Abstract
Capillary electrophoresis-time-of-flight mass spectrometry (CE-TOFMS) is a comprehensive, quantitative, and high throughput tool used to analyze metabolite profiles. In the present study, we used CE-TOFMS to profile metabolites found in the blood plasma of 33 medication-free patients with major depressive disorder (MDD) and 33 non-psychiatric control subjects. We then investigated changes which occurred in the metabolite levels during an 8-week treatment period. The medication-free MDD patients and control subjects showed significant differences in their mean levels of 33 metabolites, including kynurenine (KYN), glutamate (Glu), glutamine (Gln), methionine sulfoxide, and methionine (Met). In particular, the ratios of KYN to tryptophan (TRP), Gln to Glu, and Met to methionine sulfoxide were all significantly different between the two groups. Among the 33 metabolites with altered levels in MDD patients, the levels of KYN and Gln, as well as the ratio of Gln to Glu, were significantly normalized after treatment. Our findings suggest that imbalances in specific metabolite levels may be involved in the pathogenesis of MDD, and provide insight into the mechanisms by which antidepressant agents work in MDD patients.
Similar content being viewed by others
Introduction
Major depressive disorder (MDD) is a common neuropsychiatric disorder with a lifetime prevalence of 16.2%1. Although various neurobiological-based hypotheses for the cause of MDD have been proposed2, the molecular mechanisms which underlie this disorder remain obscure.
Metabolomics utilizes instruments that can simultaneously quantitate thousands of small molecules in a biological sample3. Metabolite levels reflect the final response of an organism to environmental factors, genetic modifications, changes in gut microflora, and altered enzyme kinetic activity. Therefore, individual metabolic state is most closely related to phenotype among other omics technologies, such as genome, transcriptome, and proteome4. Capillary electrophoresis-time-of-flight mass spectrometry (CE-TOFMS) is a comprehensive, quantitative, and high throughput tool used to analyze metabolic profiles5,6,7. To date, CE-TOFMS has been used to identify abnormalities of blood metabolites in patients with major depression (MDD), bipolar disorder, schizophrenia, and autism spectrum disorder8,9,10. However, the study which investigated MDD was conducted in a very small cohort of 9 MDD patients and 19 control subjects9.
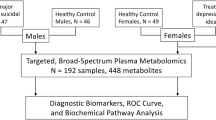
In the present study, we used CE-TOFMS to comprehensively profile metabolites found in the blood plasma of 33 medication-free patients with MDD and 33 non-psychiatric control subjects. Next, we examined correlations which existed between depression severity and the plasma levels of various metabolites. Finally, we followed the patients for 8 weeks to identify any changes which occurred in their metabolite levels.
Materials and Methods
Subjects
Thirty-three medication-free patients with MDD were recruited from Tokushima University Hospital in Japan. The diagnosis of MDD was made according to Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria by at least 2 expert psychiatrists on the basis of extensive clinical interviews and a review of medical records. We also followed up 10 patients who received a naturalistic course of treatment with an antidepressant (paroxetine n = 4, duloxetine n = 2, mirtazapine n = 1, or sertraline n = 3). Clinical symptoms were evaluated using the Hamilton Depression Rating Scale (HDRS) at baseline and again after 8 weeks of treatment11. Thirty-three age- and sex-matched non-psychiatric healthy control subjects were recruited from hospital staff, students, and company employees who were documented to be free of psychiatric problems and had no past history of mental illness. All participants were of unrelated and of Japanese origin. This study was conducted in accordance with the World Medical Association’s Declaration of Helsinki. The study protocol was approved by the institutional ethics committee of Tokushima University, and all enrolled subjects provided their signed written informed consent for participation.
Quantitative metabolome analysis
A blood sample was collected from each participant during their morning visit to the hospital. Blood plasma was isolated via centrifugation at 2,000 g for 10 minutes; after which, the plasma-containing supernatant fraction was frozen at −80 °C until further use. 50 μL of plasma sample was added to 450 μL of methanol containing 10 μM each internal standard (internal standard solution: H3304-1002; Human Metabolome Technologies, Inc.). Then, 200 μL of Milli-Q water and 500 μL chloroform were added, and the solution was centrifuged at 2300 g for 5 min at 4 °C. 400 μL of the supernatant was centrifugally filtrated through 5-kDa cut-off filter (UltrafreeMC-PLHCC 250/pk, Human Metabolome Technologies) to remove proteins. The filtrate was centrifugally concentrated in a vacuum evaporator and dissolved in 50 μl of Milli-Q water containing reference compounds before CE-TOFMS analysis. The levels of various metabolites in the plasma samples were measured using a CE-TOFMS system located at Human Metabolome Technologies, Inc. (Yamagata, Japan). Target metabolites were identified by matching their mass-to charge ratio (m/z) values and migration times with the annotation table of the metabolomic library (Human Metabolome Technologies). The relative area for each metabolite was defined as the relative concentration. Details of the procedure of sample preparation and the CE-TOFMS conditions and procedures used to analyze the CE-TOFMS data are described elsewhere7,8,9.
Statistical analyses
Welch’s t-test was used to compare the levels of each metabolite in the MDD group with its corresponding level in the control group. A false discovery rate (FDR) correction with a significance threshold of 0.05 was applied for multiple testing. Changes which occurred in metabolite levels following treatment with an antidepressant were assessed using a paired t-test. Receiver operating characteristic (ROC) curve analyses of candidate metabolites were performed to discriminate between the MDD and control group, and values for area under the curve (AUC) were obtained. Spearman’s rank correlation coefficient was used to examine relationships between metabolite relative concentrations and clinical symptoms as evaluated by the HDRS. Statistical calculations of Welch’s t-test, paired t-test, and mean ± standard deviation (SD) were carried out using Microsoft Excel 2013 software. ROC curve values and Spearman’s rank correlation coefficients were calculated using R ver 3.2.5. software.
Results
Demographics
Some clinical characteristics of the subjects in the two groups are shown in Table 1. There were no significant differences regarding the age and sex of the subjects in the the medication-free MDD group and control group. Depressive symptoms as evaluated by the HDSR were significantly improved after 8 weeks treatment with an antidepressant (mean HDSR score at baseline: 21.0 ± 6.3; mean HDSR score at 8 weeks: 8.5 ± 5.5, p = 0.007; paired t-test).
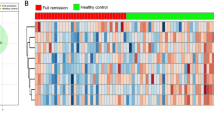
Differences in metabolites found in the MDD patients and control subjects
A total of 263 candidate peaks (148 cationic compounds and 115 anionic compounds) were detected by CE-TOFMS in our cohort of 66 participants. Among the 263 peaks, 246 peaks were assigned to specific metabolites. 246 metabolite relative concentrations of each individual subject are shown in Supplementary Table S1. Among these 246 metabolites, 106 metabolites, which were present in at least 80% of all subjects (≧53 subjects), were analyzed. Among the 106 metabolites, the levels of 33 metabolites were significantly different in the medication-free MDD group and control group (FDR q < 0.05; Welch’s t-test) (Table 2). Among those 33 metabolites, the levels of 11 metabolites were higher in the MDD group than in the control group. For example, decreased levels of kynurenine (KYN) and 5-Methoxyindoleacetic acid (5-MIAA), which are associated with tryptophan (TRP) metabolism, were found in the MDD group (FDR q = 0.0096 and 0.016, respectively). Increased glutamate (Glu) levels and decreased glutamine (Gln) levels were found in the MDD group (FDR q = 3.7 × 10−7 and 4.8 × 10−7, respectively) (Fig. 1). This was deemed important, because both Glu and Gln are associated with glutamatergic neurotransmission. Furthermore, the ratios of KYN to TRP, Gln to Glu, and methionine (Met) to methionine sulfoxide in the MDD group were lower than those in the control group (p = 5.4 × 10−4, 1.3 × 10−13, and 5.6 × 10−12, respectively) (Table 3).
Plasma amino acid levels in medication-free patients with major depressive disorder (MDD) and controls. Y axis represents relative metabolic levels. Bars indicate mean levels in the group. (a) Kynurenine were significantly lower in MDD patients than in control subjects (FDR q = 0.0096). (b) The levels of 5-Methoxyindoleacetic acid were significantly lower in MDD patients than in control subjects (FDR q = 0.016). (c) Glutamate levels were significantly higher in MDD patients than in control subjects (FDR q = 3.7 × 10−7). (d) Glutamine levels were significantly lower in MDD patients than in control subjects (FDR q = 4.8 × 10−7).
Next, we performed ROC analyses to examine the power of metabolite relative concentrations to diagnose MDD. An AUC value for each metabolite relative concentration is shown in Table 2. Methionine sulfoxide, an oxidation product of methionine and a possible biomarker of oxidative stress12, was able to discriminate medication-free MDD patients from the control subjects, and showed the best AUC among 35 metabolites examined (AUC = 0.97, sensitivity 0.91, and specificity 0.97).
Relationship between metabolite relative concentrations and depressive symptoms
We examined relationships between the relative concentrations of 106 metabolites and the depressive symptoms of the MDD patients as evaluated by their HDSR scores. We found nominally positive correlations between the relative concentrations of 6 metabolites (isoleucine, leucine, 2-hydroxybutyric acid, valine, 3-hydroxybutyric acid, and 2-aminoadipic acid) and HDSR scores (r = 0.593, r = 0.473, r = 0.421, r = 0.448, r = 0.424, r = 0.367, and r = 0.354, respectively; p < 0.05; Spearman rank correlations). However, only the correlation between a patient’s isoleucine relative concentration and their symptoms reached statistical significance when assessed by multiple comparisons (FDR q < 0.05).
Metabolite changes following 8 weeks of treatment with antidepressants
Among the 33 metabolites that displayed altered levels in medication-free MDD patients, only two metabolites (Gln and KYN) showed significant changes in their levels after 8 weeks of treatment with antidepressants (Table 4). The levels of both Gln and KYN were significantly increased after treatment (p = 3.3 × 10−4 and 3.8 × 10−3, respectively; paired-t test). Furthermore, the ratio of Gln to Glu was also significantly increased after treatment (p = 6.6 × 10−4). While the KYN to TRP ratio was increased to its control level after treatment, the increase did not reach statistically significance (p = 0.074). On the other hand, the Met to methionine sulfoxide ratio remained unchanged after treatment (p = 0.61).
Discussion
In this study, we used CE-TOFMS to comprehensively profile the metabolites found in blood plasma from medication-free MDD patients and control subjects, and identified novel differential metabolites as well as imbalances of specific metabolite in the plasma of medication-free MDD patients. An organism’s metabolite levels are regarded as its final response to environmental factors, which include treatment with medications. Moreover, several studies have demonstrated that antidepressants influence the levels of certain metabolites13, 14. Therefore, we analyzed samples of blood plasma obtained from medication-free MDD patients in an attempt to identify a precise metabolite signature for MDD. Furthermore, we conducted a longitudinal study which examined changes in metabolite abnormalities that occurred after treating MDD patients with antidepressants.
We found that plasma from medication-free MDD patients contained significantly decreased levels of Gln, increased levels of Glu, and had an altered Gln/Glu ratio. However, the abnormal Gln levels and Gln/Glu ratio became significantly normalized after 8 weeks of treatment with antidepressants. In a glutamatergic synapse, the released neurotransmitter is internalized by astrocytes through high affinity sodium-dependent glutamate transporters, and then transformed into Gln by the astrocyte-specific enzyme, glutamine synthetase, and released into the extracellular space, from which it is taken up into neurons through the neutral amino acid transporter and transformed back to Glu by phosphate-activated glutaminase15. The complete series of steps from neuronal glutamate release to resynthesis of glutamate from glutamine is called the Glu-Gln cycle16, and the Gln/Glu ratio is regarded as a potentially useful index for Glu-Gln cycle in neuronal-glial interactions and the balance of glutamatergic metabolites17,18,19. The abnormal Gln and Glu levels and Gln/Glu ratio found in MDD patients in this study suggest that abnormalities in the Glu-Gln cycle may be involved in the pathogenesis of MDD. Consistent with our results, elevated blood Glu levels in MDD patients20,21,22,23,24 as well as decreased plasma Gln in drug-naive MDD patients have been reported25. In the current study, the plasma Gln levels in MDD patients were increased after treatment with antidepressants, while the plasma Glu levels following treatment remained unchanged. However, results from other studies have suggested that antidepressant agents might decrease plasma Glu levels in MDD patients24, 26. When taken together, the above findings suggest that antidepressant agents may normalize glutamatergic abnormalities by increasing Gln levels and decreasing Glu levels.
We found significantly decreased levels of KYN and 5-MIAA, as well as significantly altered KYN/TRP ratio in the plasma samples from medication-free MDD patients. The abnormal KYN levels were significantly normalized following 8 weeks of treatment with antidepressants. Serotonin is synthesized from ~1% of the available TRP in the body, and TRP is catabolized into KYN by tryptophan 2,3-dioxygenase27. 5-MIAA is metabolite formed within the methoxyindole branch of the TRP pathway. The abnormalities of KYN, 5-MIAA, and the KYN/TRP ratio found in this study implicate disruption of the TRP pathway in the pathogenesis of MDD. Consistent with our results, a previous study which used liquid-chromatography-tandem mass spectrometry (LC-MSMS) has reported decreased serum KYN levels in drug-free MDD patients28. However, conflicting results have also been reported29, 30. These discrepancies between studies may primarily result from whether their respective patient populations received medications, as we found elevated plasma KYN levels and a trend towards elevated KYN/TRP ratio after the patients in our study had been treated with antidepressants. Previous studies have reported elevated serum KYN levels and KYN/TRP ratio during the course of antidepressant treatment in MDD patients31, 32.
We found significantly increased levels of methionine sulfoxide, decreased levels of Met, and altered Met/methionine sulfoxide ratio in samples of blood plasma collected from medication-free MDD patients. The abnormal levels of methionine sulfoxide and Met and the abnormal ration of these two metabolites did not significantly change after 8 weeks of treatment with antidepressants. Met is a sulfur-containing essential amino acid, and is used as the first amino acid during the protein translation process. As a result, Met is often a limiting factor for protein synthesis under conditions of Met deficiency33. Met also participates in one-carbon metabolism, and decreased levels of Met may be associated with aberrant DNA methylation in MDD34. Methionine sulfoxide is a primary oxidation product of Met via its nucleophilic oxidation, and this amino acid can be regarded as a biomarker of oxidative stress12. Accumulating evidence implicates oxidative stress in the pathogenesis of MDD35, 36. Consistent with our findings, a previous study showed that a 6-week course of antidepressant treatment did not alter the oxidative-antioxidative systems in MDD patients37. However, several clinical studies have shown the efficacy of adjunctive treatment with the antioxidant compound, N-acetylcysteine, in MDD patients38, 39.
We found a significant positive correlation between isoleucine relative concentration and depression severity. Isoleucine is one of branched-chain amino acids (BCAAs), and this amino acid is transported across the blood-brain barrier as nutrient signals and nitrogen donors in neurotransmitter synthesis and Glu-Gln cycle40. Consistent with our findings, depressive-like symptoms in rats following chronic administration of BCAAs41 and an association between plasma isoleucine concentration and the severity of MDD have been observed42. On the other hand, decreased blood concentrations of BCAAs in patients with MDD treated with antidepressants in comparison with healthy controls and negative correlations between BCAAs concentrations and the severity of MDD have also been reported43.
When we compared with our data of MDD with a previous blood study of bipolar disorder using CE-TOFMS10, increased Glu levels and decreased cis-Aconitic acid levels, which is an intermediate product of the citric acid cycle, have been commonly observed between studies. These results suggest that not only glutamatergic abnormalities but also abnormalities in the citric acid cycle may be commonly involved in the pathogenesis of mood disorders.
Our study has several limitations that should be mentioned. First, the sample size was relatively small, and larger studies are needed to confirm our results. Second, the patients were not all treated with the same antidepressants. Thus further studies which use specific treatment protocols are required. Third, we examined metabolite levels in samples of peripheral blood gathered from MDD patients. However, those metabolite levels may not have reflected the status of metabolites in the brain tissue of those MDD patients. On the other hand, some of the altered plasma metabolites described in the present study have also been identified in samples of brain tissues and cerebrospinal fluid (CSF). For example, a postmortem study has revealed increased Glu levels in MDD patients44. Moreover, proton magnetic resonance spectroscopy (1HMRS) studies have demonstrated reduced Gln levels in the hippocampus and pregenual anterior cingulate cortex of unmedicated MDD patients, as well as increased Glu levels in the occipital cortex region45,46,47. Furthermore, abnormality of the Gln/Glu ratio in the CSF of MDD patients and impaired Glu-Gln cycle in the brains of depressed patients have been observed19, 48. A high-performance liquid chromatography study has also revealed reduced ethanolamine levels in the CSF of MDD patients49. Fourth, we did not take potential confounding factors, such as body mass index and smoking status into consideration in our analysis due to lack of these information. Finally, the blood samples used in our study were collected when the patients visited the hospital in the morning; therefore, the interval between final food intake and blood draw was not unified, and we cannot rule out that food consumption and drinking may have affected the metabolite levels.
In conclusion, we described specific metabolite signatures that were found in samples of blood plasma obtained from medication-free MDD patients. We also conducted a longitudinal study that identified changes which occurred in those signatures after the patients had been treated with antidepressants. Our results suggest that imbalances of specific metabolites may be involved in the pathogenesis of MDD, and provide insight into the mechanisms by which antidepressants affect MDD.
References
Kessler, R. C. et al. The Epidemiology of Major Depressive Disorder. JAMA 289, 3095–105 (2003).
Miller, A. H. & Raison, C. L. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat. Rev. Immunol. 16, 22–34 (2015).
Kaddurah-Daouk, R. & Krishnan, K. R. R. Metabolomics: A Global Biochemical Approach to the Study of Central Nervous System Diseases. Neuropsychopharmacology 34, 173–186 (2009).
Klupczyńska, A., Dereziński, P. & Kokot, Z. J. Metabolomics In Medical Sciences–Trends, Challenges And Perspectives. Acta Pol. Pharm. 72, 629–41 (2015).
Soga, T. et al. Quantitative Metabolome Analysis Using Capillary Electrophoresis Mass Spectrometry. J. Proteome Res. 2, 488–494 (2003).
Soga, T. et al. Differential metabolomics reveals ophthalmic acid as an oxidative stress biomarker indicating hepatic glutathione consumption. J. Biol. Chem. 281, 16768–76 (2006).
Soga, T. et al. Metabolomic profiling of anionic metabolites by capillary electrophoresis mass spectrometry. Anal. Chem. 81, 6165–74 (2009).
Koike, S. et al. A snapshot of plasma metabolites in first-episode schizophrenia: a capillary electrophoresis time-of-flight mass spectrometry study. Transl. Psychiatry 4, e379 (2014).
Kageyama, Y. et al. Search for plasma biomarkers in drug-free patients with bipolar disorder and schizophrenia using metabolome analysis. Psychiatry Clin. Neurosci. 71, 115–123 (2017).
Yoshimi, N. et al. Blood metabolomics analysis identifies abnormalities in the citric acid cycle, urea cycle, and amino acid metabolism in bipolar disorder. BBA Clin. 5, 151–8 (2016).
Williams, J. B. W. et al. A Structured Interview Guide for the Hamilton Depression Rating Scale. Arch. Gen. Psychiatry 45, 742–7 (1988).
Mashima, R., Nakanishi-Ueda, T. & Yamamoto, Y. Simultaneous determination of methionine sulfoxide and methionine in blood plasma using gas chromatography-mass spectrometry. Anal. Biochem. 313, 28–33 (2003).
Kaddurah-Daouk, R. et al. Pharmacometabolomic mapping of early biochemical changes induced by sertraline and placebo. Transl. Psychiatry 3, e223 (2013).
Zhu, H. et al. Pharmacometabolomics of response to sertraline and to placebo in major depressive disorder - possible role for methoxyindole pathway. PLoS One 8, e68283 (2013).
Bak, L. K., Schousboe, A. & Waagepetersen, H. S. The glutamate/GABA-glutamine cycle: aspects of transport, neurotransmitter homeostasis and ammonia transfer. J. Neurochem. 98, 641–653 (2006).
Rothman, D. L., De Feyter, H. M., de Graaf, R. A., Mason, G. F. & Behar, K. L. 13C MRS studies of neuroenergetics and neurotransmitter cycling in humans. NMR Biomed. 24, 943–57 (2011).
Hashimoto, K. Abnormalities of the glutamine–glutamate–GABA cycle in the schizophrenia brain. Schizophr. Res. 156, 281–282 (2014).
Hall, M.-H. et al. Frontal P3 event-related potential is related to brain glutamine/glutamate ratio measured in vivo. Neuroimage 111, 186–191 (2015).
Hashimoto, K. et al. Abnormality in glutamine-glutamate cycle in the cerebrospinal fluid of cognitively intact elderly individuals with major depressive disorder: a 3-year follow-up study. Transl. Psychiatry 6, e744 (2016).
Kim, J. S., Schmid-Burgk, W., Claus, D. & Kornhuber, H. H. Increased serum glutamate in depressed patients. Arch. Psychiatr. Nervenkr 232, 299–304 (1982).
Altamura, C. A. et al. Plasma and platelet excitatory amino acids in psychiatric disorders. Am. J. Psychiatry 150, 1731–3 (1993).
Mauri, M. C. et al. Plasma and platelet amino acid concentrations in patients affected by major depression and under fluvoxamine treatment. Neuropsychobiology 37, 124–9 (1998).
Mitani, H. et al. Correlation between plasma levels of glutamate, alanine and serine with severity of depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 30, 1155–8 (2006).
Küçükibrahimoğlu, E. et al. The change in plasma GABA, glutamine and glutamate levels in fluoxetine- or S-citalopram-treated female patients with major depression. Eur. J. Clin. Pharmacol. 65, 571–577 (2009).
Zheng, P. et al. Plasma metabonomics as a novel diagnostic approach for major depressive disorder. J. Proteome Res. 11, 1741–8 (2012).
Maes, M., Verkerk, R., Vandoolaeghe, E., Lin, A. & Scharpé, S. Serum levels of excitatory amino acids, serine, glycine, histidine, threonine, taurine, alanine and arginine in treatment-resistant depression: modulation by treatment with antidepressants and prediction of clinical responsivity. Acta Psychiatr. Scand. 97, 302–308 (1998).
Myint, A. M. Kynurenines: from the perspective of major psychiatric disorders. FEBS J 279, 1375–1385 (2012).
Hu, L.-J. et al. A Simple HPLC-MS/MS Method for Determination of Tryptophan, Kynurenine and Kynurenic Acid in Human Serum and its Potential for Monitoring Antidepressant Therapy. J. Anal. Toxicol. doi:10.1093/jat/bkw071 (2016).
Myint, A.-M. et al. Kynurenine pathway in major depression: Evidence of impaired neuroprotection. J. Affect. Disord. 98, 143–151 (2007).
Hughes, M. M. et al. Tryptophan depletion in depressed patients occurs independent of kynurenine pathway activation. Brain. Behav. Immun. 26, 979–987 (2012).
Myint, A. M. et al. Tryptophan metabolism and immunogenetics in major depression: a role for interferon-γ gene. Brain. Behav. Immun. 31, 128–33 (2013).
Dahl, J. et al. Ongoing episode of major depressive disorder is not associated with elevated plasma levels of kynurenine pathway markers. Psychoneuroendocrinology 56, 12–22 (2015).
Lee, B. C. & Gladyshev, V. N. The biological significance of methionine sulfoxide stereochemistry. Free Radic. Biol. Med. 50, 221–227 (2011).
Numata, S. et al. Blood diagnostic biomarkers for major depressive disorder using multiplex DNA methylation profiles: Discovery and validation. Epigenetics 10, 135–141 (2015).
Smaga, I. et al. Oxidative stress as an etiological factor and a potential treatment target of psychiatric disorders. Part 2. Depression, anxiety, schizophrenia and autism. Pharmacol. Reports 67, 569–580 (2015).
Maurya, P. K. et al. The role of oxidative and nitrosative stress in accelerated aging and major depressive disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry 65, 134–44 (2016).
Sarandol, A. et al. Major depressive disorder is accompanied with oxidative stress: short-term antidepressant treatment does not alter oxidative-antioxidative systems. Hum. Psychopharmacol. 22, 67–73 (2007).
Carvalho, A. F., Macêdo, D. S., Goulia, P. & Hyphantis, T. N. N-acetylcysteine augmentation to tranylcypromine in treatment-resistant major depression. J. Clin. Psychopharmacol. 33, 719–20 (2013).
Berk, M. et al. The efficacy of adjunctive N-acetylcysteine in major depressive disorder: a double-blind, randomized, placebo-controlled trial. J. Clin. Psychiatry 75, 628–36 (2014).
Conway, M. E. & Hutson, S. M. In 99–132, doi:10.1007/978-3-319-45096-4_5 (Springer International Publishing, 2016).
Scaini, G. et al. Behavioral responses in rats submitted to chronic administration of branched-chain amino acids. JIMD Rep. 13, 159–67 (2014).
Setoyama, D. et al. Plasma Metabolites Predict Severity of Depression and Suicidal Ideation in Psychiatric Patients-A Multicenter Pilot Analysis. PLoS One 11, e0165267 (2016).
Baranyi, A. et al. Branched-Chain Amino Acids as New Biomarkers of Major Depression - A Novel Neurobiology of Mood Disorder. PLoS One 11, e0160542 (2016).
Hashimoto, K., Sawa, A. & Iyo, M. Increased Levels of Glutamate in Brains from Patients with Mood Disorders. Biol. Psychiatry 62, 1310–1316 (2007).
Sanacora, G. et al. Subtype-specific alterations of gamma-aminobutyric acid and glutamate in patients with major depression. Arch. Gen. Psychiatry 61, 705–13 (2004).
Block, W. et al. Proton MR spectroscopy of the hippocampus at 3 T in patients with unipolar major depressive disorder: correlates and predictors of treatment response. Int. J. Neuropsychopharmacol. 12, 415–22 (2009).
Walter, M. et al. The relationship between aberrant neuronal activation in the pregenual anterior cingulate, altered glutamatergic metabolism, and anhedonia in major depression. Arch. Gen. Psychiatry 66, 478–86 (2009).
Zhao, J. et al. Prefrontal changes in the glutamate-glutamine cycle and neuronal/glial glutamate transporters in depression with and without suicide. J. Psychiatr. Res. 82, 8–15 (2016).
Ogawa, S. et al. Reduced cerebrospinal fluid ethanolamine concentration in major depressive disorder. Sci. Rep. 5, 7796 (2015).
Acknowledgements
The authors would like to thank all the volunteers who understood our study purpose and participated in this study, and the physicians who helped us to collect clinical data and blood samples at the mental hospitals. The authors would also like to thank Mrs. Akemi Okada for her technical assistance. This work was supported in part by Japan Agency for Medical Research and development, AMED (T.O.), Grant-in-Aid for Scientific Research (C) (No. 15K09809) (S.N.).
Author information
Authors and Affiliations
Contributions
Numata designed the study, Ohmori and Numata managed the research, and Kinoshita, Numata, Tomioka, Umehara, and Watanabe collected the samples. Numata and Umehara performed the experiments. Ohmori and Nikawa helped to interpret data and edited the manuscript. Hatakeyama, Nakahara, and Umehara analyzed the data. Umehara and Numata wrote the draft of this paper. All authors contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
Dr. Ohmori has received research support or speakers’ honoraria from, or has served as a consultant to, Astellas, Chugai, Daiichi Sankyo, Dainippon Sumitomo, Ehzai, Eli Lilly, Glaxo SmithKline, Janssen, Meiji Seika Pharma, Mochida, MSD, Novartis, Otsuka, Ono, Pfizer, Shionogi, Takeda and Yoshitomi.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Umehara, H., Numata, S., Watanabe, Sy. et al. Altered KYN/TRP, Gln/Glu, and Met/methionine sulfoxide ratios in the blood plasma of medication-free patients with major depressive disorder. Sci Rep 7, 4855 (2017). https://doi.org/10.1038/s41598-017-05121-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-05121-6
This article is cited by
-
Effects of pharmacological treatment on metabolomic alterations in animal models of depression
Translational Psychiatry (2022)
-
Metabolomic alterations in the blood plasma of older adults with mild cognitive impairment and Alzheimer’s disease (from the Nakayama Study)
Scientific Reports (2022)
-
Oxytocin-induced increase in N,N-dimethylglycine and time course of changes in oxytocin efficacy for autism social core symptoms
Molecular Autism (2021)
-
The kynurenine pathway in major depressive disorder, bipolar disorder, and schizophrenia: a meta-analysis of 101 studies
Molecular Psychiatry (2021)
-
Antidepressants in inflammatory bowel disease
Nature Reviews Gastroenterology & Hepatology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.