Abstract
Data regarding genetic polymorphisms and platinum-based chemotherapy (PBC) treatment outcomes in patients with NSCLC are published at a growing pace, but the results are inconsistent. This meta-analysis integrated eligible candidate genes to better evaluate the pharmacogenetics of PBC in NSCLC patients. Relevant studies were retrieved from PubMed, Chinese National Knowledge Infrastructure and WANFANG databases. A total of 111 articles comprising 18,196 subjects were included for this study. The associations of genetic polymorphisms with treatment outcomes of PBC including overall response rate (ORR), overall survival (OS) and progression-free survival (PFS) were determined by analyzing the relative risk (RR), hazard ration (HR), corresponding 95% confidence interval (CI). Eleven polymorphisms in 9 genes, including ERCC1 rs11615 (OS), rs3212986 (ORR), XPA rs1800975 (ORR), XPD rs1052555 (OS, PFS), rs13181 (OS, PFS), XPG rs2296147 (OS), XRCC1 rs1799782 (ORR), XRCC3 rs861539 (ORR), GSTP1 rs1695 (ORR), MTHFR rs1801133 (ORR) and MDR1 rs1045642 (ORR), were found significantly associated with PBC treatment outcomes. These variants were mainly involved in DNA repair (EXCC1, XPA, XPD, XPG, XRCC1 and XRCC3), drug influx and efflux (MDR1), metabolism and detoxification (GSTP1) and DNA synthesis (MTHFR), and might be considered as potential prognostic biomarkers for assessing objective response and progression risk in NSCLC patients receiving platinum-based regimens.
Similar content being viewed by others
Introduction
Lung cancer is a leading cause of cancer-associated death and substantially contributes to the heavy burden worldwide, with a dismal 5-year survival rate of 16.6%1. Among all primary lung cancers, non-small cell lung cancer (NSCLC) represents approximately 85% of cases. Chemotherapy remains the standard first-line treatment for almost 80% of NSCLC patients, of which platinum-based chemotherapy (PBC) is considered as the most efficacious option, especially for patients with an advanced stage of the disease2, 3. Unfortunately, PBC efficacy varies markedly across individuals. Besides clinical and pathologic features, genetic variation is considered as an important factor to influence the treatment efficacy and prognosis.
For decades, we have witnessed a growing interest in the pharmacogenomics field, and a tremendous amount of epidemiological evidence that gene polymorphisms could give rise to varying drug response has emerged. Many studies have reported the association of genetic factors, including genes related to DNA repair pathway, drug influx and efflux, drug metabolism and detoxification, DNA synthesis, cell cycle control and apoptosis, with PBC response and prognosis of patients4,5,6,7,8. The accumulation of pharmacogenomics findings calls for a more comprehensive systematic review and meta-analysis to summarize the evidence and to identify the general genetic associations among reported results. Some meta-analyses have studied the influences of certain genes on treatment outcomes of NSCLC patients receiving PBC. However, these findings including original studies are not always consistent, and no systematic review and meta-analysis covering all tested polymorphisms has been performed thus far.
The aim of this work is to identify the effects of all eligible genes in clinical prognosis of NSCLC patients receiving platinum-based treatment. A total of 24 single nucleotide polymorphisms (SNPs) of 12 genes (ERCC1, XPA, XPC, XPD, XPG, XRCC1, XRCC3, GSTP1, MTHFR, RRM1, MDR1 and CDA) have been studied in our work. The impacts of these genetic variants on PBC efficacy in NSCLC patients were assessed by evaluating the objective response ratio (ORR), progression-free survival (PFS), and overall survival (OS). We think this comprehensive meta-analysis with robust evidence would fill the gap in the pharmacogenomics of platinum in NSCLC patients.
Materials and Methods
Search strategy, eligibility criteria and data extraction
We followed the principles proposed by the Human Genome Epidemiology Network (HuGeNet) HuGE Review Handbook of Genetic Association Studies9.
Relevant studies were searched in PubMed, Chinese National Knowledge Infrastructure (CNKI) and WANFANG databases. A two-step search strategy was implemented and last updated on January 31, 2016. First, the following three groups of keywords were used for searching in MEDLINE (via the PubMed gateway): platinum OR cisplatin OR carboplatin OR oxaliplatin OR nedaplatin, polymorphism OR SNP OR variant, NSCLC OR non-small cell lung cancer. Second, we used different combinations of the above terms for complementary searching. Besides, references cited in the retrieved papers were manually searched in case of missing relevant studies. Afterwards, we singled out the candidate genes that were eligible in our research, and the terms including a candidate gene’s official symbol and the three above-mentioned groups of keywords were used to perform a comprehensive search.
The studies included in the meta-analysis had to meet all the following inclusion criteria: (i) cancer should be confirmed as NSCLC; (ii) treatment regimens were platinum-based chemotherapies; (iii) studies provided primary outcomes of interest including ORR, PFS or OS. Studies met any one of the exclusion criteria listed below were excluded in our analysis: (i) studies without indispensable data such as genotypes, overall response rate (ORR), overall survival (OS), or progression-free survival (PFS); (ii) studies with other types of lung cancer such as small cell lung cancer (SCLC) included; (iii) reviews, case reports, and meta-analyses. (iv) studies based on cell lines and animal experiment.
All records were screened by three investigators independently (Tan, Qiu and Jin) with disagreement resolved by discussion. The following information was extracted from each of the eligible studies: first author, publication year, sample size, ethnicity, age, gender, stages of tumor, chemotherapeutic agents, SNPs and genotyping methods, treatment outcomes.
Statistical analysis
We used the ORR as an indicator for PBC efficacy. Patients were classified into two groups: the responding group, which included complete and partial responders (CR and PR), and the non-responding group, which included subjects with stable or progressive diseases (SD and PD)10. RR and the corresponding 95% CI were used to assess the association between each genetic variant and the response of NSCLC patients treated with PBC. The hazard ratios (HR) and corresponding 95% CI were determined to evaluate OS and PFS. Three genotypic models commonly used in genetic association synopses were applied in this meta-analysis: heterozygous or homozygous variant versus wild type, heterozygous variant versus wild type and homozygous variant versus wild type.
Between-study variance, also known as heterogeneity, was evaluated by the chi-square-based Q test based on chi- square as well as I2. Q tests with P > 0.10 were considered with statistical significance. I2 described the proportion of variation originating from heterogeneity rather than within-study error, whose value varied from 0 to 100 percent and indicated different heterogeneity degrees. Heterogeneity could be accepted when I2 < 50% (0 < I2 < 25%: no heterogeneity; 25 < I2 < 50%: moderate heterogeneity). Sensitivity analysis and subgroup analysis were also applied to find the source of heterogeneity. Pooled RRs and HRs were calculated using the fixed-effects model when the heterogeneity was under the moderate degree or did not exist. Otherwise, the random-effects model was used. Moreover, the potential publication bias was assessed by statistical evaluation with Begg’s funnel plot and Egger’s linear regression test. The α level of significance was set at 0.05 unless noted otherwise.
In the end, we calculated the false positive report probability (FPRP) of statistically significant results to assess whether the findings were noteworthy11. The FPRP value was determined based on the P value, the prior probability for the association and statistical power. We set a stringent FPRP threshold of 0.20 and assigned a prior probability range of 0.1–0.001, and the statistical power was based on the ability to detect an OR of 1.5, with α equal to the observed p-value.
All statistical analyses were performed with STATA/SE.12.0 (StataCorp, College station, TX) and R (version 3.2.0, R Foundation for Statistical Computing, Vienna, Austria).
Results
Characteristics of Eligible Studies
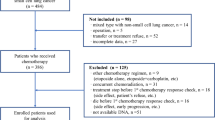
After the process of selection, a total of 111 studies met the inclusion criteria and totally 18,196 NSCLC subjects (between the ages of 51 to 84) who accepted PBC were included in the final meta-analysis. More than 80% of these articles focused on the advanced NSCLC (in disease stages of III–IV). The process of selecting publications is presented in Fig. 1 and more details about the characteristics of the studies included are listed in Table 1.
Meta-analysis findings
Genetic variants associated with response to platinum drugs
As shown in Table 2, we conducted 74 primary meta-analyses and 64 subgroup meta-analyses sorted by ethnicity to study the associations between 24 SNPs of 12 genes and the responses to PBC in NSCLC patients. Of the 138 performed meta-analyses, 26 (19%) resulted in statistically significant (P < 0.05), with the remaining 112 being non-significant. For ORR, RR < 1 indicated that patients carrying the allele or genotype had a disadvantageous response, RR > 1 donated that the allele carriers had a favorable response. Pooled RR with 95% CI of individual SNPs identified as statistically associated with favorable responses to PBC were listed as follows: XRCC1 rs25487 (AA vs. GG: overall RR = 1.27, 95% CI = 1.02–1.58), XRCC1 rs1799782 (CT vs. CC: overall RR = 1.22, 95% CI = 1.03–1.44; TT vs. CC: overall RR = 1.29, 95% CI = 1.07–1.56; CT+TT vs. CC: overall RR = 1.22, 95% CI = 1.04–1.42), XRCC3 rs861539 (CT VS CC: Caucasian RR = 1.46, 95% CI = 1.06–1.99 and overall RR = 1.31, 95% CI = 1.07–1.59; TT VS CC: Caucasian RR = 1.59, 95% CI = 1.07–2.36 and overall RR = 1.48, 95% CI = 1.12–1.97; TT+CT VS CC: Caucasian RR = 1.48, 95% CI = 1.10–2.01 and overall RR = 1.28, 95% CI = 1.07–1.52), XPA rs1800975 (AG VS AA: Asian RR = 2.17, 95% CI = 1.29–3.64 and overall RR = 1.74, 95% CI = 1.18–2.57), GSTP1 rs1695 (GG vs. AA: overall RR = 1.45, 95% CI = 1.20–1.74; AG+GG vs. AA: Asian RR = 1.47, 95% CI = 1.11–1.95 and overall RR = 1.37, 95% CI = 1.06–1.76). Pooled RR with 95% CI of individual SNPs identified as statistically associated with unfavorable responses were presented below: ERCC1 rs3212986 (AA vs. CC: Asian RR = 0.71, 95% CI = 0.54–0.94 and overall RR = 0.72, 95% CI = 0.56–0.94), XPD rs13181 (CA+CC vs. AA: Asian RR = 0.83, 95% CI = 0.71–0.98), XPD rs1799793 (AA vs. GG: Asian RR = 0.20, 95% CI = 0.05–0.76), MTHFR rs1801133 (CT vs. CC: mixed RR = 0.63, 95% CI = 0.44–0.89), MDR1 rs1045642 (CT vs. CC: Asian RR = 0.69, 95% CI = 0.50–0.95 and overall RR = 0.73, 95% CI = 0.56–0.94; TT vs. CC: Asian RR = 0.47, 95% CI = 0.26–0.85 and overall RR = 0.52, 95% CI = 0.34–0.81; CT+TT vs. CC: Asian RR = 0.61, 95% CI = 0.48–0.79 and overall RR = 0.64, 95% CI = 0.52–0.80).
Genetic variants associated with OS and PFS
Statistically significant results with HR > 1 indicated that patients carrying the allele or genotype harbored a poorer OS or PFS, while with HR < 1 meant better OS or PFS of patients. As for OS (Table 3), 52 meta-analyses were preformed to examine the influence of 22 SNPs in 11 genes on the overall survival. Seven results were identified as statistically significantly associated with OS. Of them, ERCC1 rs11615 (CT+TT vs. CC: HR = 1.47, 95% CI = 1.15–1.88), ERCC1 rs3212986 (AA vs. CC: HR = 2.06, 95% CI = 1.19–3.57), XPD rs13181 (AC+CC vs. AA: HR = 1.24, 95% CI = 1.07–1.44), and XPD rs1052555 (CT+TT vs. CC: HR = 1.71, 95% CI = 1.31–2.23) might be related to a poorer OS, while XPG rs873601 (GG vs. AA: HR = 0.67, 95% CI = 0.46–0.97), XPG rs2296147 (TT vs. CC: HR = 0.40, 95% CI = 0.27–0.61), and XPD rs1799793 (GA vs. GG: HR = 0.78, 95% CI = 0.62–0.99) might be potentially related to a better OS. No significant association was identified in the remaining SNPs. As for PFS (Table 4), 19 meta-analyses were conducted and 11 SNPs of 4 genes were investigated to explore their associations with the PFS of NSCLL patients. Our findings showed that patients with C allele of XPD rs13181 had a poorer PFS (AC+CC vs. AA: HR = 1.38, 95% CI = 1.10–1.73), and the T allele of XPD rs1052555 also indicated a poorer PFS (CT+TT vs. CC: HR = 1.97, 95% CI = 1.38–2.83).
Heterogeneity and publication bias
A total of 54% (n = 97) of meta-analyses showed no heterogeneity (I2: 0 to 25%) and 14% (n = 25) presented moderate heterogeneity (I2: 25 to 50%), and large heterogeneity even extreme heterogeneity existed in other meta-analyses. Sensitivity analysis and subgroup analysis were also applied to find the source of heterogeneity. The clinical heterogeneity such as disease stages, different chemotherapy regimens might be the major reason for the large or extreme heterogeneity.
We used P value for Egger’s test to evaluate the potential publication bias. Our results suggested that effects of XPD rs238406 (CA+AA vs. CC), XRCC1 rs25487 (GA+AA vs. GG), XRCC1 rs1799782 (CT vs. CC) and XRCC3 rs861539 (CT vs. CC, TT vs. CC and TT+CT vs. CC) on the ORR had significant publication bias. There was also some publication bias in analysis of the effects of XRCC1 rs25487 (GA vs. GG, GA+AA vs. GG) on the OS. Three meta-analyses showed bias in the association of certain SNPs with PFS, including XPD rs13181 (AC+CC vs. AA), XPD rs1799793 (GA+AA vs. GG) and XRCC1 rs25487 (GA+AA vs. GG). More details were listed in Tables 2 and 3.
False positive report probability
False positive findings regarding associations between genetic variants and diseases lead to a confounding effect. Here we assessed the FPRP to determine whether our finding was noteworthy. As shown in Table 5, 23 out of 35 results had FPRP lower than 0.2, with the prior probability set as 0.1 and the cut-off FPRP value as 0.2. The details of significant associations characterized by assessing FPRP are reported in Table 5.
High-quality significant associations that emerged from the current meta-analysis were discussed below.
Excision Repairs Cross-complementation Groups 1 (ERCC1)
Data showed that ERCC1 rs3212986 (C8092A) variant was related to the treatment response to PBC, and A allele may have poorer response comparing with C allele in Asians (AA vs. CC: pooled OR = 0.71, 95% CI = 0.54–0.94). Only moderate between-study heterogeneity was observed (I2 = 29.2%), and with a low FPRP when prior probability level was set as 0.1, suggesting that A allele of ERCC1 rs3212986 might be specifically linked to the poorer response in Asians.
ERCC1 rs11615 (C354T) was associated with OS, and T allele carriers might have unfavorable OS with HR being 1.47 and corresponding 95% CI being 1.15–1.88, and with no heterogeneity and low FPRP when prior probability level was set as 0.1, but subgroup classification by ethnicity were not performed.
Xeroderma Pigmentosum Group D (XPD)
Only the dominant model was used to analyze the relation between XPD rs13181 (A2251C) mutation and OS due to insufficient raw data. We found that the variant C allele was remarkably associated with the adverse OS in overall NSCLC patients treated with PBC (AC+CC vs. AA: HR = 1.24, 95% CI = 1.07–1.44). There was no heterogeneity and publication bias in the meta-analysis, and FPRP was low with the prior probability level being 0.1. C allele was also related to poor PFS with low FPRP at the high prior probability levels (AC+CC vs. AA: HR = 1.38, 95% CI = 1.10–1.73). No heterogeneity with statistical significance was observed, but the P value for Egger’s test showed that there was some publication bias in the meta-analysis. These results indicated that C allele was a risk allele for the poor clinical prognosis of NSCLC patients.
For other SNPs (rs1052555, C2133T) of XPD, we found that T allele was a risk allele and might be significantly associated with unfavorable OS (CT+TT vs. CC: HR = 1.71, 95% CI = 1.31–2.23). In the beginning, we included 4 articles in the meta-analysis and found that extreme heterogeneity and publication bias existed. After sensitivity analysis, we removed one article that was identified as the major source of heterogeneity, then I2 reduced to zero and no bias was observed from these data. The report had low FRPR with the prior probability level being 0.1 or 0.01. T allele was also related to poor PFS, and pooled HR was 1.97 and the 95% CI ranged from 1.38 to 2.83, though the report had low FPRP at high prior probability levels and no heterogeneity was observed. Further investigation with a larger sample size is needed to confirm the association between rs1052555 variant and prognosis of NSCLC patients.
Xeroderma Pigmentosum Group G (XPG)
XPG rs2296147 (T242C) might be associated with NSCLC patients’ prognosis receiving platinum drugs. We found that T allele acted as a protective allele with the carriers having favorable OS (TT vs. CC: HR = 0.40, 95% CI = 0.27–0.61), no heterogeneity and publication bias was detected, and the FPRP was low both at the high (0.1) and intermediate (0.01) prior probability levels. The strength of association needs to be further studied because of the small sample size of current meta-analysis.
X-Ray Cross-Complementing Group 1 (XRCC1)
Three genetic models were used to analyze the association between XRCC1 rs1799782 (C580T) polymorphisms and ORR, and results confirmed the positive response of patients carrying T allele to PBC with a low FPRP at the high (0.1) prior probability level, but large between-study heterogeneity existed in the three meta-analyses ((CT vs. CC: HR = 1.22, 95% CI = 1.03–1.44, I2: 63.4%); (TT vs. CC: HR = 1.29, 95% CI = 1.07–1.56, I2: 50.5%); (CT+TT vs. CC: HR = 1.22, 95% CI = 1.04–1.42, I2: 65.1%)).
X-Ray Cross-Complementing Group 3 (XRCC3)
Results from subgroup meta-analysis sorted by ethnicity showed that T allele of XRCC1 rs861539 (C241T) was associated with the positive response of PBC treatment in Caucasian population, three genetic models had consistent results (CT VS CC: RR = 1.46, 95% CI = 1.06–1.99; TT VS CC: RR = 1.59, 95% CI = 1.07–2.36; TT+CC VS CC: RR = 1.48, 95% CI = 1.10–2.01), no heterogeneity has been found. Begg’s test and Egger’s test revealed that some publication bias existed in the meta-analysis. However, Lower FRPR values suggested that the findings were statistically significant. Genetic variant of XRCC1 rs861539 was not associated with OS and PFS in the current meta-analysis.
Methylenetetrahydrofolate Reductase (MTHFR)
T allele of MTHFR rs1801133 (C665T) might be related to the negative response, the report had low FPRP at the high (0.1) prior probability level, with pooled HR = 0.63, 95% CI = 0.44–0.89, I2 = 41.0% when comparing CT and CC genotypes. The other genetic models including TT vs. CC and CT+TT vs. CC didn’t show statistical significance.
Glutathione S-transferase P1 (GSTP1)
For GSTP1 rs1695 (A313G), two genetic models showed consistent results about the association of the SNP with response (GG vs. AA: HR = 1.45, 95% CI = 1.20–1.74; AG+GG vs. AA: HR = 1.37, 95% CI = 1.06–1.76), the same effects were also observed in the Asian group by subgroup analysis in model AG+GG vs. AA (HR = 1.47, 95% CI = 1.11–1.95). However, we did not find a significant association in model AG vs. AA, low frequency of G allele and an insufficient sample size might be a major reason for it. We further assessed the FPRP value, and data showed low FPRP with probability level being 0.1. These results suggested that the G allele might play a protective role in the response of platinum-based treatment.
Multidrug resistance 1 (MDR1)
There were statistically significant associations between MDR1 rs1045642 (T3435C) polymorphism and treatment response in both overall and Asian groups in three comparison genetic models (CT vs. CC, TT vs. CC, CT+TT vs. CC), and results are presented in Table 2. Three statistically significant findings with low FPRP were considered as noteworthy (CT vs. CC: overall RR = 0.73, 95% CI = 0.56–0.94; CT+TT vs. CC: Asian RR = 0.61, 95% CI = 0.48–0.79; CT+TT vs. CC: overall RR = 0.64, 95% CI = 0.52–0.80). Significant between-study heterogeneity and potential bias were not observed in all comparison models.
Biological pathways associated with platinum drugs treatment outcomes in NSCLC patients
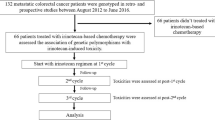
Genetic variants significantly associated with treatment outcomes of NSCLC patients receiving PBC had impacts on several biological pathways or certain physiological functions. As shown in Fig. 2, they included DNA repair pathway (EXCC1, XPD, XPG and XRCC1), drug influx and efflux (MDR1), metabolism and detoxification (GSTP1) and DNA synthesis (MTHFR).
Discussion
In this study, we described the meta-analysis findings of associations between genetic polymorphisms and treatment outcomes of NSCLC patients receiving platinum drugs. Our study identified that 14 SNPs in 10 genes were statistically associated with clinical prognosis including treatment response, OS and PFS. We further calculated FPRPs of the statistically significant results and 23 results were identified with high-quality evidence (Table 5).
The anti-cancer activity of platinum agents mainly depends on the formation of DNA adducts which inhibit DNA replication, hinder cell division and induce cell apoptosis11. DNA repair pathways including nucleotide excision repair (NER) and base excision repair (BER) could timely repair the damaged DNA induced by platinum agents and thus lead to treatment failure122. ERCC1, XPA, XPC, XPD and XPG are important components of NER. Being consistent with the studies by Yang et al.123 and Xu et al.124, our results confirmed the association between T allele of ERCC1 rs11615 and shorter OS. In addition, we found that A allele of ERCC1 rs3212986 was a risk allele that could shorten the carriers’ OS and decrease the activity of platinum, while some previously published meta-analyses did not report this effect124,125,126,127. However, the association should be replicated in other subsequent studies. In the present meta-analysis, we firstly assessed the influence of ERCC1 rs2298881 variant, but no significant association was found. We studied four SNPs of XPD in this work and found that XPD rs13181, a common SNP of XPD, was closely related to reduced OS and PFS. For the other SNP (rs1052555) of XPD, we found that T allele was a risk allele and might significantly associate with unfavorable OS and PFS. This is the first meta-analysis to assess the XPD rs1052555 variant, and the robust association needs to be further confirmed by subsequent studies with larger sample sizes. For XPG, we found that rs2296147 might be related to patients’ OS, and T allele could indicate a favorable OS. The other three SNPs of XPG (rs1047768, rs17655 and rs873601) showed no significant association with the ORR, OS and PFS. XRCC1 is a limiting factor in the base excision repair (BER) pathway. Our results and the previous studies confirmed the positive role of rs1799782 T allele in response to PBC128,129,130. For rs25487 of XRCC1, the statistically significant association between rs25487 polymorphism and ORR deserves to be further studied due to the high FRPR. XRCC3 is also important for DNA repair, Qiu et al. previously reported that XRCC3 rs861539 variation was related to good response of platinum treatment but not to survival, the same result was shown from the present meta-analysis. The MTHFR gene encodes an enzyme that is a central regulator for folate metabolism. It is suggested that MTHFR mutation was associated with increased risk of cardiovascular diseases and cancer131. We identified that the T allele was related to a negative response of PBC. MDR1 gene encodes for P-glycoprotein (P-gp), which plays a major role in the process of drug efflux and influx across the cell membrane132. We found that MDR1 rs1045642 variant was associated with ORR only in Asians, and published meta-analyses supported the association133, 134. GST is a phase II metabolic enzyme involved in the platinum detoxification, mediated by glutathione (GSH) conjugation123. Increasing GSH content would decrease platinum-DNA binding and result in platinum resistance. GSTP1 gene was found to be associated with platinum treatment response, and our results indicated that T allele of GSTP1 rs1695 increased the ORR in NSCLL patients, but the association was only observed in Asians. A previous meta-analysis also reported the same effect as ours123.
Great efforts have been made to identify the molecular predictive markers of platinum sensitivity. By further integrating our results according to genes biological functions, we found that the majority of polymorphisms of those genes significantly associated with treatment outcomes of platinum agents were involved in four biological pathways or physiological functions. According to the mechanism of platinum, DNA repair pathway may play a key role in the response of platinum therapy. Our results showed that the important components of DNA repair pathways (ERCC1, XPD, XPG, XRCC1 and XRCC3) were involved in the efficacy of platinum treatment and clinical outcome of NSCLL patients. MDR1 and GSTP1, which were related to drug transportation and detoxification respectively, influenced the outcome of platinum treatment. Another potential key gene was MTHFR, which was involved in regulating folate metabolism and DNA synthesis and was correlated with platinum sensitivity.
In the current meta-analysis, we comprehensively searched the relevant articles and explored all the eligible genes related to multiple biological functions, aiming to provide an updated and more critical summary of the available evidence of genetic polymorphisms and treatment outcomes of PBC in NSCLC patients. We first analyzed six SNPs including ERCC1 rs2298881, XPD rs1052555, XPD rs238406, XPG rs17655, XPG rs2296147 and XPG rs873601. There is a high chance that an initial “statistically significant” finding based on P value alone turns out to be a false-positive finding, so we calculated the FPRP of each statistically significant association to ensure the credibility of our findings, and we identified 11 SNPs in 9 genes that might truly associate with the ORR and/or OS and/or PFS of NSCLC patients receiving platinum drugs.
However, there were some limits in the present meta-analysis. First, despite the intensive efforts we have made to comprehensively search the related studies, some information might have been missed. Second, between-study heterogeneity existed in the current meta-analysis. Although sensitivity analysis and subgroup analysis were applied to find the source of heterogeneity, some heterogeneity couldn’t be fully explained by statistical methods. Clinical heterogeneity might play a role in the large between-study heterogeneity, such as disease stage and age. Third, three genotypic models (heterozygote variant vs. wild type, homozygote variant vs. wild type and the dominant model) were used for this study, the other models including recessive model and allele comparison were not performed because of limited raw data. However, the models used in the study were commonly used in genetic analysis, and could in part decrease the type I error inflation135. Fourth, we didn’t analyze the role of gene-gene as well as gene-environment interactions in the modification of chemotherapy efficacy, and attention should be paid to these factors in further studies.
In conclusion, this collection of data might provide a useful platform for research and clinical healthy practice. Further work still needs to be done to pinpoint the use of these SNPs as prognostic biomarkers for assessing objective response and progression risk in NSCLC patients receiving platinum-based regimens.
References
Ettinger DS FAU Wood, D. E. et al. Non-Small Cell Lung Cancer, Version 1.2015. J Natl Compr Canc Netw. 2014 Dec, 12(12), 1738–61 (2014).
Rossi, A. & Di Maio, M. Platinum-Based Chemotherapy in Advanced Non-Small-Cell Lung Cancer: Optimal Number of Treatment Cycles. Expert Rev Anticancer Ther (2016).
Bonanno, L., Favaretto A FAU Rosell, R. & Rosell, R. Platinum Drugs and Dna Repair Mechanisms in Lung Cancer. Anticancer Res. 2014 Jan, 34(1), 493–501 (2014).
Kilari, D. Role of Copper Transporters in Platinum Resistance. World Journal of Clinical Oncology 7, 106 (2016).
Germa-Lluch, J. R. & Piulats, J. M. [Molecular Bases of Platinum-Resistance in Testicular Cancer]. Arch Esp Urol 66, 524–535 (2013).
Martin, L. P., Hamilton TC FAU Schilder, R. J. & Schilder, R. J. Platinum Resistance: The Role of Dna Repair Pathways. Clin Cancer Res. 2008 Mar 1, 14(5), 1291–5, doi:10.1158/1078-0432.CCR-07-2238 (2008).
Rosell, R., Mendez P FAU Isla, D., Isla D FAU Taron, M. & Taron, M. Platinum Resistance Related to a Functional Ner Pathway. J Thorac Oncol. 2007 Dec, 2(12), 1063-6 (2007).
Muggia, F. M. & Los, G. Platinum Resistance: Laboratory Findings and Clinical Implications. Stem Cells 11, 182–193 (1993).
Sagoo, G. S., Little, J. & Higgins, J. P. Systematic Reviews of Genetic Association Studies. Human Genome Epidemiology Network. Plos Med 6, e28 (2009).
Eisenhauer, E. A. et al. New Response Evaluation Criteria in Solid Tumours: Revised Recist Guideline (Version 1.1). Eur J Cancer 45, 228–247 (2009).
Wacholder, S., Chanock, S., Garcia-Closas, M., El, G. L. & Rothman, N. Assessing the Probability that a Positive Report is False: An Approach for Molecular Epidemiology Studies. J Natl Cancer Inst 96, 434–442 (2004).
Camps, C. et al. Assessment of Nucleotide Excision Repair Xpd Polymorphisms in the Peripheral Blood of Gemcitabine/Cisplatin-Treated Advanced Non-Small-Cell Lung Cancer Patients. Clin Lung Cancer 4, 237–241 (2003).
Ryu, J. S. et al. Association Between Polymorphisms of Ercc1 and Xpd and Survival in Non-Small-Cell Lung Cancer Patients Treated with Cisplatin Combination Chemotherapy. Lung Cancer 44, 311–316 (2004).
Gurubhagavatula, S. et al. Xpd and Xrcc1 Genetic Polymorphisms are Prognostic Factors in Advanced Non-Small-Cell Lung Cancer Patients Treated with Platinum Chemotherapy. J Clin Oncol 22, 2594–2601 (2004).
Isla, D. et al. Single Nucleotide Polymorphisms and Outcome in Docetaxel-Cisplatin-Treated Advanced Non-Small-Cell Lung Cancer. Ann Oncol 15, 1194–1203 (2004).
Zhou, W. et al. Excision Repair Cross-Complementation Group 1 Polymorphism Predicts Overall Survival in Advanced Non-Small Cell Lung Cancer Patients Treated with Platinum-Based Chemotherapy. Clin Cancer Res 10, 4939–4943 (2004).
Wang, Z. H. et al. Single Nucleotide Polymorphisms in Xrcc1 and Clinical Response to Platin-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer. Ai Zheng 23, 865–868 (2004).
Yuan, P. et al. Correlation of Genetic Polymorphisms in Nucleotide Excision Repair System to Sensitivity of Advanced Non-Small Cell Lung Cancer Patients to Platinum-Based Chemotherapy. Ai Zheng 24, 1510–1513 (2005).
Lu, C. et al. Association Between Glutathione S-Transferase Pi Polymorphisms and Survival in Patients with Advanced Nonsmall Cell Lung Carcinoma. Cancer-Am Cancer Soc 106, 441–447 (2006).
de Las, P. R. et al. Polymorphisms in Dna Repair Genes Modulate Survival in Cisplatin/Gemcitabine-Treated Non-Small-Cell Lung Cancer Patients. Ann Oncol 17, 668–675 (2006).
Booton, R. et al. Xeroderma Pigmentosum Group D Haplotype Predicts for Response, Survival, and Toxicity After Platinum-Based Chemotherapy in Advanced Nonsmall Cell Lung Cancer. Cancer-Am Cancer Soc 106, 2421–2427 (2006).
Yuan, P. et al. Xrcc1 and Xpd Genetic Polymorphisms Predict Clinical Responses to Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer. Zhonghua Zhong Liu Za Zhi 28, 196–199 (2006).
Booton, R. et al. Glutathione-S-Transferase P1 Isoenzyme Polymorphisms, Platinum-Based Chemotherapy, and Non-Small Cell Lung Cancer. J Thorac Oncol 1, 679–683 (2006).
Shi, M. et al. Genetic Polymorphisms in Methylenetetrahydrofolate Reductase and Clinical Response to Chemotherapy in Non-Small Cell Lung Cancer. Zhongguo Fei Ai Za Zhi 9, 519–524 (2006).
Shi, M. Q. et al. Polymorphisms in Xrcc1 Gene and Sensitivity to Platin- Based Chemotherapy in Advanced Lung Cancer. Chinese Clinical Oncology 575–578 (2006).
Su, D. et al. Genetic Polymorphisms and Treatment Response in Advanced Non-Small Cell Lung Cancer. Lung Cancer 56, 281–288 (2007).
SUN Xin-chen, S. N. C. H. Xpa a23G Polymorphism and Clinical Response to Platin Based Chemotherapy in Advanced Non-Small Cell Lung Cancer. Journal of Medical Postgraduates 1271–1273 (2007).
Song, D. G., Liu, J., Wang, Z. H., Song, B. & Li, C. Z. Single Nucleotide Polymorphisms in Xrcc1 and Xpd Predict Sensitivity to Platinum-Based Chemotherapy in Advanced Nsclc. Chinese Journal of Gerontology 1684–1686 (2007).
Yu, Q. Z. et al. The Relationship Between the Polymorphisms of Gene Xpg and Mdr1 and the Responsiveness of Advanced Non- Small Cell Lung Cancer to Platinum-Based Chemotherapy. The practical journal of cancer 252–256 (2007).
Pan, J. H. et al. Mdr1 Single Nucleotide Polymorphisms Predict Response to Vinorelbine-Based Chemotherapy in Patients with Non-Small Cell Lung Cancer. Respiration 75, 380–385 (2008).
Tibaldi, C. et al. Correlation of Cda, Ercc1, and Xpd Polymorphisms with Response and Survival in Gemcitabine/Cisplatin-Treated Advanced Non-Small Cell Lung Cancer Patients. Clin Cancer Res 14, 1797–1803 (2008).
Wu, X. et al. Germline Genetic Variations in Drug Action Pathways Predict Clinical Outcomes in Advanced Lung Cancer Treated with Platinum-Based Chemotherapy. Pharmacogenet Genomics 18, 955–965 (2008).
Ding, Z. H. et al. Polymorphisms in Xpd751 Gene and Sensitivity to Gemcitabine/Cisplatin Chemotherapy in Advanced Stage of Non-Small-Cell Lung Cancer. Acta Universitatis Medicinalis Nanjing (Natural Science) 457–461 (2008).
Liu, X. Z., Qian, X. P., Liu, B. R., Hu, W. J. & Wang, L. F. Single Nucleotide Polymorphisms in Xrcci, Xpd and Platinum Prognosis in Non-Small-Cell Lung Cancer Patients. Journal of Clinical Medicine in Practice 7–11 (2008).
Pan, J. H. et al. Mdr1 Single Nucleotide Polymorphism G2677T/a and Haplotype are Correlated with Response to Docetaxel-Cisplatin Chemotherapy in Patients with Non-Small-Cell Lung Cancer. Respiration 78, 49–55 (2009).
Sun, X. et al. Polymorphisms in Xrcc1 and Xpg and Response to Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer Patients. Lung Cancer 65, 230–236 (2009).
Feng, J. F. et al. Polymorphisms of the Ribonucleotide Reductase M1 Gene and Sensitivity to Platin-Based Chemotherapy in Non-Small Cell Lung Cancer. Lung Cancer 66, 344–349 (2009).
Feng, J. et al. Xpa a23G Polymorphism is Associated with the Elevated Response to Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer. Acta Bioch Bioph Sin 41, 429–435 (2009).
Kalikaki, A. et al. Dna Repair Gene Polymorphisms Predict Favorable Clinical Outcome in Advanced Non-Small-Cell Lung Cancer. Clin Lung Cancer 10, 118–123 (2009).
Hong, C. Y., Xu, Q., Yue, Z., Zhang, Y. & Yuan, Y. Correlation of the Sensitivity of Np Chemotherapy in Non-Small Lung Cancer with Dna Repair Gene Xrcc1 Polymorphism. Ai Zheng 28, 1291–1297 (2009).
Gao, C. M. et al. Polymorphisms in Ercc1, Xrcc1 Genes and Sensitivity to Gemcitabine/Cisplatin Chemotherapy in Non-Small Cell Lung Cancer. Chin J Cancer Prev Treat 27–30 (2009).
Hu, S. N., Feng, J. F., Wu, J. Z., Gao, C. M. & Shi, M. Q. Polymorphisms in Rrm1 Gene and Sensitivity to Platin Based Chemotherapy in Non-Small Cell Lung Cancer Patients. Chin J Cancer Prev Treat 1477–1481 (2009).
Takenaka, T. et al. Effects of Excision Repair Cross-Complementation Group 1 (Ercc1) Single Nucleotide Polymorphisms On the Prognosis of Non-Small Cell Lung Cancer Patients. Lung Cancer 67, 101–107 (2010).
Sun, N. et al. Mrp2 and Gstp1 Polymorphisms and Chemotherapy Response in Advanced Non-Small Cell Lung Cancer. Cancer Chemother Pharmacol 65, 437–446 (2010).
Chen, S. et al. Association of Mdr1 and Ercc1 Polymorphisms with Response and Toxicity to Cisplatin-Based Chemotherapy in Non-Small-Cell Lung Cancer Patients. Int J Hyg Environ Health 213, 140–145 (2010).
Li, F. et al. Association Between Polymorphisms of Ercc1 and Xpd and Clinical Response to Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer. Am J Clin Oncol 33, 489–494 (2010).
Zhou, C. et al. Predictive Effects of Ercc1 and Xrcc3 Snp On Efficacy of Platinum-Based Chemotherapy in Advanced Nsclc Patients. Jpn J Clin Oncol 40, 954–960 (2010).
Zu-hong, Z. X. S. X. Xpc Lys939Gln Polymorphism is Associated with the Decreased Response to Platinum Based Chemotherapy in Advanced Non-Small-Cell Lung Cancer. Chinese Medical Journal 123, 3427–3432 (2010).
Wang, J. et al. Association Between Polymorphisms of Ercc1 and Response in Patients with Advanced Non-Small Cell Lung Cancer Receiving Cisplatin-Based Chemotherapy. Zhongguo Fei Ai Za Zhi 13, 337–341 (2010).
Yuan, P. et al. No Association Between Xrcc1 Polymorphisms and Survival in Non-Small-Cell Lung Cancer Patients Treated with Platinum-Based Chemotherapy. Cancer Biol Ther 10, 854–859 (2010).
Okuda, K. et al. Excision Repair Cross Complementation Group 1 Polymorphisms Predict Overall Survival After Platinum-Based Chemotherapy for Completely Resected Non-Small-Cell Lung Cancer. J Surg Res 168, 206–212 (2011).
Vinolas, N. et al. Single Nucleotide Polymorphisms in Mdr1 Gen Correlates with Outcome in Advanced Non-Small-Cell Lung Cancer Patients Treated with Cisplatin Plus Vinorelbine. Lung Cancer 71, 191–198 (2011).
Liu, L. et al. Assessment of Xpd Lys751Gln and Xrcc1 T-77C Polymorphisms in Advanced Non-Small-Cell Lung Cancer Patients Treated with Platinum-Based Chemotherapy. Lung Cancer 73, 110–115 (2011).
KimCurran, V. et al. Lack of Correlation Between Ercc1 (C8092a) Single Nucleotide Polymorphism and Efficacy/Toxicity of Platinum Based Chemotherapy in Chinese Patients with Advanced Non-Small Cell Lung Cancer. Adv Med Sci 56, 30–38 (2011).
Cui, L. H. et al. Influence of Polymorphisms in Mthfr 677 C–>T, Tyms 3R–>2R and Mtr 2756 a–>G On Nsclc Risk and Response to Platinum-Based Chemotherapy in Advanced Nsclc. Pharmacogenomics 12, 797–808 (2011).
Ryu, J. S. et al. Differential Effect of Polymorphisms of Cmpk1 and Rrm1 On Survival in Advanced Non-Small Cell Lung Cancer Patients Treated with Gemcitabine Or Taxane/Cisplatinum. J Thorac Oncol 6, 1320–1329 (2011).
Zhou, F. et al. Genetic Polymorphisms of Gstp1 and Xrcc1: Prediction of Clinical Outcome of Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer (Nsclc) Patients. Swiss Med Wkly (2011).
Ludovini, V. et al. Association of Cytidine Deaminase and Xeroderma Pigmentosum Group D Polymorphisms with Response, Toxicity, and Survival in Cisplatin/Gemcitabine-Treated Advanced Non-Small Cell Lung Cancer Patients. J Thorac Oncol 6, 2018–2026 (2011).
Xu, C., Wang, X., Zhang, Y. & Li, L. Effect of the Xrcc1 and Xrcc3 Genetic Polymorphisms On the Efficacy of Platinum-Based Chemotherapy in Patients with Advanced Non-Small Cell Lung Cancer. Zhongguo Fei Ai Za Zhi 14, 912–917 (2011).
Yan, P. W., Huang, X. E., Yan, F., Xu, L. & Jiang, Y. Influence of Mdr1 Gene Codon 3435 Polymorphisms On Outcome of Platinum-Based Chemotherapy for Advanced Non Small Cell Lung Cancer. Asian Pac J Cancer Prev 12, 2291–2294 (2011).
Cheng, H. Y. et al. Relationship of Single Nucleotide Polymorphisms and Clinical Response to Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer. Jiang su Med J 272–274 (2011).
Jia, X. F. et al. Relationship Between Xpa and Xpg Polymorphisms and Platinum-Based Chemotherapy Outcomes in Advanced Non-Small Cell Lung Cancer. Progress in Modern Biomedicine 1718–1722 (2011).
Li, D. R. et al. Association of Dna Repair Gene Polymorphisms with Response to Platinum-Based Chemotherapy in Patients with Non-Small Cell Lung Cancer. Tumor 348–353 (2011).
Li, D. R. et al. Correlation of Excision Repair Cross-Complementing Group 2 Polymorphisms and Response to Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer. China Journal of Modern Medicine 2004–2007 (2011).
Zhao, W. et al. Relationship of Xrcc1, Parp1 and Ape1 Polymorphisms with Efficacy of Platinum-Based Chemotherapy for Patients with Advanced Non-Small Cell Lung Cancer. Acta Universitatis Medicinalis Nanjing (Natural Science) 1021–1026 (2011).
Zhou, F. et al. Association of Gstp1 and Xrcc1 Genetic Polymorphisms with the Effects of Platinum-Based Chemotherapy On Advanced Non-Small Cell Lung Cancer Patients. Chinese Clinical Oncology 304–309 (2011).
Ren, S. et al. Association Between Polymorphisms of Dna Repair Genes and Survival of Advanced Nsclc Patients Treated with Platinum-Based Chemotherapy. Lung Cancer 75, 102–109 (2012).
Dong, J. et al. Potentially Functional Polymorphisms in Dna Repair Genes and Non-Small-Cell Lung Cancer Survival: A Pathway-Based Analysis. Mol Carcinog 51, 546–552 (2012).
Li, D., Zhou, Q., Liu, Y., Yang, Y. & Li, Q. Dna Repair Gene Polymorphism Associated with Sensitivity of Lung Cancer to Therapy. Med Oncol 29, 1622–1628 (2012).
Joerger, M. et al. Germline Polymorphisms in Patients with Advanced Nonsmall Cell Lung Cancer Receiving First-Line Platinum-Gemcitabine Chemotherapy: A Prospective Clinical Study. Cancer-Am Cancer Soc 118, 2466–2475 (2012).
Cheng, J. et al. A C118T Polymorphism of Ercc1 and Response to Cisplatin Chemotherapy in Patients with Late-Stage Non-Small Cell Lung Cancer. J Cancer Res Clin Oncol 138, 231–238 (2012).
Li, W. et al. Polymorphisms in Gstm1, Cyp1a1, Cyp2E1, and Cyp2D6 are Associated with Susceptibility and Chemotherapy Response in Non-Small-Cell Lung Cancer Patients. Lung 190, 91–98 (2012).
Chen, X. et al. Association of Xrcc3 and Xpd751 Snp with Efficacy of Platinum-Based Chemotherapy in Advanced Nsclc Patients. Clin Transl Oncol 14, 207–213 (2012).
Wu, W. et al. Effect of Polymorphisms in Xpd On Clinical Outcomes of Platinum-Based Chemotherapy for Chinese Non-Small Cell Lung Cancer Patients. Plos One 7, e33200 (2012).
Butkiewicz, D. et al. Influence of Dna Repair Gene Polymorphisms On Prognosis in Inoperable Non-Small Cell Lung Cancer Patients Treated with Radiotherapy and Platinum-Based Chemotherapy. Int J Cancer 131, E1100–E1108 (2012).
Krawczyk, P. et al. Predictive Value of Ercc1 Single-Nucleotide Polymorphism in Patients Receiving Platinum-Based Chemotherapy for Locally-Advanced and Advanced Non-Small Cell Lung Cancer–A Pilot Study. Folia Histochem Cytobiol 50, 80–86 (2012).
Liao, W. Y. et al. Genetic Polymorphism of Xrcc1 Arg399Gln is Associated with Survival in Non-Small-Cell Lung Cancer Patients Treated with Gemcitabine/Platinum. J Thorac Oncol 7, 973–981 (2012).
Dogu, G. G. et al. Mdr1 Single Nucleotide Polymorphism C3435T in Turkish Patients with Non-Small-Cell Lung Cancer. Gene 506, 404–407 (2012).
Ke, H. G. et al. Prognostic Significance of Gstp1, Xrcc1 and Xrcc3 Polymorphisms in Non-Small Cell Lung Cancer Patients. Asian Pac J Cancer Prev 13, 4413–4416 (2012).
Lv, H. Y. et al. Relationship Between Gstp1 and Xpg Genetic Polymorphisms and Survival of Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer Patients. China Oncology 609–617 (2012).
Zhang, Y. P., Sheng, G. F., Liu, Y. P., Xue, H. B. & Ling, Y. The Relationship of Gstp1 and Clinical Response to Platinum Based Chemotherapy in Advanced Non-Small Cell Lung Cancer. J Med The or & Prac 3003–3004 (2012).
Provencio, M. et al. Prospective Assessment of Xrcc3, Xpd and Aurora Kinase a Single-Nucleotide Polymorphisms in Advanced Lung Cancer. Cancer Chemoth Pharm 70, 883–890 (2012).
He, C., Duan, Z., Li, P., Xu, Q. & Yuan, Y. Role of Ercc5 Promoter Polymorphisms in Response to Platinum-Based Chemotherapy in Patients with Advanced Non-Small-Cell Lung Cancer. Anticancer Drugs 24, 300–305 (2013).
Hong, W. et al. Methylenetetrahydrofolate Reductase C677T Polymorphism Predicts Response and Time to Progression to Gemcitabine-Based Chemotherapy for Advanced Non-Small Cell Lung Cancer in a Chinese Han Population. J Zhejiang Univ Sci B 14, 207–215 (2013).
Liu, H. N., Liu, Y. P., Xue, H. B., Deng, Y. Q. & Ling, Y. Association of Repair Gene Polymorphisms with Clinical Response to Platinum-Based Chemotherapy in Advanced Lung Cancer. Modern Medical Journal 659–661 (2013).
Zhao, W. et al. Polymorphisms in the Base Excision Repair Pathway Modulate Prognosis of Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer. Cancer Chemother Pharmacol 71, 1287–1295 (2013).
Li, X. D., Han, J. C., Zhang, Y. J., Li, H. B. & Wu, X. Y. Common Variations of Dna Repair Genes are Associated with Response to Platinum-Based Chemotherapy in Nsclcs. Asian Pac J Cancer Prev 14, 145–148 (2013).
Li, W. J. et al. Polymorphisms in Thymidylate Synthase and Reduced Folate Carrier () Genes Predict Survival Outcome in Advanced Non-Small Cell Lung Cancer Patients Treated with Pemetrexed-Based Chemotherapy. Oncol Lett 5, 1165–1170 (2013).
Cheng, H. et al. Predictive Effect of Xpa and Xpd Polymorphisms On Survival of Advanced Nsclc Patients Treated with Platinum-Based Chemotherapy: A Three-Dimensional (3-D), Polyacrylamide Gel-Based Dna Microarray Method. Technol Cancer Res Treat 12, 473–482 (2013).
Zhang, T. et al. Xpg is Predictive Gene of Clinical Outcome in Advanced Non-Small-Cell Lung Cancer with Platinum Drug Therapy. Asian Pac J Cancer Prev 14, 701–705 (2013).
Lee, S. Y. et al. Polymorphisms in Dna Repair and Apoptosis-Related Genes and Clinical Outcomes of Patients with Non-Small Cell Lung Cancer Treated with First-Line Paclitaxel-Cisplatin Chemotherapy. Lung Cancer 82, 330–339 (2013).
Mlak, R. et al. Predictive Value of Ercc1 and Rrm1 Gene Single-Nucleotide Polymorphisms for First-Line Platinum- And Gemcitabine-Based Chemotherapy in Non-Small Cell Lung Cancer Patients. Oncol Rep 30, 2385–2398 (2013).
Yuli, Y. et al. Xpg is a Novel Biomarker of Clinical Outcome in Advanced Non-Small-Cell Lung Cancer. Pak J Med Sci 29, 762–767 (2013).
Lu, H. D., Cui, E. H. & Hua, F. The Association Between the Susceptibility to Platinum Drugs and the Genetic Polymorphisms of Ercc1 and Bag -1 in Patients with Advanced Non-Small Cell Lung Cancer. China Modern Doctor 65–67 (2013).
Sheng, G. F. et al. Relationship of Xrcc1 and Efficacy of Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer. Jiangsu Med J 295–297 (2013).
Yang, W. J., Wang, N. J. & Chen, D. M. Mutation in Xrcc1, Polymorphism in Rrm1 and Efficacy of Platin-Based Chemotherapy in Patients with Advanced Non-Small Cell Lung Cancer. Journal of Ningxia Medical University 13–17 (2013).
Zhang, Y. P., Xue, H. B., Ling, Y., Liu, Y. P. & Sheng, G. F. Correlation Between the Polymorphisms in Xpd751 Gene and Sensitivity and Toxicity of Chemotherapy in Advanced Non-Small Cell Lung Cancer. Hainan Med J 648–650 (2013).
Zhou, G. R. et al. Effects of Genetic Polymorphisms of Xrcc1 On the Efficacy of Platinum-Based Chemotherapy for Advanced Nonsmall Cell Lung Cancer. Pract Geriatr 897–899 (2013).
Huang, S. J., Wang, Y. F., Jin, Z. Y., Sun, J. Y. & Guo, Z. L. Role of Ercc1 Variants in Response to Chemotherapy and Clinical Outcome of Advanced Non-Small Cell Lung Cancer. Tumour Biol 35, 4023–4029 (2014).
Zhang, L., Ma, W., Li, Y., Wu, J. & Shi, G. Y. Pharmacogenetics of Dna Repair Gene Polymorphisms in Non-Small-Cell Lung Carcinoma Patients On Platinum-Based Chemotherapy. Genet Mol Res 13, 228–236 (2014).
Jin, Z. Y. et al. Effects of Polymorphisms in the Xrcc1, Xrcc3, and Xpg Genes On Clinical Outcomes of Platinum-Based Chemotherapy for Treatment of Non-Small Cell Lung Cancer. Genet Mol Res 13, 7617–7625 (2014).
Hu, W., Pan, J., Zhao, P., Yang, G. & Yang, S. Genetic Polymorphisms in Xpg Could Predict Clinical Outcome of Platinum-Based Chemotherapy for Advanced Non-Small Cell Lung Cancer. Tumour Biol 35, 5561–5567 (2014).
Peng, Y. et al. Association of Dna Base Excision Repair Genes (Ogg1, Ape1 and Xrcc1) Polymorphisms with Outcome to Platinum-Based Chemotherapy in Advanced Nonsmall-Cell Lung Cancer Patients. Int J Cancer 135, 2687–2696 (2014).
Zhou, M. et al. Association of Xeroderma Pigmentosum Group D (Asp312Asn, Lys751Gln) and Cytidine Deaminase (Lys27Gln, Ala70Thr) Polymorphisms with Outcome in Chinese Non-Small Cell Lung Cancer Patients Treated with Cisplatin-Gemcitabine. Genet Mol Res 13, 3310–3318 (2014).
Zhao, X., Zhang, Z., Yuan, Y. & Yuan, X. Polymorphisms in Ercc1 Gene Could Predict Clinical Outcome of Platinum-Based Chemotherapy for Non-Small Cell Lung Cancer Patients. Tumour Biol 35, 8335–8341 (2014).
Lv, H. et al. Genetic Polymorphism of Gstp1 and Ercc1 Correlated with Response to Platinum-Based Chemotherapy in Non-Small Cell Lung Cancer. Med Oncol 31, 86 (2014).
Krawczyk, P. et al. Polymorphisms in Ts, Mthfr and Ercc1 Genes as Predictive Markers in First-Line Platinum and Pemetrexed Therapy in Nsclc Patients. J Cancer Res Clin Oncol 140, 2047–2057 (2014).
Sullivan, I. et al. Pharmacogenetics of the Dna Repair Pathways in Advanced Non-Small Cell Lung Cancer Patients Treated with Platinum-Based Chemotherapy. Cancer Lett 353, 160–166 (2014).
Dong, C. H., Kang, M. F., Zhao, Y. Y., Lin, J. & Tao, L. Y. Correlation of Methylenetetrahydrofolate Reductase (Mthfr) C677T Polymorphism and Chemotherapy Efficacy in Lung Adenocarcinoma. Chin J of Oncol Prev and Treat 35–38 (2014).
Liu, D., Wu, J., Shi, G. Y., Zhou, H. F. & Yu, Y. Role of Xrcc1 and Ercc5 Polymorphisms On Clinical Outcomes in Advanced Non-Small Cell Lung Cancer. Genet Mol Res 13, 3100–3107 (2014).
Kou, G., Liu, Z. T., Zhang, Z., Mei, Z. J. & Wang, S. H. Ercc1 Gene Polymorphism and Efficacy and Prognosis of Platinum Combination Regimens in Advanced Lung Adenocarcinoma Patients. The practical journal of cancer 483–485 (2014).
Kalikaki, A. et al. Ercc1 Snps as Potential Predictive Biomarkers in Non-Small Cell Lung Cancer Patients Treated with Platinum-Based Chemotherapy. Cancer Invest 33, 107–113 (2015).
Zou, H. Z. & Zhao, Y. Q. Xpg Polymorphisms are Associated with Prognosis of Advanced Non-Small Cell Lung Cancer Treated with Platinum-Based Doublet Chemotherapy. Genet Mol Res 14, 500–506 (2015).
Yuan, Z. J. et al. Association of Gstp1 and Rrm1 Polymorphisms with the Response and Toxicity of Gemcitabine-Cisplatin Combination Chemotherapy in Chinese Patients with Non-Small Cell Lung Cancer. Asian Pac J Cancer Prev 16, 4347–4351 (2015).
Deng, J. H., Deng, J., Shi, D. H., Ouyang, X. N. & Niu, P. G. Clinical Outcome of Cisplatin-Based Chemotherapy is Associated with the Polymorphisms of Gstp1 and Xrcc1 in Advanced Non-Small Cell Lung Cancer Patients. Clinical and Translational Oncology 17, 720–726 (2015).
Shi, Z. H., Shi, G. Y. & Liu, L. G. Polymorphisms in Ercc1 and Xpf Gene and Response to Chemotherapy and Overall Survival of Non-Small Cell Lung Cancer. Int J Clin Exp Pathol 8, 3132–3137 (2015).
Han, B. et al. Association of Gstp1 and Xrcc1 Gene Polymorphisms with Clinical Outcome of Advanced Non-Small Cell Lung Cancer Patients with Cisplatin-Based Chemotherapy. Int J Clin Exp Pathol 8, 4113–4119 (2015).
Li, P., Wang, Y. D., Cheng, J., Chen, J. C. & Ha, M. W. Association Between Polymorphisms of Bag-1 and Xpd and Chemotherapy Sensitivity in Advanced Non-Small-Cell Lung Cancer Patients Treated with Vinorelbine Combined Cisplatin Regimen. Tumour Biol 36, 9465–9473 (2015).
Liu, J. Y., Li, L. R. & Liu, Q. M. Association of Gstp1 and Xrcc1 Gene Polymorphisms with Clinical Outcomes of Patients with Advanced Non-Small Cell Lung Cancer. Genet Mol Res 14, 10331–10337 (2015).
Wu, G., Jiang, B., Liu, X., Shen, Y. & Yang, S. Association of Gsts Gene Polymorphisms with Treatment Outcome of Advanced Non-Small Cell Lung Cancer Patients with Cisplatin-Based Chemotherapy. Int J Clin Exp Pathol 8, 13346–13352 (2015).
Zhu, M. Z., Xu, H. Y., Zhu, Z. X. & J., H. Association of Genetic Polymorphisms of Hif-1Α and Ercc1 with the Short-Term Efficacy of Platinum Drugs for Advanced Non- Small Cell Lung Cancer. The practical journal of cancer 1276–1280 (2015).
Reed, E. Platinum-Dna Adduct, Nucleotide Excision Repair and Platinum Based Anti-Cancer Chemotherapy. Cancer Treat Rev 24, 331–344 (1998).
Yang, Y. & Xian, L. The Association Between the Gstp1 a313G and Gstm1 Null/Present Polymorphisms and the Treatment Response of the Platinum-Based Chemotherapy in Non-Small Cell Lung Cancer (Nsclc) Patients: A Meta-Analysis. Tumour Biol 35, 6791–6799 (2014).
Xu, T. P., Shen, H., Liu, L. X. & Shu, Y. Q. Association of Ercc1-C118T and -C8092a Polymorphisms with Lung Cancer Risk and Survival of Advanced-Stage Non-Small Cell Lung Cancer Patients Receiving Platinum-Based Chemotherapy: A Pooled Analysis Based On 39 Reports. Gene 526, 265–274 (2013).
Yu, D. et al. Pharmacogenetic Role of Ercc1 Genetic Variants in Treatment Response of Platinum-Based Chemotherapy Among Advanced Non-Small Cell Lung Cancer Patients. Tumour Biol 33, 877–884 (2012).
Yang, Y. & Xian, L. The Association Between the Ercc1/2 Polymorphisms and the Clinical Outcomes of the Platinum-Based Chemotherapy in Non-Small Cell Lung Cancer (Nsclc): A Systematic Review and Meta-Analysis. Tumour Biol 35, 2905–2921 (2014).
Huang, D. & Zhou, Y. Nucleotide Excision Repair Gene Polymorphisms and Prognosis of Non-Small Cell Lung Cancer Patients Receiving Platinum-Based Chemotherapy: A Meta-Analysis Based On 44 Studies. Biomed Rep 2, 452–462 (2014).
Gu, A. Q. et al. Xrcc1 Genetic Polymorphisms and Sensitivity to Platinum-Based Drugs in Non-Small Cell Lung Cancer: An Update Meta-Analysis Based On 4708 Subjects. Int J Clin Exp Med 8, 145–154 (2015).
Li, L., Wan, C. & Wen, F. Q. Polymorphisms in the Xrcc1 Gene are Associated with Treatment Response to Platinum Chemotherapy in Advanced Non-Small Cell Lung Cancer Patients Based On Meta-Analysis. Genet Mol Res 13, 3772–3786 (2014).
Wu, J. et al. Predictive Value of Xrcc1 Gene Polymorphisms On Platinum-Based Chemotherapy in Advanced Non-Small Cell Lung Cancer Patients: A Systematic Review and Meta-Analysis. Clin Cancer Res 18, 3972–3981 (2012).
Moll, S. & Varga, E. A. Homocysteine and Mthfr Mutations. Circulation 132, e6–e9 (2015).
Brambila-Tapia, A. J. Mdr1 (Abcb1) Polymorphisms: Functional Effects and Clinical Implications. Rev Invest Clin 65, 445–454 (2013).
Yin, J. Y., Huang, Q., Zhao, Y. C., Zhou, H. H. & Liu, Z. Q. Meta-Analysis On Pharmacogenetics of Platinum-Based Chemotherapy in Non Small Cell Lung Cancer (Nsclc) Patients. Plos One 7, e38150 (2012).
Wei, H. B. et al. Polymorphisms of Ercc1 C118T/C8092a and Mdr1 C3435T Predict Outcome of Platinum-Based Chemotherapies in Advanced Non-Small Cell Lung Cancer: A Meta-Analysis. Arch Med Res 42, 412–420 (2011).
Wacholder, S., Chanock, S., Garcia-Closas, M., El Ghormli, L. & Rothman, N. Assessing the Probability that a Positive Report is False: An Approach for Molecular Epidemiology Studies. JNCI Journal of the National Cancer Institute 96, 434–442 (2004).
Acknowledgements
This work was supported by the National Key Research and Development Plan (SQ2016YFSF110100, 2016YFC0905000), National Natural Science Foundation of China (81373490, 81573508, 81573463), Hunan Provincial Science and Technology Plan of China (2015JC3025), and Open Foundation of Innovative Platform in University of Hunan Province of China (421530004).
Author information
Authors and Affiliations
Contributions
L.M.T. and Z.Q.L. conceived and designed the study. L.M.T., C.F.Q., T.Z. and Y.X.J. acquired the data, performed data extraction. L.M.T. analyzed the data. L.M.T. wrote the paper. X.L., J.Y.Y., W.Z. and H.H.Z. provided valuable comments and important insights.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tan, LM., Qiu, CF., Zhu, T. et al. Genetic Polymorphisms and Platinum-based Chemotherapy Treatment Outcomes in Patients with Non-Small Cell Lung Cancer: A Genetic Epidemiology Study Based Meta-analysis. Sci Rep 7, 5593 (2017). https://doi.org/10.1038/s41598-017-05642-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-05642-0
This article is cited by
-
Genetic polymorphisms as potential pharmacogenetic biomarkers for platinum-based chemotherapy in non-small cell lung cancer
Molecular Biology Reports (2024)
-
The association between XRCC3 rs1799794 polymorphism and cancer risk: a meta-analysis of 34 case–control studies
BMC Medical Genomics (2021)
-
Genetic polymorphisms and haplotypes of ERCC1 and ERCC2 associated with quality of life, depression, and anxiety status among patients with lung cancer
BMC Cancer (2021)
-
Differential molecular markers of primary lung tumors and metastatic sites indicate different possible treatment selections in patients with metastatic lung adenocarcinoma
Clinical and Translational Oncology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.