Abstract
Mutations in BRCA1 or BRCA2 define a subset of prostate cancer patients. Herein, we address the question whether BRCA1/2 mutations have a predictive impact on chemotherapy with docetaxel, a widely used drug in patients with metastatic castration resistant prostate cancer (mCRPC). Fifty-three men treated with docetaxel for mCRPC were tested for somatic BRCA1/2 mutations of the primary tumor. In a subgroup of patients, BRCA1/2 protein expression was tested as a potential surrogate marker for BRCA1/2 inactivation. Eight of 53 patients (15.1%) harbored a deleterious BRCA2 mutation. No BRCA1 mutation was found. Patients with a BRCA2 mutation showed a response rate of 25% to docetaxel in comparison to 71.1% in men with wildtype BRCA2 (p = 0.019). While the time to develop castration resistance was similar in both subgroups, the overall survival was significantly shorter in patients harboring a BRCA2 mutation. No correlation between the BRCA1/2 protein expression and the response to docetaxel was found. While the presence of a BRCA2 mutation does not preclude a response to docetaxel, there is overall a significant correlation between BRCA2 inactivation and a poor response rate. Our results suggest that a close oncological monitoring of patients with BRCA2 mutations for taxane resistance is warranted.
Similar content being viewed by others
Introduction
Prostate cancer is the most common non-cutaneous cancer and a leading cause of cancer-related mortality in men1. There is compelling evidence that genetic factors strongly contribute to the risk of developing prostate cancer. Prominent examples of such risk factors are mutations in the BRCA1 and BRCA2 DNA repair genes. Men below the age of 65 carrying a germline mutation in BRCA1 or BRCA2 have a 3.4-fold and 8.6-fold, respectively, risk to develop prostate cancer, which make BRCA2 mutations the strongest known genetic risk factor for prostate cancer2,3,4. A number of studies suggest that prostate cancer patients with germline BRCA1 or BRCA2 mutations present at a younger age, have more poorly differentiated tumors and present with a more aggressive clinical course of disease2, 5,6,7. In metastatic castration-resistant prostate cancer (mCRPC), the prevalence of germline mutations in DNA repair genes was 11.8% in a recent study8. Several studies have shown a high rate of somatic BRCA mutations, in particular in BRCA2, in prostate cancer9,10,11,12,13,14,15. The frequency of somatic BRCA2 mutations was found to vary between 3% in localized tumors up to 14% in men with mCRPC9, 10, 14, 15.
BRCA1 and BRCA2 are tumor suppressor genes located on chromosome 17 and chromosome 13, respectively. The BRCA1 and BRCA2 genes are structurally unrelated but both function in DNA double strand break (DSB) repair through homologous recombination (HR)16, 17. In line with this notion, inactivation of BRCA1 or BRCA2 has been found to lead to enhanced mutagenesis and an increase of small indels and copy number alterations (CNAs)18,19,20.
BRCA1 and BRCA2 mutations were first reported in women with hereditary breast and ovarian cancer21 and have been shown to be associated with sensitivity to poly-(adenosine diphosphate [ADP]-ribose) polymerase (PARP) inhibitors such as olaparib22.
A recent phase II trial has shown an overall response rate of 88% in patients with mCRPC harboring deleterious mutations in DNA repair genes and treated with olaparib monotherapy9. While these results hold the promise for the first biomarker-driven targeted therapy in prostate cancer, the vast majority of men with mCRPC will continue to receive a taxane-based chemotherapy at some point of time during the course of disease23. Notably, there are currently no molecular markers available to predict the response to taxanes.
In this retrospective study, we assessed the frequency and predictive significance of somatic BRCA1/2 mutations for docetaxel monotherapy in 53 men with mCRPC. We found somatic BRCA2 mutations in the primary tumor in 15.1% of the patients including one patient with a known germline BRCA2 mutation. The response rate (RR) to docetaxel was 25% in men with a BRCA2 mutation in comparison to 71.1% in men with wildtype BRCA2. While the presence of a BRCA2 mutations did not preclude a response to docetaxel, our results suggest that close oncological monitoring for taxane resistance is warranted in these patients.
Patients and Methods
Patients
In this retrospective study, a total of 53 men were included who were initially diagnosed with locally advanced (≥pT3) or primary metastatic prostate cancer and subsequently were treated with docetaxel for mCRPC at the University of Heidelberg School of Medicine (Table 1). All patients received a prostate biopsy or surgery at the study center between 1998 and 2016. None of these patients had histopathological evidence of neuroendocrine differentiation at the time of diagnosis.
All patients and/or their legal guardian(s) provided written informed consent to the study. All experimental protocols and methods were approved under ethics vota 206/2005, 207/2005 and S-085/2012 of the Ethics Committee of the University of Heidelberg School of Medicine. All experiments were carried out in accordance with the June 1964 Declaration of Helsinki (entitled “Ethical Principles for Medical Research Involving Human Subjects”), as last revised, concluded by the World Medical Association.
A response to docetaxel therapy was defined as a reduction in the PSA level of ≥50% at any timepoint during treatment24. PSA values immediately before docetaxel treatment and PSA value within two weeks after the last cycle were considered to assess the therapy response.
Library preparation and semiconductor sequencing
For library preparation, the multiplex PCR-based Ion Torrent AmpliSeqTM technology (Life Technologies) with an FFPE-optimised modified version of the BRCA1/2 community panel (IonTorrent/Thermo Fisher Scientific, Waltham, USA) covering all exons and splice junctions of these genes was used.
Amplicon library preparation was performed with the Ion AmpliSeq Library Kit v2.0 using approximately 10 ng of DNA for each of the three pools. Briefly, the DNA was mixed with each primer pool and the AmpliSeq HiFi Master Mix and transferred to a PCR cycler (BioRad, Munich, Germany)25. After the end of the PCR reaction, primer end sequences were partially digested using FuPa reagent, followed by the ligation of barcoded sequencing adapters (Ion Xpress Barcode Adapters, Life Technologies). The final library was purified using AMPure XP magnetic beads (Beckman Coulter, Krefeld, Germany) and quantified using qPCR (Ion Library Quantitation Kit, Thermo Fisher Scientific, Waltham, USA) on a StepOne qPCR machine (Thermo Fisher Scientific, Waltham, USA). The individual libraries were diluted to a final concentration of 100 pM and processed to library amplification on Ion Spheres using Ion PGM™ Template OT2 200 Kit. Unenriched libraries were quality-controlled using Ion Sphere quality control measurement on a QuBit instrument. After library enrichment (Ion OneTouch ES), the library was processed for sequencing using the Ion Torrent PGM HiQ sequencing chemistry and the barcoded libraries were loaded onto a chip, generating a mean coverage of 1000–3000 fold per amplicon.
Variant Calling and Annotation
Data analysis was performed using the Ion Torrent Suite Software (version 4.4) as described previously26. After base calling, the reads were aligned against the human genome (hg19) using the TMAP algorithm within the Torrent Suite. Variant calling was performed with the variant caller plugin within the Torrent Suite Software and the IonReporter package using a corresponding bed-file containing the coordinates of the amplified regions. Only variants with an allele frequency >5% and minimum coverage >200 reads were taken into account. Variant annotation was performed using Annovar27. Annotations included information about nucleotide and amino acid changes of RefSeq annotated genes, COSMIC and dbSNP entries as well as detection of possible splice site mutations. For data interpretation and verification, the aligned reads were visualized using the IGV browser (Broad Institute)28.
Immunohistochemistry
Formalin-fixed, paraffin-embedded tissue specimens from a total of sixteen prostate cancers were provided by the tissue bank of the National Center for Tumor Diseases (NCT, Heidelberg, Germany) in accordance with the regulations of the tissue bank and the approval of the ethics committee of the University of Heidelberg School of Medicine. Paraffin sections were deparaffinized in xylene and rehydrated in a graded ethanol series. Antigen retrieval was performed with a steam cooker using retrieval buffer (Target Retrieval Solution, Dako). Primary antibodies were incubated overnight at 4 °C and directed against BRCA1 (clone MS110, Millipore, 1:25), BRCA2 (Sigma, 1:200) and Ki-67 (clone MIB-1, Dako, 1:100). Immunodetection was performed using the Histostain-Plus Detection Kit (3rd Generation, Invitrogen) according to manufacturer’s recommendations. Nuclear counterstaining was provided by hematoxylin (Thermo Scientific).
Tissue specimens were analyzed by two independent observers (C.N. and S.D.). For BRCA1/2 protein expression, five staining categories were defined: negative, weak, partial loss, moderate or strong. Negative, weak and a partial loss of staining were considered as a reduced protein expression and moderate or strong staining as not reduced.
Statistical analysis
Statistical analyses were conducted with the use of SPSS Statistics 17.0 (SPSS Inc, Chicago, IL). Percentage changes in PSA levels related to docetaxel response was represented in a waterfall plot. Associations of BRCA2 mutation status or BRCA1/2 protein expression with treatment response to docetaxel and clinico-pathological parameters were statistically analyzed by Fisher’s Exact Test or the Mann-Whitney U test, as appropriate. A p value of ≤0.05 was considered significant.
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
Results
High prevalence of BRCA2 mutations in patients with high-risk prostate cancer
To investigate the prevalence of BRCA1/2 gene mutations at the time of diagnosis, targeted next generation sequencing (NGS) of tissue specimens obtained through a radical prostatectomy (n = 36), prostate biopsy (n = 13), lymphadenectomy (n = 2) or transurethral resection of the prostate (n = 2) was performed. A deleterious somatic BRCA2 mutation was found in eight of 53 patients (15.1%; Table 1). One patient carried a known germline BRCA2 mutation, which was also detected in the primary tumor and has previously been reported29. We did not detect any somatic BRCA1 mutations in this high-risk prostate cancer patient cohort. There was no significant correlation between BRCA2 mutation status and patient age at diagnosis, ECOG performance status, initial PSA, TNM stage or Gleason score (Suppl. Table 1). The time from diagnosis to castration resistance was 21.9 versus 35.5 months for BRCA2-mutated and wildtype patients (Suppl. Table 1). This difference of over one year could be due to the aggressive behaviour of BRCA2-mutated tumours but also due to the fact that 87.5% of BRCA2-mutated cases presented with metastases at diagnosis compared to 68.9% of patients with wildtype BRCA2 (Suppl. Table 1). We would like to emphasize that we cannot rule out that the lack of statistical significance may be related to the small sample size.
BRCA2 mutation status and the patient response to docetaxel
All 53 patients of our cohort developed castration resistance after ADT and subsequently received docetaxel with a median number of treatment cycles of six in both men who were BRCA2 wildtype (range, 3–12) and in men harboring a BRCA2 mutation (range, 3–8). The overall RR to docetaxel defined as a PSA decline of ≥50% at any time point during treatment was 64.2% (95% CI, 50.7–75.7%; Table 1).
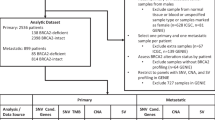
Of eight patients with a BRCA2 mutation, two patients showed a response to docetaxel with an >90% PSA decline (RR = 25%; 95% CI, 7.2–59.1%; Fig. 1). However, six of eight patients (75%) showed either a poor response to docetaxel (<50% PSA decline) or a PSA progression (95% CI, 40.9–92.9%; Fig. 1). In comparison, of 45 men who were wildtype for BRCA2, 32 showed a PSA response (RR = 71.1%; 95% CI, 56.6–82.3%) whereas 13 patients (28.9%; 95% CI, 17.7–43.4%) showed a poor response or PSA progression under therapy (Fig. 1). The correlation between BRCA2 mutation status and PSA response to docetaxel was statistically significant (p = 0.019, Fisher’s Exact test; Fig. 1, Suppl. Table 1).
BRCA2 mutation status and response to docetaxel. Waterfall plot showing the PSA responses (% PSA change) in 53 men with primary metastatic or locally advanced prostate cancer. The dotted line indicates the threshold for defining a PSA response (PSA decline ≥50%). Changes in the protein coding sequence are given for all patients with a BRCA2 mutation. There was a statistically significant correlation between the presence of a BRCA2 mutation and the response to docetaxel (p = 0.019, Fisher’s Exact test). The circumflex denotes a patient who carried a known germline BRCA2 mutations that was also present in the tumor and whose course of disease has previously been reported29. The y axis was cut off at 100%.
To address the question whether prior treatment may have affected the reponse to docetaxel, we first stratified patients into PSA responders and non-responders and analyzed whether there were any significant differences in the treatment received prior to docetaxel. No significant differences in the prior treatment between PSA responders and non-responders was detected (p > 0.05, Fisher“s Exact test: Suppl. Table 2). In addition, we performed a multivariate logistic regression analysis and found that none of the prior treatment modalities had a significant impact on a favorable PSA response. Variables used were radical prostatectomy (odds ratio [OR] 0.6, p = 0.57), any radiotherapy (OR 1.79, p = 0.42), and enzalutamide and/or abiraterone treatment (OR 0.3, p = 0.16). In this multivariate model, the presence of a BRCA1/2 mutation was negatively associated with a PSA response with borderline significance (OR 0.18, p = 0.065).
Of eight BRCA2 mutations detected in our patient cohort, six affected exon 11, which encodes the BRC repeat region, whereas two affected the C-terminal DNA binding domain. The two patients with a favorable response to docetaxel both harbored exon 11 mutations, but there was overall no significant correlation between the localization of mutations and the docetaxel response (p > 0.05). One patient with a known BRCA2 germline mutation showed a PSA progression upon docetaxel treatment (Fig. 1).
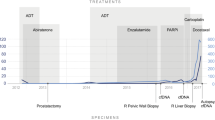
While the time from diagnosis to castration resistance was similar between patients harboring a BRCA2 mutation in comparison to BRCA2 wildtype patients (Fig. 2), there was a significantly reduced overall survival in BRCA2 mutated patients to which the poor response to docetaxel in the majority of patients may have contributed (p = 0.029, log-rank; Fig. 2). However, the small sample size represents a limitation to this conclusion.
BRCA2 mutation status and patient survival. (A,B) Kaplan Meier curves showing time to castration resistance in 45 men who were wildtype for BRCA2 and eight men with a deleterious BRCA2 mutation (A). Overall survival (B) was significantly shorter in six men with a BRCA2 mutation in comparison to 40 men who carried the wildtype gene (p = 0.029; log-rank test). Differences in the patient number in (B) are due to the fact that seven men were lost to follow up.
Taken together, these results show that BRCA2 mutations can be detected in a substantial proportion of high-risk prostate cancer patients and that the presence of a BRCA2 mutation is associated with a poor response to docetaxel in the majority, but not all patients.
No correlation between BRCA1/2 mutation status and BRCA1/2 protein expression
In order to determine a potential role of BRCA1/2 protein expression as surrogate marker for BRCA1/2 inactivation, tumor specimens of a subgroup of 16 patients selected from our cohort were analyzed by immunohistochemistry (Fig. 3).
Heterogeneity in BRCA1/2 protein expression and BRCA1/2 mutational status. Immunohistochemical staining for BRCA1, BRCA2 or Ki-67 in four representative tumors. Note that the two BRCA1/2 wildtype tumors showed either a strong nucleocytoplasmic expression of both BRCA1 and BRCA2 or a weak cytoplasmic expression of both proteins. BRCA2 mutated tumors show a partial loss of BRCA2 protein expression but such a loss was also detectable in BRCA1/2 wildtype tumors (e.g., second row from the bottom). Scale bar = 50 µm.
BRCA1 and BRCA2 protein expression was seen as predominantly nuclear or nucleocytoplasmic staining in line with previous reports30, 31. We found that BRCA2 protein expression was partially lost in some tumors, likely reflecting clonal heterogeneity, a pattern that was not detected for BRCA1.
BRCA1 protein expression was reduced (i.e., negative or weak expression) in five of 16 (31.3%) tumors despite the fact that all tumors were BRCA1 wildtype. A reduction of BRCA2 protein expression (i.e., negative, weak or partial loss of expression) was found in 12 of 16 patients (75%). All five tumor specimens with BRCA2 mutation had a reduced BRCA2 protein expression, however, a reduced BRCA2 protein expression was also detected in tumors harboring wildtype BRCA2 (63.6%). There was no statistically significant correlation between BRCA2 mutation status and BRCA2 protein expression (p > 0.05), nor between BRCA2 mutation status and BRCA1 protein expression (p > 0.05; Fig. 4).
Correlation of BRCA1/2 mutational status or BRCA1/2 protein expression to the PSA response to docetaxel. Waterfall plots for the percentage PSA change after docetaxel treatment stratified into BRCA1/2 mutation status (A), BRCA1 protein expression (B) or BRCA2 protein expression (C). The dotted line indicates the threshold for defining a PSA response (PSA decline ≥50%). The y axis was cut off at 100%.
The median Ki-67 proliferation index across tumors was 12% (range, 3–60%). Two patients with a BRCA2 mutation showed an excessive proliferation with Ki-67 indices over 50%, however, there was overall no statistically significant correlation between BRCA2 mutation status and proliferation index. There was also no statistically significant correlation between BRCA1/2 protein expression and clinico-pathological parameters including Gleason score, PSA level at diagnosis, tumor stage, lymph node metastases, distant metastases or the Ki-67 proliferation index (not shown).
In conclusion, BRCA1/2 protein expression is not a suitable surrogate maker for BRCA1/2 inactivation in prostate cancer.
Discussion
In the present study, we detected BRCA2 mutations in approximately 15% patients with primary metastatic or localized high-risk prostate cancer who subsequently developed castration resistance and were treated with docetaxel. We show that the presence of a BRCA2 mutation in the primary tumor negatively affects the RR to docetaxel, which was 25% in BRCA2-mutated patients and 71.1% in patients who were wildtype for BRCA2. We demonstrate that the heterogeneity of BRCA1/2 protein expression and the lack of concordance with the mutation status precludes the use as a surrogate biomarker for BRCA1/2 inactivation in prostate cancer32.
While the small sample size is a limitation of this study, it underscores the role of BRCA2 not only in the progression prostate cancer but also in the response to one of the current standard therapies.
The key question that arises from our findings is whether a taxane based chemotherapy in prostate cancer patients with a BRCA2 mutation is the optimal treatment considering our finding that the RR in these patients was only 25%. This proportion is considerably lower than in the BRCA2 wildtype group presented here or in previous clinical trials where a PSA RR of 50% was reported33. Nevertheless, we identified two patients with a deleterious somatic BRCA2 mutation who showed an ≥90% PSA decline. These findings underscore that patients with a BRCA2 mutation can have a favorable PSA response and docetaxel resistance may not represent a uniform feature. The exact role of taxane based chemotherapy for the treatment of BRCA1/2 mutated prostate cancer patients has therefore to be further elucidated but our data suggest that patients with known BRCA1/2 mutation should be carefully monitored for PSA response when receiving a taxane based chemotherapy.
A previous study had suggested that BRCA2 germline carrier status and a response to docetaxel treatment are not mutually exclusive34. However, the one patient with a germline BRCA2 mutation in our study showed a poor response to docetaxel. One caveat of the previous study is that one of the responding patients did receive a combination of docetaxel plus carboplatin and had a significantly longer overall survival than the other patients treated with docetaxel monotherapy. It hence remains unclear, which agent actually lead to the favorable response34.
A high response rate to the PARP inhibitor olaparib has been reported in patients with either somatic or germline mutations in BRCA2, ATM or other genes involved in HR repair9. However, some patients may benefit only transiently from such treatment since PARP inhibitor resistance is not uncommon29, 35. BRCA2 inactivation has also been shown to enhance the sensitivity to platinum salts36 and, most recently, high-dose testosterone37. The increased mutational load associated the BRCA1/2 deficiency18,19,20 may also encourage the use of immune checkpoint blockade in these patients. However, all these alternative treatment modalities, as well as combination therapies such as PARP inhibition in combination with platinum compounds, need to be tested in prospective, multicentric clinical trials, which are so far missing. In addition, a better understanding of the molecular basis of taxane resistance in BRCA2 mutated prostate cancer is needed for strategies to re-sensitize patients.
BRCA2 has been shown to play a role in a number of mitotic processes including the spindle assembly checkpoint, cytokinesis and daughter cell abcission38. A functional spindle assembly checkpoint is critical for taxane-induced cell death. It is hence possible that a defective spindle assembly checkpoint associated with BRCA2 inactivation causes an impaired efficacy of docetaxel. In addition, a link between BRCA2 inactivation and multidrug resistance has been reported39. Since docetaxel is a substrate for multidrug resistance transporters such as P-glycoprotein, docetaxel efflux may be enhanced in BRCA2-mutated prostate cancers. However, since not all BRCA2-mutated patients showed an unfavorable response to docetaxel, clonal heterogeneity of the somatic mutation need to be taken into consideration12.
There are certain similarities as well as dissimilarities between BRCA2-mutated prostate cancer and other tumor entities in which HR defects occur at a sizable proportion such as triple negative breast cancer (TNBC). In TNBCs, docetaxel appears to be less effective than carboplatin in women carrying a BRCA1/2 mutation similar to our findings40. TNBCs do not respond to antihormonal treatment. However, in the cohort presented herein, the time to castration resistance was not significantly different between wildtype and patients with a BRCA2 mutation suggesting that androgen deprivation therapy is not ineffective in the latter subgroup. Whether the RR to next-generation anti-androgens such a abiraterone or enzalutamide differs in BRCA2-mutated men in comparison to patients without such a mutation remains to be determined.
Collectively, our results underscore that a substantial proportion of primary metastatic or locally advanced prostate cancer patients who subsequently develop mCRPC harbor a deleterious BRCA2 mutation. We provide evidence that the majority, but not all, of these patients respond poorly to docetaxel. Clearly, larger studies conducted in a prospective manner are warranted. Given the current lack of these trials, we believe that it would be premature to omit taxanes from the therapeutic armamentarium to treat BRCA2-mutated prostate cancer patients. However, close oncological monitoring for docetaxel resistance appears to be necessary.
References
Siegel, R., Naishadham, D. & Jemal, A. Cancer statistics, 2013. CA Cancer J Clin 63, 11–30 (2013).
Castro, E. et al. Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer. J. Clin. Oncol. 31, 1748–1757 (2013).
Leongamornlert, D. et al. Germline BRCA1 mutations increase prostate cancer risk. Br. J. Cancer 106, 1697–1701 (2012).
Levy-Lahad, E. & Friedman, E. Cancer risks among BRCA1 and BRCA2 mutation carriers. Br. J. Cancer 96, 11–15 (2007).
Edwards, S. M. et al. Prostate cancer in BRCA2 germline mutation carriers is associated with poorer prognosis. Br. J. Cancer 103, 918–924 (2010).
Gallagher, D. J. et al. Germline BRCA mutations denote a clinicopathologic subset of prostate cancer. Clin. Cancer Res. 16, 2115–2121 (2010).
Mitra, A. et al. Prostate cancer in male BRCA1 and BRCA2 mutation carriers has a more aggressive phenotype. Br. J. Cancer 98, 502–507 (2008).
Pritchard, C. C. et al. Inherited DNA-Repair Gene Mutations in Men with Metastatic Prostate Cancer. N. Engl. J. Med. 375, 443–453 (2016).
Mateo, J. et al. DNA-Repair Defects and Olaparib in Metastatic Prostate Cancer. N. Engl. J. Med. 373, 1697–1708 (2015).
Robinson, D. et al. Integrative clinical genomics of advanced prostate cancer. Cell 161, 1215–1228 (2015).
Gundem, G. et al. The evolutionary history of lethal metastatic prostate cancer. Nature 520, 353–357 (2015).
Boutros, P. C. et al. Spatial genomic heterogeneity within localized, multifocal prostate cancer. Nat. Genet. 47, 736–745 (2015).
Hong, M. K. H. et al. Tracking the origins and drivers of subclonal metastatic expansion in prostate cancer. Nat Commun 6, 6605 (2015).
Cancer Genome Atlas Research Network The Molecular Taxonomy of Primary Prostate Cancer. Cell 163, 1011–1025 (2015).
Beltran, H. et al. Targeted next-generation sequencing of advanced prostate cancer identifies potential therapeutic targets and disease heterogeneity. Eur. Urol. 63, 920–926 (2013).
Moynahan, M. E., Pierce, A. J. & Jasin, M. BRCA2 is required for homology-directed repair of chromosomal breaks. Mol. Cell 7, 263–272 (2001).
O’Donovan, P. J. & Livingston, D. M. BRCA1 and BRCA2: breast/ovarian cancer susceptibility gene products and participants in DNA double-strand break repair. Carcinogenesis 31, 961–967 (2010).
Decker, B. et al. Biallelic BRCA2 Mutations Shape the Somatic Mutational Landscape of Aggressive Prostate Tumors. Am. J. Hum. Genet. 98, 818–829 (2016).
Castro, E. et al. High burden of copy number alterations and c-MYC amplification in prostate cancer from BRCA2 germline mutation carriers. Ann. Oncol. 26, 2293–2300 (2015).
Zámborszky, J. et al. Loss of BRCA1 or BRCA2 markedly increases the rate of base substitution mutagenesis and has distinct effects on genomic deletions. Oncogene, doi:10.1038/onc.2016.243 (2016).
Stratton, M. R. & Rahman, N. The emerging landscape of breast cancer susceptibility. Nat. Genet. 40, 17–22 (2008).
Lord, C. J. & Ashworth, A. BRCAness revisited. Nat. Rev. Cancer 16, 110–120 (2016).
Tannock, I. F. et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N. Engl. J. Med. 351, 1502–1512 (2004).
Bubley, G. J. et al. Eligibility and response guidelines for phase II clinical trials in androgen-independent prostate cancer: recommendations from the Prostate-Specific Antigen Working Group. J. Clin. Oncol. 17, 3461–3467 (1999).
Endris, V. et al. Molecular diagnostic profiling of lung cancer specimens with a semiconductor-based massive parallel sequencing approach: feasibility, costs, and performance compared with conventional sequencing. J Mol Diagn 15, 765–775 (2013).
Jesinghaus, M. et al. Genotyping of colorectal cancer for cancer precision medicine: Results from the IPH Center for Molecular Pathology. Genes Chromosomes Cancer 55, 505–521 (2016).
Wang, K., Li, M. & Hakonarson, H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 38, e164 (2010).
Robinson, J. T. et al. Integrative genomics viewer. Nat. Biotechnol. 29, 24–26 (2011).
Nientiedt, C. et al. PARP inhibition in BRCA2-mutated prostate cancer. Ann. Oncol., doi:10.1093/annonc/mdw445 (2016).
Fiorentino, M. et al. Immunohistochemical expression of BRCA1 and lethal prostate cancer. Cancer Res. 70, 3136–3139 (2010).
Thorgeirsson, T. et al. Intracellular location of BRCA2 protein expression and prostate cancer progression in the Swedish Watchful Waiting Cohort. Carcinogenesis 37, 262–268 (2016).
Edwards, S. M. et al. Immunohistochemical expression of BRCA2 protein and allelic loss at the BRCA2 locus in prostate cancer. CRC/BPG UK Familial Prostate Cancer Study Collaborators. Int. J. Cancer 78, 1–7 (1998).
Petrylak, D. P. et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N. Engl. J. Med. 351, 1513–1520 (2004).
Gallagher, D. J. et al. Germline BRCA mutation does not prevent response to taxane-based therapy for the treatment of castration-resistant prostate cancer. BJU Int 109, 713–719 (2012).
Barber, L. J. et al. Secondary mutations in BRCA2 associated with clinical resistance to a PARP inhibitor. J. Pathol. 229, 422–429 (2013).
Cheng, H. H., Pritchard, C. C., Boyd, T., Nelson, P. S. & Montgomery, B. Biallelic Inactivation of BRCA2 in Platinum-sensitive Metastatic Castration-resistant Prostate Cancer. Eur. Urol. 69, 992–995 (2016).
Teply, B. A., Kachhap, S., Eisenberger, M. A. & Denmeade, S. R. Extreme Response to High-dose Testosterone in BRCA2- and ATM-mutated Prostate Cancer. Eur. Urol., doi:10.1016/j.eururo.2016.09.020 (2016).
Venkitaraman, A. R. Tumour suppressor mechanisms in the control of chromosome stability: insights from BRCA2. Mol. Cells 37, 95–99 (2014).
Jaspers, J. E. et al. BRCA2-deficient sarcomatoid mammary tumors exhibit multidrug resistance. Cancer Res. 75, 732–741 (2015).
Mustacchi, G. & De Laurentiis, M. The role of taxanes in triple-negative breast cancer: literature review. Drug Des Devel Ther 9, 4303–4318 (2015).
Acknowledgements
This work was supported by the Medical Faculty Heidelberg. We are grateful to Constanze Rapp and Christine Geisler for patient data management and Tanja Proctor for statistical support. We would like to thank the tissue bank of the National Center for Tumor Diseases Heidelberg for the procurement of tissue samples.
Author information
Authors and Affiliations
Contributions
C.N., A.S., M.Ho., C.G., and S.D. conceived, supervised and coordinated the study. C.N. and S.D. wrote the manuscript. M.He. and M.A.T.-L. performed immunohistochemical stainings and scored and interpreted the results. V.E., A.L.V., P.S., and A.S. performed, supervised and interpreted panel next generation sequencing. A.D. and H.S. gave helpful advice to data interpretation. C.N., S.Z., D.J. and C.G. contributed to patient identification, treatment and management.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nientiedt, C., Heller, M., Endris, V. et al. Mutations in BRCA2 and taxane resistance in prostate cancer. Sci Rep 7, 4574 (2017). https://doi.org/10.1038/s41598-017-04897-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-04897-x
This article is cited by
-
Therapeutic sensitivity to standard treatments in BRCA positive metastatic castration-resistant prostate cancer patients—a systematic review and meta-analysis
Prostate Cancer and Prostatic Diseases (2023)
-
Molekulare zielgerichtete Therapie und Immuntherapie des Prostatakarzinoms
Der Urologe (2020)
-
Olaparib beim metastasierten Prostatakarzinom – die PROfound-Studie
Der Urologe (2020)
-
Notwendigkeit neuer Begrifflichkeiten
Uro-News (2020)
-
The BRCA2 mutation status shapes the immune phenotype of prostate cancer
Cancer Immunology, Immunotherapy (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.