Abstract
C-type lectin receptors (CLRs) have been demonstrated to be involved in several autoimmune diseases. The role of CLRs in Behcet’s disease (BD) is unknown and thus was the purpose of this study. A two-stage association study was carried out and a total of 766 BD patients and 1674 healthy controls were recruited. Genotyping of 14 SNPs of 13 genes in CLRs was carried out by iPLEX Gold genotyping or polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) assay. The expression of mannose binding lectin 2 (MBL2) and killer cell lectin like receptor C4 (KLRC4) was measured by Real-time PCR. Significantly increased frequencies of the A allele as well as AA genotype of rs1800450 in MBL2 (Pc = 2.50 × 10−6, OR = 1.494; Pc = 2.24 × 10−6,OR = 2.899; respectively) and TT genotype of rs2617170 in KLRC4 (Pc = 2.53 × 10−6, OR = 1.695) and decreased frequencies of GG genotype of rs1800450 (Pc = 1.56 × 10−3, OR = 0.689) and C allele as well as CC genotype of rs2617170 (Pc = 2.05 × 10−9,OR = 0.664; Pc = 1.20 × 10−5, OR = 0.585; respectively) were observed in BD. Two variants, p.Gly54Asp (rs1800450) and p.Asn104Ser (rs2617170) affect MBL2 and KLRC4 protein stability and expression. Our study demonstrates that the MBL2/rs1800450 and KLRC4/rs2617170 are susceptibility factors for BD in a Chinese Han population.
Similar content being viewed by others
Introduction
Behcet’s disease (BD) is a well-known multisystem vasculitis, characterized by recurrent uveitis, oral ulcerations, genital ulcerations and typical skin lesions1. It often occurs in young adulthood and causes serious disability and significant visual impairment. BD is more frequent among populations along the “silk route” from the Mediterranean Basin to East Asia2. Although the pathogenesis of BD is not yet exactly known, it has been hypothesized that autoimmunity and genetic factors are responsible for this disease3. Recent studies have implicated that Human Leukocyte Antigen (HLA) and non-HLA genes seem to collectively contribute to the genetic background causing this disorder among different populations4,5,6,7,8,9,10,11,12. Most of the non-HLA genes such as TNFAIP3, IL23R,-IL12RB2, IL10, CCR1, STAT4, KLRC4, ERAP1, FUT2, and IL12A have been reported with genome-wide significance whereas NOS3 and JAK1 were reported with study-wide significance.
C-type lectin receptors (CLRs) are a large group of extracellular Metazoan proteins expressed on immune cells that have been classified as pattern recognition receptors (PRRs) which play an important role in the binding of pathogens via their surface carbohydrate structures. CLRs not only play a pivotal role in the process of anti-inflammatory immune responses but also in the maintenance of host immune-homeostasis13. Growing evidence suggests that various members of CLRs are associated with severe immune mediated diseases like juvenile idiopathic arthritis (JIA)14, type 1 diabetes (T1DM)15, systemic lupus erythematosus (SLE)16, rheumatoid arthritis (RA)17 and multiple sclerosis (MS)18. It was recently shown that patients with BD had significantly lower median serum mannose-binding lectin (MBL) levels compared to healthy controls19. Whether gene polymorphisms of CLRs are associated with the susceptibility to BD is not yet known and was therefore the purpose of our study. We identified two variants, p.Gly54Asp (rs1800450) in MBL2 and p.Asn104Ser (rs2617170) in KLRC4, to contribute to the risk of developing BD.
Results
Clinical characteristics of BD patients
Clinical features, age as well as gender distribution in the recruited BD patients and healthy controls are presented in Table 1. All patients had uveitis. Our BD patient group contained more males than the control group. The genotype frequencies of the 14 SNPs were tested and the results did not deviate from the Hardy-Weinberg equilibrium in the healthy controls.
Frequency of genotypes and alleles of the examined SNPs in BD versus healthy controls in the first-phase study
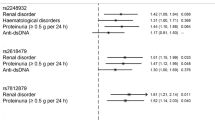
The fourteen SNPs were tested in 388 BD cases and 742 healthy controls during the first phase study. The frequencies of MBL2/rs1800450 AA genotype (Pc = 0.02, OR = 2.556) and KLRC4/rs2617170 TT genotype (Pc = 8.90 × 10−3, OR = 1.688) were significantly higher in BD. A significant lower frequency of the KLRC4/rs2617170 C allele and CC genotype was also observed (Pc = 1.66 × 10−4, OR = 0.661; Pc = 1.02 × 10−2, OR = 0.576; respectively) in BD (Table 2). However, we failed to find a significant association between the remaining SNPs and ocular BD (Supplementary Table 1).
Genotype and allele frequency of the examined SNPs in BD versus healthy controls in the second phase and combined study
To validate the results from the first stage study, a different cohort of patients (378 BD cases and 932 healthy individuals) was recruited for the second stage study. The frequencies of the MBL2/rs1800450 A allele and AA genotype in BD patients was significantly higher (Pc = 6.70 × 10−5, OR = 1.637; Pc = 2.32 × 10−3, OR = 3.204; respectively), whereas a lower frequency of the GG genotype (Pc = 1.90 × 10−3, OR = 0.6) was observed in BD compared with controls (Table 2). The KLRC4/rs2617170 C allele and CC genotype frequencies were significantly lower in BD compared to controls (Pc = 1.47 × 10−4, OR = 0.667; Pc = 1.63 × 10−2, OR = 0.593, respectively), while a higher frequency of the TT genotype was detected in BD (Pc = 4.16 × 10−3, OR = 1.701) (Table 2). Combination of the data from the two stage studies confirmed that rs1800450 in MBL2 was correlated with the risk to BD (A allele: Pc = 2.50 × 10−6, OR = 1.494; AA genotype: Pc = 2.24 × 10−6, OR = 2.899; GG genotype: Pc = 1.56 × 10−3, OR = 0.689;) (Table 2), and that rs2617170 in KLRC4 also contributed to susceptibility of BD (C allele: Pc = 2.05 × 10−9, OR = 0.664; CC genotype: Pc = 1.20 × 10−5, OR = 0.585; TT genotype: Pc = 2.53 × 10−6, OR = 1.695) (Table 2).
The Influence of MBL2/rs1800450 and KLRC4/rs2617170 on gene mRNA transcription and cytokine production
In order to find a biological explanation for the association of BD with MBL2/rs1800450 and KLRC4/rs2617170, the mRNA expression of MBL2 as well as KLRC4 of healthy genotyped individuals was measured in their PBMCs. We also evaluated whether different genotypes of MBL2/rs1800450 and KLRC4/rs2617170 could influence the production of cytokines important in the development of BD such as IFN-γ, IL-6, IL-8, IL-1β, IL-10 and TNF-α. These experiments were performed in healthy individuals to eliminate confounding effects such as the inflammatory status and immunosuppressive drug effects in our BD patient group.
Real-time PCR data demonstrated that the mRNA level of MBL2/rs1800450 in GG carriers was remarkably higher than AG carriers (P = 0.019) (Fig. 1). We did not test AA carriers since the frequency of this genotype is very low (<3–4%). The mRNA expression of KLRC4/rs2617170 in CC carriers showed a significant increase compared to CT/TT individuals (Fig. 2, P < 0.001).
The effect of MBL2 and KLRC4 genotype on cytokine production was tested in LPS treated PBMCs isolated from genotyped healthy controls. ELISA was applied to test the concentration of IFN-γ, IL-6, IL-8, IL-1β, IL-10 as well as TNF-α in the 72 hr cell culture supernatants. LPS stimulated PBMCs from GG genotype MBL2/rs1800450 carriers secreted higher amount of INF-γ, IL-6 and IL-8 than AG carriers (P = 0.002; p = 0.009; p = 0.005; respectively) (Fig. 3a,b,c). Compared to CC (P = 0.002; P = 0.004) carriers, an elevated secretion of IL-8 and IL-10 was observed in TT KLRC4/rs2617170 (Fig. 4a,b). No effect of the various rs1800450 and rs2617170 genotypes on the release of other cytokines could be detected.(Figs 3d,e,f and 4c,d,e).
Discussion
In this study we show that gene polymorphisms of MBL2 encoding rs1800450 and KLRC4 encoding rs2617170 are associated with BD. Furthermore, the two SNPs were found to affect their gene expression. mRNA expression of MBL2 and KLRC4 were higher in individuals with the GG(BD-protective) genotype of rs1800450 and CC(BD-protective) genotype of rs2617170 as compared to the other genotype carriers. Additionally, INF-γ, IL-6 and IL-8 production by stimulated PBMCs from GG genotype carriers of rs1800450 and IL-8, IL-10 production by stimulated PBMCs from CC genotype carriers of rs2617170 were increased.
C-type lectin receptors (CLRs), often containing the C-type lectin-like domain (CTLD), are a large family of extracellular proteins13. CLRs can bind carbohydrate through CTLD and activate different signaling pathways, which induce the expression of specific cytokines ultimately affecting T cell subtype polarization20. Recent findings also showed that CLRs are vital in immune homeostasis, which can induce both pro-inflammatory and anti-inflammatory immune responses20. BD is a multifactorial autoinflammatory disease and the interactions between susceptibility genes and environmental factors may affect susceptibility3. Several studies suggest that the expression of some members of CLRs are significantly different between BD cases and healthy individuals, such as the increased CD94 expression in BD patients21 and decreased mannose-binding lectin (MBL) concentration as compared to healthy controls18. Moreover, previous reports showed that CLRs are involved in the development of certain autoimmune diseases such as JIA, T1MD, SLE, RA, MS14,15,16,17,18. Based on these studies, we assumed that CLR genetic polymorphisms might also be associated with BD. To validate this hypothesis, we examined the association of polymorphisms of CLRs in BD patients and found a strong association between 2 SNPs, rs1800450 in the MBL2 gene and rs2617170 in KLRC4, with BD in a Chinese Han population. The fact that CLRs play vital roles in the innate immune response against microbial pathogens strengthens the view that BD is caused by an aberrant response against environmental stimuli20.
MBL2 belongs to the C-type collectin family, and plays a potential role in innate immunity. Many studies showed that a low or high serum MBL level is involved in several immune mediated diseases (e.g., RA, Crohn’s disease, Sjögren disease and diabetic retinopathy22,23,24). Immune defense function of MBL is associated with its serum level and oligomeric type23. Five SNPs of the MBL2 gene, including three structure variants, codon 52 (rs5030737), 54 (rs1800450), 57 (rs1800451) and two promoter variants, −550 (rs11003125) and −221(rs7096206) are thought to be responsible for reducing MBL2 serum levels and influencing the formation as well as the stability of oligomeric MBL225,26,27. However, others didn’t find any association between genetic polymorphisms of MBL2 and BD susceptibility28. In our study, we confirmed that MBL2 is a predisposing gene for BD in a Chinese Han population. Sample selection bias and different genetic backgrounds may explain the observed discrepancy between studies. We did not measure MBL2 levels in serum of our BD patients or controls, since the patients were often treated with immunosuppressive drugs, which may influence the serum concentration of MBL2. Further studies are needed to address this issue.
NKG2F encoded by the KLRC4 gene is a recently described member of the NKG2 family receptors, and its function has not been examined in detail29. This receptor can activate NK cells following the binding with its ligand DAP1230. A recent GWAS has shown that rs2617170 of KLRC4 is associated with BD in Turkish and Japanese patients31. However, it has not yet been reported in the Chinese population. Our results indicate that only the rs2617170 association (C allele: Pc = 2.05 × 10−9, OR = 0.664; CC genotype: Pc = 1.20 × 10−5, OR = 0.585) exceeds the threshold for genome-wide significance (P < 5e-08), Our study confirms the results of a previous GWAS regarding the association of KLRC4/rs2617170 with BD32. Interestingly, the C allele of rs2617170 was associated with disease risk in this GWAS study31, whereas the C allele had a higher frequency in the controls as compared to the BD patients in our study, and would therefore seem to be associated with disease protection. On the other hand, Dixon et al 32. have reported that rs2617170 is a significant eQTL for KLRC4 expression, and the C allele is associated with reduced KLRC4 gene expression. This is in contrast with our findings where we showed that the C allele is associated with higher gene expression. The reasons for these discrepancies may be due to different ancestral backgrounds of the subjects investigated and this issue clearly deserves further study. Until now, the role of KLRC4 in BD has not received much attention. It has been demonstrated that the stimulation of IL-2 and IL-15 led to an up-regulation of KLRC4 on NK cells30. Other groups have reported that IL-15 levels were elevated in serum, cerebrospinal fluid, and aqueous humor from patients with BD33,34,35. Further experiments are needed to unravel the functional role of KLRC4 variants on BD pathogenesis. It is interesting to point out that we observed a lower frequency of CC (30.4%) and a higher frequency of CT of rs2617170 in our healthy control group (47.7%) as compared to data reported in the Asian population as shown in the NCBI Resource (42.2% and 35.6%, respectively). However, our results are similar to a previous report on rs2617170 genotype frequencies36 in a Chinese Han population (27.4% and 55.8%, respectively), indicating heterogeneity between Asian populations.
Our study has a number of limitations. Firstly, since we only chose the loci with known associations between CLRs and various autoimmune or auto inflammatory diseases, it cannot be excluded that other SNPs in CLRs may have an association with BD. Detailed sequence analysis should be carried out to investigate the potential involvement of other rare variants of these factors in BD development. Secondly, our BD patients were Chinese Han patients recruited from an ophthalmic department and all had uveitis. Not all patients with BD have uveitis and depending on their complaints will see different medical departments. Further studies including BD patients from other medical departments (e.g., dermatology, rheumatology, stomatology) and other populations are therefore required to confirm our results and to investigate whether the observed associations are not only confined to the subpopulation of BD patients with uveitis. Due to sample size we also did not investigate whether subgrouping of our patients according to clinical features had an effect on the CLR gene associations. Last but not least, although our study identified rs1800450 of MBL2 and rs2617170 of KLRC4 as possible risk factors contributing to the susceptibility for BD, the exact mechanism how these variants affect the disease pathogenesis are not yet exactly clarified and await further study.
In summary, our study confirmed that MBL2/rs1800450 and KLRC4/rs2617170 polymorphisms affect disease susceptibility in the Chinese Han population. Further studies are needed to reveal the crucial role of the CLRs pathways in the pathogenesis of BD.
Materials and Methods
Study population
All BD uveitis patients (n = 766) and healthy individuals (n = 1674) included in the present study (n = 2440) were ethnic Han Chinese, recruited from the First Affiliated Hospital of Chongqing Medical University from May 2008 to August 2015. The diagnostic criteria of BD strictly followed the International Study Group for BD37. Controls were matched for age, geographic origin and ethnicity with BD patients. A case-control study including two phases was performed. In the first phase, 388 BD patients and 742 healthy individuals were included. and in the second phase, 378 BD cases and 932 controls were recruited. The major clinical symptoms in the recruited BD cases are clarified in Table 1. This study was conducted under the approval of the Clinical Research Ethics Committee of the First Affiliated Hospital of Chongqing Medical University (Permit Number: 2009-201008). All the procedures complied with the tenets of the Declaration of Helsinki. Informed written consent was provided by all patients and controls.
Single nucleotide polymorphisms (SNPs) selection
SNPs were chosen from previous studies on the correlation between CLRs and various autoimmune or auto-inflammatory diseases31, 38,39,40,41,42,43,44,45,46.Minor allele frequency (MAF) and linkage disequilibrium (LD) were tested by HaploView 4.2 software based on the data of Han Chinese in the HapMap database (MAF > 0.05 as well as an r2-value of LD < 0.8). Based on this analysis, we selected a total of 14 SNPs, including 2 SNPs (rs180045038, rs709620639) in MBL2, one SNPs (91188740) in SFTPD, one SNP (rs132346141) in CLEC12A, one SNP (rs237742242) in CLEC4A, one SNP (376402243) in CLEC2D, one SNP (rs228788644) in CD209, one SNPs (rs476387915) in CD69, one SNP (rs230248945) in KLRD1, one SNP (rs273444017) in KLRC1, one SNP (rs225533617) in KLRK1, one SNP (rs261717031) in KLRC4, one SNP (rs476365518) in KLRB1 and one SNP (rs112140146) in KLRG1. CLEC16A 47 and selectins48 were excluded from this study because they have been reported previously by our team.
Genomic DNA Extraction and Genotyping
Genomic DNA extraction from peripheral blood cells was performed using the QIAamp DNA Blood Mini Kit (Qiagen, Valencia, California, USA), according to instructions of the manufacturer. The concentration and quality of DNA were analyzed with a Nanodrop 2000 (Thermo Fisher Scientific, Wilmington, DE, USA) and then the DNA samples were standardized and kept at −20 °C until used.
In the first stage, all SNPs in our study (except rs1800450) were genotyped by the MassARRAY platform (Sequenom, USA) and iPLEX Gold Assay. The PCR reaction was carried out by the Gene Amp PCR System 9700 instrument (ABI, Foster City, CA, USA). MassARRAY Assay design software was used to design the primers (Table 3). Experimental data were analyzed through SpectroTYPER software (version 4.0; Sequenom). Rs2617170 in the second stage was performed by the TaqManH SNP Genotyping Assay in the 7500 Real-Time PCR system (Applied Biosystems, USA). The results were examined through TaqManH Genotyper Software. Rs1800450 was genotyped by the PCR-RFLP method.
Cell isolation and culture
Ficoll-Hypaque density-gradient centrifugation was used to separate Peripheral blood mononuclear cells (PBMC) from fresh venous blood of healthy male controls. PBMCs were seeded into 24-well culture plates (1 × 106 cells/well) in medium RPMI 1640 (supplemented with 10% fetal calf serum, 100 U/ml penicillin and 100 μg/ml streptomycin). To test the production of cytokine IFN-γ, IL-6, IL-8, IL-1β, IL-10 and TNF-α, PBMCs were stimulated with 100 ng/ml lipopolysaccharide (LPS, 100 ng/ml; Sigma, Missouri, USA) for 24 h.
Real-time PCR
Total RNA extraction from PBMCs was performed using the TRIzol (Invitrogen, San Diego, California, USA) method. RNA was reverse transcribed into cDNA with a Takara transcriptase kit (Takara, Dalian, China). The assays were carried out on an ABI 7500 real-time system with the following primers (KLRC4: 5′-GGAATGACAAGACATATCACTG-3′and 5′-GTCAGTTGAATACTACACAGACT-3′; MBL2: GCAAACAGAAATGGCACGTAT and AGAGGCCTGGAACTTGACA). The expression level was measured by the 2−ΔΔCt method.
Measurement of cytokines by ELISA
The concentration of IFN-γ, IL-6, IL-8, IL-1β, IL-10 and TNF-α in the supernatants of PBMCs were analyzed through using the human Duoset ELISA development kit (R&D Systems, Minneapolis, Minnesota, USA).
Statistical analysis
The differences between BD cases and healthy individuals with regard to allele and genotype frequencies were analyzed by the chi-square (χ2) test with SPSS17.0 statistical software package (version17.0, SPSS, Chicago, IL). Hardy-Weinberg equilibrium was examined by the SHEsis website.
For multiple comparisons, the Bonferroni correction was used to adjust P values to corrected P values (Pc) according to the number of performed analyses. A pc < 0.05 was viewed as significant. Expression of KLRC4, MBL2 and cytokine levels among three genotype groups was tested by the non-parametric Mann-Whitney test or student t test, with P < 0.05 (Two-tailed) taken as being statistically significant.
References
Yang, P. et al. Clinical features of Chinese patients with Behcet’s disease. Ophthalmology. 115, 312–318 (2008).
Wasseem Skef, M. J. & Haamilton, T. A. Gastrointestinal Behçet’s disease: A review. World J Gastroenterol 21(13), 3801–3812 (2015).
Ortiz-Fernández, L. et al. Genetic Analysis with the Immunochip Platform in Behçet Disease. Identification of Residues Associated in the HLA Class I Region and New Susceptibility Loci. PLoS one. 11(8), e016130 (2016).
Yan Zhou. et al. Association of a NOS3 gene polymorphism with Behçet’s disease but not with Vogt-Koyanagi-Harada syndrome in Han Chinese. Molecular Vision. 22, 311–318 (2016).
Hou, S. et al. Genetic variants in the JAK1 gene confer higher risk of Behcet’s disease with ocular involvement in Han Chinese. Hum Genet. 132(9), 1049–1058 (2013).
Li, H. et al. TNFAIP3 gene polymorphisms confer risk for Behcet’s disease in a Chinese Han population. Hum Genet. 132(3), 293–300 (2013).
Remmers, E. F. et al. Genomewide association study identifies variants in the MHC class I, IL10, and IL23R-IL12RB2 regions associated with Behcet’s disease. Nat Genet. 42(8), 698–702 (2010).
Mizuki, N. et al. Genome-wide association studies identify IL23R-IL12RB2 and IL10 as Behcet’s disease susceptibility loci. Nat Genet. 42(8), 703–706 (2010).
Yu, H. et al. Identification of susceptibility SNPs in IL10 and IL23R-IL12RB2 for Behçet’s disease in Han Chinese. J Allergy Clin Immunol 139(2), 621–627 (2017).
Kirino, Y. et al. Targeted resequencing implicates the familial Mediterranean fever gene MEFV and the toll-like receptor 4 gene TLR4 in Behçet disease. Proc Natl Acad Sci USA. 110(20), 8134–8139 (2013).
Xavier, J. M. et al. FUT2: filling the gap between genes and environment in Behçet’s disease? Ann Rheum Dis. 74(3), 618–24 (2015).
Kappen, J. H. et al. Genome-wide association study in an admixed case series reveals IL12A as a new candidate in Behçet disease. PloS One. 10(3), e0119085 (2015).
Yan, H., Ohno, N. & Tsuji, N. M. The role of C-type lectin receptors in immune homeostasis. International Immunopharmacology. 16(3), 353–357 (2013).
Skinningsrud, B. et al. A CLEC16A variant confers risk for juvenile idiopathic arthritis and anti-cyclic citrullinated peptide antibody negative rheumatoid arthritis. Ann Rheum Dis. 69(8), 1471–1474 (2010).
Barrett, J. C. et al. Genome-wide association study and meta-analysis finds over 40 loci affect risk of type 1 diabetes. Nat Genet. 41(6), 703–707 (2009).
Morris, D. L. et al. Variation in the upstream region of P-Selectin (SELP) is a risk factor for SLE. Genes and Immunity. 10(5), 404–413 (2009).
Park, K. S., Park, J. H. & Song, Y. W. Inhibitory NKG2A and activating NKG2D and NKG2C natural killer cell receptor genes: susceptibility for rheumatoid arthritis. Tissue Antigens. 72, 342–346 (2008).
Søndergaard, H. B. et al. Alterations in KLRB1 gene expression and a Scandinavian multiple sclerosis association study of the KLRB1 SNP rs4763655. European Journal of Human Genetics 19(10), 1100–1103 (2011).
Inanc, N. et al. Serum mannose-binding lectin levels are decreased in behcet’s disease and associated with disease severity. J Rheumatol. 32(2), 287–291 (2005).
Geijtenbeek, T. B. & Gringhuis, S. I. Signalling through C-type lectin receptors:shaping immune responses. Nat Rev Immunol 9(7), 465–479 (2009).
Saruhan-Direskeneli, G. et al. Expression of KIR and C-type lectin receptors in Bechet’s disease. Rheumatology. 43(4), 423–427 (2004).
Turner, M. W. The role of mannose-binding lectin in health and disease. Mol Immunol. 40(7), 423–429 (2003).
Scorza, M., Liguori, R., Elce, A., Salvatore, F. & Castaldo, G. Biological role of mannose binding lectin: From newborns to centenarians. Clin Chim Acta 451, 78–81 (2015).
Geng, P., Ding, Y., Qiu, L. & Lu, Y. Serum mannose-binding lectin is a strong biomarker of diabetic retinopathy in chinese patients with diabetes. Diabetes Care. 38(5), 868–875 (2015).
Seyfarth, J., Garred, P. & Madsen, H. O. The ‘involution’ of mannose-binding lectin. Hum Mol Genet 14(19), 2859–2869 (2005).
Garred, P., Larsen, F., Seyfarth, J., Fujita, R. & Madsen, H. O. Mannose-binding lectin and its genetic variants. Genes Immun. 7(2), 85–94 (2006).
Gordon, A. C. et al. Mannose-binding lectin polymorphisms in severe sepsis: relationship to levels incidence, and outcome. Shock. 25(1), 88–93 (2006).
Kim, J. et al. Mannose-binding lectin gene-2 polymorphisms and serum mannose-binding lectin Levels in Behçet’s disease. Clin Exp Rheumatol. 27(2 Suppl 53), S13–17 (2009).
Huang, H. et al. Up-regulation of NKG2F receptor, a functionally unknown killer receptor, of human natural killer cells by interleukin-2 and interleukin-15. Oncol Rep. 24(4), 1043–1048 (2010).
Kim, D. K. et al. Human NKG2F is expressed and can associate with DAP12. Mol Immunol. 41(1), 53–62 (2004).
Kirino, Y. et al. Genome-wide association analysis identifies new susceptibility loci for Behçet’s disease and epistasis between HLA-B*51 and ERAP1. Nat Genet. 45(2), 202–207 (2013).
Dixon, A. L. et al. A genome –wide association study of global gene expression. Nat Gene 39(10), 1202–1207 (2007).
Ahn, J. K., Yu, H. G., Chung, H. & Park, Y. G. Intraocular cytokine environment in active Behcet uveitis. Am J Ophthalmol. 142(3), 429–34 (2006).
Hamzaoui, K., Hamzaoui, A., Ghorbel, I., Khanfir, M. & Houman, H. Levels of IL-15in serum and cerebrospinalfluid of patients with Behcet’s disease. Scand J Immunol 64(6), 655–660 (2006).
Curnow, S. J. et al. Serum cytokine profiles in Behcet’s disease: is there a role for IL-15 in pathogenesis? Immunol Lett. 121, 7–12 (2008).
Ma, J. et al. Association of NKG2D Genetic Polymorphism with Susceptibility to Chronic Hepatitis B in a Han Chinese Population. J Med Virol 82(9), 1501–1507 (2010).
Criteria for diagnosis of Behcet’s disease. International Study Group for Behcet’s Disease. Lancet 335, 1078–1080 (1990).
Panda, A. K. et al. Low producer MBL genotypes are associated with susceptibility to systemic lupus erythematosus in Odisha, India. Human Immunology. 74(1), 114–119 (2013).
Gergely, P. Jr. et al. Structural polymorphisms in the mannose-binding lectin gene are associated with juvenile idiopathic arthritis. J Rheumatol. 36(4), 843–847 (2009).
Tanaka, M. et al. Genetic Variants in Surfactant, Pulmonary-associated Protein D (SFTPD) and Japanese Susceptibility to Ulcerative Colitis. Inflamm Bowel Dis 15, 918–925 (2009).
Michou, L. et al. A genetic association study of the CLEC12A gene in rheumatoid arthritis. Joint Bone Spine 79, 451–456 (2012).
Guo, J. et al. A Replication Study Confirms the Association of Dendritic Cell Immunoreceptor (DCIR) Polymorphisms with ACPA - Negative RA in a Large Asian Cohort. Plos one. 7(7), e41228 (2012).
Wolfkamp, S. C. et al. Single nucleotide polymorphisms in C-type lectin genes,clustered in the IBD2 and IBD6 susceptibility loci,may play a role in the pathogenesis of inflammatory bowel diseases. Eur J Gastroenterol Hepatol 24(8), 965–70 (2012).
Kuo, H.-C. et al. Genetic Variants of CD209 Associated with Kawasaki Disease Susceptibility. Plos one. 9(8), e105236 (2014).
Seo, J. et al. Association of CD94/NKG2A, CD94/NKG2C, and its ligand HLA-E polymorphisms with Behcet’s disease. Tissue Antigens. 70(4), 307–313 (2007).
Armstrong, D. L. et al. Identification of new SLE-associated genes with a two-step Bayesian study design. Genes and Immunity 10(5), 446–456 (2009).
Li, K., Hou, S., Qi, J., Kijstra, A. & Yang, P. A variant of CLEC16A gene confers protection for Vogt- Koyanagi- Harada syndrome but not for Behcet’s disease in a Chinese Han population. Experimental Eye Research 132, 225–230 (2015).
Zheng, M. et al. Genetic polymorphisms of cell adhesion molecules in Behcet’s disease in a Chinese Han population. Scientific Reports 6, 24974 (2016).
Acknowledgements
The authors would like to thank all patients and healthy volunteers enrolled in the present study. This work was supported by the State Key Program for Basic Research of China (Grant No. 2016YFC0904000), Natural Science Foundation Major International (Regional) Joint Research Project (81320108009), Key Project of Natural Science Foundation (81130019), National Natural Science Foundation Project (31370893), Chongqing Key Laboratory of Ophthalmology (CSTC, 2008CA5003), National Key Clinical Specialties Construction Program of China, Key Project of Health Bureau of Chongqing (2012-1-003), Research fund for Traditional Chinese Medicine of Chongqing Health and Family Planning Commission (ZY201401013) and Chongqing Science & Technology Platform and Base Construction Program(cstc2014pt-sy10002).
Author information
Authors and Affiliations
Contributions
Peizeng Yang and Yi Yang conceived and designed the study. Yi Yang, Handan Tan and Bolin Deng performed the laboratory work and analyzed data. Jiayue Hu, Qingfeng Cao and Gangxiang Yuan collected blood of all patients and controls. Yi Yang wrote the paper. Hongsong Yu, Guannan Su, Aize Kijlstra and Peizeng Yang reviewed and edited the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, Y., Tan, H., Deng, B. et al. Genetic polymorphisms of C-type lectin receptors in Behcet’s disease in a Chinese Han population. Sci Rep 7, 5348 (2017). https://doi.org/10.1038/s41598-017-05877-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-05877-x
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.