Abstract
The digit ratio has been used as a retrospective noninvasive biomarker to investigate the putative effects of prenatal exposure to androgens. In recent years, many scholars have paid attention to the association between 2D:4D (the second and fourth digits) and prostatic cancer. This study explored the prognostic significance of digit ratio in prostate cancer patients. We reviewed the progressive status and survival of 382 prostate cancer patients who had received hormone therapy at our institutions. Survival of clinicopathological variables analyzed as categorical variables were determined by the log-rank test. According to Cox’s proportional hazards analysis, R2D:4D, L2D:4D, PSA at 6 month,bone metastasis were significant independent factors for prostate cancer. The risk of any progression of prostate cancer similarly depressed with increasing 2D:4D, for any progression (R2D:4D HR = 0.71, p = 0.003; L2D:4D HR = 0.67, p = 0.001), for cancer-specific death (R2D:4D HR = 0.67, p = 0.025; L2D:4D HR = 0.74, p = 0.036). Digit ratio may not only have predictive value in risk but also prognosis of prostatic cancer. This finding suggests that low 2D:4D can be used as prognostic factors to identify patients with a poor prognosis. These patients may benefit from more aggressive management.
Similar content being viewed by others
Introduction
Prostate cancer is one of the most common malignant tumors in men, with a reported incidence of 165.8 per 100, 0001. In China, it is known that prostate cancer is a serious public health problem. For now, this cancer is the second-leading cause of cancer deaths in men, after lung and bronchial cancer, according to the National Cancer Prevention Office. Although exact etiology of prostate cancer is currently unknown, it has been correlated to factors such as age, race, familial history, dietary habits and hormone exposure2.
The ratio between the second and fourth digits (2D:4D), also known as digit ratio is a proxy marker for the prenatal influence of sexual hormones - mainly testosterone and estrogen3,4,5. In mice, nineteen genes have been identified to influence in digit ratio establishment6, and the HOX, androgen receptor (AR) and LIN28B have been speculated to reflect on digit ratio in humans7, 8. These genes are correlated with prenatal testosterone (PT) or prenatal estrogen (PE), being up or down regulated by the exposure to these hormones. So digit ratio can be thought of as a candidate marker for the action of these genes, and, subsequently for it used as a predictor of hormone-related disease susceptibility9,10,11,12.
In 2002, Manning et al. started to focus on the possible links between 2D:4D and reproductive cancers (prostate, breast, ovary, uterus), they suggested that low 2D:4D may be negatively related to high PSA and high risk of prostate cancer13. Recently, prostate cancer is the neoplasm most connected to 2D:4D, which has been studied by several ethnic groups such as American, Australian, Brazilian, British, Indian, Korean, and Spanish9, 14,15,16,17,18,19,20. These groups have evaluated the influence of digit ratio over the prevalence and severity of prostate cancer, as well as prostatic specific antigen (PSA) and Gleason scores.
However, no correlative literature has investigated the association between digit ratio and survival in prostate cancer patients, whether digit ratio can be used to predict the progressive status and survival has not been reported as far as we know.
Based on such considerations, this study was undertaken to explore the prognostic significance of digit ratio in prostate cancer patients who had received hormone therapy at our institutions.
Methods
Participants
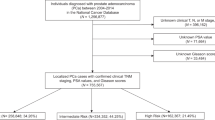
This study was performed in three large academic medical centers in china. Patients with prostate cancer were recruited from the oncology and urology department of The Second Affiliated Hospital Of XinJiang Medical University, Shandong Provincial Hospital, China-Japan Union Hospital of Jilin University, and met the following inclusion criteria: having a diagnosis of prostate adenocarcinoma and undergoing whole-course endocrine therapy at our institution.
The study population consisted initially of 926 patients who underwent endocrine therapy from march 2011 to march 2014 at our institutions. Patients were excluded for the following reasons: History of related radiation or surgery (n = 435); Histologic slides, Gleason score, PSA data or digit ratio values not available (n = 25); Not right-handed, skeletal dysplasias, or who had suffered from any kind of injuries to the fingers (n = 43); Lack of research authorization (n = 41). Nevertheless, sedatives or analgesic medication, limited operations to remove lower urinary tract obstructions (cystostomy or catheterization) were permitted.
The final study group consisted of 382 prostate cancer patients who were diagnosed pathologically at our institutions from march 2011 to march 2014. Among these participants, 337 patients were treated with endocrine therapy, using medical castration (using a luteinizing hormone-releasing hormone analogue) with antiandrogens, and the remaining 45 patients were treated with simple medical castration.
Our study was approved by The Ethics Committee of The XinJiang Medical University and all of the relevant hospitals. Informed consent was provided according to the Declaration of Helsinki and all of the patients’ guardians informed written consent. We confirming that all experiments were performed in accordance with relevant guidelines and regulations that promote respect for all human subjects and protect their health and rights.
Follow-up information
The median time of follow-up and the follow-up range were 45.0 months and 1–72 months, respectively.
All these patients were followed every month for the first 3 months and once every 3 months thereafter. Serum PSA levels, complete blood cell counts, blood chemistry studies, rectal examinations were recorded and analyzed. Serum levels of PSA were assayed by CanAg PSA ElA (CanAg Diagnostics AB). Meanwhile, chest x-rays and radionuclide bone scans (injection of 25 mCi Tc-99m methylene diphosphonate) were performed every 6 months. If the patient complained of subjective symptoms, computerized tomography of the abdomen and pelvis or abdominal ultrasonography was also performed to measure the disease’s progression. The TNM classification system was used for staging and the Gleason system was used for grading.
Any progression of the prostate cancer was defined as: (1) Progression to hormone refractory prostate cancer, when PSA increased after hormone treatment twice in succession and continued to increase even after suspension of flutamide; (2) Local recurrence, cancer on biopsy of prostatic bed without evidence of systemic recurrence. (3) Systemic progression, involved demonstrable metastatic deposits on biopsies, abdominal CT scan or bone scan. Prostate cancer death was defined as death in any patient with metastasis that showed any progression following hormonal therapy.
Digit measurement
Figure 1 shows how to measure the digit length. The 2D and 4D were measured by unified specially-trained investigators with a standard vernier caliper (recorded to 0.01 mm) from the basal palmar crease of the finger to the tip. This measurement has been previously reported providing a high degree of repeatability21, 22. When two creases were visible at the base of the digit, the crease proximal to the palm was chosen. The measurers had no information about the progression and therapy about the patients. All measurements were made twice by two investigators and the mean value was adopted. We got the 2D:4D values at the beginning of the treatment mostly. The intraclass correlation coefficient (ICC) of two repeated measures of digit ratio by a single investigator was 0.918. This direct measurement method is probably better, as indirect finger measurements (e.g. from photocopies or scans) may lead to distortions that result in consistently lower 2D:4D values23, 24.
Statistical analysis
For the analysis of the results, the patients were divided into groups according to 2D:4D (<0.950 versus ≥0.950), pathological Gleason score (<6 or 7 versus 8–10), initial PSA (<20, 20–99.9, 100–1000, >1000), PSA at 3 month (<4 versus ≥4), PSA at 6 month (<4 versus ≥4), bone metastasis (yes versus no), lung metastasis (yes versus no), lymph node metastasis (yes versus no), therapy (monotherapy versus combined) and pathological tumor stage (TX, T0, T1 or T2 or T3 versus T4).
All statistical analyses were performed by using the SPSS software (SPSS Inc., Chicago, Illinois) with a significance level of 0.05.
Variables of the different groups were compared using Student’s t test or Fisher’s exact test. Survival curves were constructed by the Kaplan-Meier method, survival of clinicopathological variables analyzed as categorical variables were determined by the log-rank test. Multivariate analysis was then performed according to the Cox proportional hazards regression model to determine the significant factor in predicting disease outcome. To obtain a multivariate model with the maximum precision of the important variables, a stepwise selection procedure was used.
Results
Follow up results
Patient characteristics of the study are summarized in Table 1, all of the participants were Chinese Han patients.
This study did not find a relationship between Gleason score and 2D:4D, but encountered significant negative correlation between 2D:4D and PSA at 3 months, 6 months after treatment (Table 2).
Among 382 patients, 281 (73.6%) patients had disease progression (as defined above), 117 (30.6%) died of prostate carcinoma, 11 (2.9%) were non-cancer related deaths, and 20 (5.2%) were excluded from analysis due to loss to follow-up after treatment.
Univariate and multivariate analysis
Individual parameters were evaluated using univariate analysis for possible correlation with any progression of prostate cancer, R2D:4D, L2D:4D, initial PSA, PSA at 6 month after treatment, bone metastasis, lymph node metastasis influenced the progression (Table 3). However, by multivariate analysis, stepwise inclusion of variables in the Cox’s proportional hazards model showed that the significant prognostic factors were R2D:4D, L2D:4D, initial PSA, PSA at 6 month, bone metastasis were significant independent factors (Table 4).
According to univariate analysis, R2D:4D, L2D:4D, initial PSA, PSA at 6 month after treatment, bone metastasis and lymph node metastasis affected the cancer-specific death (Table 3). However, Cox’s proportional hazards analysis using a stepwise inclusion of variables demonstrated that R2D:4D, L2D:4D, PSA at 6 month, bone metastasis were significant independent factors (Table 5).
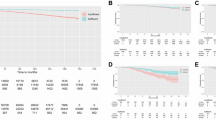
The survival curves
The risk of any progression of prostate cancer similarly depressed with increasing 2D:4D (Fig. 2). While patients with a higher 2D:4D were at nearly 0.7 depressed risk for any progression (R2D:4D HR 0.71, 95% CI 0.57–0.91, p = 0.003; L2D:4D HR 0.67, 95% CI 0.54–0.86, p = 0.001). Similarly, for cancer-specific death (Fig. 3), higher 2D:4D depressed the risk as well (R2D:4D HR 0.67, 95% CI 0.51–0.97, p = 0.025; L2D:4D HR 0.74, 95% CI 0.51–1.06, p = 0.036).
Discussion
Several converging lines of evidence suggest that prenatal hormone exposure is associated with digit ratio, and much of relevant evidence has been previously reviewed25. A direct evidence, Lutchmaya et al. reported that L2D:4D is negatively correlated with the ratio of testosterone to oestradiol measured by amniocentesis in the second trimester3. HOX genes regulate the embryogenesis, morphogenesis and cell differentiation of human, including the genitals and digits, and they have been suggested to be deregulated in malignant tumors26, 27. In primary prostate cancer cells, HOX8 or MSX2 gene expressions are greatly reduced, followed by a gradual increase in more aggressive prostate cancer cell lines28. Despite the controversy and criticism29, it has been postulated that digit ratio was associated with the CAG repeats number in the AR (androgen receptors) genes30. It is generally known that testosterone and AR play crucial roles in prostate growth and the progress of prostate cancer. The short CAG repeats of AR have been reported to be associated with the pathogenesis of prostate cancer31, 32. Furthermore, the polymorphisms of AR gene may occur in advanced prostate cancer, which became resistant to hormonal treatment33, 34.
Recently, many experts and scholars had a strong interest in the relation between 2D:4D and prostate. In a case-control study, compared with low 2D:4D men, abnormal development (persistence of mid-line cyst formation) of the prostate was more common in men with high 2D:4D. This suggests that 2D:4D may relate to the normal development of prostate35. In another convincing study, the researchers found that the digit ratio is a predictor of the response to dutasteride (one inhibitor of the action of 5α-reductase) treatment36. This suggests that the 2D:4D may be linked to the function of the prostate. In tumor research studies, prostate cancer is the cancer most connected to 2D:4D, which is considered to develop as a result of hormonal carcinogenesis. Whereby hormones promote cell division and cell proliferation, and the accumulation of genetic mutations that arise during the process of cell division eventually result in a malignant phenotype37.
In 2010, a significant study to evaluate the correlations between 2D:4D and prostate cancer found that individuals with a higher risk of prostate biopsy possessing high levels of PSA presented lower 2D:4D values20. Then, in a major cohort study in the United Kingdom, researchers have proposed that 2D:4D may be a simple marker of prostate cancer risk, with length of 2D greater than 4D suggestive of lower risk9. Another investigation in 2012, the Korean researchers found an association between 2D:4D, prostate cancer volume and Gleason score after investigating 770 men with lower urinary tract symptoms38. However, in 2013, one US study found lower right-hand digit ratios for African-Americans with prostate cancer in comparison to Caucasians, but no significant differences for Gleason scores14. Similarly, in our study, we found no correlation between 2D:4D and Gleason scores either. Such differences may reside in the different evaluation of digit ratios, technique use, data processing mode and the different backgrounds of the samples (patients condition and prognosis, ethnic). In short, prostate cancer is a kind of multifactorial disease and influenced by both ethnic, environmental and genetic factors, larger multi-center prospective study may be necessary for further research.
In 2011, when we started this research, we measured the digit ratio and collected the relevant data of prostate cancer patients to examine whether 2D:4D is associated with prostate cancer risk. At that time, more and more attentions were paid to this subject in academia, and many major studies carried out. Then, we noted that all of these experiments restricted to investigations on the relationship between 2D:4D and risk (prevalence or severity) of prostate cancer, whether associations exist between 2D:4D and the disease prognosis was never mentioned. So, based on previous researches, we turned our attention to the prognostic significance of digit ratio in prostate cancer patients. During an average follow-up of 45.0 months, we found that digit ratio may not only have predictive value in risk but also prognosis of prostatic cancer finally.
Due to limited practical condition and research competence, our study has several potential limitations. Prostate cancer is indolent tumor that has long survival, even with metastases39. In our study, with relatively short-term following up, the number of outcome events was limited. Therefore, our results should be considered preliminary. So, longer-term studies are desperately needed to catch more significant differences in the progression.
Actually, the use of 2D:4D for outcome prediction may be not as straightforward as the result suggest. The main reason is that ethnic groups differ in mean 2D:4D. In a meta-analysis on Chinese 2D:4D, of the results of 28 studies (19,093 participants), the left 2D:4D was 0.951 in Chinese men, Q (26) = 658.61, P < 0.001, and the right 2D:4D was 0.948, Q (28) = 753.56, P < 0.00140. After analyzing the data of relevant research, it was found that the 2D:4D in Chinese individuals (Han ethnicity) was found to be higher than in Black populations but lower than in Caucasians and Hispanics41,42,43. These ethnic differences in 2D:4D further indicate that genetic factors likely affect the 2D:4D. Furthermore, the diagnosis, therapy and prognosis of prostatic cancer show significant differences in different countries and nationality44, 45.For instance, the screening of prostate cancer in China is not as widespread as in Western countries, and the age-adjusted incidence and mortality rates of prostate cancer in Asia are much lower than Europe and the United States. In conclusion, due to all of the participants are Chinese Han in our study, the conclusion may be specific to the particular ethnic and regional composition of our study sample.
Since Huggins and Hodges found the beneficial effect of androgen ablation on metastatic prostate cancer in 194146. androgen deprivation therapy, specifically medical castration, has been the first line treatment for advanced prostate cancer. And, there have been many experiments to study diverse prognostic factors for prostate cancer47,48,49. In our study, the results indicate that digit ratio may be associated with the prognosis of patients with prostate cancer, and 2D:4D can be used as prognostic factors to identify patients with a poor prognosis, who may benefit from more aggressive management. At present, detailed interpretation of this result is difficult due to the fact that we can only provide an indication that prenatal androgen exposure might be associated with the prognosis of prostatic cancer, the biochemical pathway or molecular mechanism cannot be explained systematically. Here we offer two possible explanations: 1) differences in fetal exposure to androgens or the sensitivity of AR may be related to the appearance and proliferation of the receptor-negative tumour cells, and 2) by other possible mechanism of gene regulation, prenatal androgen exposure may be associated with the proliferation, invasion, migration, apoptosis and multi drug resistance of tumor cells.
In conclusion, despite this current limitation, 2D:4D remains a simple, easy to measure marker of prenatal androgen exposure which may not only have predictive value in risk but also prognosis of prostatic cancer.
References
Edwards, B. K. et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 116, 544–73 (2010).
Hsing, A. W. & Chokkalingam, A. P. Prostate cancer epidemiology. Frontiers in Bioscience. 11(11), 1388 (2006).
Lutchmaya S, Baron-Cohen S, Raggatt P, Knickmeyer R, Manning J. T. 2nd to 4th digit ratios, fetal testosterone and estradiol. Early Hum Dev. 77, 23–28.
Manning, J. T. et al. The ratio of 2nd to 4th digit length: a predictor of sperm numbers and concentrations of testosterone, luteinizing hormone and oestrogen. Human Reproduction. 13(11), 3000–3004 (1998).
Hönekopp, J. & Watson, S. Meta-analysis of digit ratio 2D:4D shows greater sex difference in the right hand. American Journal of Human Biology. 22(5), 619–630 (2010).
Zheng, Z. & Cohn, M. J. Developmental basis of sexually dimorphic digit ratios. Developmental Biology. 108(39), 16289 (2011).
Manning, J. T., Callow, M. & Bundred, P. E. Finger and toe ratios in humans and mice: implications for the aetiology of diseases influenced by HOX genes. Med Hypotheses. 60, 340–3 (2003).
Medland, S. E. et al. A variant in LIN28B is associated with 2D:4D finger-length ratio, a putative retrospective biomarker of prenatal testosterone exposure. Am J Hum Genet. 86, 519–25 (2010).
Rahman, A. A. et al. Hand pattern indicates prostate cancer risk. Br J Cancer. 104, 175–177 (2011).
Muller, D. C. et al. Second to fourth digit ratio (2D:4D), breast cancer risk factors, and breast cancer risk: a prospective cohort study. Br J Cancer. 107, 1631–1636 (2012).
Neyse, L. et al. Overconfidence, Incentives and Digit Ratio. Scientific Reports. 6, 23294 (2016).
Li, G. et al. 2D:4D indicates phimosis risk: A study on digit ratio and early foreskin development. Early Human Development. 99, 21 (2016).
Manning J. T. Digit Ratio: A Pointer to Fertility, Behavior, and Health. Rutgers University Press. (2002).
Waters, M. et al. Second to fourth digit ratio and prostate cancer severity. Prostate Cancer & Prostatic Diseases. 16, 107–110 (2013).
Muller, D. C. et al. Second to fourth digit ratio (2D:4D) and prostate cancer risk in the Melbourne Collaborative Cohort Study. Br J Cancer. 105, 438–440 (2011).
Hopp, R. N. & Jorge, J. Right hand digit ratio (2D:4D) is associated with prostate cancer: findings of an admixed population study. J Solid Tumors. 2, 22–25 (2012).
Mendes, P. H. et al. Comparison of digit ratio (2D:4D) between Brazilian men with and without prostate cancer. Prostate Cancer & Prostatic Diseases. 19, 107–110 (2016).
Ashraf, M., Mohan, T. & Fernandes, E. Hand patterns in prostatic cancers. Losr Journal of Dental & Medical Sciences. 13(3), 72–74 (2014).
Jung, H., Kim, K. H., Yoon, S. J. & Kim, T. B. Second to fourth digit ratio: a predictor of prostate-specific antigen level and the presence of prostate cancer. BJU Int. 107, 591–596 (2010).
García-Cruz, E. et al. Higher second fourth digit ratio predicts higher incidence of prostate cancer in prostate biopsy. Arch Esp Urol. 65, 816–821 (2013).
Scutt, D. & Manning, J. T. Symmetry and ovulation in women. Hum Reprod. 11, 2477–80 (1996).
Manning, J. T. Fluctuating asymmetry and bodyweight in men and women: implications for sexual selection. Ethol Sociobiol. 16, 145–52 (1995).
Manning, J. T. et al. Photocopies Yield Lower Digit Ratios (2D:4D) Than Direct Finger Measurements. Archives of Sexual Behavior. 34(3), 329–333 (2005).
Ribeiro, E. et al. Direct Versus Indirect Measurement of Digit Ratio (2D:4D): A Critical Review of the Literature and New Data. Evolutionary Psychology. 1, 8 (2016).
McIntyre, M. H. The use of digit ratios as markers for perinatal androgen action. Reproductive Biology and Endocrinology. 4, 10 (2006).
Nunes, F. D., de Almeida, F. C., Tucci, R. & de Sousa, S. C. Homeobox genes: a molecular link between development and cancer. Pesqui Odontol Bras. 17, 94–98 (2003).
Takahashi, Y. et al. Expression profiles of 39 HOX genes in normal human adult organs and anaplastic thyroid cancer cell lines by quantitative real-time RT-PCR system. Exp Cell Res. 293, 144–153 (2004).
Chua, C. W. et al. Differential expression of MSX2 in nodular hyperplasia, high-grade prostatic intraepithelial neoplasia and prostate adenocarcinoma. Apmis. 118, 918–926 (2010).
Hönekopp, J. No Evidence that 2D:4D is Related to the Number of CAG Repeats in the Androgen Receptor Gene. Frontiers in Endocrinology. 4, 185–185 (2013).
Manning, J., Bundred, P. & Flanagan, B. The ratio of 2nd to 4th digit length: a proxy for transactivation activity of the androgen receptor gene? Medical Hypotheses. 59(3), 334–336 (2002).
Giovannucci, E. et al. The CAG repeat within the androgen receptor gene and its relationship to prostate cancer. Proceedings of the National Academy of Sciences. 94(7), 3320–3 (1997).
Stanford, J. L. et al. Polymorphic repeats in the androgen receptor gene: molecular markers of prostate cancer risk. Cancer Res. 15(57), 1194–8 (1997).
Taplin, M. E. et al. Selection for androgen receptor mutations in prostate cancers treated with androgen antagonist. Cancer Res. 59, 2511–2515 (1999).
Th, V. D. et al. Androgen receptors in endocrine-therapy-resistant human prostate cancer. International Journal of Cancer Journal International Du Cancer. 48(2), 189 (1991).
Furuya, S. et al. Novel insight for midline cyst formation in prostate:The involvement of decreased prenatal testosterone suggested by second-to-fourth digit ratio study. International Journal of Urology. 22(11), 1063–7 (2015).
Kim, T. B. et al. Dutasteride, who is it more effective for? Second to fourth digit ratio and the relationship with prostate volume reduction by dutasteride treatment. Bju International. 110(11c), 857–63 (2012).
Henderson, B. E. & Feigelson, H. S. Hormonal carcinogenesis. Carcinogenesis. 21(3), 427 (2000).
Oh, J. K., Kim, K. H., Jung, H., Yoon, S. J. & Kim, T. B. Second to fourth digit ratio: its relationship with core cancer volume and Gleason score in prostate biopsy. Int Braz J Urol. 38, 611–9 (2012).
Schmid, H. P., McNeal, J. E. & Stanley, T. A. Clinical observations on the doubling time of prostate cancer. Eur Urol. 23, 60–63 (1993).
Xu, Y. & Zheng, Y. The digit ratio (2D:4D) in China: A meta-analysis. American Journal of Human Biology. 27(3), 304–309 (2014).
Brañasgarza, P., Kovářík, J. & Neyse, L. Second-to-fourth digit ratio has a non-monotonic impact on altruism. Plos One. 8(4), e60419 (2013).
Manning, J. T., Stewart, A. & Bundred, P. E. et al. Sex and ethnic differences in 2nd to 4th digit ratio of children. Early Human Development. 80(2), 161–168 (2004).
Mcfadden, D. et al. A Reanalysis of Five Studies on Sexual Orientation and the Relative Length of the 2nd and 4th Fingers (the 2D:4D Ratio). Archives of Sexual Behavior. 34(3), 341–356 (2005).
Robbins, A. S. et al. Differences in prognostic factors and survival among white and Asian men with prostate cancer, California, 1995-2004. American Journal of Epidemiology. 110(1), 1255–1263 (2007).
Sim, H. G. & Cheng, C. W. Changing demography of prostate cancer in Asia. Eur J Cancer. 41, 834–45 (2005).
Cooper, E. H. et al. Prostatic specific antigen and the prediction of prognosis in metastatic prostatic cancer. Cancer suppl. 66, 1025 (1990).
Rigaud, J. et al. Prognostic value of bone scan in patients with metastatic prostate cancer treated initially with androgen deprivation therapy. European Urology Supplements. 2(1), 1423 (2003).
Akashi, T. et al. Tissue factor expression and prognosis in patients with metastatic prostate cancer. Urology. 62(6), 1078–1082 (2003).
Benaim, E. A., Pace, C. M., Lam, P. M. & Roehrborn, C. G. Nadir P-SA as a progression to androgen-independent prostate cancer. Urology. 59, 73 (2002).
Acknowledgements
We would like to thank all participants. We also thank the collaborators from The Second Affiliated Hospital Of XinJiang Medical University, Shandong Provincial Hospital, and China-Japan Union Hospital of Jilin University for help with the collection of data. Also contributing to the study were researchers from the Peking University, XinJiang Medical University, Shandong University, as well as medical workers and health centers. This work is supported by the Xinjiang medical university Researcher innovation project startup Foundation of China (CXCY2017066).
Author information
Authors and Affiliations
Contributions
All authors have contributed significantly in the content of the manuscript. Guanjian Li proposed the study and wrote the first draft. Jie Guo and Ying Zhang performed project design. Shixing Li, Bo Li, Jing Cao, Pengfei Lu, Jiajia Yang, Xin Yang, Le Gao, Yi He and Tao Cui acquired data and drafted the figures. Bin Ma is the guarantor, provided senior oversight for design, analysis and interpretation. All authors contributed to the design and interpretation of the study and to further drafts.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, G., Sun, K., Guo, J. et al. Prognostic significance of the digit ratio after hormone therapy for prostate cancer: a prospective multicenter study. Sci Rep 7, 5229 (2017). https://doi.org/10.1038/s41598-017-05638-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-05638-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.