Abstract
The study aimed to evaluate whether the benefits of dual antiplatelet therapy would be influenced by blood pressure (BP) levels, among acute minor stroke or transient ischemic attack (TIA). In CHANCE (Clopidogrel in High-Risk Patients with Acute Nondisabling cerebrovascular Events) trail, Patients were stratified by systolic BP (SBP) and diastolic BP (DBP) level measured on admission, respectively, using the supine position BP within 24 hours after symptoms onset. The primary efficacy outcome was stroke recurrence, bleeding was the safety outcome. Patients with SBP ≥ 140 mmHg, dual antiplatelet treatment could reduce the risk of stroke recurrence significantly (HR 0.654, 95% CI 0.529–0.793, p < 0.001) than mono antiplatelet therapy. And patients with DBP ≥ 90 mmHg, clopidogrel-aspirin significantly reduced the risk of recurrent stroke (HR 0.588, 95% CI 0.463–0.746, p < 0.001), compared with aspirin alone. However, in patients with SBP < 140 mmHg or DBP < 90 mmHg, no significant difference was observed between clopidogrel plus aspirin and aspirin alone. there was no difference in bleeding episodes by treatment assignment across categories of SBP or DBP. Patients with SBP ≥ 140 mmHg or DBP ≥ 90 mmHg after minor stroke or TIA got more benefits from dual antiplatelet therapy. Bleeding risk from dual antiplatelet treatment did not increase among patients with higher BP level on admission.
Similar content being viewed by others
Introduction
Minor ischemic stroke and transient ischemic attack (TIA) patients are at high risk of recurrent stroke from 12% to 20% during the first 3 months after the index stroke or TIA1,2,3. The Clopidogrel in High-risk patients with Acute Nondisabling Cerebrovascular Events (CHANCE) trial found that dual antiplatelet therapy (clopidogrel plus aspirin) within 24 hours after symptom onset could reduce the risk of subsequent stroke by 32.0%, as compared with aspirin alone4. Besides dual antiplatelet therapy, antihypertensive therapy is also an effective intervention for prevention of recurrent stroke in minor stroke patients5, 6. As we know, the Secondary Prevention of Small Subcortical Strokes (SPS3) trial support that in patients with recent lacunar stroke, the use of a systolic-blood-pressure (SBP) target of less than 130 mm Hg is likely to be beneficial7. However, no studies had focused on whether these 2 intervention strategies have interaction on stroke outcomes.
In this subgroup analysis of the Clopidogrel in High-Risk Patients with Acute Nondisabling cerebrovascular Events (CHANCE) trail, we aimed to investigate whether there was interaction between BP (SBP and DBP) level and antiplatelet therapy on stroke recurrence among patients with minor stroke and high-risk TIA.
Results
Baseline Characteristics
There were four patients missing the SBP value among the total patients, so 5166patients were enrolled in the final analysis. Among the SBP ≥ 140 mmHg and SBP < 140 mmHg group, the baseline characteristics of mono and dual antiplatelet therapy were well balanced (Table 1). The baseline characteristics of patients stratified by DBP were shown in Table 1S (Supplementary Table S1).
Efficacy and Safety Outcomes
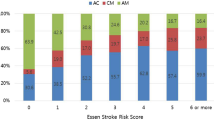
In patients with SBP < 140 mmHg, clopidogrel-aspirin could reduce the recurrent stroke (8.7% versus 13.2%, crude hazard ratio [HR] 0.654, 95% confidence interval [CI], 0.529–0.793, p < 0.001) and combined vascular events significantly (8.9% versus 13.4%, HR 0.651, 95% CI, 0.536–0.791, p < 0.001), compared with aspirin alone(Table 2 and Fig. 1). In addition, among patients with DBP ≥ 90 mmHg, dual antiplatelet therapy also significantly reduced the occurrence of new stroke (8.0 versus 13.3%, crude HR 0.588, 95% CI, 0.463–0.746, p < 0.001), and combined vascular events (8.2 versus 13.6%, crude HR 0.585, 95% CI, 0.462–0.741, p < 0.001) compared with mono antiplatelet treatment (Table 3 and Fig. 2).
Kaplan-Meier curves showing the time to stroke outcomes in patients with SBP ≥ 140 mmHg or SBP < 140 mmHg, treated with clopidogrel-aspirin or aspirin alone. (A) Cumulative probability of CVD by treatment among patients with SBP ≥ 140 mmHg; (B) Cumulative probability of CVD by treatment among patients with SBP < 140 mmHg; (C) Cumulative probability of stroke by treatment among patients with SBP ≥ 140 mmHg; (D) Cumulative probability of stroke by treatment among patients with SBP < 140 mmHg. Abbreviations: CVD = combined vascular events (ischemic stroke, hemorrhagic stroke, myocardial infarction, or vascular death); SBP = systolic blood pressure.
Kaplan-Meier curves showing the time to stroke outcomes in patients with DBP ≥ 90 mmHg or DBP < 90 mmHg, treated with clopidogrel-aspirin or aspirin alone. (A) Cumulative probability of CVD by treatment among patients with DBP ≥ 90 mmHg; (B) Cumulative probability of CVD by treatment among patients with DBP < 90 mmHg; (C) Cumulative probability of stroke by treatment among patients with DBP ≥ 90 mmHg; (D) Cumulative probability of stroke by treatment among patients with DBP < 90 mmHg. Abbreviations: CVD = combined vascular events (ischemic stroke, hemorrhagic stroke, myocardial infarction, or vascular death); DBP = diastolic blood pressure.
However, in patients with SBP < 140 mmHg or DBP < 90 mmHg, no significant difference was observed in the occurrence rate of recurrent stroke, and combined vascular events between clopidogrel -aspirin and aspirin alone (Figs 1 and 2).
After adjusting for gender, age, BMI, current or previous smoking and drinking, medical history (TIA or ischemic stroke, hypertension, hypercholesterolemia, diabetes mellitus), qualifying event (TIA or minor stroke), and secondary medication (anti-hypertension, anti-diabetes and lowering-lipid), the multivariable Cox proportional hazards models showed the similar results (Tables 2 and 3).
In addition, there was no significant difference of bleeding event rate between dual and mono antiplatelet treatment, either in SBP or DBP subgroup (Table 2 and 3).
Discussion
In this post-hoc analysis of the CHANCE trial, we found that patients with SBP ≥ 140 mmHg or DBP ≥ 90 mmHg got more benefits from dual antiplatelet therapy on stroke recurrence and CVD than patients with SBP < 140 mmHg or DBP < 90 mmHg. And clopidogrel plus aspirin did not increase the risk of bleeding in patients with SBP ≥ 140 mmHg or DBP ≥ 90 mmHg.
Why the BP level could affect the efficacy of dual antiplatelet therapy on patients with minor stroke or TIA? The precise underlying mechanism remains unclear. Because baseline BP was measured within 24 hours after stroke onset, we considered that the protection mechanism8,9,10 of stress-induced hypertension after stroke may amplify the efficacy of dual antiplatelet therapy, especially for those with large artery stenosis in cerebral or carotid arteries. Previous studies11, 12 indicated that dual antiplatelet therapy with clopidogrel and aspirin was more effective than aspirin alone in reducing microembolic signals in patients with ischemic stroke or TIA due to extracranial or intracranial arterial stenosis. And patients with multiple stenosis of cerebral arteries need higher BP level to maintain the cerebral perfusion13,14,15. The synergistic effect between high BP and dual antiplatelet may contribute to the current finding.
Elevated BP upon admission was common in patients with acute ischemic stroke, which was considered to play an important role in maintain the cerebral circulation and cerebral perfusion of ischemic tissue16, 17. However, several previous studies also demonstrated that increased BP in acute phase may be detrimental to the brain edema and hemorrhage transformation18,19,20. So the relationship between early elevation in BP and prognosis remains controversial, some reports suggested that initially high blood pressure was associated with a poor prognosis21,22,23, while other study suggested that elevated BP contributed to a more favorable prognosis8 or did not affect the prognosis24. The previous study demonstrated that elevated BP was significantly associated with a past history of hypertension, which was consisted with our study (See Table 1)17. As we all known, hypertension is one of the most important risk factor for atherosclerosis and stroke25, so patients with past history of hypertension maybe combine more serious atherosclerosis than normotensive patients, and need higher BP level to maintain the cerebral perfusion of ischemic tissue. We suspect that synergies between the hypertension and dual antiplatelet may improve the prognosis.
In the present study, clopidogrel plus aspirin did not seem to increase the greater bleeding risk in patients with elevated BP on admission than patients with SBP < 140 mmHg or DBP < 90 mmHg. Although the exact mechanism underlying the conflicting results was not clear, and the possible explanation for the difference as follow. First, compared with previous studies including patients with more severe stroke, the patients in our trail at a relative low risk for bleeding or hemorrhage transformation. Second, in our trail, dual antiplatelet treatment was administered for just 21days, followed by clopidogrel alone for a total of 90 days. Dual antiplatelet therapy in short term did not increase the risk of bleeding.
Our study has some limitations. Firstly, not all patients had imaging data in CHANCE trail26, we could not get the information about extracranial or intracranial arterial stenosis of all the patients, so the above assumption cannot be validated in the study. Further investigation is needed to investigate the synergistic effect between BP and dual antiplatelet therapy in ischemic stroke patients with symptomatic extracranial or intracranial arterial stenosis. Secondly, the incidence of bleeding events was lower in CHANCE trail, which may reduce the statistical power. So the future study need to further manifested the relationship between very high BP after ischemic stroke and bleeding risk, among patients who received dual antiplatelet treatment. Third, this study was a post-hoc analysis, which may increase the type I error, so our result need to be confirmed by other studies.
In conclusion, we found an interesting phenomenon, which may give some implications for clinical practice. That is, minor stroke or TIA patients with SBP ≥ 140 mmHg or DBP ≥ 90 mmHg, maybe more suitable for dual antiplatelet therapy. With respect to safety outcome, bleeding risk of dual antiplatelet therapy did not seem to increase with elevated BP.
Methods
Study population
CHANCE was a randomized, double-blind, placebo-controlled clinical trial at 114 clinical centers in China as reported elsewhere4, 27. In brief, patients ≥ 40 years with acute minor stroke (NIH Stroke Scale < [NIHSS]28 ≤3) or high-risk TIA (ABCD2 ≥4) within 24 hours of symptoms ictus were randomly assigned to either dual antiplatelet treatment (clopidogrel at an initial dose of 300 mg, followed by 75 mg per day for 90days, plus aspirin at a dose of 75 mg per day for the first 21 days) or mono antiplatelet treatment (aspirin at a dose of 75 mg per day for 90 days). The CHANCE protocol was approved by ethics committees of Beijing Tiantan Hospital and all other study centers. All participants or their legal proxies provided written informed consent.
Blood Pressure Measurement and Group Assignment
At admission, within 24 hours after symptoms ictus, three BP readings separated by at least two minutes in the supine position were recorded by doctors or trained nurses. Measurement of BP was according to a protocol for BP measurement in the clinic or office recommended by the American Heart Association29, and the average of the three readings as the BP on admission.
In this subgroup analysis, we tested the efficacy and safety of dual antiplatelet therapy in patients stratified by the BP level on admission: SBP ( ≥140 mmHg or < 140 mmHg),and DBP ( ≥90 mmHg or < 90 mmHg), respectively.
Outcomes assessment
The efficacy outcomes4 were stroke recurrence (ischemic stroke or hemorrhage stroke), and combined vascular events (ischemic stroke, hemorrhagic stroke, myocardial infarction, or vascular death) during 90 days of follow-up. The safety outcome was any bleeding, according to the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries (GUSTO) definition30. Moreover, the follow-up at 90-day was done by face to face. All of the efficacy and safety outcomes were confirmed by the central adjudication committee which was blinded to the study group assignments.
Statistical analysis
We used SAS version 9.4 (SAS Institute Inc, Cary, NC) for all statistical analyses. For descriptive analysis, proportions and medians were used for categorical and continuous variables. The baseline characteristics among dual and mono antiplatelet therapy in BP subgroup were compared by Chi-square tests or Fisher exact test for categorical variables and continuous variables were compared by Kruskal-Wallis test. For each group stratified by BP level, the differences between dual and mono antiplatelet therapy in the rates of stroke recurrence, combined vascular events, and bleeding during the 90 days follow up were evaluated by using crude and multivariable Cox proportional hazards models. Two-tailed p value less than 0.05 indicated statistical significance.
References
Coull, A. J., Lovett, J. K. & Rothwell, P. M. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. Bmj 328, 326 (2004).
Johnston, S. C., Gress, D. R., Browner, W. S. & Sidney, S. Short-term prognosis after emergency department diagnosis of TIA. Jama 284, 2901–2906 (2000).
Kleindorfer, D. et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 36, 720–723 (2005).
Wang, Y. et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med 369, 11–19 (2013).
Mills, K. T. et al. Global Disparities of Hypertension Prevalence and ControlClinical Perspective. Circulation 134, 441–450 (2016).
PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 358, 1033–1041 (2001).
Benavente, O. R. et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet 382, 507–515 (2013).
Chamorro, A. et al. Blood pressure and functional recovery in acute ischemic stroke. Stroke 29, 1850–1853 (1998).
Sharma, V. K. Elevated Blood Pressure in Acute Ischemic Stroke–Treat or Leave? Cerebrovasc Dis 41, 101–102 (2016).
Rusanen, H., Saarinen, J. T. & Sillanpaa, N. The association of blood pressure and collateral circulation in hyperacute ischemic stroke patients treated with intravenous thrombolysis. Cerebrovasc Dis 39, 130–137 (2015).
Wong, K. S. et al. Clopidogrel plus aspirin versus aspirin alone for reducing embolisation in patients with acute symptomatic cerebral or carotid artery stenosis (CLAIR study): a randomised, open-label, blinded-endpoint trial. The Lancet Neurology 9, 489–497 (2010).
Markus, H. S. et al. Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic carotid stenosis evaluated using doppler embolic signal detection: the Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis (CARESS) trial. Circulation 111, 2233–2240 (2005).
Rordorf, G. et al. Pharmacological elevation of blood pressure in acute stroke. Clinical effects and safety. Stroke 28, 2133–2138 (1997).
Lee, M. et al. Effect of Blood Pressure Lowering in Early Ischemic Stroke: Meta-Analysis. Stroke 46, 1883–1889 (2015).
Liu, S., Li, C., Li, T., Xiong, J. & Zhao, X. Effects of Early Hypertension Control after Ischaemic Stroke on the Outcome: A Meta-Analysis. Cerebrovasc Dis 40, 270–278 (2015).
Eizenberg, Y., Koton, S., Tanne, D. & Grossman, E. Association of age and admission mean arterial blood pressure in patients with stroke-data from a national stroke registry. Hypertension Research 39, 356–361 (2016).
Manabe, Y., Kono, S., Tanaka, T., Narai, H. & Omori, N. High blood pressure in acute ischemic stroke and clinical outcome. Neurology International 1, e1 (2009).
Ishitsuka, K. et al. High blood pressure after acute ischemic stroke is associated with poor clinical outcomes: Fukuoka Stroke Registry. Hypertension 63, 54–60 (2014).
Wu, W. et al. Relationship between Blood Pressure and Outcomes in Acute Ischemic Stroke Patients Administered Lytic Medication in the TIMS-China Study. PLoS One 11, e0144260 (2016).
Koton, S., Eizenberg, Y., Tanne, D. & Grossman, E. Trends in admission blood pressure and stroke outcome in patients with acute stroke and transient ischemic attack in a National Acute Stroke registry. Journal of hypertension 34, 316–322 (2016).
Kjeldsen, S. E. & Berge, E. Blood pressure and early neurological deterioration in acute ischemic stroke. Journal of hypertension 33, 2020–2021 (2015).
Geeganage, C. et al. Relationship between baseline blood pressure parameters (including mean pressure, pulse pressure, and variability) and early outcome after stroke: data from the Tinzaparin in Acute Ischaemic Stroke Trial (TAIST). Stroke 42, 491–493 (2011).
Sandset, E. C. et al. Relation between change in blood pressure in acute stroke and risk of early adverse events and poor outcome. Stroke 43, 2108–2114 (2012).
Leonardi-Bee, J. et al. Blood Pressure and Clinical Outcomes in the International Stroke Trial. Stroke 33, 1315–1320 (2002).
Feigin, V. L. et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet Neurology 15, 913–924 (2016).
Liu, L. et al. Dual antiplatelet therapy in stroke and ICAS: Subgroup analysis of CHANCE. Neurology 85, 1154–1162 (2015).
Wang, Y. et al. Rationale and design of a randomized, double-blind trial comparing the effects of a 3-month clopidogrel-aspirin regimen versus aspirin alone for the treatment of high-risk patients with acute nondisabling cerebrovascular event. American Heart Journal 160(380–386), e381 (2010).
Lyden, P. et al. Improved reliability of the NIH Stroke Scale using video training. NINDS TPA Stroke Study Group. Stroke 25, 2220–2226 (1994).
Pickering, T. G. et al. Recommendations for blood pressure measurement in humans: an AHA scientific statement from the Council on High Blood Pressure Research Professional and Public Education Subcommittee. Journal of ClinicalHypertension 7, 102–109 (2005).
GUSTO investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. The GUSTO investigators. N Engl J Med 329, 673–682 (1993).
Acknowledgements
The authors thank all participating investigators.The study was supported by grants from the Ministry of Science and Technology of the People’s Republic of China (2011BAI08B01, and 2013BAI09B03), and a grant from Beijing Municipal Administration of Hospitals’ Youth Programme (QML2015 0504).
Author information
Authors and Affiliations
Contributions
J.X. ad Y.T. wrote the manuscript. H.L. and H.G. analyzed data. X.X., X.M., and Y.X. performed the research. Yilong Wang and Yongjun Wang conceived, designed and supervised the study. All authors reviewed and finally approved the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, J., Tao, Y., Li, H. et al. Different levels of blood pressure, different benefit from dual antiplatelet therapy in minor stroke or TIA patients. Sci Rep 7, 3884 (2017). https://doi.org/10.1038/s41598-017-04169-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-04169-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.