Abstract
This study evaluated the prevalence and factors associated with sleep disturbance in a large cohort of HIV-infected patients across China. A cross-sectional study was conducted among HIV-infected patients on antiretroviral therapy at 20 AIDS clinics. The Pittsburgh Sleep Quality Index was self-administered by subjects. Socio-demographic characteristics, medical history and HIV-related clinical data were collected. 4103 patients had complete data for analysis. Sleep disturbances were observed in 43.1% of patients. Associated factors in multivariable analysis included psychological factors: anxiety (odds ratio [OR], 3.13; 95% confidence interval [CI], 2.44–4.00; P < 0.001), depression (OR, 2.09; 95% CI, 1.70–2.57; P < 0.001), and both anxiety and depression (OR, 5.90; 95% CI, 4.86–7.16; P < 0.001); sociodemographic factors: MSM (OR, 1.26; 95% CI, 1.04–1.52; P = 0.018), being single (OR, 1.45; 95%CI 1.21–1.74; P < 0.001), higher education (OR, 1.25; 95% CI, 1.03–1.53; P = 0.025); and clinical factors: suboptimal adherence (OR,1.51; 95% CI,1.23–1.85; P < 0.001), regimen-switching (OR, 1.94; 95% CI, 1.12–3.35; P = 0.018), and antidepressant use (OR, 1.98; 95% CI, 1.47–2.67; P = 0.044). Prevalence of sleep disturbance is high in this large Chinese cohort. Associated factors appear related to psychological and social-demographic factors. Health workers may consider routinely assessing sleep disturbances among HIV-infected patients, especially in the first three months after HIV diagnosis, and referring for mental health services, which may positively impact adherence to treatment.
Similar content being viewed by others
Introduction
HIV-infected individuals appear to be more vulnerable to sleep disturbances than the general population1,2,3,4. However, awareness of sleep disturbance as a health issue in general and as an HIV-related health issue specifically is low among patients, who do not emphasize such issues with their physician5, 6. Administration of standardized sleep assessment tools, such as the Pittsburg Sleep Quality Index (PSQI), Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), and the International Classification of Sleep Disorders (ICSD-2) in cohorts of HIV-infected individuals have observed a high prevalence of sleep disturbances from 40% to 70%4, 7, 8. Major sleep disturbances frequently go undiagnosed and untreated and may have severe health consequences, such as depression and anxiety6, 9. A range of primary sleep disorder symptoms overlap with psychological and behavioral factors, requiring targeted diagnostic and treatment interventions10, 11.
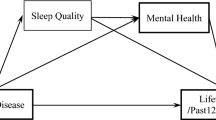
The pathophysiology of sleeping disturbances among HIV-infected patients is unclear, but may be related to the ability of HIV to infect the central nervous system (CNS), the impact of antiretroviral medications, mental health issues, and substance abuse6, 12,13,14. Sleep disturbances occur throughout all stages of infection, and may be associated with the virus itself, antiretroviral drugs, or antidepressants. It may also increase the risk for psychiatric disorders, cardiovascular morbidity, and mortality, but the degree and direction of causality are unclear15, 16.
Although the prevalence of sleeping disorders is reportedly high among HIV-infected persons, relatively few studies exist in the literature during the antiretroviral therapy (ART) era15, 17. Recent studies have largely focused on the impact of specific antiretroviral agents (e.g., efavirenz) on sleep disturbances18,19,20. Anxiety and depression are psychological factors that have been found to affect sleep quality4, 21, 22. Regardless of its etiology, sleep disturbances is clinically important in this population due to potential impact on quality of life, adherence to ART cognition impairment, comorbid psychiatric disorders like anxiety/depression and immune system function6, 23, 24. The purpose of this paper is to evaluate the epidemiology and associated risk factors for sleep disorders in AIDS patients and to recommend early evaluation for and detection of these conditions among people living with HIV.
Results
Characteristics of study population
We evaluated 4103 HIV-infected persons (Tables 1 and 2). Mean age of the cohort was 37.6 years (standard deviation [SD], 11.7 years), 79.4% were male, and 38.5% were MSM. The median time from HIV diagnosis to study enrollment was 27 months (interquartile range [IQR], 11–58 months), the median duration of ART was 18 months (IQR, 6–43 months), 15.5% had a current CD4+ cell count below 200 cells/mm3, and 48.4% had an undetectable HIV RNA level. 75.4% of patients were on their original first-line ART regimen and had not experienced an ART regimen switch.
Prevalence of sleep disturbances
Median PSQI score for 3873 HIV-infected persons was 5 (IQR: 3–7). Over 40% (43.1%, 95% confidence interval [CI], 41.5%–44.7%) of participants had a PSQI score >5, suggestive of sleep disturbance.
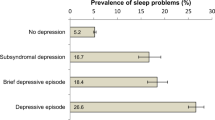
Prevalence of sleep disturbances among patients with anxiety and depression
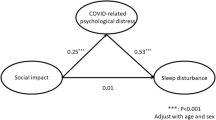
Median HADS score was 5 (IQR: 2–8) for anxiety and 5 (IQR: 2–9) for depression. Among the 3873 HIV-infected persons evaluated for anxiety and depression, prevalence of sleep disturbances differed significantly (P < 0.001) between those who suffered anxiety (68.1%) and those who did not (33.6%), and between those who suffered depression (61.2%) and those who did not (34.3%).
Factors associated with sleep disturbances
In univariate analyses, factors associated with sleep disturbance (PSQI > 5) included age, education, transmission route, marital status, support from family/friends, time of diagnosed with HIV infection, drug adherence, number of ART regimens, current antidepressant use, and anxiety and depression. There were no significant associations with HIV-specific clinical factors including ART use (including EFV- containing regimens) and sleep. In the final multivariable model combining all of the significant variables above, factors associated with sleep disturbance based on the PSQI included education (P = 0.044), transmission route (P = 0.040), marital status (P < 0.001), drug adherence (P = 0.001), current EFV-based regimen (P = 0.039), antidepressant use (P = 0.039), and anxiety and depression (P < 0.001) (Table 3).
Regarding the association of poor sleep and depression by Hospital Anxiety and Depression (HAD) scores, sleep disturbance was present in 34.3% of those without depression (P < 0.001). Moreover, higher HAD scores were significantly associated with higher PSQI scores (r = 0.365; P < 0.001). Participants with a higher risk of anxiety (HAD > 8) had a 4-fold higher odds of sleep disturbance than those with lower HAD scores (HAD ≤ 8) (odds ratio [OR], 4.22; 95% CI, 3.63–4.91; P < 0.001), whereas those with a higher risk of depression (HAD > 8) had a 3-fold higher odds of sleep disturbance relative to those with a HAD ≤ 8 (OR, 3.01; 95% CI, 2.62–3.46; P < 0.001).
Discussion
This study represents one of the largest epidemiologic studies of the prevalence of sleep disturbances as measured by PSQI among HIV-infected persons in the ART era25, 26. The PSQI is a standardized questionnaire frequently used in studies of HIV-positive persons, which has a cut-off score indicative of sleep disturbance, however, it lacks specificity for insomnia11, 27,28,29,30.
HIV remains a highly stigmatized condition in China, with patients reporting emotional, financial, and physical burdens resulting from stigma31. Discrimination is experienced from both medical and non-medical sources31, 32, despite legal protection from discrimination in accessing medical care, employment, and educational opportunities33. The potential interaction between the experience of stigma and sleep disturbance have not been studied in this context but could potentially play a role in understanding sleep disturbance in this population.
Data from general population surveys in China suggest that the prevalence of sleep disturbance in healthy populations is about 10%34. Our finding that HIV-infected persons have a high prevalence of sleep disturbance even in the ART era suggests that there are specific mechanisms causing poor sleep quality that are unique to this population or to HIV infection. HIV-infected persons with poor immune recovery did not have a statistically significantly higher rate of sleep disturbance when compared to those who had better immune recovery with nearly normal CD4+ cell counts above 500 cells/mm3. We did not find a relationship between sleep and CD4+ cell counts or HIV RNA in either direction. This is consistent with some studies that have not found any relationship15, 18, however others have found that sleep disturbances are independently related to immune status26, 35,36,37. Other studies conducted in the pre-ART era showed an association between sleep and CD4+ cell counts or HIV RNA7, 38, 39. The divergence of findings may be due to the differences in the tools used or to the fact that the prior studies were conducted in the pre-ART era when HIV perhaps played a more direct role in sleep.
Regarding HIV-specific factors, we found pill burden, poor adherence and more frequent switching of ART regimens were associated with higher proportions of poor sleep. These data suggest that in the ART era, patients with optimal adherence and patients who had not switched ART had lower rates of sleep disturbances. Duration of ART did not have statistical significance. Furthermore, patients on EFV-based regimen did not suffer a higher rate of sleep disturbance compared with patients on non-EFV-based regimens. However, patients who had initiated an EFV-based regimen in the last half year did have a marginally higher rate of sleep disturbance. This suggests that the sample may be biased, in that patients who had suffered CNS side effects from EFV may have switched regimens prior to the cross-sectional study, leaving only patients who did not suffer EFV-related side effects in the sample. In addition, antiretroviral agents with high CNS penetration effectiveness scores may be protective of HIV’s effects on the CNS. On the other hand, some drugs may be associated with adverse sleep effects (e.g., EFV), especially at higher plasma levels36, 40, 41. Data from prior studies among HIV-infected persons with EFV-based regimen did find much higher rates of sleep disturbance40. However, these studies were conducted when patients had concurrent opportunistic infections42, making attribution to EFV difficult. Our population consisted of all HIV-infected persons with free access to antiretroviral therapy, without AIDS-related opportunistic infections at the time of investigation.
In our study, the length of time since HIV diagnosis was found to be associated with sleep disturbances, with a significant association between shorter duration from diagnosis and poor quality of sleep. HIV infection remains a highly stigmatized illness in China, and can be accompanied by identity stigma and low self-esteem. These symptoms can be considered normal emotional responses to the reality of living with HIV as well as symptoms of depression. These may explain the higher rate of sleep disturbances in the first several months after diagnosis7. This finding however conflicts with that of other studies that have assessed sleep disturbances in relation to duration of infection. Imeri and Opp and Seay et al. did not find any association between them in their studies39, 43.
In addition, HIV-infected women did not have a statistically significantly burden of sleep disturbance compared with men. People who used illicit drugs and MSM had a higher rate of sleep disturbances as compared to heterosexuals, which may be related to their marginalized position in Chinese society44. Individuals with higher education had statistically greater odds of poor sleep compared with those with less education. Married individuals had a lower rate of sleep disturbance, potentially due to marriage conferring more family support, as we found that patients who report support from family or friends consistently had a lower rate of poor sleep.
The strongest associations found in our study were between depression and anxiety and sleep disturbance. This finding is consistent with other studies21, 45, 46, and shows that psychiatric disorders are a major factor in sleep disturbances among HIV-infected patients. Given the likely bidirectional association between sleep and depression or anxiety, targeted management of one may improve the other. Therefore, treating depression and anxiety might improve sleep quality, and addressing sleep disturbances may relieve psychological morbidity45, 47, 48.
Despite a high prevalence of sleep disturbance among HIV- infected persons, among patients with PSQI > 5, only 11.19% were regularly using sleep medication. Treatment with cognitive behavioral therapy for sleep disturbance or insomnia, considered first line treatment for insomnia, was not measured. Prior studies have also noted that most patients with sleep disturbances remain untreated and often have a poor understanding of available treatment options8, 49.
Our study had several potential limitations. Sleep disturbances were diagnosed based on questionnaire data rather than polysomnograms or actigraphy data; however, we used standardized instruments comparable to those used in other studies, and some experts suggest that self-reported data may be more representative of sleep issues4, 27, 50. The cross-sectional study design did not allow for assessment of the temporal relationship between poor sleep and factors (e.g., depression improvement or pre- and post-ART), the direction of causality, or for the assessment of whether sleep disturbances were transient or chronic in nature. Presence of pain, which has been shown to be associated with sleep disturbance in the literature, was not assessed. Finally, the lack of HIV-uninfected controls is a limitation of the study.
Our study had several strengths. This study is one of the largest study to date assessing sleep disturbance among HIV-infected patients on treatment15, 38, 51. It used validated measures that are quick and inexpensive to implement to assess sleep disturbances, anxiety and depression and could easily be integrated into routine clinical practice27, 50.
In summary, the high prevalence of poor sleep suggests that treating sleep disturbances in those with HIV infection may have a positive impact on their quality of life and could potentially yield improvements to adherence to ARTs and mental health. HIV providers may consider routinely assessing sleep disturbances especially in the first three months of HIV diagnosis, and referring for mental health and social support services if PSQI > 5. Therefore, integrating assessment of sleep disturbance into routine care and even extensive sleep quality evaluations at home for HIV-infected patients may be advisable in China. Prospective cohort studies that track sleep disturbance from time of diagnosis through treatment initiation and continuation could be useful to characterize the relationship between sleep disturbance, HIV, and treatment further.
Methods
Study Design and Participants
We conducted a cross-sectional study among 4724 HIV-infected adults on treatment, collecting data between January 2014 and December 2015 from patients at 20 HIV clinics across China covering Beijing, Guangxi, Yunnan and other major municipalities. The study enrolled patients accessing services at HIV clinics who were at least 18 years, diagnosed with HIV infection, on antiretroviral therapy, and not pregnant within the prior 3 months. Exclusion criteria included the presence of any acute medical condition that could affect the ability to complete the study questionnaire.
All participants provided written informed consent to complete a survey and have their medical data abstracted from their medical records. The study was approved by Beijing Youan Hospital institutional review board. All experiments were performed in accordance with relevant guidelines and regulations.
Main Outcomes
Each participant completed the PSQI questionnaire, a 19-item questionnaire that assesses seven sleep components (sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of hypnotics, and daytime dysfunction) during the prior month. The scores for these components range from 0 (no difficulty) to 3 (severe difficulty) and are summed to produce a global measure of sleep disturbance, with a higher score denoting poorer sleep quality (range: 0–21). The Chinese version of PSQI was developed, widely used in adolescents, adults and elderly healthy and clinical groups, and showed good internal consistency, split half and retest reliability52, 53. We used the PSQI cut off of global score >5 on the PSQI instrument27 (sensitivity of 90% and specificity of 87%) to define sleep disturbance in this cohort. The HAD scale which consists of seven items relating to depression (HAD-D) and another seven relating to anxiety (HAD-A) was also administered and anxiety and depression were defined as a HAD score ≥8 on each subscale54.
Demographic, behavioral, and psychosocial data were collected through self-administered survey. Clinical data were abstracted from medical records. This included HIV-specific data, like date of HIV diagnosis, history of medical conditions, current CD4+ cell counts and HIV RNA levels, and ART regimen at the time of survey. 4103 (86.9%) patients had complete data for analysis.
Statistical Analysis
Descriptive statistics are presented as means with SDs, or counts with proportions, as appropriate. Two sample t tests were used to compare means, and χ2 tests were used to compare proportions. Logistic regression analysis was used to investigate associations between sleep outcome and demographic, behavioral, psychosocial, and clinical factors. Odds ratios for sleep disturbance were estimated with 95% CIs. Factors with a P value < 0.10 in univariate models were initially included in the multivariable model and were then eliminated using backward selection. Linear regression and the Pearson correlation coefficient were used to explore the relationship between the PSQI score and HAD score. All P values were 2-sided, and P values < 0.05 were considered significant. Analyses were conducted using SPSS software 21.0.
References
Xiang, Y. T. et al. I. Sleep 31, 1655–1662 (2008).
Norman, S. E. et al. Sleep disturbances in HIV-seropositive patients. Jama 260, 922 (1988).
White, J. L. et al. Early central nervous system response to HIV infection: sleep distortion and cognitive-motor decrements. AIDS 9, 1043–1050 (1995).
Reid, S. & Dwyer, J. Insomnia in HIV infection: a systematic review of prevalence, correlates, and management. Psychosom Med 67, 260–269, doi:10.1097/01.psy.0000151771.46127.df (2005).
Morin, C. M., LeBlanc, M., Daley, M., Gregoire, J. P. & Merette, C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med 7, 123–130, doi:10.1016/j.sleep.2005.08.008 (2006).
Low, Y., Goforth, H., Preud’homme, X., Edinger, J. & Krystal, A. Insomnia in HIV-infected patients: pathophysiologic implications. AIDS Rev 16, 3–13 (2014).
Oshinaike, O. et al. Quality of Sleep in an HIV Population on Antiretroviral Therapy at an Urban Tertiary Centre in Lagos, Nigeria. Neurol Res Int 2014, 298703, doi:10.1155/2014/298703 (2014).
Rubinstein, M. L. & Selwyn, P. A. High prevalence of insomnia in an outpatient population with HIV infection. J Acquir Immune Defic Syndr Hum Retrovirol 19, 260–265 (1998).
Taibi, D. M. Sleep disturbances in persons living with HIV. J Assoc Nurses AIDS Care 24, S72–85, doi:10.1016/j.jana.2012.10.006 (2013).
Wibbeler, T., Reichelt, D., Husstedt, I. W. & Evers, S. Sleepiness and sleep quality in patients with HIV infection. J Psychosom Res 72, 439–442, doi:10.1016/j.jpsychores.2012.03.003 (2012).
Mollayeva, T. et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev 25, 52–73, doi:10.1016/j.smrv.2015.01.009 (2016).
Ian, E. et al. The burden of HIV-associated neurocognitive disorder (HAND) in the Asia-Pacific region and recommendations for screening. Asian J Psychiatr, doi:10.1016/j.ajp.2015.10.009 (2015).
Byun, E., Gay, C. L. & Lee, K. A. Sleep, Fatigue, and Problems With Cognitive Function in Adults Living With HIV. J Assoc Nurses AIDS Care 27, 5–16, doi:10.1016/j.jana.2015.10.002 (2016).
Heaton, R. K. et al. Neurocognitive change in the era of HIV combination antiretroviral therapy: the longitudinal CHARTER study. Clin Infect Dis 60, 473–480, doi:10.1093/cid/ciu862 (2015).
Allavena, C. et al. Prevalence and Risk Factors of Sleep Disturbance in a Large HIV-Infected Adult Population. AIDS Behav 20, 339–344, doi:10.1007/s10461-015-1160-5 (2016).
Wu, J., Wu, H., Lu, C., Guo, L. & Li, P. Self-reported sleep disturbances in HIV-infected people: a meta-analysis of prevalence and moderators. Sleep Med 16, 901–907, doi:10.1016/j.sleep.2015.03.027 (2015).
Li, J. et al. Prevalence and associated factors of depressive and anxiety symptoms among HIV-infected men who have sex with men in China. AIDS Care 28, 465–470, doi:10.1080/09540121.2015.1118430 (2016).
Crum-Cianflone, N. F. et al. Prevalence and factors associated with sleep disturbances among early-treated HIV-infected persons. Clin Infect Dis 54, 1485–1494, doi:10.1093/cid/cis192 (2012).
Kelly, C. M. et al. HIV associated neurocognitive disorders (HAND) in Malawian adults and effect on adherence to combination anti-retroviral therapy: a cross sectional study. PloS one 9, e98962, doi:10.1371/journal.pone.0098962 (2014).
Gamaldo, C. E. & McArthur, J. C. The evaluation and diagnosis of “insomnia” in relation to sleep disturbance prevalence and impact in early-treated HIV-infected persons. Clin Infect Dis 55, 1429–1430, author reply 1430-1421, doi:10.1093/cid/cis698 (2012).
Leyro, T. M., Babson, K. A. & Bonn-Miller, M. O. Anxiety sensitivity in relation to sleep quality among HIV-infected individuals. J Assoc Nurses AIDS Care 25, 638–645, doi:10.1016/j.jana.2014.02.002 (2014).
Low, Y., Preud’homme, X., Goforth, H. W., Omonuwa, T. & Krystal, A. D. The association of fatigue with depression and insomnia in HIV-seropositive patients: a pilot study. Sleep 34, 1723–1726, doi:10.5665/sleep.1446 (2011).
Saberi, P., Neilands, T. B. & Johnson, M. O. Quality of sleep: associations with antiretroviral nonadherence. AIDS Patient Care STDS 25, 517–524, doi:10.1089/apc.2010.0375 (2011).
Miners, A. et al. Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: a cross-sectional comparison with the general population. Lancet HIV 1, e32–40, doi:10.1016/S2352-3018(14)70018-9 (2014).
Darko, D. F., McCutchan, J. A., Kripke, D. F., Gillin, J. C. & Golshan, S. Fatigue, sleep disturbance, disability, and indices of progression of HIV infection. Am J Psychiatry 149, 514–520, doi:10.1176/ajp.149.4.514 (1992).
Perkins, D. O. et al. Somatic symptoms and HIV infection: relationship to depressive symptoms and indicators of HIV disease. Am J Psychiatry 152, 1776–1781, doi:10.1176/ajp.152.12.1776 (1995).
Buysse, D. J., Reynolds, C. F. 3rd, Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28, 193–213 (1989).
Gamaldo, C. E. et al. Evaluating sleep and cognition in HIV. J Acquir Immune Defic Syndr 63, 609–616, doi:10.1097/QAI.0b013e31829d63ab (2013).
Low, Y. et al. Comparison of polysomnographic data in age-, sex- and Axis I psychiatric diagnosis matched HIV-seropositive and HIV-seronegative insomnia patients. Clin Neurophysiol 123, 2402–2405, doi:10.1016/j.clinph.2012.05.004 (2012).
Gamaldo, C. E. et al. Sleep, function and HIV: a multi-method assessment. AIDS Behav 17, 2808–2815, doi:10.1007/s10461-012-0401-0 (2013).
Zhang, C. et al. Emotional, physical and financial burdens of stigma against people living with HIV/AIDS in China. AIDS care 28(Suppl 1), 124–131, doi:10.1080/09540121.2016.1146206 (2016).
Liu, Y. et al. Barriers and Facilitators of Linkage to and Engagement in HIV Care Among HIV-Positive Men Who Have Sex with Men in China: A Qualitative Study. AIDS patient care and STDs 30, 70–77, doi:10.1089/apc.2015.0296 (2016).
Kaufman, J. In Thinking Politically about HIV (eds Kent Buse & Dennis Altman) (Routledge, 2013).
Xiang, Y. T. et al. The prevalence of insomnia, its sociodemographic and clinical correlates, and treatment in rural and urban regions of Beijing, China: a general population-based survey. Sleep 31, 1655–1662 (2008).
Lee, K. A. et al. Types of sleep problems in adults living with HIV/AIDS. J Clin Sleep Med 8, 67–75, doi:10.5664/jcsm.1666 (2012).
Nokes, K. M. & Kendrew, J. Correlates of sleep quality in persons with HIV disease. J Assoc Nurses AIDS Care 12, 17–22, doi:10.1016/S1055-3290(06)60167-2 (2001).
Cohen, F. L., Ferrans, C. E., Vizgirda, V., Kunkle, V. & Cloninger, L. Sleep in men and women infected with human immunodeficiency virus. Holist Nurs Pract 10, 33–43 (1996).
Allavena, C. et al. Prevalence and risk factors of sleep disturbances in a large HIV-infected adult population. J Int AIDS Soc 17, 19576, doi:10.7448/IAS.17.4.19576 (2014).
Seay, J. S. et al. Self-reported sleep disturbance is associated with lower CD4 count and 24-h urinary dopamine levels in ethnic minority women living with HIV. Psychoneuroendocrinology 38, 2647–2653, doi:10.1016/j.psyneuen.2013.06.022 (2013).
Nunez, M. et al. Higher efavirenz plasma levels correlate with development of insomnia. J Acquir Immune Defic Syndr 28, 399–400 (2001).
Moyle, G., Fletcher, C., Brown, H., Mandalia, S. & Gazzard, B. Changes in sleep quality and brain wave patterns following initiation of an efavirenz-containing triple antiretroviral regimen. HIV Med 7, 243–247, doi:10.1111/j.1468-1293.2006.00363.x (2006).
Gallego, L. et al. Analyzing sleep abnormalities in HIV-infected patients treated with Efavirenz. Clin Infect Dis 38, 430–432, doi:10.1086/380791 (2004).
Imeri, L. & Opp, M. R. How (and why) the immune system makes us sleep. Nat Rev Neurosci 10, 199–210, doi:10.1038/nrn2576 (2009).
Li, H. H., Holroyd, E., Lau, J. & Li, X. Stigma, Subsistence, Intimacy, Face, Filial Piety, and Mental Health Problems Among Newly HIV-Diagnosed Men Who Have Sex With Men in China. J Assoc Nurses AIDS Care 26, 454–463, doi:10.1016/j.jana.2015.02.004 (2015).
Ford, D. E. & Kamerow, D. B. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? Jama 262, 1479–1484 (1989).
Junqueira, P., Bellucci, S., Rossini, S. & Reimao, R. Women living with HIV/AIDS: sleep impairment, anxiety and depression symptoms. Arq Neuropsiquiatr 66, 817–820 (2008).
Soehner, A. M., Kaplan, K. A. & Harvey, A. G. Prevalence and clinical correlates of co-occurring insomnia and hypersomnia symptoms in depression. J Affect Disord 167, 93–97, doi:10.1016/j.jad.2014.05.060 (2014).
Soehner, A. M. & Harvey, A. G. Prevalence and functional consequences of severe insomnia symptoms in mood and anxiety disorders: results from a nationally representative sample. Sleep 35, 1367–1375, doi:10.5665/sleep.2116 (2012).
Ancoli-Israel, S. & Roth, T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep 22(Suppl 2), S347–353 (1999).
Johns, M. W. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14, 540–545 (1991).
Luo, J. et al. Prevalence and risk factors of poor sleep quality among Chinese elderly in an urban community: results from the Shanghai aging study. PloS one 8, e81261, doi:10.1371/journal.pone.0081261 (2013).
Guo, S., Sun, W., Liu, C. & Wu, S. Structural Validity of the Pittsburgh Sleep Quality Index in Chinese Undergraduate Students. Front Psychol 7, 1126, doi:10.3389/fpsyg.2016.01126 (2016).
Tzeng, J. I., Fu, Y. W. & Lin, C. C. Validity and reliability of the Taiwanese version of the Pittsburgh Sleep Quality Index in cancer patients. Int J Nurs Stud 49, 102–108, doi:10.1016/j.ijnurstu.2011.08.004 (2012).
Christodoulou, C. et al. Hospital anxiety and depression scale. A quantitative analysis in medical outpatients, psychiatric outpatients and normal subjects. Psychiatriki 21, 279–286 (2010).
Acknowledgements
The authors thank the site leaders and other SAD study group members, Prof. Taisheng Li (Peking Union Medical College Hospital), Dr. Lijun Sun (Beijing Youan Hospital, Capital Medical University), Dr. Haolan He, Dr. Huolin Zhong (The Eighth People’s Hospital of Guangzhou), Dr. Rongxia Ye (The Sixth People’s Hospital of Hangzhou), and Dr. Gang Xiao (The First People’s Hospital of Changsha), whom they acknowledge as critical in the development, implementation, and analysis of this study. This work was supported by Major Project of Beijing Municipal Science and Technology Committee (D141100000314005, D141100000314002, D131100005313005), Beijing Key Laboratory (No. BZ0089), Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (No. ZY201401), and the National Natural Science Foundation of China (No. 81501731).
Author information
Authors and Affiliations
Contributions
Xiaojie Huang and Hui Chen led the analysis and writing of this manuscript. Xiaojie Huang, Hao Wu, Kathrine Meyers and Hui Chen contributed to the final version. Hao Wu is the Principle Investigator and designed the study. Huiqin Li, Kathrine Meyers, Zhihao Meng, Wei Xia, Chongxi Li, Jinsong Bai, Shenghua He, Weiping Cai, Chengyu Huang, Shuiqing Liu, Hui Wang, Xuemei Ling, Ping Ma, Daling Tan, Fuxiang Wang, Lianguo Ruan, Hongxin Zhao, Hongxia Wei, Yanfen Liu, Jianhua Yu, Hongzhou Lu, Min Wang and Tong Zhang were involved in managing the data collection. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, X., Li, H., Meyers, K. et al. Burden of sleep disturbances and associated risk factors: A cross-sectional survey among HIV-infected persons on antiretroviral therapy across China. Sci Rep 7, 3657 (2017). https://doi.org/10.1038/s41598-017-03968-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03968-3
This article is cited by
-
Neurological care for LGBT+ people
Nature Reviews Neurology (2024)
-
Psychological Mechanisms of Internalized HIV Stigma Affect Sleep Impairment among People Living with HIV in China: A follow-up Study
AIDS and Behavior (2024)
-
Lived experiences of Palestinian patients with COVID-19: a multi-center descriptive phenomenological study of recovery journey
BMC Public Health (2022)
-
Sleep Disturbances and Chronic Pain in People with HIV: Implications for HIV-Associated Neurocognitive Disorders
Current Sleep Medicine Reports (2022)
-
Effects of an intensive lifestyle intervention and the role of sleep in people living with HIV and prediabetes: a pilot and feasibility study
BMC Research Notes (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.