS102895-treated cells, BMSC-induced increase in EF50 was significantly decreased (Fig. 2f); and the increased MOR expression in RVM was also significantly reduced (Fig. 2g). Since CCR2 has been shown important for MSC homing38, 39, we examined whether blocking CXCL12 (SDF-1)-CXCR4 signaling, key to migration of BMSCs to the injured site4, led to a reduction of antihyperalgesia. TL rats were pretreated with AMD3100 (plerixafor, 10 mg/kg/day, i.p. for 4 days), an antagonist of CXCL12 receptor CXCR4. AMD3100 did not affect BMSC-produced antihyperalgesia (Supplementary Fig. 4). These results suggest that pain attenuation after systemic BMSCs involves chemokine interactions with immune cells, but not necessarily involving homing. However, intrathecal BMSCs may escape the lung trapping and CXCR4 signaling appears important for the antihyperalgesia induced by intrathecal BMSCs4.
The role of monocytes/macrophages in pain-relieving effect of BMSCs
Our observations led to a hypothesis that host immune cells relay BMSCs’ input through chemotactic interactions to produce long-lasting antihyperalgesia. Monocytes/macrophages have been shown to mediate the BMSC-produced anti-sepsis22. Depletion of macrophages attenuated opioid-induced analgesia47. To evaluate a role of monocytes/macrophages, we employed the liposome-encapsulated clodronate (Lipo-Clo) procedure to deplete monocytes/macrophages48,49,50. Liposome-encapsulated clodronate was injected i.p. 3 times in three days (10 mg/2 ml/injection/rat). After the injections, peritoneal cells were collected and labeled with macrophage marker CD11b. The reduced peritoneal macrophage expression was verified by flow cytometry and ED1-immunostaining of spleen sections (Supplementary Fig. 5a,b). The Lipo-Clo treatment attenuated BMSC-produced antihyperalgesia. In rats pretreated with vehicle of Lipo-Clo, the EF50s were significantly increased from 3 d post-BMSCs compared to 14d-TL, indicating antihyperalgesia (Fig. 3a). However, with Lipo-Clo pretreatment, the EF50s were not significantly increased until 14-d after BMSCs when they were still lower than that of veh-treated rats (p < 0.001). When stable antihyperalgesia had been established, post-treatment with Lipo-Clo at 5d after BMSC infusion rekindled hyperalgesia between 8-21 d after BMSC (Fig. 3b). The MOR mRNAs were also significantly reduced in Lipo-Clo-treated rats (Fig. 3c).
The role of monocyte/macrophage in BMSC’s antihyperalgesia. Liposome-encapsulated clodronate (Lipo-Clo) was injected i.p. 3 times in three days (10 mg/2 ml/injection/rat). (a,b) Lipo-Clo treatment attenuated BMSC-produced antihyperalgesia (a, pretreatment, b, post-treatment). Compared to Veh-treated rats, Lipo-Clo treatment led to a reduction in EF50. Veh: Phosphate buffered saline-filled liposome. Error bars are 95% confidence intervals. *p < 0.05, **p < 0.01, ***p < 0.001, vs. 14d-TL; #p < 0.01, ###p < 0.001, vs. veh. n = 5-9/Group. (c) RVM MOR mRNA levels were reduced in Lipo-Clo-treated rats (Sample taken at 7d post-Lipo-Clo from BMSC-treated rats). P < 0.05, n = 3. (d) Flow chart of the experiments shown in (e and f). Bottom image shows the injection site in RVM. Coronal brainstem sections were stained with green fluorescent Nissl stain. Arrow indicates the injection needle track and circle shows the site of injection. (e) Injection of MC (Arrow, 10,000 cells/0.5 μl) from BMSC-treated TL animals into the RVM attenuated behavioural hyperalgesia in TL rats, as compared to MC from medium-treated TL rats. ***p < 0.001 vs. Med-MC, n = 6/Group. (f) BMSC induced changes in monocyte phenotype. RT-qPCR was performed on peripheral blood monocytes isolated from TL rats treated with primary or 20P-BMSC or culture medium. Note that four M2 macrophage related markers were upregulated in primary BMSC-treated rats. *p < 0.05, ***p < 0.001, vs. naive; #p < 0.05, ##p < 0.01, vs. medium; +p < 0.05, vs. 20 P, n = 3. Statistics: (a,b,e) Two-way ANOVA followed by post-hoc comparisons with Bonferroni corrections; (c) Unpaired, Two-tailed Student’s t-test; (f) One-way ANOVA followed by post-hoc comparisons with Bonferroni corrections.
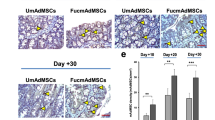
To further confirm a role of monocytes/macrophage population in BMSCs’ antihyperalgesia, we isolated peripheral blood monocytes (MC) from TL rats that received either BMSCs or culture medium treatment (Fig. 3d). Flow cytometry showed that 30.9% of gated population was positive for monocyte marker CD11b (Supplementary Fig. 6a). This population was further purified by FACS. The isolated monocytes show characteristic CD11b and CD68 immunostaining (Supplementary Fig. 6b). Direct intra-RVM injection of monocytes from BMSC-treated animals attenuated hyperalgesia, as compared to monocytes from medium-treated rats (Fig. 3d,e). The two experiments involving manipulation of monocytes/macrophages provide convergent support for the involvement of monocytes/macrophages in BMSC-induced antihyperalgesia. Interestingly, some markers of M2 macrophages showed increased mRNA expression in monocytes from primary BMSC-treated rats, including Irf4, CD206 and CD163 (Fig. 3f, left). Irf5 and Cxcl10, genes related to M1 macrophage showed decreased expression after BMSCs and Il-6 gene expression was increased in both PRI-BMSC-treated rats (Fig. 3f, right). These results suggest that BMSCs promote polarization of macrophages toward an anti-inflammatory phenotype.
Monocytes-derived CXCL1 contributes to antihyperalgesia
An intermediate role of MC in BMSC-produced antihyperalgesia raised a possibility that the pain-relieving effect of BMSCs was mediated by immune mediators from MC. We compared the gene transcription profiles of major rat inflammatory cytokines/chemokines and their receptors between MC purified from PRI- and 20P-BMSC-treated TL rats (Fig. 4a). Three genes (Ccl2, Cxcl1 and Ilr1) showed consistent higher levels of expression in three repeated arrays in MC isolated from PRI-BMSC-treated rats (Fig. 4b, Supplementary Fig. 7). Among the three genes exhibited higher levels, Cxcl1 is related to regulation and release of opioids from immune cells30, 44. Thus, we further pursued the role of CXCL1 in BMSCs’ antihyperalgesia. The increased Cxcl1 mRNA in PRI-BMSC-treated rats was further verified (Fig. 4c). We next confirmed that, in MC isolated from rats receiving Ccl4 shRNA-treated BMSCs, Cxcl1 mRNA was dramatically reduced (Fig. 4d).
CXCL1 and antihyperalgesia. (a) Flow chart of the experiment. (b) The Rat Inflammatory Cytokines PCR Array revealed an upregulation of three genes in MC purified at 1 d after treatment with PRI BMSC in 7d-TL rats, compared to that of 20P-BMSC-treated rats. (c) q-PCR confirmed the upregulation of Cxcl1 in MC. Compared to medium-(Med) and 20 P BMSC treatments, PRI-BMSC induced an increase in Cxcl1 mRNA levels. *p < 0.05, vs. Med and 20 P, n = 3. (d) Cxcl1 mRNA expression was reduced in MC of rats treated with BMSCs transduced with Ccl4 shRNA lentivirus, compared to Ctrl shRNA treatment (n = 3, RT-qPCR). *p < 0.05, vs. ctrl shRNA. (e) Antibody array (ARY008, R&D) was performed on serum isolated from naïve, medium- or PRI BMSC-treated rats. There was an increased CXCL1 expression in PRI-BMSC-treated rats. CNTF (ciliary neurotrophic factor) was an example of proteins that did not show changes in expression. RS, reference spot, coated with an irrelevant biotinylated protein to show Streptavidin-HRP reaction. *p < 0.05, vs. Naïve and Med, n = 3. (f) Direct injection of serum (Arrow, 0.5 μl) isolated from BMSC-treated animals (BMSC-Serum) into the RVM attenuated behavioral hyperalgesia in TL rats, as compared to serum from medium-treated rats (Med-Serum). Incubation of BMSC-Serum with anti-CXCL1 antibody (ab) attenuated its antihyperalgesic effect. ***p < 0.001, vs. Med-Serum and BMSC-Serum + ab, n = 5-6/Group. (g). RVM MOR mRNA levels were increased in rats treated with serum isolated from BMSC-treated TL rats, compared to Med-Serum-treated rats. Sample taken at 7 d post-serum injection. *p < 0.05, n = 3. Statistics: (b,c,e) One-way ANOVA followed by post-hoc comparisons with Bonferroni corrections. (d,g) Unpaired, Two-tailed Student’s t-test. (f) Two-way ANOVA followed by post-hoc comparisons with Bonferroni corrections.
CXCL1 can cross the blood-brain barrier51. Selective upregulation of CXCL1 in monocytes suggests that CXCL1 may be released and accesses the CNS to relay the effect of BMSCs. To test this possibility, we isolated serum from TL rats that received BMSCs or control medium treatment and observed an increase in CXCL1 in the serum derived from PRI-BMSC treated rats (Fig. 4e). Further, direct intra-RVM injection of the serum from BMSC-treated rats similarly attenuated hyperalgesia (Fig. 4f). Pre-incubation of BMSC-serum with anti-CXCL1 antibody significantly attenuated antihyperalgesia of BMSC-serum (Fig. 4g). Consistently, MOR mRNAs in the RVM were upregulated in rats treated with serum isolated from PRI-BMSC-treated rats (Fig. 4f).
CXCR2 signaling in RVM contributes to BMSC-produced antihyperalgesia
CXCL1 belongs to the CXC chemokine family and signals through its receptor CXCR2. CXCR2 signaling triggers opioid release from immune cells and induces analgesia30. Although CXCR2 is also localized in the CNS52, 53, there has been no report on potential role of CXCR2 in descending pain modulation. This prompted us to explore whether CXCL1-CXCR2 signaling is involved in central mechanisms of BMSC-produced antihyperalgesia. We first examined whether CXCR2 was localized in the RVM. CXCR2-NeuN double immunostaining showed that CXCR2 was localized in RVM neurons (Fig. 5a). However, CXCR2 did not show double immunostaining with microglia marker Iba-1 (Fig. 5b, left) and astroglia marker GFAP (Fig. 5b, right). CXCR2 immunoreactivity was detected in MOR-containing neurons (Fig. 5c), indicating their colocalization in RVM. In other brain regions examined, CXCR2 immunoreactivity was found in the trigeminal ganglion, subnucleus caudalis of the spinal trigeminal complex, periaqueductal gray, but not in the periventricular nucleus of the hypothalamus (data not shown). CXCR2 immunostaining and Western blot showed that CXCR2 was upregulated in RVM at 1w and 8w after BMSC infusion (Fig. 5d,e). Further analysis of CXCL1 in cerebrospinal fluid (CSF) showed that BMSC treatment led to increased CXCL1 levels, compared to medium-treated rats (Fig. 5f), supporting increased CXCL1-CXCR2 signaling in the brain after BMSC infusion.
Co-localization of CXCR2 with MOR and BMSC-induced upregulation of CXCR2 in the RVM and CXCL1 in cerebrospinal fluid (CSF). (a) Double immunostaining showing localization of CXCR2-like immunoreactivity (red) in RVM neurons (NeuN, green). Small rectangles on the left are enlarged to the right, illustrating examples of double-labeled neurons (arrows). (b) Lack of colocalization of CXCR2-immunoreactivity with glial markers Iba-1 (microglia) and GFAP (astroglia). (c) Colocalization of CXCR2-immunoreactivity with MOR in RVM. For (a,b,c) Scale = 0.05 mm. (d) Top four images show increased CXCR2-immunoreacitivty in RVM at 1w and 8 w after primary BMSC infusion in TL rats, compared to medium-infused rats. Bottom images show CXCR2 immunostaining in naïve rats and wide type (WT) mice and loss of staining after incubation with blocking peptide for anti-CXCR2 antibody and in CXCR2 knockout mice. Scale = 0.1 mm. (e) TL rats received primary BMSCs or culture medium at 7d post injury and RVM tissues were collected. An example of western blot is shown on top and the relative protein levels are shown in the bottom. β-actin was a loading control. CXCR2 proteins were upregulated in RVM at 1w and 8w after injection of BMSC. ***p < 0.001, vs. Med, n = 4/group. Cropped gel images are shown. See Supplementary Figure 9 for full-length blots. (e) TL rats received primary BMSC or culture medium at 7d post injury and CSF was collected. Compared to medium-treated rats, CXCL1 proteins were increased in CSF at 1w and 8w after injection of BMSC. **p < 0.01; ***p < 0.001, vs. Med, n = 4/group. Statistics: One-way ANOVA followed by post-hoc comparisons with Bonferroni corrections.
We then examined whether CXCR2 in the RVM plays a role in BMSC-produced antihyperalgesia. We first tested the effect of two CXCR2 antagonists SB225002 and NVP CXCR2 20 (NVP). SB225002 (100 pmol/500 nl) or NVP (200 pmol/500 nl) was injected into the RVM at 1w and 8w after infusion of BMSCs when EF50 on the injured side was elevated. Both antagonists produced a significant reduction of EF50 at the 3 h time point and NVP also reduced EF50 at 1 h (Fig. 6a,b), indicating attenuation of antihyperalgesia. Injection of NVP into the site dorsal to the RVM did not affect BMSC-produced antihyperalgesia (n = 4) (Supplementary Fig. 8). We then employed shRNA of Cxcr2 in RVM. Pretreatment with Cxcr2 shRNA Lentivirus significantly attenuated BMSC-produced antihyperalgesia (Fig. 6c). Transduction of RVM with Cxcr2 shRNA Lentivirus at 8w post-BMSC significantly decreased EF50 (Fig. 6d), suggesting rekindling of hyperalgesia. Knockdown of CXCR2 by RNAi of Cxcr2 in RVM was shown by western blot (Fig. 6e). MOR mRNA levels were decreased after CXCR2 knockdown (Fig. 6f). Finally, we tested the effect of BMSCs in CXCR2 knockout mice. The chronic constriction injury of the infraorbital nerve (CCI-ION)54 was produced in mice to induce persistent pain since the mouse masseter tendon was thin and vulnerable to manipulation. We have shown that BMSC attenuated pain hypersensitivity in the CCI-ION model5. We did not observe an antihyperalgesic effect of BMSCs in CXCR2 knockout mice while BMSC produced pain relief in the control wild type mice (Fig. 6g). These results suggest that CXCL1-CXCR2 signaling contributes to BMSC-produced long-lasting antihyperalgesia.
Role of RVM CXCR2 in BMSC-produced antihyperalgesia. (a,b) Attenuation of BMSC-induced antihyperalgesia by a CXCR2 antagonists SB225002 and NVP CXCR2 20 (NVP) injected into the RVM at 1w (a) and 8w (b) post-BMSC injection. *-***p < 0.05-0.001, p < 0.01; vs. Veh. (c) Cxcr2 shRNA Lentivirus was microinjected into the RVM at 3d after TL and BMSCs were infused i.v. at 10d post-siRNA. Pretreatment with RNAi of Cxcr2 attenuated BMSC-produced antihyperalgesia. (d) Cxcr2 shRNA Lentivirus was microinjected into the RVM at 8w after BMSC infusion when antihyperalgesia is present. RNAi of Cxcr2 led to a reduction of EF50, or rekindle of hyperalgesia. ***p < 0.001, vs. Ctrl shRNA. (e) Western blot illustrating knock-down of CXCR2 in RVM after RNAi. Samples taken at 2w post-shRNA injection. **p < 0.01, n = 4. Cropped gel images are shown. See Supplementary Figure 9 for full-length blots. (f) RVM MOR mRNA levels were decreased in rats treated with Cxcr2 shRNA, compared to Ctrl shRNA-treated rats. Sample taken at 2w post-shRNA injection. *p < 0.05, n = 4. (g) Mice received chronic constriction injury of the infraorbital nerve (CCI-ION) to induce hyperalgesia. The antihyperalgesic effect of BMSC was absent in the CXCR2 knockout mice. *p < 0.05, **p < 0.01, ***p < 0.001, vs. CXCR2-wt. (a–d,g) Error bars are 95% confidence intervals, n = 6–8/group; (e,f) Error bars are S.E.M., n = 5/group. (h) Summary diagram of immune interactions of BMSCs in producing pain relief. Note reciprocal interactions between BMSCs and host immune cells and autocrine signaling of BMSCs (curved arrows). Immune cells may also directly release opioid peptide and contribute to pain relief through peripheral nervous system (PNS). The role of peripheral opioid in the BMSC-produced pain relief was not studied. Statistics: (a–d,g) Two-way ANOVA followed by post-hoc comparisons with Bonferroni corrections. (e,f) Unpaired, Two-tailed Student’s t-test.
Discussion
We have studied the mechanisms of BMSC-produced antihyperalgesia from a novel immune regulation and endogenous opioid perspective. Our first major finding was that, together with a pain-attenuating effect, BMSCs induced selective upregulation of MOR in the RVM, a key site for endogenous pain modulation. The finding is consistent with our hypothesis that endogenous opioids are involved in BMSCs’ antihyperalgesia5. This effect of BMSCs may be a global phenomenon since MOR in other pain-related regions also showed upregulation (unpublished observations). The ability of BMSCs to engage the endogenous opioid system has important implications since there has been great interest in searching for ways of activating the endogenous system for pain relief.
Importantly, we show that BMSC-produced long-lasting pain relief involved their interactions with immune cells and subsequent release of immune mediators (Fig. 6h). Our findings suggest that the maintenance of antihypergesia could be achieved by persistent chemokine signaling in the CNS. This may explain the discrepancy between the BMSCs’ lengthy pain-relieving effect and their relatively short survival in the host after systemic transplantation. In the capacity of therapeutic use of MSCs other than structural repair and replacement, more attention needs to be directed on their role as immune modulators.
Our results indicate that chemotactic interactions with host immune cells are key to BMSCs’ lasting pain relief. Compared to 20P-BMSCs that are ineffective, a number of chemokines and receptors exhibited higher levels of gene expression in pain-relieving primary BMSCs (also see ref. 29). Deletion of Ccl4 and antagonism of CCR2 signaling in BMSCs significantly attenuated their ability to produce antihyperalgesia and MOR upregulation. Both CCL4-CCR5 and CCL2-CCR2 signaling pathways are involved in monocyte chemotaxis32, 40. Thus, chemotactic interactions in the circulation may occur immediately after BMSC infusion and subsequent down-stream effect in host immune cells are critical of BMSCs’ antihyperalgesia. It should be cautioned that potential roles of additional chemokines cannot be ruled out since chemokines function in a redundant and overlapping fashion55 and in vivo interactions of BMSCs should involve a cohort of chemoattractants and their receptors.
Thus, BMSC-derived mediators apparently require collaboration of host immune system in producing antihyperaglesia. Our monocytes/macrophages depletion experiments suggest that monocytes/macrophages are targeted by BMSCs to relay their biological effect. After systemic infusion, BMSCs travel to the lungs and show close relationship to macrophages22, suggesting a site of interaction between BMSCs and monocytes/macrophages. Monocytes from BMSC-treated animals exhibited selective upregulation of CXCL1 chemokine that is related to opioid release from immune cells30, 44. Intriguingly, CXCL1 also showed an increased level in the serum and CSF derived from BMSC-treated TL rats and direct injection of this serum upregulated MOR in RVM and mimicked BMSC’s antihyperalgesia. This raises a possibility that BMSC-induced immune mediators may access the brain to facilitate antihyperalgesia. Indeed, CXCL1 readily penetrates the blood brain barrier to reach the brain parenchyma in a matter of minutes51.
CXCL1 initiates its biological effect through the receptor CXCR2 that is also localized in the CNS52, 53. Antagonism of CXCR2 in RVM counteracted BMSC-produced MOR upregulation and antihyperalgesia, suggesting a critical role of CXCL1-CXCR2 signaling in BMSC-produced pain relief. Relevant to these observations, CXCL1 is neuroprotective during autoimmune demyelination56, facilitates opioid analgesia43, and potentially antinociceptive against neuropathic pain57. We noticed that studies have shown hyperalgesic action of CXCL1-CXCR2 signaling52, 58, 59. These phenomena should be understood with a view that the same immune mediators involved in pain sensitization may also be neuroprotective and promote pain relief under certain conditions60, 61. Similar dual roles of the same mediator in pain and analgesia have also been observed. Glucocorticoids compounds are anti-inflammatory through activation of their receptors, but activation of glucocorticoid receptors may also be proinflammatory and pronociceptive after injury62. Endothelin-B receptors are pro-algesic along with the ability to activate analgesic pathway63. While the anti-inflammatory cytokines and receptors Tgfβ, IL10 and IL10ra showed higher expression in primary BMSCs, consistent with BMSCs’ pain relieving effect, genes of proinflammatory cytokines Tnf, IL1β and IL18 and complement components C3 and C5 also exhibited higher levels of expression in primary BMSCs. In monocytes isolated from BMSC-treated rats, proinflammatory CCL2 and IL1R showed higher levels of expression. The presence of these inflammatory factors may contribute to the effect of BMSCs by promoting chemotactive interactions of BMSCs with immune cells21. Further, TNF may stimulate MOR gene expression in neurons42 and CXCR2 related ligands CXCL1/2/5 may induce opioid release from peripheral immune cells43.
Although our results suggest positive interactions between CXCR2 and MOR, this is rather unexpected. The interaction between chemokine receptors and opioid receptors often leads to heterologous desensitization involving formation of heterodimers64, although CXCR2 has been shown not involved in MOR desensitization65. The nature of potential interactions between CXCL1-CXCR2 signaling and MOR in the event of BMSC intervention under injurious conditions requires further study.
Methods
Animals
Sprague-Dawley rats (200-250 g) were purchased from Harlan, Indianapolis, IN. GFP transgenic S-D rats [SD-Tg(GFP)Bal] were purchased from University of Missouri Rat Resource and Research Center. The breeder pair CXCR2 knockout [C.129S2(B6)-Cxcr2tm1Mwm/J] and wild type control (BALB/c) mice were from The Jackson laboratory and bred in the Animal Facility of the University of Maryland School of Dentistry. Genotyping was performed by Geno Typing Center of America (Bangor, ME). All behavioral tests were conducted under blind conditions. The rat brain atlas66 was referred to for identifying and approaching brain structures. All experiments were carried out in accordance with the National Institute of Health Guide for the Care and Use of Laboratory Animals (NIH Publications No. 80-23) and approved by the University of Maryland, Baltimore, Institutional Animal Care and Use Committee, School of Dentistry and School of Medicine.
Data analysis
Power analyses were performed based on our previous data to determine the necessary number of animals needed to provide an 80% chance to achieve statistical significance (alpha = 0.05) and minimal number of animals were used in some experiments when statistical significance was achieved. Data are presented as mean (95% confidence interval) for EF50s and mean ± S.E.M. for other data. Statistical comparisons were made by ANOVA followed by post-hoc comparisons with Bonferroni corrections. For unbalanced sample size, multiple regressions were performed and Type III sum-of-squares was used to calculate P values (GraphPad Prism). For animals that were subject to repeated testing, ANOVA with repeated measures was used. P < 0.05 was considered significant for all cases.
Additional Methods are available in the online version of the paper.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Drela, K., Siedlecka, P., Sarnowska, A. & Domanska-Janik, K. Human mesenchymal stem cells in the treatment of neurological diseases. Acta Neurobiol. Exp. (Wars) 73, 38–56 (2013).
Franchi, S. et al. Adult stem cell as new advanced therapy for experimental neuropathic pain treatment. Biomed. Res. Int 2014, 470983 (2014).
Guo, W., Imai, S., Dubner, R. & Ren, K. Multipotent stromal cells for arthritic joint pain therapy and beyond. Pain Manag 4, 153–162 (2014).
Chen, G., Park, C. K., Xie, R. G. & Ji, R. R. Intrathecal bone marrow stromal cells inhibit neuropathic pain via TGF-b secretion. J. Clin. Invest. 125, 3226–3240 (2015).
Guo, W. et al. Bone marrow stromal cells produce long-term pain relief in rat models of persistent pain. Stem Cells 29, 1294–1303 (2011).
Hua, Z. et al. Mesenchymal Stem Cells Reversed Morphine Tolerance and Opioid-induced Hyperalgesia. Sci. Rep 6, 32096, doi:10.1038/srep32096 (2016).
Sacerdote, P. et al. Systemic administration of human adipose-derived stem cells reverts nociceptive hypersensitivity in an experimental model of neuropathy. Stem Cells Dev 22, 1252–1263 (2013).
Siniscalco, D. et al. Long-lasting effects of human mesenchymal stem cell systemic administration on pain-like behaviors, cellular, and biomolecular modifications in neuropathic mice. Front. Integr. Neurosci 5, 79 (2011).
Vickers, E. R., Karsten, E., Flood, J. & Lilischkis, R. A preliminary report on stem cell therapy for neuropathic pain in humans. J. Pain Res 7, 255–263 (2014).
Pettine, K. A., Murphy, M. B., Suzuki, R. K. & Sand, T. T. Percutaneous injection of autologous bone marrow concentrate cells significantly reduces lumbar discogenic pain through 12 months. Stem Cells 33, 146–156 (2015).
Dayan, V. et al. Mesenchymal stromal cells mediate a switch to alternatively activated monocytes/macrophages after acute myocardial infarction. Basic Res. Cardiol. 106, 1299–1310 (2011).
Harting, M. T. et al. Intravenous mesenchymal stem cell therapy for traumatic brain injury. J. Neurosurg. 110, 1189–1197 (2009).
Lee, R. H. et al. Intravenous hMSCs improve myocardial infarction in mice because cells embolized in lung are activated to secrete the anti-inflammatory protein TSG-6. Cell Stem Cell 5, 54–63 (2009).
Bai, L. et al. Human bone marrow-derived mesenchymal stem cells induce Th2-polarized immune response and promote endogenous repair in animal models of multiple sclerosis. Glia 57, 1192–1203 (2009).
Chen, J. et al. Therapeutic benefit of intravenous administration of bone marrow stromal cells after cerebral ischemia in rats. Stroke 32, 1005–1011 (2001).
Park, B. N. et al. Early distribution of intravenously injected mesenchymal stem cells in rats with acute brain trauma evaluated by (99m)Tc-HMPAO labeling. Nucl. Med. Biol. 38, 1175–1182 (2011).
Mitkari, B. et al. Intra-arterial infusion of human bone marrow-derived mesenchymal stem cells results in transient localization in the brain after cerebral ischemia in rats. Exp. Neurol. 239, 158–162 (2013).
Augello, A., Tasso, R., Negrini, S. M., Cancedda, R. & Pennesi, G. Cell therapy using allogeneic bone marrow mesenchymal stem cells prevents tissue damage in collagen-induced arthritis. Arthritis Rheum. 56, 1175–1186 (2007).
Pluchino, S. & Cossetti, C. How stem cells speak with host immune cells in inflammatory brain diseases. Glia 61, 1379–1401 (2013).
Heldring, N., Mäger, I., Wood, M. J., Le Blanc, K. & Andaloussi, S. E. Therapeutic Potential of Multipotent Mesenchymal Stromal Cells and Their Extracellular Vesicles. Hum Gene Ther 26, 506–517 (2015).
Moll, G. et al. Mesenchymal stromal cells engage complement and complement receptor bearing innate effector cells to modulate immune responses. PLoS One 6, e21703 (2011).
Németh, K. et al. Bone marrow stromal cells attenuate sepsis via prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat. Med 15, 42–49 (2009).
Fox, J. M., Chamberlain, G., Ashton, B. A. & Middleton, J. Recent advances into the understanding of mesenchymal stem cell trafficking. Br. J. Haematol. 137, 491–502 (2007).
Noël, D., Djouad, F., Bouffi, C., Mrugala, D. & Jorgensen, C. Multipotent mesenchymal stromal cells and immune tolerance. Leuk. Lymphoma 48, 1283–1289 (2007).
Ren, K. & Dubner, R. Interactions between the immune and nervous systems in pain. Nat. Med 16, 1267–1276 (2010).
Guo, W. et al. Further observations on the behavioral and neural effects of bone marrow stromal cells in rodent pain models. Mol Pain. 2016, doi:10.1177/1744806916658043 (2016).
Corder, G. et al. Constitutive μ-opioid receptor activity leads to long-term endogenous analgesia and dependence. Science 341, 1394–1399 (2013).
Mothe, A. J. et al. Analysis of green fluorescent protein expression in transgenic rats for tracking transplanted neural stem/progenitor cells. J. Histochem. Cytochem. 53, 1215–1226 (2005).
Honczarenko, M. et al. Human bone marrow stromal cells express a distinct set of biologically functional chemokine receptors. Stem Cells 24, 1030–1041 (2006).
Rittner, H. L., Brack, A. & Stein, C. Pain and the immune system. Br. J. Anaesth 101, 40–44 (2008).
Schaffner, A., Rhyn, P., Schoedon, G. & Schaer, D. J. Regulated expression of platelet factor 4 in human monocytes–role of PARs as a quantitatively important monocyte activation pathway. J. Leukoc. Biol. 78, 202–209 (2005).
Koch, A. E. et al. Macrophage inflammatory protein-1 beta: a C-C chemokine in osteoarthritis. Clin. Immunol. Immunopathol. 77, 307–314 (1995).
Tanaka, Y. et al. T-cell adhesion induced by proteoglycan-immobilized cytokine MIP-1 beta. Nature 361, 79–82 (1993).
Sohy, D. et al. Hetero-oligomerization of CCR2, CCR5, and CXCR4 and the protean effects of “selective” antagonists. J. Biol. Chem. 284, 31270–31279 (2009).
Guan, E., Wang, J. & Norcross, M. A. Identification of human macrophage inflammatory proteins 1alpha and 1beta as a native secreted heterodimer. J. Biol. Chem. 276, 12404–12409 (2001).
Bleul, C. C. et al. A highly efficacious lymphocyte chemoattractant, stromal cell-derived factor 1 (SDF-1). J. Exp. Med. 184, 1101–1109 (1996).
Abbott, J. D. et al. Stromal cell-derived factor-1alpha plays a critical role in stem cell recruitment to the heart after myocardial infarction but is not sufficient to induce homing in the absence of injury. Circulation 110, 3300–3305 (2004).
Belema-Bedada, F., Uchida, S., Martire, A., Kostin, S. & Braun, T. Efficient homing of multipotent adult mesenchymal stem cells depends on FROUNT-mediated clustering of CCR2. Cell Stem Cell 2, 566–575 (2008).
Karp, J. M. & Leng Teo, G. S. Mesenchymal stem cell homing: the devil is in the details. Cell Stem Cell 4, 206–216 (2009).
Shi, C. & Pamer, E. G. Monocyte recruitment during infection and inflammation. Nat. Rev. Immunol. 11, 762–774 (2011).
Crown, S. E., Yu, Y., Sweeney, M. D., Leary, J. A. & Handel, T. M. Heterodimerization of CCR2 chemokines and regulation by glycosaminoglycan binding. J. Biol. Chem. 281, 25438–25446 (2006).
Liou, J. T., Yuan, H. B., Mao, C. C., Lai, Y. S. & Day, Y. J. Absence of C-C motif chemokine ligand 5 in mice leads to decreased local macrophage recruitment and behavioral hypersensitivity in a murine neuropathic pain model. Pain 153, 1283–1291 (2012).
Kraus, J., Börner, C., Giannini, E. & Höllt, V. The role of nuclear factor kappaB in tumor necrosis factor-regulated transcription of the human mu-opioid receptor gene. Mol. Pharmacol. 64, 876–884 (2003).
Brack, A. et al. Control of inflammatory pain by chemokine-mediated recruitment of opioid-containing polymorphonuclear cells. Pain. 112, 229–238 (2004).
Ren, K. An improved method for assessing mechanical allodynia in the rat. Physiol. Beh 67, 711–716 (1999).
Charo, I. F. & Ransohoff, R. M. The many roles of chemokines and chemokine receptors in inflammation. N. Engl. J. Med. 9(354), 610–621 (2006).
Brack, A. et al. Tissue monocytes/macrophages in inflammation: hyperalgesia versus opioid-mediated peripheral antinociception. Anesthesiology 101, 204–211 (2004).
Van Rooijen, N. & Sanders, A. Liposome mediated depletion of macrophages: mechanism of action, preparation of liposomes and applications. J. Immunol. Methods 174, 83–93 (1994).
Sunderkotter, C. et al. Subpopulations of mouse blood monocytes differ in maturation stage and inflammatory response. J. Immunol. 172, 4410–4417 (2004).
Kitamoto, K. et al. Effects of liposome clodronate on renal leukocyte populations and renal fibrosis in murine obstructive nephropathy. J. Pharmacol. Sci. 2009(111), 285–292 (2009).
Pan, W. & Kastin, A. J. Changing the chemokine gradient: CINC1 crosses the blood-brain barrier. J. Neuroimmunol. 115, 64–70 (2001).
Chen, G. et al. Connexin-43 induces chemokine release from spinal cord astrocytes to maintain late-phase neuropathic pain in mice. Brain 137, 2193–2209 (2014).
Tsai, H. H. et al. The chemokine receptor CXCR2 controls positioning of oligodendrocyte precursors in developing spinal cord by arresting their migration. Cell 110, 373–383 (2002).
Wei, F., Guo, W., Zou, S., Ren, K. & Dubner, R. Supraspinal glial-neuronal interactions contribute to descending pain facilitation. J. Neurosci. 28, 10482–10495 (2008).
Kraemer, S., Alampour-Rajabi, S., El Bounkari, O. & Bernhagen, J. Hetero-oligomerization of chemokine receptors: diversity and relevance for function. Curr. Med. Chem. 20, 2524–2536 (2013).
Omari, K. M., Lutz, S. E., Santambrogio, L., Lira, S. A. & Raine, C. S. Neuroprotection and remyelination after autoimmune demyelination in mice that inducibly overexpress CXCL1. Am. J. Pathol. 174, 164–176 (2009).
Malon, J. T. & Cao, L. Potential anti-nociceptive role of chemokine CXCL1 in peripheral nerve injury-induced neuropathic pain. J Immunol. 196, (1 Supplement) 51.4 (2016).
Lorenzetti, B. B. et al. Cytokine-induced neutrophil chemoattractant 1 (CINC-1) mediates the sympathetic component of inflammatory mechanical hypersensitivitiy in rats. Eur. Cytokine Netw. 13, 456–461 (2002).
Sun, Y. et al. Epigenetic regulation of spinal CXCR2 signaling in incisional hypersensitivity in mice. Anesthesiology. 119, 1198–1208 (2013).
Milligan, E. D. & Watkins, L. R. Pathological and protective roles of glia in chronic pain. Nat. Rev. Neurosci. 10, 23–36 (2009).
Ren, K. & Dubner, R. Activity-triggered tetrapartite neuron-glial interactions following peripheral injury. Curr. Opin. Pharmacol. 26, 16–25 (2016).
Wang, S., Lim, G., Zeng, Q., Sung, B., Yang, L. & Mao, J. Central glucocorticoid receptors modulate the expression and function of spinal NMDA receptors after peripheral nerve injury. J. Neurosci. 25, 488–495 (2005).
Khodorova, A., Zou, S., Ren, K., Dubner, R., Davar, G. & Strichartz, G. Dual Roles for Endothelin-B Receptors in Modulating Adjuvant-Induced Inflammatory Hyperalgesia in Rats. Open Pain J 2, 30–40 (2009).
Steele, A. D., Szabo, I., Bednar, F. & Rogers, T. J. Interactions between opioid and chemokine receptors: heterologous desensitization. Cytokine Growth Factor Rev 13, 209–222 (2002).
Szabo, I. et al. Heterologous desensitization of opioid receptors by chemokines inhibits chemotaxis and enhances the perception of pain. Proc. Natl. Acad. Sci. USA 99, 10276–10281 (2002).
Paxinos, G. & Watson, C. The rat brain in stereotaxic coordinates. Seventh ed. (Amsterdam, Netherlands: Elsevier) (2014).
Acknowledgements
This work was supported by Maryland Stem Cell Foundation grant 2014-MSCRFI-0584 (KR); National Institutes of Health grants: DE11964, DE025137 (KR), NS019296 (FW), DE021804 (RD). YXC was supported by National Natural Science Foundation of China (No. 31600852). We thank Dr. George T-J Huang for his advice on the early stages of this project and Dr. Guang Bai for his advice on biochemical analysis.
Author information
Authors and Affiliations
Contributions
W.G., S.I.: conception and design, BMSC cultures, collection and assembly of behavioral, PCR and western blot data, data analysis and interpretation, manuscript writing. J.-L.Y.: immunohistochemical data collection and analysis. S.Z., Y.-X.C. and Z.M.: collection and assembly of behavioral data. M.W.: tracing GFP-labeled BMSC experiments. H.K. BMSC procedures and design. K.D.M. immune cell procedures and design. F.W., R.D. and K.R. conception and design, data analysis and interpretation, and manuscript writing. All authors gave final approval of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guo, W., Imai, S., Yang, JL. et al. In vivo immune interactions of multipotent stromal cells underlie their long-lasting pain-relieving effect. Sci Rep 7, 10107 (2017). https://doi.org/10.1038/s41598-017-10251-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-10251-y
This article is cited by
-
Potential Plausible Role of Stem Cell for Treating Depressive Disorder: a Retrospective Review
Molecular Neurobiology (2023)
-
Multilineage-differentiating stress-enduring cells alleviate atopic dermatitis-associated behaviors in mice
Stem Cell Research & Therapy (2021)
-
Exosomes in perspective: a potential surrogate for stem cell therapy
Odontology (2019)
-
The Chemokine CCL4 (MIP-1β) Evokes Antinociceptive Effects in Mice: a Role for CD4+ Lymphocytes and Met-Enkephalin
Molecular Neurobiology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.