Abstract
The present study aims to examine and compare the predictors of changes in self-reported sleep duration in older adults. A total of 2,294 participants over the age of 65 in the Shih-Pai Sleep Study were followed-up for an average of 3 years. According to the self-reported sleep duration at baseline and the results of a follow-up survey conducted 3 years later, participants were classified into three categories: mid-range sleepers (6–7 hours), short sleepers (≤5 hours), and long sleepers (≥8 hours). The main outcome variable was the sleep duration at the follow-up survey. A comparison of the results of the baseline and follow-up surveys revealed that only 45.9% of participants remained in the same spectrum of sleep duration in both surveys, with baseline long sleepers having the lowest consistency rate (27.6%). Only incident diseases, with the exception of prevalent diabetes and physical disability, predicted shortening of sleep duration. In contrast, prevalent morbidities or baseline characteristics correlated with the lengthening of sleep duration. The findings suggested that the self-estimated sleep duration fluctuated in a significant proportion of study participants over time. Predictors of lengthening of sleep duration were essentially different from predictors of shortening of sleep duration.
Similar content being viewed by others
Introduction
In the past decade, several studies that investigated the relationship between extreme sleep duration and health have consistently reported that short/long sleep duration per se or change in sleep duration were predictors of elevated risk of adverse health outcomes1,2,3,4. As a result of a recent professional consensus, an optimal sleep duration has been recommended for adults5. However, the underlying mechanisms that link short/long sleep duration to adverse health outcomes remain unclear. Regarding its association with morbidity and mortality, deviant sleep duration may act as a direct or indirect causative factor, a mediator, or a confounder; moreover, it may have a reverse causal or bidirectional relationship with adverse outcomes5. Understanding the temporal relationship is fundamental to establishing the direction of the association between short/long sleep duration and its correlates. Moreover, evidence from cross-sectional studies indicates two distinct sets of correlates for short and long sleep duration6, 7. Thus, the two ends of the sleep duration spectrum may differ in their effects and underlying causes or predictors, and warrant specific investigation and intervention8.
While many studies have investigated the relationship between short/long sleep duration and specific outcomes, very little is known about factors that are antecedent to short/long sleep duration9. Although factors that predict change in mid-range sleep duration have been recently reported in a Chinese older cohort, other important factors that are also crucial for the development of short/long sleep duration, such as depression and sleep-related parameters10, have not been investigated. Furthermore, predictors of changes from one end of the sleep duration spectrum to the other over time remain unclear. Accordingly, longitudinal studies that examine the predictors of short/long sleep duration are particularly important for elucidating the phenomenon of short/long sleep duration and for enhancing our ability to formulate effective interventions. Therefore, in the present study, we aimed to prospectively explore and compare factors that predict short/long sleep duration in community-dwelling older adults.
Methods
Study design and participants
The present study is a part of the Shih-Pai Sleep Study (SSS), wherein a fixed cohort of community-dwelling older adults was followed-up at 3-year intervals. The study cohort was established during 1999–2002 (the first wave) in Shih-Pai area, Taipei, Taiwan. In the first wave survey (T1), a total of 4,064 older adults participated in the investigation. According to the official registration database in 1999, 9,141 older adults aged ≥65 years resided in the Shih-Pai area. Excluding 1,990 ineligible older adults (institutionalized, died before interview, vacant households), a total of 7,151 eligible participants were included in the study. After door-to-door visits, 3,087 eligible participants did not complete the interview because of refusal to participate or not being successfully contacted for three visits. The response rate in the first wave was 56.8%. There were no significant differences in the distribution of age and sex between the final participants and the registered data (1999) for the population aged ≥65 years in the entire city of Taipei. Details of the baseline survey in the SSS have been described elsewhere11. In the first wave, 4,064 participants had a self-reported night sleep duration and they were followed-up from 2003 to 2005 (the second wave). In the second wave survey, 560 eligible participants were lost to follow-up because of death before the follow-up interview. Another 1,210 older adults were excluded owing to refusal to participate in the second wave survey, not being contacted after three visits, or vacant households. In the second wave (T2), a total of 2,294 participants in the baseline survey completed the follow-up investigation. Excluding the dead individuals, the follow-up response rate was 65.5%. The institutional review board of Taipei Veterans General Hospital and National Yang-Ming University approved this study. Informed consents were obtained from all participants. All methods were performed in accordance with the relevant guidelines and regulations.
Definition of outcome variables
The self-reported sleep duration was estimated using a single question from the Pittsburgh Sleep Quality Index (PSQI): “During the past month, how many hours of actual sleep did you get at night?”12. The sleep duration was categorized using hourly units. Since a non-linear relationship has been observed between sleep duration and mortality in older adults11, 13,14,15,16,17,18, and the mechanisms linking short and long sleep durations with adverse health outcomes may differ8, the main outcome variable for the present study was categorically subgrouped as a self-reported short, long, or mid-range sleep duration. In the literature, ≥9 hours of night sleep is regarded as the cutoff for an unfavorable long sleep duration for older adults5, 19. However, several studies using different cohorts in Taiwan consistently demonstrated that ≥8 hours of night sleep was the lowest cutoff that correlated with adverse health outcomes, including mortality risk11, 13, 20, sarcopenia21, weaker hand grip strength22 and poor cardiac autonomic control23. In addition, in the SSS cohort, only a few participants reported ≥9 hours of sleep in both T1 and T2 (see Supplementary Table S1). Therefore, individuals who slept ≥8 hours were defined as self-reported long sleepers in the present study. Moreover, a sleep duration ≤5 hours has been consistently regarded as unfavorable with respect to the risk for various morbidities and mortality5. Therefore, older adults who reported a sleep duration ≤5 hours were defined as short sleepers. Accordingly, the mid-range sleep duration was defined as 6–7 hours.
Definition of candidate predictors
In addition to basic demographic data, history of smoking and alcohol consumption and anthropometric data were collected. Body height and weight data were collected unless the participants were physically disabled and were unable to cooperate. For participants with this condition, information regarding height and weight was presented as ‘physical disability’. Body mass index (BMI) values of 18.0 kg/m2 and 25.0 kg/m2 were used as cut-off points for defining underweight and overweight in older adults, respectively24.
With respect to chronic medical morbidities, self-reported information about hypertension, diabetes mellitus and cardic disease (heart failure, myocardial infarction, and coronary events) were collected. Medical diseases were recorded as present only for participants who reported both a diagnosis and a treatment experience that included prescribed medications or non-pharmacological interventions. To examine whether incident diseases predict the development of short/long sleep duration, the status of medical diseases during the follow-up period were further categorized into incident cases (absent at baseline but present in the follow-up survey), persistent cases (present at both points of the survey), and healthy (absent at both points of the survey). Pain severity in the past 1 month was evaluated with a single item question. Severity was scaled as none, mild, moderate, or severe. Moderate and severe pain was categorized as significant pain.
Depressive symptoms were evaluated using the Geriatric Depression Scale - Short Form. Participants with scores >5 were considered to have significant depression25. Owing to the possibility of remission, the status of depression during the follow-up period was categorized into four subgroups, including no depression across two waves of the survey, incident depression, remitted depression, and sustained depression. Habitual snoring was assessed with a question that includes the following responses: none, mild, moderate, and severe. Those who reported mild habitual snoring were defined as prominent snorers, and those who had moderate and severe habitual snoring were categorized as disturbing snorers. Sleep quality was assessed with the PSQI. The cutoff for PSQI-defined poor sleep quality was a score >512. Finally, the number of nights in the last 4 weeks that the participants needed hypnotics to fall asleep was assessed. Frequent users of hypnotics were defined as those who were exposed to hypnotics for ≥14 nights in the past 4 weeks.
Statistical analysis
Statistical analyses were performed using SPSS for Windows, version 13.0 (SPSS Inc., Chicago, IL, USA). In addition to univariate analyses with the χ2 test, multinomial logistic regression analyses were conducted to identify independent factors that predicted a shift in the sleep duration category in the follow-up survey. Potential predictors, including sociodemographic characteristics, lifestyle factors, anthropometrics, physical or mental comorbidities and sleep-related parameters, were entered using the forced entry option into the multinomial logistic regression models. In all final models, a p-value < 0.05 was considered statistically significant.
Results
A total of 2,294 participants successfully completed the two waves of the survey at an average interval of 2.9 ± 0.5 years (range: 1.5–4.3 years). A comparison between the demographic and clinical characteristics of the participants that were successfully followed and those that were lost to follow-up is summarized in Table 1. Participants who were lost to follow-up were more likely to be ≥75 years old (p < 0.001), illiterate (p < 0.001), single/widowed/separated/divorced (p < 0.001), physically disabled (p < 0.001), current smokers (p = 0.02), and depressed (p < 0.001; Table 1).
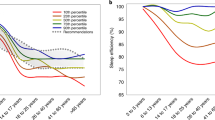
At baseline (T1, the first wave survey), 53.4% (n = 1226), 26.7% (n = 612), and 19.9% (n = 456) were short, mid-range, and long sleepers, respectively. At follow-up (T2, the second wave survey), 51.1% (n = 1173) of participants were mid-range sleepers, 30.4% (n = 697) were short sleepers, and 18.4% (n = 424) were long sleepers. The self-reported sleep duration between T1 and T2 differed significantly (χ2 = 70.5, df = 4, p < 0.001). The number of short sleepers at T2 appeared to be more than that at T1. Figure 1 depicts the change in the proportion of participants in different sleep duration categories between T1 and T2. Only 45.9% individuals remained in the same category of sleep duration from T1 to T2. Strikingly, a total of 47.5% of T1 short sleepers and 44.3% of T1 long sleepers became mid-range sleepers at T2. In addition, 12.3% of T1 short sleepers and 28.1% of T1 long sleepers changed to the opposite end of the sleep duration spectrum at T2. Furthermore, up to 72.4% of T1 long sleepers shifted to other categories of sleep duration. The details of the distribution of the self-reported sleep duration in 1-hour intervals across two surveys can be found in Supplementary Table S1.
To examine predictors of a shift in self-reported sleep duration category, multinomial logistic regressions were performed in each category of T1 sleep duration. Among T1 mid-range sleepers, individuals with incident depression (OR = 2.31, 95% CI: 1.35–3.95), incident diabetes (OR = 2.19, 95% CI: 1.19–4.02), prevalent diabetes (OR = 1.66, 95% CI: 1.05–2.63), or incident cardiac diseases (OR = 1.86, 95% CI: 1.20–2.87) were more likely to change into short sleepers at T2. In parallel, current smoking (OR = 1.76, 95% CI: 1.12–2.75) and prevalent diabetes (OR = 2.12, 95% CI: 1.31–3.45) were predictors of a change into long sleepers at T2 (Table 2).
Table 3 summarizes the factors that predicted a shift to longer sleep duration among T1 short sleepers. Regarding long sleep duration at T2, T1 short sleepers with poor sleep quality (OR = 2.14, 95% CI: 1.06–4.34) or BMI ≥25 kg/m2 (OR = 2.38, 95% CI: 1.10–5.14) were more likely to become long sleepers at T2 than their counterparts without these predictors were. Furthermore, T1 short sleepers who were current alcohol drinkers had a higher likelihood of being in the mid-range sleep category at T2 (OR = 2.15, 95% CI: 1.05–4.41).
Finally, factors that were associated with shortening of sleep duration at T2 among T1 long sleepers are shown in Table 4. T1 long sleepers who were physically disabled at T1 (OR = 2.59, 95% CI: 1.30–5.18) or had incident hypertension during the follow-up period (OR = 2.78, 95% CI: 1.13–6.87) were more likely to become short sleepers at T2. In parallel, individuals with incident depression were less likely to have mid-range sleep duration at T2 (OR = 0.33, 95% CI: 0.12–0.92).
Table 5
summarizes the predictors of a change in self-reported sleep duration across each category of baseline sleep duration.
Discussion
Although sleep attainment is a potentially modifiable behavior, sleep duration in young adults is often self-imposed in order to satisfy social demand and could be corrected by direct behavioral modification. In contrast, sleep duration in older adults, who are usually in the retired status, is more likely driven by the underlying pathomechanism. To the best of our knowledge, this is the first study that used a large cohort of community-dwelling older adults to examine predictors for deviant self-reported sleep duration. Not only a comprehensive set of candidate predictors but also the impact of the change of disease status was evaluated. The results of the present study indicate that the self-estimated sleep duration fluctuated in a significant proportion of study participants over time. Predictors of lengthening of sleep duration were essentially different from predictors of shortening of sleep duration. These findings of temporal sequence provide some evidence for the unsolved issue of short/long self-reported sleep duration.
The inconsistency of self-reported sleep duration across the survey period
Using a large older cohort, the present study showed that only 45.9% of individuals remained in the same category of sleep duration in both surveys, and baseline long sleepers had the lowest consistency rate (27.6%). To the best of our knowledge, the change in sleep duration has not been considered in studies examining the relationship between short/long sleep duration and mortality in older adults. Numerous studies have reported the effect of a change in sleep duration on mortality risk in younger adults, including the Whitehall II cohort and the British Household Panel Survey in England and the Older Finnish Twin cohort in Finland1, 26, 27. Among these three cohorts, the rates of a consistent self-reported sleep duration across two waves of surveys ranged from 67.4–71.8% (follow-up period: 4–7 years). In comparison to the literature, the follow-up period of the present study was shorter (3 years), but the rate of consistent sleep duration across surveys was lower. Although the cutoffs for sleep duration varied among different cohorts, mid-range sleepers consistently had the highest rates of consistent sleep duration across surveys. In two of the above-mentioned cohorts, individuals who were long sleepers at baseline also had the lowest rate (23.5–40.0%) to remain in the same category at follow-up26, 27. In most studies investigating sleep in older adults, the follow-up period for mortality events was longer than 3 years. Our findings suggest that the self-reported sleep duration of older adults may change to a greater extent during the follow-up period in comparison to younger adults. If only the baseline sleep duration is used to predict adverse events, the time-dependent self-reported sleep duration may introduce bias when examining the link between sleep duration and adverse health outcomes in older adults.
Predictors for incident short sleep duration among mid-range sleepers
A bidirectional relationship was observed between type II diabetes and poor sleep quality. Short sleep duration increased the risk for developing type II diabetes4, 28, 29, and symptoms and complications of type II diabetes were found to affect sleep quality30. In contrast, although short sleep duration has been well illustrated to predict elevated risk for cardiovascular disease3, and depression31, 32, only a few studies have examined whether the reverse exists. Compared with the present study, except for diabetes mellitus, baseline physical/mental comorbidities surprisingly failed to predict shortening sleep duration. Instead, incident physical or mental conditions, including incident diabetes mellitus, cardiac disease and depression, were closely related to short sleep duration in the follow-up survey. Because the history of medical illness at baseline was confirmed by both self-reported diagnosis and the respective treatment experience, the acute impact of these prevalent diseases on sleep may have been mitigated by the effect of treatment. Uniquely, unlike other physical diseases, both incident and prevalent diabetes mellitus predicted a shortening of the sleep duration among mid-range sleepers. The symptoms or complications of diabetes mellitus, such as nocturia, nocturnal hypoglycemia, peripheral neuropathy, restless legs syndrome, and sleep-disordered breathing, may constitute the link between prevalent diabetes mellitus and shortening of sleep duration33. Owing to a 3-year follow-up interval, it was not possible to discern the exact temporal sequence between incident diseases and incident short sleep duration. However, these incident physical/mental morbidities appear to be closely associated with short sleep duration in a temporal manner. According to our findings, the recent appearance of diabetes mellitus, cardiac disease, and depression indicates an elevated risk of shortening of sleep duration, which may further predispose an individual to other medical conditions known to be precipitated by sleep insufficiency in older adults.
Predictors for incident long sleep duration among mid-range sleepers
In the literature, little is known about factors affecting the development and maintenance of long sleep duration. The present study showed that prevalent diabetes mellitus and current smoker at the baseline survey predicted lengthening of sleep duration. Prevalent diabetes mellitus was an unusual predictor of change in sleep duration in the present study because it predicted not only shortening but also lengthening of sleep duration among baseline mid-range sleepers. Because various complications may develop during the course of diabetes mellitus, the chronic impact of the disease or the severity of associated complications may explain the bidirectional predictive ability of diabetes mellitus33. In addition, smokers in the first wave of survey were also found to have lengthened sleep duration at follow-up survey. In contrast, smoking was found to be correlated with short sleep duration in previous cross-sectional studies34, 35. Similar to diabetes mellitus, it may be the long-term impact of smoking, such as COPD or emphysema, rather than its immediate influence that increases bed confinement and induces changes in sleep duration during the follow-up interval.
Differential patterns of predictors for short/long sleepers
In studies with a cross-sectional design, the characteristics of correlates for short and long sleep differ in many domains, such as sociodemographics6, life style36, anthropometric measurement21, cardiac autonomic control23, hand grip strength22, medical morbidities37, psychological profile38, sleep-related parameters39, and types of medication use6. Compared to a long sleep duration, a short sleep duration is associated with several correlates and demonstrates better morbidity prediction. However, regarding the mortality risk, long sleep may even be more robust than short sleep5. Therefore, the pathomechanisms underlying the two ends of the sleep duration are believed to be different8. The findings of the present prospective study also revealed that the number of predictors for short sleep is greater than that for long sleep duration. Besides, except for disability, physical/mental incident comorbidities also have a closer relationship with short sleep duration. In contrast, lifestyle- or behavior-related chronic conditions such as smoking, prevalent diabetes mellitus, obesity, and poor sleep quality predicted the lengthening of sleep duration. This finding suggests that shortening of sleep duration might be more closely related to biologically mediated mechanisms and lengthening of sleep duration might be more likely associated with non-specific risk factors for a process of failing health. These differences in the prediction pattern for short/long sleep duration were in line with those demonstrated in previous cross-sectional studies. Besides, the pattern of predictors for short/long sleep duration observed in the present study also supported the contention that short sleep duration affects health via comorbidities and long sleep may simply non-specifically reflects the process of failing health. However, this differential pattern should be interpreted with caution. Long sleep duration, instead of short sleep duration, was identified as a risk factor for mortality in a previous study using this SSS cohort11. Older adults who developed long sleep duration but died before the second wave of the survey introduce a selection bias and could contribute to the differing pattern of predictors.
Predictors of switching to the opposite end of self-reported sleep duration
Among baseline short sleepers, obese older adults and those with poor sleep quality were more likely to become long sleepers than their counterparts were. Because obesity is a risk factor for sleep-disordered breathing, prolonged sleep duration may be a compensatory consequence of hypoxemia. In a previous large cross-sectional study, disrupted sleep and the use of sleeping medication were associated with both short sleep and long sleep duration in older adults6. Compared to the present prospective study, hypnotic use and poor sleep quality failed to predict a change in sleep duration among mid-range sleepers. This finding suggests that the relationship between baseline sleep quality and the sleep duration at follow-up may be moderated by the baseline sleep duration. In contrast to mid-range and long sleepers, baseline short sleepers with poor sleep quality may develop compensatory sleep to a greater extent.
In contrast with short sleep duration, the mechanisms that explain the link between long sleep duration and adverse health outcomes remain unclear5. In a previous meta-analysis, long sleep duration was correlated with a higher risk of cardiovascular mortality40. In addition, a previous study that used an identical cohort from the SSS also found an independently elevated risk of cardiovascular mortality in long sleepers11. In comparison, the present study revealed that long sleepers with incident hypertension were more likely to change to short sleepers 3 years later. The reciprocal interaction between short sleep duration and hypertension may result in a vicious cycle that increases the risk for cardiovascular mortality. Thus, the association between baseline long sleep duration and the risk for cardiovascular mortality may be partly related to the change of sleep duration during the follow-up period. Furthermore, long sleepers with disability were also prone to becoming short sleepers at the follow-up survey. Older adults with disability may initially have longer sleep duration because of prolonged bed confinement, but may develop short sleep duration because of inadequate activity level, which can compromise sleep homeostasis.
Limitations
There are a few limitations to the present study. First, subjectively estimated sleep duration may be biased. Second, subjective sleep duration in older adults may represent the behavioral consequence of lifestyle-related issues. Failure to control for the effect of physical activity may also have introduced bias. Third, the sleep duration on the weekend may differ from that on weekdays. In the present study, a snapshot of the sleep duration in the past month may have over- or under-estimated the average sleep duration and may have introduced bias. However, the difference between the sleep duration on the weekend and weekdays was minimal among older adults in Taiwan in comparison to that in young adults41. Future studies examining the factors that predict a change in the sleep duration should differentiate between weekend and weekday sleep, particularly in the younger population. Fourth, some other medical conditions such as cancer and primary sleep disorders were not included as candidate predictors in the present study. Because medical morbidities often confound or increase the likelihood of reverse causality in the relationship between extreme sleep duration and adverse outcomes42. Fifth, the present study did not evaluate participants’ cognitive function, which may have biased the self-reported sleep duration. Although the cognitive demand to complete the interview in the SSS should equate to a certain level of cognitive function in participants, future studies investigating the predictors of changes in the self-reported sleep duration should assess cognitive function directly. Finally, the present study was conducted in community-dwelling older adults residing in an urban area. Therefore, caution should be exercised in generalizing these results to institutionalized older adults and individuals with different sociodemographic backgrounds.
Conclusions
In conclusion,the present study indicates that self-reported sleep duration tends to fluctuate with time. Moreover, the patterns of predictors for developing short/long sleep duration appear to be essentially different. Considering the association between extreme sleep durations and adverse outcomes, knowledge of these predictors may aid the development of suitable preventive interventions. In the future, a larger cohort with higher frequencies of follow-up is necessary to determine the nature of the differential pattern.
References
Ferrie, J. E. et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep 30, 1659–1666 (2007).
Cappuccio, F. P. et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31, 619–626 (2008).
Cappuccio, F. P., Cooper, D., D’Elia, L., Strazzullo, P. & Miller, M. A. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European Heart Journal 32, 1484–1492, doi:10.1093/eurheartj/ehr007 (2011).
Cappuccio, F. P., D’Elia, L., Strazzullo, P. & Miller, M. A. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 33, 414–420, doi:10.2337/dc09-1124 (2010).
Watson, N. F. et al. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. Sleep 38, 1161–1183, doi:10.5665/sleep.4886 (2015).
Ohayon, M. M. Interactions between sleep normative data and sociocultural characteristics in the elderly. Journal of Psychosomatic Research 56, 479–486, doi:10.1016/j.psychores.2004.04.365 (2004).
Stranges, S. et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. American Journal of Epidemiology 168, 1353–1364, doi:10.1093/aje/kwn337 (2008).
Knutson, K. L. & Turek, F. W. The U-shaped association between sleep and health: the 2 peaks do not mean the same thing. Sleep 29, 878–879 (2006).
Smagula, S. F., Koh, W. P., Wang, R. & Yuan, J. M. Chronic disease and lifestyle factors associated with change in sleep duration among older adults in the Singapore Chinese Health Study. Journal of Sleep Research 25, 57–61, doi:10.1111/jsr.12342 (2016).
Smagula, S. F., Stone, K. L., Fabio, A. & Cauley, J. A. Risk factors for sleep disturbances in older adults: Evidence from prospective studies. Sleep Medicine Reviews 25, 21–30, doi:10.1016/j.smrv.2015.01.003 (2016).
Chen, H. C., Su, T. P. & Chou, P. A nine-year follow-up study of sleep patterns and mortality in community-dwelling older adults in Taiwan. Sleep 36, 1187–1198, doi:10.5665/sleep.2884 (2013).
Buysse, D. J., Reynolds, C. F. 3rd, Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research 28, 193–213 (1989).
Lan, T. Y., Lan, T. H., Wen, C. P., Lin, Y. H. & Chuang, Y. L. Nighttime sleep, Chinese afternoon nap, and mortality in the elderly. Sleep 30, 1105–1110 (2007).
Goto, A., Yasumura, S., Nishise, Y. & Sakihara, S. Association of health behavior and social role with total mortality among Japanese elders in Okinawa, Japan. Aging Clin Exp Res 15, 443–450 (2003).
Gangwisch, J. E. et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep 31, 1087–1096 (2008).
Gale, C. & Martyn, C. Larks and owls and health, wealth, and wisdom. BMJ 317, 1675–1677 (1998).
Ruigomez, A., Alonso, J. & Anto, J. M. Relationship of health behaviours to five-year mortality in an elderly cohort. Age and Ageing 24, 113–119 (1995).
Branch, L. G. & Jette, A. M. Personal health practices and mortality among the elderly. American Journal of Public Health 74, 1126–1129 (1984).
Hirshkowitz, M. et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health 1, 233–243, doi:10.1016/j.sleh.2015.10.004 (2015).
Lee, W. J., Peng, L. N., Liang, C. K., Chiou, S. T. & Chen, L. K. Long sleep duration, independent of frailty and chronic Inflammation, was associated with higher mortality: A national population-based study. Geriatrics & gerontology international, doi:10.1111/ggi.12899 (2016).
Chien, M. Y., Wang, L. Y. & Chen, H. C. The Relationship of Sleep Duration with Obesity and Sarcopenia in Community-Dwelling Older Adults. Gerontology 61, 399–406, doi:10.1159/000371847 (2015).
Chen, H. C., Hsu, N. W. & Chou, P. The Association between Sleep Duration and Hand Grip Strength in Community-Dwelling Older Adults: The Yilan Study, Taiwan. Sleep, doi:10.1093/sleep/zsx021 (2017).
Chen, H. C., Hsu, N. W. & Chou, P. The Association Between Extreme Sleep Duration and Cardiac Autonomic Control in Community-Dwelling Older Adults: The Yilan Study, Taiwan. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, doi:10.1093/gerona/glx045 (2017).
Margetts, B. M., Thompson, R. L., Elia, M. & Jackson, A. A. Prevalence of risk of undernutrition is associated with poor health status in older people in the UK. European Journal of Clinical Nutrition 57, 69–74, doi:10.1038/sj.ejcn.1601499 (2003).
Wong, M. T. et al. Development and inter-rater reliability of a standardized verbal instruction manual for the Chinese Geriatric Depression Scale-short form. International Journal of Geriatric Psychiatry 17, 459–463 (2002).
Tang, N. K., Fiecas, M., Afolalu, E. F. & Wolke, D. Changes in Sleep Duration, Quality, and Medication Use Are Prospectively Associated With Health and Well-being: Analysis of the UK Household Longitudinal Study. Sleep 40, doi:10.1093/sleep/zsw079 (2017).
Hublin, C., Partinen, M., Koskenvuo, M. & Kaprio, J. Sleep and mortality: a population-based 22-year follow-up study. Sleep 30, 1245–1253 (2007).
Holliday, E. G., Magee, C. A., Kritharides, L., Banks, E. & Attia, J. Short sleep duration is associated with risk of future diabetes but not cardiovascular disease: a prospective study and meta-analysis. Plos One 8, e82305, doi:10.1371/journal.pone.0082305 (2013).
Shan, Z. et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care 38, 529–537, doi:10.2337/dc14-2073 (2015).
Lamond, N., Tiggemann, M. & Dawson, D. Factors predicting sleep disruption in Type II diabetes. Sleep 23, 415–416 (2000).
van Mill, J. G., Vogelzangs, N., van Someren, E. J. W., Hoogendijk, W. J. G. & Penninx, B. W. J. H. Sleep duration, but not insomnia, predicts the 2-year course of depressive and anxiety disorders. Journal of Clinical Psychiatry 75, 119–126, doi:10.4088/JCP.12m08047 (2014).
Babson, K. A., Trainor, C. D., Feldner, M. T. & Blumenthal, H. A test of the effects of acute sleep deprivation on general and specific self-reported anxiety and depressive symptoms: an experimental extension. Journal of Behavior Therapy and Experimental Psychiatry 41, 297–303, doi:10.1016/j.jbtep.2010.02.008 (2010).
Surani, S., Brito, V., Surani, A. & Ghamande, S. Effect of diabetes mellitus on sleep quality. World J Diabetes 6, 868–873, doi:10.4239/wjd.v6.i6.868 (2015).
Palmer, C. D., Harrison, G. A. & Hiorns, R. W. Association between smoking and drinking and sleep duration. Annals of Human Biology 7, 103–107 (1980).
Cohrs, S. et al. Impaired sleep quality and sleep duration in smokers-results from the German Multicenter Study on Nicotine Dependence. Addict Biol 19, 486–496, doi:10.1111/j.1369-1600.2012.00487.x (2014).
Kronholm, E., Harma, M., Hublin, C., Aro, A. R. & Partonen, T. Self-reported sleep duration in Finnish general population. Journal of Sleep Research 15, 276–290, doi:10.1111/j.1365-2869.2006.00543.x (2006).
Patel, S. R., Malhotra, A., Gottlieb, D. J., White, D. P. & Hu, F. B. Correlates of long sleep duration. Sleep 29, 881–889 (2006).
Hartmann, E. Sleep requirement: long sleepers, short sleepers, variable sleepers, and insomniacs. Psychosomatics 14, 95–103, doi:10.1016/S0033-3182(73)71362-1 (1973).
Kronholm, E. et al. Trends in self-reported sleep duration and insomnia-related symptoms in Finland from 1972 to 2005: a comparative review and re-analysis of Finnish population samples. Journal of Sleep Research 17, 54–62 (2008).
da Silva, A. A. et al. Sleep duration and mortality in the elderly: a systematic review with meta-analysis. BMJ Open 6, e008119, doi:10.1136/bmjopen-2015-008119 (2016).
The Directorate-General of Budget, Accounting and Statistics. The Social Development Trends Survey, http://eng.stat.gov.tw/ct.asp?xItem=9378&ctNode=1647&mp=5 (2000).
Zee, P. C. & Turek, F. W. Sleep and health: Everywhere and in both directions. Archives of Internal Medicine 166, 1686–1688, doi:10.1001/archinte.166.16.1686 (2006).
Acknowledgements
The authors thank Prof. Tung-Ping Su for his contribution to the study design and data collection at the baseline evaluation. This study was supported by a grant from National Science Council, Taiwan (NSC 96-2628-B-010-012-MY3) to Prof. Pesus Chou and partially supported by the grants from the Ministry of Science and Technology, Taiwan (MOST 105-2627-E-002-003 and MOST 105-2314-B-002-066) to Dr. Hsi-Chung Chen.
Author information
Authors and Affiliations
Contributions
P.C. designed the research and performed supervision. H.C.C. performed statistical analysis. All authors participated in drafting and revision of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, HC., Chou, P. Predictors of Change in Self-Reported Sleep Duration in Community-Dwelling Older Adults: The Shih-Pai Sleep Study, Taiwan. Sci Rep 7, 4729 (2017). https://doi.org/10.1038/s41598-017-04932-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-04932-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.