Abstract
The vitamin D levels in mothers affect the health status of both the mother and breastfeeding infant. Vitamin D deficient mothers’ infants are prone to rickets. While tumor necrosis factor-related apoptosis inducing ligand (TRAIL) has been implicated in cellular growth/apoptosis, immune cell function and bone-resorbing osteoclast formation, the expression of TRAIL in human milk as a function of vitamin D status in mothers remains unknown. We hypothesized that vitamin D deficiency alters TRAIL protein levels in human breast milk and mammary epithelial cells. Milk from vitamin D deficient mothers showed high levels of TRAIL (α and β) proteins compared to milk from vitamin D replete women. Western blot analysis of total cell lysate obtained from normal human mammary epithelial (HME-1) cells treated with variable doses (0–20 nM) of vitamin D for 24 h demonstrated that low levels (0.5 to 5 nM) significantly increased the TRAIL α but no change in β expression. In contrast, vitamin D at 20 nM concentration suppressed the expression of both TRAIL α and β proteins. Consistently, vitamin D regulated TRAIL mRNA expression in HME-1 cells. Our results indicate that vitamin D status in mothers modulates TRAIL expression in breast milk, which may have implications for both mother and infant health.
Similar content being viewed by others
Introduction
Vitamin D deficiency has been shown to play an important role in bone health and autoimmune diseases and adversely affects pregnancy and birth outcomes1, 2. It has been shown that vitamin D regulates calcium uptake, bone homeostasis, mammalian cell growth and division. In addition, vitamin D is implicated in the regulation of T-lymphocytes, monocytes and macrophages of the immune system3,4,5. Various factors such as less sunlight exposure due to indoor activity during the day or use of sunscreen, darker skin pigmentation, and health conditions such as pregnancy and obesity result in vitamin D deficiency in people6. Vitamin D deficiency during pregnancy has been shown to be associated with adverse health consequences such as osteomalacia, gestational diabetes, low phosphate levels and elevated levels of PTH in mothers as well as impaired bone development in children7, 8. The mammary epithelial cells' differentiation is critical to forming a functional mammary gland for infant breastfeeding9, 10. It has been reported that vitamin D is involved in mammary gland development and lactation11. Studies have suggested that the vitamin D status of mother determines the vitamin D levels of breastfeeding infant12,13,14. Evidently, randomized controlled clinical trials indicated the beneficial role of maternal vitamin D supplementation on the vitamin D status of breastfed infants14, 15. Therefore, vitamin D deficient mothers are more likely to have infants with vitamin D deficiency which affects immune and bone health16. It has been reported that infants of vitamin D deficient mothers are prone to develop rickets17. However, it is unknown whether vitamin D deficiency in lactating mothers modulates the expression of cellular factor(s) in human milk that is associated with immune health and skeletal development in breastfeeding infants.
Tumor necrosis factor (TNF)-related apoptosis inducing ligand (TRAIL) is a member of the TNF superfamily18. TRAIL is detectable as a soluble protein in biological fluids19. TRAIL isoforms (α, β and ɣ) have been identified and implicated in cellular growth/differentiation20. Also, TRAIL induces apoptosis in malignant cells and at low doses could promote proliferation of normal cells20. TRAIL functions through death receptors DR4, DR5 which promote apoptosis and also binds to DcR1, DcR2 receptors that lack a death domain21. Similar to vitamin D, TRAIL has been shown to regulate immune cell functions, bone remodeling and cell growth/differentiation20, 22. However, the association between the levels of vitamin D in the maternal blood and TRAIL expression in human milk has not been previously described. Therefore, we hypothesize that vitamin D deficiency in mothers alters TRAIL expression in breast milk. In this study, we identified that milk samples collected from vitamin D deficient mothers contain elevated levels of TRAIL compared to the vitamin D replete group. Furthermore, our experiments revealed that vitamin D levels differentially regulates TRAIL isoform expression in mammary epithelial cells in vitro.
Results
Vitamin D deficiency in mothers increases TRAIL expression in breast milk
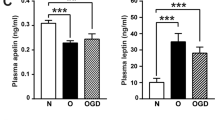
Physiologic levels of vitamin D has been implicated as an important stimulant for innate immunity and bone remodeling. TRAIL expression has been shown to be upregulated in monocytes and macrophages in response to immune cytokines such as interferon-β (IFN-β)23, 24. Vitamin D and TRAIL have been associated with modulation of immune function and bone health. However, their relationship to one another during lactation has not been described. Therefore, serum samples from fifteen breastfeeding mothers aged 20–38 years that included seven Caucasian, seven African-American, and one Hispanic mother were analyzed. Serum 25(OH)D levels were measured to evaluate the active form of vitamin D [1,25(OH)2D] status in maternal blood as classified by the Endocrine Society clinical practice guideline25. Measurement of total circulating 25(OH)D concentrations identified seven samples with normal range (>30 ng/ml) and therefore considered vitamin D-sufficient group. There were eight mother’s serum samples which demonstrated low levels of 25(OH)D (<20 ng/ml) and were considered as a vitamin D deficient group (Fig. 1). Milk samples from 15 of the mothers (8 deficient and 7 sufficient) were analyzed for TRAIL expression by western blot. As shown in Fig. 2a–c, we identified TRAIL α expression in all the milk samples obtained from vitamin D sufficient mother group. However, TRAIL β expression is at very low levels in all the samples analyzed. Interestingly, milk from vitamin D deficient mothers showed elevated levels of TRAIL proteins (α and β) compared to milk from mothers with sufficient vitamin D levels. However, TRAIL ɣ protein is not detectable in human breast milk and mammary epithelial cells (data not shown). These results suggest that vitamin D status in mothers modulate TRAIL expression levels in human breast milk.
Serum 25(OH)D concentrations in mother groups. Serum samples collected from fifteen nursing mothers’ were measured for 25(OH)D levels to evaluate vitamin D status in mother groups as described in methods. Sufficiency: >30 ng/mL; Deficiency: <20 ng/mL. Each bar represents the mean ± SD (P < 0.05). *compared to control sufficient group.
TRAIL expression in human breast milk. Milk samples from vitamin D sufficient and deficient mother groups containing an equal amount of protein (50 µg) were subjected to western blot analysis for TRAIL expression using a specific anti-TRAIL antibody. Ponceau staining of the membrane was performed as a loading control (a and b). The band intensity was quantified by NIH ImageJ. The relative band intensity was normalized by band detected by Ponceau staining (c). *TRAIL α compared to sufficient group; #TRAIL β compared to sufficient group. The values are expressed as mean ± SD (*p < 0.05). S- sufficient; D- deficient. *compared to 0 nM of 1,25(OH)2D treatment. (full-length blots are included in the Supplementary Information Figs 1 and 2).
Effect of vitamin D on TRAIL expression in human breast epithelial cells
Since the expression of TRAIL is elevated in vitamin D deficient mothers’ breast milk, we next examined the direct effect of vitamin D on normal human breast epithelial cells to analyze the TRAIL expression. Although 25(OH)D is the main circulating metabolite, 1,25(OH)2D is the active form which responsible for most of the biological actions26. Therefore, HME-1 cells were treated with 1,25(OH)2D at variable concentrations (0–20 nM) as used previously27 for 24 h. Western blot analysis of total cell lysate obtained from these cells treated with low doses (0–5 nM) demonstrated increased TRAIL α (6-fold) expression. However, the levels of β expression did not alter. In contrast, 1,25(OH)2D at 10–20 nM concentrations dose-dependently suppressed both the TRAIL α and β protein expression (Fig. 3a,b). We further tested the TRAIL mRNA expression in breast epithelial cells following treatment with 1,25(OH)2D at selected doses (0, 0.5 and 20 nM) for 24 h. Real-time RT-PCR analysis of total RNA isolated from the cells showed a 9-fold increase at 5 nM concentration of 1,25(OH)2D compared to untreated control cells. Conversely, 1,25(OH)2D at high dose (20 nM) inhibited TRAIL mRNA expression (Fig. 4). These results indicate that the active form of vitamin D regulates TRAIL expression in normal human breast epithelial cells.
Western blot analysis for vitamin D [1,25(OH)2D] regulation of TRAIL isoforms expression in normal human breast epithelial cells. HME1 cells were treated with different concentrations of 1,25(OH)2D at 0–20 nM for 24 h. (a and b) Total cell lysates were subjected to western blot for TRAIL expression using a specific anti-TRAIL antibody. The band intensity was quantified by NIH ImageJ program. β-actin expression served as a control. The values are expressed as mean ± SD (*p < 0.05). (Full-length blot is included in the Supplementary Information Fig. 3).
Vitamin D regulation of TRAIL mRNA expression in normal human breast epithelial cells. HME-1 cells were treated with vitamin D [1,25(OH)2D] at 0, 5 and 20 nM for 24 h. Total RNA isolated from these cells was subjected to real-time RT-PCR analysis for TRAIL mRNA expression as described. The relative mRNA expression was normalized on GAPDH amplification. The values are expressed as mean ± SD (*p < 0.05). *compared to 0 nM of 1,25(OH)2D treatment.
Discussion
This study demonstrated that breast milk from vitamin D deficient mothers contains high levels of TRAIL (α and β) proteins compared to sufficient mother group. Further, we identified that low doses of the active form of vitamin D (0.5 to 5 nM) treatment to HME-1 cells increased the TRAIL α but no change in β expression. However, 1,25(OH)2D at high doses (20 nM) suppressed the expression of both TRAIL α and β proteins. Therefore, our results indicate that TRAIL is expressed in breast milk as a function of vitamin D status in mothers. Vitamin D is involved in immune cell function and activation28. Vitamin D supplementation of mothers results in vitamin D sufficiency in breast-fed infants13, thus potentially modulating the immune signature of maternal breast milk to her recipient infant. It has been reported that human soluble TRAIL is an immune regulator present in human milk and supports the infant immune system29. Thus, our findings that vitamin D is associated with altered TRAIL expression in breast milk may be an important link to the mother and infant immune system. Evidence suggests that vitamin D deficiency could be carcinogenic to the brains of offspring in mouse model30. TRAIL present in human milk has been shown to play a role in anti-cancer activity31. Since there is no TRAIL toxicity demonstrated in vitro and in vivo treatment32, 33, it is possible that TRAIL expression in the milk of mothers with vitamin D deficiency could be a compensatory mechanism to protect infant health. The functional role of vitamin D in fetus and infant’s bone development has been previously demonstrated. Vitamin D influences the acquisition of bone mineralization in the rapidly growing fetal skeleton34. Mother-offspring group studies have shown that maternal vitamin D insufficiency leads to reduced bone mass during childhood35, 36. We recently demonstrated that TRAIL enhances bone-resorbing osteoclast differentiation37, 38. Therefore, elevated levels of TRAIL expression due to vitamin D deficiency may have a significant impact on both mother and infant bone growth/development.
Vitamin D at sufficient levels has been implicated in the protection of the immune system28. TRAIL has been shown to be upregulated by lipopolysaccharide (LPS) and IFN-β produced by immune cells39. Therefore, it is possible that mammary cells, as well as immune cells, can contribute to TRAIL expression in human breast milk. Previously, it has been shown that vitamin D deficiency during pregnancy increases genotoxic risks in newborns40. Vitamin D deficiency during pregnancy may also be associated with smaller fetal thymus and systemic inflammatory response41. Similarly, it has been shown that early exposure to TRAIL causes a loss of thymic cellularity and neutralizes all acute inflammatory responses in mice42, 43. This evidence suggests that vitamin D and TRAIL expression in mammalian cells play a major role in both mother and infant immune health. Therefore, specific modulators of the TRAIL signaling axis and vitamin D analogs may lead to the development of randomized clinical trials to rescue from the consequences of vitamin D deficiency in both mother and infant. Also, these studies may have implications regarding vitamin D supplemention during lactation. However, this study should be performed in lactating women with diverse ethnic groups in a large population.
TRAIL has been shown to increase normal mammalian cell growth and induce apoptosis in cancer cells. In contrast, 25(OH)D inhibits the growth of the human mammary epithelial cells44. Therefore, it is possible that elevated levels of TRAIL influence vitamin D metabolism in mammary epithelial cells45. High dose vitamin D decreased TRAIL expression compared to basal levels, suggesting that low levels of vitamin D may be required to stimulate TRAIL expression in mammary epithelial cells. It is likely that the down-regulation of the TRAIL-α and β in response to high doses (>20 nM) of vitamin D could be a compensatory mechanism to protect the mammary cells. Thus, our results suggest that the vitamin D modulation of TRAIL expression in mammary epithelial cells may contribute to TRAIL protein levels in human milk, which may have implications for both mother and infant health under vitamin D deficient and sufficient conditions.
Methods
Serum and breast milk sample collection
All the experimental protocols were approved by IRB (HR#10727) at the Medical University of South Carolina and all methods were performed in accordance with the relevant guidelines and regulations. The collection of breast milk and serum samples from women participating in an NICHD-sponsored study of vitamin D supplementation during lactation was carried out by the approved guidelines. All subjects were taking a prenatal vitamin with 400 IU of vitamin D. Blood samples were collected by venipuncture at the time of the study visit; then placed in a serum separator tube, centrifuged, and serum stored at −20 °C until later analysis. Milk samples were collected using an electric breast pump. Human milk was collected from the left breast directly into a small sampling bottle at the regular feeding time in the morning, 2 h after the previous breastfeed for consistency of results. The samples were stored in a −20 °C freezer for subsequent analysis.
Quantification of circulating 25(OH)D
Concentrations of circulating 25(OH)D were quantified by chemiluminescent immunoassay (DiaSorin Co., Ltd., Stillwater, MN) as described46, 47. Total circulating serum 25(OH)D concentration was measured in duplicate within the month the blood sample was obtained. Vitamin D sufficiency was defined as a total circulating 25(OH)D concentration of >30 ng/mL and deficiency as <20 ng/mL as per the Endocrine Society clinical practice guidelines25.
Normal human breast epithelial cell culture
Normal human breast epithelial (HME-1) cells were maintained in Clonetics® MEBM® Mammary epithelial basal medium (MEBM) supplemented with bovine pituitary extract, GA-1000, human epidermal growth factor, insulin, and hydrocortisone (Lonza, Walkersville, MD). Cells were cultured in a humidified chamber with 5% CO2 and 95% air at 37 °C.
Western blot analysis
Total protein content of the milk samples from vitamin D sufficient and deficient women and HME-1 cells stimulated with 0–20 nM of vitamin D [1,25(OH)2D]48, 49 was measured using the Bradford protein assay method (Bio-Rad, Hercules, CA). Protein (50 μg) samples were then subjected to SDS-PAGE using 4–12% Tris–HCl gels and blot transferred onto a nitrocellulose membrane. Blocking was performed with 3% bovine serum albumin in TBS-T (50 mM Tris, pH 7.2, 150 mM NaCl; 0.1% Tween 20) for 1 h followed by incubation with anti-TRAIL (Abcam Inc., Cambridge, MA) overnight at 4 °C. The blots were then incubated for 1 h with HRP-conjugated secondary antibody and developed using ECL system. The analysis of β-actin expression levels and Ponceau staining of the membrane was performed as a loading control. The band intensities were quantified by NIH ImageJ program.
Real-time RT-PCR
Total RNA was isolated from HME-1 cells treated with different concentrations (0, 5 and 20 nM) of 1,25(OH)2D for 24 h using RNAzol reagent (Molecular Research Center, Inc. Cincinnati, OH). The reverse transcription reaction was performed using poly-dT primer and moloney murine leukemia virus reverse transcriptase (Applied Biosystems, Foster City, CA) in a 25 μl reaction volume containing total RNA (2 μg), 1× PCR buffer and 2 mM MgCl2, at 42 °C for 15 min followed by 95 °C for 5 min. The quantitative real-time RT-PCR was performed using IQ™ SYBR Green Supermix in an iCycler (iCycler iQ Single-color real-time-PCR detection system; Bio-Rad, Hercules, CA). The primer sequences used to amplify human glyceraldehyde-3-phosphate dehydrogenase (hGAPDH) mRNA were sense 5′-CCT ACC CCC AAT GTA TCC GTT GTG-3 and anti-sense 5′-GGA GGA ATG GGA GTT GCT GTT GAA-3′; TRAIL mRNA primer sequences were sense 5′-TTC ACA GTG CTC CTG CAG TC-3′ and antisense 5′-CAG CAG GGG CTG TTC ATA CT-3′. Thermal cycling parameters were 94 °C for 4 min, followed by 35 cycles of amplifications at 94 °C for 30 s, 58 °C for 1 min, 72 °C for 2 min, and 72 °C for 10 min as the final elongation step. Relative levels of mRNA expression were normalized in all the samples analyzed on the levels of GAPDH amplification.
Statistical analysis
Results are represented as mean ± SD of at least three independent experiments. Differences between experimental groups were analyzed by one-way ANOVA and Tukey test using GraphPad Prism software (GraphPad Software, Inc, La Jolla, CA). Values were considered significantly different at p < 0.05.
References
Pludowski, P. et al. Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and mortality-a review of recent evidence. Autoimmun Rev 12, 976–989 (2013).
Wagner, C. L. et al. Post-hoc analysis of vitamin D status and reduced risk of preterm birth in two vitamin D pregnancy cohorts compared with South Carolina March of Dimes 2009–2011 rates. J Steroid Biochem Mol Biol 155, 245–251 (2016).
Grant, W. B. & Holick, M. F. Benefits and requirements of vitamin D for optimal health: a review. Altern Med Rev 10, 94–111 (2005).
Veldman, C. M., Cantorna, M. T. & DeLuca, H. F. Expression of 1,25-dihydroxyvitamin D(3) receptor in the immune system. Arch Biochem Biophys 374, 334–338 (2000).
Cantorna, M. T., Snyder, L., Lin, Y. D. & Yang, L. Vitamin D and 1,25(OH)2D regulation of T cells. Nutrients 7, 3011–3021 (2015).
Spiro, A. & Buttriss, J. L. Vitamin D: An overview of vitamin D status and intake in Europe. Nutr Bull 39, 322–350 (2014).
Dawodu, A. & Akinbi, H. Vitamin D nutrition in pregnancy: current opinion. Int J Womens Health 5, 333–343 (2013).
Vandevijvere, S., Amsalkhir, S., Van Oyen, H. & Moreno-Reyes, R. High prevalence of vitamin D deficiency in pregnant women: a national cross-sectional survey. PLoS One 7, e43868 (2012).
Kim, N. S. et al. Survival and differentiation of mammary epithelial cells in mammary gland development require nuclear retention of Id2 due to RANK signaling. Mol Cell Biol 31, 4775–4788 (2011).
Dawodu, A. & Tsang, R. C. Maternal vitamin D status: effect on milk vitamin D content and vitamin D status of breastfeeding infants. Adv Nutr 3, 353–361 (2012).
Zinser, G. M. & Welsh, J. Accelerated mammary gland development during pregnancy and delayed postlactational involution in vitamin D3 receptor null mice. Mol Endocrinol 18, 2208–2223 (2004).
Le Boulch, N., Cancela, L. & Miravet, L. Calcidiol in human milk. The effect of prohormone on vitamin D status of breast fed unsupplemented infants. Endocrinol Exp 20, 325–328 (1986).
Hollis, B. W. et al. Maternal Versus Infant Vitamin D Supplementation During Lactation: A Randomized Controlled Trial. Pediatrics 136, 625–634 (2015).
Hollis, B. W. & Wagner, C. L. Vitamin D requirements during lactation: high-dose maternal supplementation as therapy to prevent hypovitaminosis D for both the mother and the nursing infant. Am J Clin Nutr 80, 1752S–1758S (2004).
Oberhelman, S. S. et al. Maternal Vitamin D Supplementation to Improve the Vitamin D Status of Breast-fed Infants: A Randomized Controlled Trial. Mayo Clin Proc 88, 1378–1387 (2013).
Holick, M. F. Vitamin D deficiency in 2010: health benefits of vitamin D and sunlight: a D-bate. Nat Rev Endocrinol 7, 73–75 (2011).
Winzenberg, T. & Jones, G. Vitamin D and bone health in childhood and adolescence. Calcif Tissue Int 92, 140–150 (2013).
Almasan, A. & Ashkenazi, A. Apo2L/TRAIL: apoptosis signaling, biology, and potential for cancer therapy. Cytokine Growth Factor Rev 14, 337–348 (2003).
Secchiero, P. et al. Decreased levels of soluble TNF-related apoptosis-inducing ligand (TRAIL) in the conjunctival sac fluid of patients with diabetes affected by proliferative retinopathy. Diabet Med 28, 1277–1278 (2011).
Krieg, A. et al. TRAIL-beta and TRAIL-gamma: two novel splice variants of the human TNF-related apoptosis-inducing ligand (TRAIL) without apoptotic potential. Br J Cancer 88, 918–927 (2003).
Labovsky, V., Vallone, V. B., Martinez, L. M., Otaegui, J. & Chasseing, N. A. Expression of osteoprotegerin, receptor activator of nuclear factor kappa-B ligand, tumor necrosis factor-related apoptosis-inducing ligand, stromal cell-derived factor-1 and their receptors in epithelial metastatic breast cancer cell lines. Cancer Cell Int 12, 29 (2012).
Falschlehner, C., Schaefer, U. & Walczak, H. Following TRAIL’s path in the immune system. Immunology 127, 145–154 (2009).
Liu, W. C. et al. Vitamin D and immune function in chronic kidney disease. Clin Chim Acta 450, 135–144 (2015).
Ehrlich, S., Infante-Duarte, C., Seeger, B. & Zipp, F. Regulation of soluble and surface-bound TRAIL in human T cells, B cells, and monocytes. Cytokine 24, 244–253 (2003).
Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96, 1911–1930 (2011).
Lips, P. Relative value of 25(OH)D and 1,25(OH)2D measurements. J Bone Miner Res 22, 1668–1671 (2007).
Kemmis, C. M. & Welsh, J. Mammary epithelial cell transformation is associated with deregulation of the vitamin D pathway. J Cell Biochem 105, 980–988 (2008).
Prietl, B., Treiber, G., Pieber, T. R. & Amrein, K. Vitamin D and immune function. Nutrients 5, 2502–2521 (2013).
Zauli, G. et al. Levels of TNF-related apoptosis-inducing ligand (TRAIL) show a long-term stability in the breast milk of mothers of preterm infants. J Hum Lact 29, 350–353 (2013).
Bhatti, P., Doody, D. R., McKean-Cowdin, R. & Mueller, B. A. Neonatal vitamin D and childhood brain tumor risk. Int J Cancer 136, 2481–2485 (2015).
Davanzo, R. et al. Human colostrum and breast milk contain high levels of TNF-related apoptosis-inducing ligand (TRAIL). J Hum Lact 29, 23–25 (2013).
Lemke, J., von Karstedt, S., Zinngrebe, J. & Walczak, H. Getting TRAIL back on track for cancer therapy. Cell Death Differ 21, 1350–1364 (2014).
Wang, H., Davis, J. S. & Wu, X. Immunoglobulin Fc domain fusion to TRAIL significantly prolongs its plasma half-life and enhances its antitumor activity. Mol Cancer Ther 13, 643–650 (2014).
Specker, B. Vitamin D requirements during pregnancy. Am J Clin Nutr 80, 1740S–1747S (2004).
Javaid, M. K. et al. Maternal vitamin D status during pregnancy and childhood bone mass at age 9 years: a longitudinal study. Lancet 367, 36–43 (2006).
Harvey, N. C. et al. Paternal skeletal size predicts intrauterine bone mineral accrual. J Clin Endocrinol Metab 93, 1676–1681 (2008).
Sundaram, K. et al. STAT-6 mediates TRAIL induced RANK ligand expression in stromal/preosteoblast cells. Bone 71, 137–144 (2015).
Sambandam, Y. et al. Microgravity Induction of TRAIL Expression in Preosteoclast Cells Enhances Osteoclast Differentiation. Sci Rep 6, 25143 (2016).
Allen, J. E. & El-Deiry, W. S. Regulation of the human TRAIL gene. Cancer Biol Ther 13, 1143–1151 (2012).
O’Callaghan-Gordo, C. et al. Vitamin D insufficient levels during pregnancy and micronuclei frequency in peripheral blood T lymphocytes mothers and newborns (Rhea cohort, Crete). Clin Nutr (2016).
Gur, E. B. et al. Vitamin D deficiency in pregnancy may affect fetal thymus development. Ginekol Pol 87, 378–383 (2016).
Na, I. K. et al. The cytolytic molecules Fas ligand and TRAIL are required for murine thymic graft-versus-host disease. J Clin Invest 120, 343–356 (2010).
Marcuzzi, A., Secchiero, P., Crovella, S. & Zauli, G. TRAIL administration down-modulated the acute systemic inflammatory response induced in a mouse model by muramyldipeptide or lipopolysaccharide. Cytokine 60, 43–46 (2012).
Kemmis, C. M., Salvador, S. M., Smith, K. M. & Welsh, J. Human mammary epithelial cells express CYP27B1 and are growth inhibited by 25-hydroxyvitamin D-3, the major circulating form of vitamin D-3. J Nutr 136, 887–892 (2006).
Jones, G., Prosser, D. E. & Kaufmann, M. Cytochrome P450-mediated metabolism of vitamin D. J Lipid Res 55, 13–31 (2014).
Yi, H. J. et al. Evaluation of vitamin D level in patients from neurosurgical intensive care unit. Neural Regen Res 8, 1528–1534 (2013).
Snellman, G. et al. Determining vitamin D status: a comparison between commercially available assays. PLoS One 5, e11555 (2010).
Weeres, M. A. et al. The effects of 1,25-dihydroxyvitamin D3 on in vitro human NK cell development from hematopoietic stem cells. J Immunol 193, 3456–3462 (2014).
Milani, C. et al. Transcriptional effects of 1,25 dihydroxyvitamin D(3) physiological and supra-physiological concentrations in breast cancer organotypic culture. BMC Cancer 13, 119 (2013).
Acknowledgements
The authors like to thank the women who participated in the NICHD lactation vitamin D supplementation trial as well as Judy Shary, M.S. and Renee Washington, M.S. for their assistance with human milk samples collection and storage.
Author information
Authors and Affiliations
Contributions
Experimental design and manuscript preparation were by S.V.R., C.W., Y.S. and J.M. Collection of human milk and serum vitamin D were analyzed by C.W. and J.M. Western blot analysis of milk sample and breast epithelial cells was done by Y.S. and C.J. Real-time PCR analysis was performed by Y.S.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sambandam, Y., Reddy, S.V., Mulligan, J.L. et al. Vitamin D Modulation of TRAIL Expression in Human Milk and Mammary Epithelial Cells. Sci Rep 7, 4362 (2017). https://doi.org/10.1038/s41598-017-04521-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-04521-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.