Abstract
To determine the association of birth weight (BW) and waist circumference (WC) on cardiovascular disease (CVD). The longitudinal cohort study consisted of 745 participants who were able to provide their birth weight information and were followed from 2002 to 2014. During the follow-up, 83 events of CVD were confirmed. After adjusting for confounding factors, subjects with birth weight <2500 g were at a significantly increased CVD risk when compared to subjects with birth weight between 2500–3999 g (OR 2·47, 95%CI, 1·07–5·71). When high waist circumference (HWC), a measurement of adult obesity, was incorporated into stratifying factors according to presence or absence of low birth weight (LBW, birth weight <2500 g), adjusted CVD risk was significantly elevated in -LBW/+ HWC group (OR 1·94, 95%CI, 1·10–3·43) and marginally significantly increased in +LBW/-HWC group (OR 2·94, 95%CI, 1·00–8·64). CVD risk was highest in subjects with LBW and HWC (+LBW/+HWC), OR 4·74 (95%CI, 1·48–15·21). Higher waist circumference in adulthood is an especially strong risk factor for cardiovascular disease among those small at birth. In this cohort, birth size and adiposity in adulthood interact to predict events of cardiovascular disease.
Similar content being viewed by others
Introduction
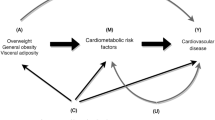
Accumulating evidence indicates that early life determinants may be important in the pathogenesis of adult disease1,2,3,4,5. In 1989, birth weight (BW) was reported to be inversely associated with the risk of dying from ischemic heart disease during adulthood6. Since then low birth weight (LBW) has been consistently confirmed as a risk factor of cardiovascular disease (CVD) by several independent studies3, 4. In the meantime, others carried on to investigate anthropometric measurements in adulthood to find better predictors7, 8. Some researchers believe that these two factors should not be treated independently, and that BW and adult body size are likely to interact with each other to increase the risk of coronary heart disease4. It was reported that waist circumference (WC) was the best predictor for CVD among the anthropometric measurements in population9. However, no thorough investigation has been done regarding the comparison and combination of WC with other early life risk factors. The present study investigated the effects of BW and WC on CVD risk by analyzing a cohort in a Chinese community with 10 years follow-up.
Results
At baseline, a total of 1010 individuals provided their BW information from birth certification and hospital case records. Among them, 745 participants (283 males and 462 females) were followed and were enrolled in this study. The mean follow-up time was 10·9 years (10·5y–12·0y). From 2002 to 2014, we confirmed 83 cardiovascular events.
The mean values of anthropometric data and metabolic parameters in 2002 were presented in Table 1 according to BW subgroups. Within this cohort, significant discrepancies were demonstrated among groups concerning gender distribution, WC, incidence of diabetes, baseline glycemic level, cigarettes use, while incidence of hypertension, baseline blood pressure, lipid level, alcohol use and economic status were similar between groups. Furthermore, because about 1/4 individuals were lost to follow up, we compared the participants who attended follow-up with those who were lost and found no significant differences in BW, glucose levels, blood lipid profile, blood pressure and any other factors between these two groups (data not shown).
During the follow up, 83 (11·1%) events of CVD were confirmed through the health records. The corresponding incidence rates of CVD in BW < 2500 g group, BW among 2500–3999 g group, and BW ≥400 0 g group were 24·4%, 9·9% and 17·1%, respectively. As shown in Table 2, risk of CVD was lowest in the BW among 2500 g –3999 g group (reference group) and was highest with lower BW (adjusted OR 2·73, 95%CI, 1·20 to 6·25). Individuals with BW equaled to or exceeded 4000 g bore similar risks to those in the reference group (adjusted OR 2·31, 95%CI, 0·84 to 6·30). Findings were confirmed in the additional models with BW dichotomized (BW < 2500 g vs. BW ≥250 0 g), showing adjusted hazard ratio of 2·87 (95% CI 1·28–6·42) in the group with BW < 2500 g.
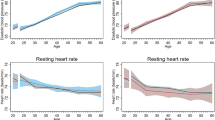
Table 3 shows all the significant contributing factors to increased CVD risk in multivariate analyses after adjusted for age, sex, diabetes status, hypertension status, lipid profile, waist circumference, drinking and smoking status, physical activity at baseline in our study. Female, older age, lower high-density lipoprotein cholesterol (HDL-c) and higher total cholesterol (TC) were all related to higher odds of CVD compared with their counterparts. Most importantly, both BW subgroups and WC were significantly associated with risk of CVD. Every 1-centimeter increase in WC was associated with a 3.2% increase in risk for developing CVD.
Overall prevalence of high waist circumference (HWC) was 19·7% in the present analyses. In order to examine the influence of BW and adult WC on cardiovascular disease, we identified individuals with BW < 2500 g as LBW (+) group, and the others as LBW (−) group. As is shown in Table 4, compared with subjects without LBW and HWC (-LBW/-HWC, reference group), both subjects with isolated LBW (+LBW/-HWC) and adult obesity (−LBW/+HWC) were significantly related to increased risk of CVD, demonstrating adjusted OR of 2·94 (95%CI 1·00–8·64) and 1·94 (95%CI, 1·10–3·43), respectively. Surprisingly, the risk for developing CVD was highest in subjects with LBW and HWC, up to 4·74 times when compared with that in the reference group, and still much higher than that in any of the isolated condition.
Discussion
The present analysis demonstrated that subjects with LBW and HWC in adulthood were associated with the increased risk of CVD after controlling for potential confounders. Subjects with LBW and HWC in adulthood are associated with higher risk of CVD, up to 4·74 times when compared with those without LBW and HWC. These findings suggest that both LBW and adult HWC could be simple and practical predictors of unfavorable CVD outcomes in the general population.
BW is inversely associated with CVD risk factors such as raised blood pressure, dyslipidemia, and glucose intolerance10,11,12,13. But only a small number of studies have demonstrated an association between BW and CVD outcomes, which is considered of greater importance than showing that size at birth is related to risk factors3, 4, 14, and even fewer have looked at this association in population-based Chinese study. Our study is based on general population from a wide range of age distribution, and supports the importance of both BW and adult WC in predicting CVD.
Adjustment for adult WC did not change the association between BW and CVD in the present analysis. Subjects with LBW exhibited higher risk for CVD, while subjects with high birth weight (BW ≥ 4000 g) showed similar risk when compared with those with normal BW (2500–3999 g). Our results support a previous analysis that the risk of coronary heart disease increased linearly for subjects with BW below 3·4 kg and reached 1·28 (95% CI: 1·13 to 1·44) with BW at 2 kg. The association weakened with BW above 3·4 kg, and there was virtually no association when subjects with BW from about 4 kg15.
In our study, using logistic regression model showed that age, sex, HDL-c and TC at baseline, BW and WC were factors contributing to the development of CVD consistent with many studies16,17,18,19. Previous investigators suggested that BW and adult body size could not be investigated independently4, while comparison and combination of WC with early life risk factors were very limited. Therefore we stratified BW and WC to investigate their effects on CVD risk.
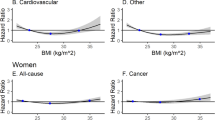
The present analysis indicated that risk of CVD was highest among those who were smaller at birth and grew up to become adults with high waist circumference. A moderate but consistent association between LBW and cardiovascular risk was found when studying the influence of adult body size and birth size on predicting CVD. Previous studies have demonstrated how growth during infancy, childhood, and adulthood modifies the increased risk of coronary heart disease associated with small body size at birth3, 20,21,22,23. In a Finland hospital-based study, after age 1 year, rapid weight gain is associated with further increase in risk of coronary heart disease, but only among boys who were thin at birth. In these boys the adverse effects of rapid weight gain on later coronary heart disease are already apparent at age 3 years21. Higher body mass index in adulthood is an especially strong risk factor for coronary heart disease among women who were small at birth4. Risk of coronary heart disease was especially high for women who crossed from a low centile of weight at birth to a high centile of body mass index in adulthood. In the large cohort of women, size at birth and adiposity in adulthood interacted to predict events of coronary heart disease. WC and BMI were highly correlated, and HWC itself contributed to increased CVD risk significantly21. So we choose WC, which reflects abdominal obesity and was considered highly correlated to incident CVD, in our statistical model. Previous studies were mainly conducted on populations who were born before the 1940s. In contrast, the overwhelming proportion of our population was born in or after the 1940s. Our study provide a more contemporary birth cohort to investigate the association of birth weight and waist circumference on cardiovascular disease.
Our findings are limited by several facts. Firstly, our sample size was relatively small and our follow-up rate was relatively low. However, we followed the principle of randomization in baseline enrollment to ensure the representativeness of the sample. The rigorous design and nonselective loss-to-follow-up have greatly reduced the selection bias. Because about one quarter individuals with their BW information at baseline were lost to follow up, we compared the basic characteristics in the participants who attended follow-up with those who were lost, and found no significant differences between the two groups. Secondly, our survey were performed at two time points (baseline and follow up), lacking the data of waist circumference, blood glucose and hypertension evaluation at the period that participants experienced CVD events. In addition, we can’t comment on whether premature birth was the cause of the low birthweight because of lack of the information of gestational age at the time of birth. Moreover, without the information of breastfeeding and birth length, we were unable to analyze the interplay of early growth and CVD risks. However, we demonstrated LBW in the general population could be a predictor of cardiovascular outcome. Finally, as these data are observational, they can only be used to demonstrate a strong association and cannot be interpreted to demonstrate causality.
In conclusion, our findings that birth size and adult adiposity independently predict events of cardiovascular disease have added to the evidence that protection of fetal growth is key in strategies for the primary prevention of CVD. Further benefit will come from preventing abdominal obesity in adulthood, especially for those with low birthweight.
Method
Ethics Statement
This study was approved by Ruijin Hospital Ethics Committee (Approval No. 2014–114). Written informed consent signed by each of participants and all methods were carried out in accordance with the relevant guidelines and regulations.
Study design and Subjects
This cohort was established in 2002 and the design of the study and formation of the study population has been described previously24, 25. A cross-sectional survey for the prevalence of type 2 diabetes was conducted in an urban community in Shanghai, China in 2002. A stratified multistage cluster sampling design was employed. First, four (Huoxin, Mingyuancun, Jinsheng, Jiangpu) out of 33 sectors were randomly sampled from the Pingliang community. Then, a sample of 2200 people was randomly selected from 18 000 eligible permanent inhabitants in the four sectors. Valid information was obtained from 2132 people of the sample. All subjects were permanent residents who must live in the community for above 5 years without leaving Shanghai for more than 6 months. There were no serious air pollution, chemical and metal contamination reported in Pingliang community in the past several decades.
The first examination of participants of 2132 men and women aged 18 to 76 years from Pingliang community was conducted from November 2002 to January 2003. At the baseline, all subjects were interviewed with physical examination and standardized questionnaires including information about physician-diagnosed diabetes and hypertension, family history of diabetes, educational background, lifestyle factors, such as cigarette smoking, alcohol consumption and presently used medications for hypertension and diabetes. Plasma glucose was measured during an oral glucose tolerance test (OGTT) and serum lipid profile assayed in all subjects.
The follow-up survey, consisting of 1609 participants, lasted from July to December 2013, but an additional follow-up was made in September to October 2014 for those unavailable at that time25. All participants at follow up were interviewed with the same standardized questionnaires with the addition of the information of CVD events.
At baseline, a total of 1010 individuals (389 males and 621 females) provided their birth weight information from birth certification and hospital case records24. Among them, 745 participants (283 males and 462 females) were followed (73·8%) and were enrolled in this study for analysis. The mean follow-up time was 10·9 years.
Birth weight and waist circumference assessment
LBW was defined as BW < 2500 g. WC was measured at the narrowest point below the ribs or halfway between the lowest ribs and the iliac crest in centimeters. Body weight, height and WC were respectively measured to the nearest 0·1 kg and 0·1 cm. HWC was defined as WC ≥ 85 cm in females and WC ≥ 90 cm in males26.
Documentation of end points
We considered CVD (including nonfatal coronary heart disease, nonfatal cerebrovascular disease and cardiovascular death) that occurred between baseline 2002 and October 2014 as major outcomes. Coronary heart disease was further defined as angina pectoris, myocardial infarctions, abnormal coronary arteriography, a cardiac procedure; and cerebrovascular disease includes cerebral ischemic attack, cerebral hemorrhage and cerebral infarction from any cause. Information on deaths was obtained from the official death certificates of the district. In our survey, participants firstly reported their physician-diagnosed CVD and/or medication use during follow up. Then, a physician reviewed their medical records if available. After that, a community staff check the information in the Health Records in this district and a CDC professional confirmed all 83 events in Shanghai Health Records.
Other variables of interest
Plasma glucose was measured during a 75 g oral glucose tolerance test (OGTT) and type 2 diabetes was defined by a fasting plasma glucose level ≥7.0 mmol/l and/or a 2-h postchallenge glucose level ≥11.1 mmol/l, a previous physician-diagnosed type 2 diabetes, or using antidiabetic medication at baseline. Blood pressure was measured through a mercury sphygmomanometer in sitting position after 5 minutes of rest. Hypertension was defined as the average of the blood pressure values (with a systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg), or a physician-diagnosed hypertension at baseline. Smoking and alcohol consumption, educational background, diet and physical activity were acquired through well-designed questionnaires. Assessment methods of the above variables have been specifically described elsewhere24, 25. Briefly, smoking and drinking status were classified into currently, formerly, and never consumed. Physical activity was calculated as the product of the duration and frequency of each activity (in hours per day) weighted by an estimate of the metabolic equivalent of that activity25.
Statistical analyses
All data were analyzed using SPSS for Windows, Version 18·0 (SPSS, Chicago, IL, USA).
Baseline characteristics were analyzed for significance of differences between groups using one-way analysis of variance (ANOVA) for continuous variables and the chi-squared test for categorical variables. Student’s t-test was applied for comparisons of basic characteristics in those who attended follow-up with those who were lost at follow-up. Binary logistic regression models were used to estimate the adjusted odds ratios (ORs) and 95% confidence intervals (95%CI) for CVD. The analyses were performed adjusting for adult age, sex, diabetes status, hypertension status, lipid profile, WC, smoking and drinking status, physical activity and economic status at baseline in adjusted model. The analyses were carried out to examine the influence of BW and adult WC on cardiovascular disease. Data were expressed as mean ± SD, n (%), or OR (95% CI), all statistical tests were two sided, and a p value of less than 0·05 was considered to be statistically significant.
References
Barker, D. J. The fetal origins of coronary heart disease. European heart journal 18, 883–884 (1997).
Victora, C. G. et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 371, 340–357, doi:10.1016/S0140-6736(07)61692-4 (2008).
Lawlor, D. A., Ronalds, G., Clark, H., Smith, G. D. & Leon, D. A. Birth weight is inversely associated with incident coronary heart disease and stroke among individuals born in the 1950s: findings from the Aberdeen Children of the 1950s prospective cohort study. Circulation 112, 1414–1418, doi:10.1161/CIRCULATIONAHA.104.528356 (2005).
Rich-Edwards, J. W. et al. Longitudinal study of birth weight and adult body mass index in predicting risk of coronary heart disease and stroke in women. Bmj 330, 1115, doi:10.1136/bmj.38434.629630.E0 (2005).
Wang, T. et al. Low birthweight and risk of type 2 diabetes: a Mendelian randomisation study. Diabetologia 59, 1920–1927, doi:10.1007/s00125-016-4019-z (2016).
Barker, D. J., Winter, P. D., Osmond, C., Margetts, B. & Simmonds, S. J. Weight in infancy and death from ischaemic heart disease. Lancet 2, 577–580 (1989).
Balkau, B. et al. International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation 116, 1942–1951, doi:10.1161/CIRCULATIONAHA.106.676379 (2007).
Kahn, H. S., Bullard, K. M., Barker, L. E. & Imperatore, G. Differences between adiposity indicators for predicting all-cause mortality in a representative sample of United States non-elderly adults. PloS one 7, e50428, doi:10.1371/journal.pone.0050428 (2012).
Wang, Z. & Hoy, W. E. Waist circumference, body mass index, hip circumference and waist-to-hip ratio as predictors of cardiovascular disease in Aboriginal people. European journal of clinical nutrition 58, 888–893, doi:10.1038/sj.ejcn.1601891 (2004).
Huxley, R., Neil, A. & Collins, R. Unravelling the fetal origins hypothesis: is there really an inverse association between birthweight and subsequent blood pressure? Lancet 360, 659–665, doi:10.1016/S0140-6736(02)09834-3 (2002).
Li, Y. et al. Exposure to the chinese famine in early life and the risk of metabolic syndrome in adulthood. Diabetes care 34, 1014–1018, doi:10.2337/dc10-2039 (2011).
Whincup, P. H. et al. Birth weight and risk of type 2 diabetes: a systematic review. Jama 300, 2886–2897, doi:10.1001/jama.2008.886 (2008).
Crane, J. D. et al. ELBW survivors in early adulthood have higher hepatic, pancreatic and subcutaneous fat. Scientific reports 6, 31560, doi:10.1038/srep31560 (2016).
Fan, Z. et al. Relationship between birth size and coronary heart disease in China. Annals of medicine 42, 596–602, doi:10.3109/07853890.2010.514283 (2010).
Andersen, L. G. et al. Birth weight, childhood body mass index and risk of coronary heart disease in adults: combined historical cohort studies. PloS one 5, e14126, doi:10.1371/journal.pone.0014126 (2010).
Nordestgaard, B. G. & Varbo, A. Triglycerides and cardiovascular disease. Lancet 384, 626–635, doi:10.1016/S0140-6736(14)61177-6 (2014).
Rader, D. J. & Hovingh, G. K. HDL and cardiovascular disease. Lancet 384, 618–625, doi:10.1016/S0140-6736(14)61217-4 (2014).
Klingberg, S. et al. Increase in waist circumference over 6 years predicts subsequent cardiovascular disease and total mortality in nordic women. Obesity 23, 2123–2130, doi:10.1002/oby.21203 (2015).
Huxley, R. R. et al. Age- and Sex-Specific Burden of Cardiovascular Disease Attributable to 5 Major and Modifiable Risk Factors in 10 Asian Countries of the Western Pacific Region. Circulation journal: official journal of the Japanese Circulation Society 79, 1662–1674, doi:10.1253/circj.CJ-15-0661 (2015).
Rich-Edwards, J. W. et al. Birth weight and risk of cardiovascular disease in a cohort of women followed up since 1976. Bmj 315, 396–400 (1997).
Eriksson, J. G., Forsen, T., Tuomilehto, J., Osmond, C. & Barker, D. J. Early growth and coronary heart disease in later life: longitudinal study. Bmj 322, 949–953 (2001).
Frankel, S., Elwood, P., Sweetnam, P., Yarnell, J. & Smith, G. D. Birthweight, body-mass index in middle age, and incident coronary heart disease. Lancet 348, 1478–1480, doi:10.1016/S0140-6736(96)03482-4 (1996).
Burggren, W. W. & Mueller, C. A. Developmental critical windows and sensitive periods as three-dimensional constructs in time and space. Physiological and biochemical zoology: PBZ 88, 91–102, doi:10.1086/679906 (2015).
Tian, J. Y. et al. Birth weight and risk of type 2 diabetes, abdominal obesity and hypertension among Chinese adults. Eur J Endocrinol 155, 601–607, doi:10.1530/eje.1.02265 (2006).
Qiu, M. et al. Effects of prediabetes mellitus alone or plus hypertension on subsequent occurrence of cardiovascular disease and diabetes mellitus: longitudinal study. Hypertension 65, 525–530, doi:10.1161/HYPERTENSIONAHA.114.04632 (2015).
Bao, Y. et al. Optimal waist circumference cutoffs for abdominal obesity in Chinese. Atherosclerosis 201, 378–384, doi:10.1016/j.atherosclerosis.2008.03.001 (2008).
Acknowledgements
We would like to acknowledge all staff and volunteers from three hospital who attend this study. This work was supported by the Chinese National Natural Science Foundation (81270935), Transform Medicine Innovation Foundation of Shanghai Jiao Tong University School of Medicine (15ZH2001), Research Project Funded by the Shanghai Municipal Health Bureau (20114301) and the Fund of the Key Laboratoty of Stem Cell Biology of Chinese Academy of Sciences (No. 201601).
Author information
Authors and Affiliations
Contributions
J.T., X.S., W.W. and G.N. designed the study. J.T., M.Q., X.Z., H.W., W.T., H.Z., S.Z., X.S. researched data. M.Q. analyzed data and wrote manuscript. J.T., Y.L., S.S., N.S. and G.N. reviewed/edited manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tian, J., Qiu, M., Li, Y. et al. Contribution of birth weight and adult waist circumference to cardiovascular disease risk in a longitudinal study. Sci Rep 7, 9768 (2017). https://doi.org/10.1038/s41598-017-10176-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-10176-6
This article is cited by
-
Long-term effects of blood pressure 130–139/80–89 mmHg on all-cause and cardiovascular mortality among Chinese adults with different glucose metabolism
Cardiovascular Diabetology (2023)
-
A randomized controlled trial of Baduanjin exercise to reduce the risk of atherosclerotic cardiovascular disease in patients with prediabetes
Scientific Reports (2022)
-
Birth weight and heart rate autonomic recovery following exercise in healthy term-born adults
Scientific Reports (2021)
-
Δ9-tetrahydrocannabinol exposure during rat pregnancy leads to symmetrical fetal growth restriction and labyrinth-specific vascular defects in the placenta
Scientific Reports (2020)
-
Birth Weight and Risk of Cardiovascular Disease Incidence in Adulthood: a Dose-Response Meta-analysis
Current Atherosclerosis Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.