Abstract
The study aims to evaluate, using the Iterative Closest Point (ICP) algorithm, the repeatability of successive corneal elevation measurements taken post-LASIK. Two topography maps of 98 LASIK participants were recorded preoperatively (Pre), 1 month (Pos1M) and 3 months postoperatively (Pos3M). Elevation of the second measurement was fitted to the first measurement by calculating using ICP, and correcting for, both translational and rotational misalignment components. The RMS of elevation differences between anterior corneal measurements were statistically significant post-LASIK compared to preoperation (P < 0.05). A misalignment ratio used to describe the weighting of the elevation difference caused by misalignment relative to the total difference remained stable (0.40 and 0.23 for anterior and posterior corneal surfaces, respectively) in different periods. The study also considered the combined misalignment parameter (CM), which represents the total effect of all individual misalignment components on the repeatability of corneal topography maps. CM was significantly greater post-LASIK relative to pre-LASIK (P < 0.05). Overall, the contribution of misalignment to the total difference between successive corneal measurements remained stable pre and post operation, while the combined effect of refractive error correction and optical diameter appeared to have a significant influence on the elevation repeatability in the early stages of the follow up period.
Similar content being viewed by others
Introduction
The cornea contributes approximately two thirds to the total refractive power of the eye1. Recent advances in technology to measure corneal topography are allowing clinicians to better evaluate the cornea and its continuation to ocular refractive power2. Reliable characterisation of corneal topography is critical for the evaluation of visual quality and in several applications including, the planning of refractive surgery3, 4, diagnosis and management of corneal disorders5, 6, and contact lens fitting7, 8. For these applications and for the longitudinal monitoring of progressive corneal conditions, corneal topography measurements available to clinicians should be repeatable.
While Placido disc–based reflective topography can only map the anterior surface of the cornea2. Scheimpflug tomography can measure the elevation data (height) of both the anterior and posterior corneal surfaces. Compared with Placido disc-based systems, the corneal elevation profile can represent the shape of corneal surface more accurately9, and locate the corneal apex post laser in situ keratomileusis (LASIK) more efficiently. Consequently, the Pentacam (which employs Scheimpflug technology) has become a valuable tool for corneal anterior segment analysis, and known for its repeatable anterior and posterior corneal measurements10,11,12. Earlier studies also showed evidence the Pentacam provides repeatable measurements of biometric parameters such as corneal curvature, central corneal thickness and anterior chamber depth (ACD)12,13,14,15,16 in normal corneas.
Keratorefractive surgery, particularly LASIK, has become a commonly used procedure for the correction of myopia. In order to correctly assess the outcome of LASIK, it is important for clinicians to accurately determine corneal topography postoperatively. Erroneous postoperative corneal topography measurements may mislead the clinical decision regarding corneal surgery enhancement17, estimation of intraocular lens power4, 18 and measurement of the intraocular pressure19. In these applications, the high repeatability of topography measurements is essential for ensuring reliability in monitoring changes in corneal shape during surgery follow-up.
Repeatability, or the consistency between readings for the same subject taken on the same instrument under constrained conditions, should be high. Data on repeatability of different videokeratography instruments can be found in the literature16, 20; however, data regarding the repeatability of measurements from a global perspective is scarce. Reliance on point matching methods in earlier studies on three-dimensional (3-D) topography testing is considered a limitation, in which discrete points located in different regions of corneal surface should be picked up to get an overall impression of the topography measurement. Therefore, the present study is designed to compare the repeatability of Pentacam measurements in pre-operative, 1 month and 3 months post-operative eyes using a surface matching method can estimate and correct for the misalignment between successive topography measurements.
Results
The surgery parameters for the 98 eyes included in the study included the optical diameter (OD = 6.58 ± 0.34 mm), residual stromal bed thickness (RSB = 342.09 ± 26.07 μm), and maximum ablation depth (MAD = 95.68 ± 21.62 μm). The measurement results of corneal curvature in the horizontal (Kh) and vertical (K v) directions, the corneal shaper factor in 30 degree (Q30), and central corneal thickness (CCT) are shown in Table 1. Although Kh, K v and CCT decreased and Q30 increased postoperatively than in preoperation (P < 0.05, Table 1), there were no significant differences between successive measurements of these four biometric parameters taken in 3 different periods (Pre, Pos1M and Pos3M) (P > 0.05, Table 1).
Topography match results for the 98 subjects can be seen in Tables 2, 3, 4, 5 and 6. For the anterior corneal surface, the mean differences between successive elevation maps (calculated both before and after misalignment correction using ICP; PreICP-RMS and PosICP-RMS) were significantly higher one month after surgery (Pos1M) and three months after surgery (Pos3M) compared to before surgery (Pre). On the other hand, the misalignment ratio, which describes the weighting of difference between successive measurements caused by misalignment to the total difference remained similar at approximately 0.40 (Tables 2 and 3) in different periods (Pre, Pos1M and Pos3M). For the posterior corneal surface, only PreICP-RMS at Pos3M was statistically significant when compared to Pre. Further, the mean differences between elevation maps (calculated both before and after misalignment correction using ICP; PreICP-RMS and PosICP-RMS) were not statistically significant one month after surgery (Pos1M) compared to both before surgery (Pre) and three months after surgery (Pos3M). The misalignment ratio in posterior corneal surface data at all stages remained constant at approximately 0.23 (Tables 2 and 3).
The area of overlap from the topography matching of successive measurements decreased from Pre to Pos3M, but not between Pre and Pos1M or between Pos1M and Pos3M (Table 3). Most of the rotational and translational misalignment parameters in the Pre stage were different from zero (p < 0.05) except for γ (p = 0.67). However, this was not the case at the Pos1M and Pos3M stages where most of the rotational and translational misalignment parameters were not different from zero (p > 0.05) except for z0 (p < 0.00). Although some misalignment parameters were different from zero, the differences were too small to be considered important in clinical practice. All of the rotational and translational misalignments parameters (x0, y0, z0, α, β, γ) between successive measurements in different periods (Pre, Pos1M and Pos3M) were not significant when compared within each stage (Pre vs Pos1M, Pre vs Pos3M, Pos1M vs Pos3M, P > 0.05) (Table 4). Further, the combined misalignment parameter (CM), which aims to combine the effect of all misalignment components on topography misalignment, was significantly lower in the Pre stage than it was at the Pos1M and Pos3M stages (Table 4).
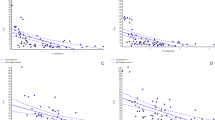
The correlation of PreICP-RMS and PosICP-RMS for both anterior and posterior surfaces with the surgerical parameters and with the spherical equivalent error (SE) in different postoperative periods (Pos1M and Pos3M) are concluded in Table 5. All the PreICP-RMS and PosICP-RMS for the anterior surface were correlated with surgerical parameters and SE in Pos1M, while the correlation decreased in Pos3M. For the posterior surface, all correlations decreased when compared to the anterior surface and none of them was significant. The correlations of OD with PreICP-RMS and PosICP-RMS was much higher than RSB, MAD and SE. OD was statistically correlated with SE (r = 0.688, P = 0.00). However, after correcting for the effects of SE, all correlations decreased and most of them became insignificant (Table 6).
Discussion
The Pentacam utilises a Scheimpflug camera and a monochromatic slit light source, which rotate together around the ocular optical axes to acquire images of the anterior and posterior surfaces of cornea and offer a non-invasive method of obtaining a three-dimensional representation of the anterior segment. Corneal elevation, according to which corneal curvature and pachymetry are calculated, is the primary data obtained by Pentacam. In order to carry out a repeatability analysis of corneal biometric parameters, a large number of points located in the different regions are required to make a comprehensive evaluation20,21,22. In these studies, the repeatability analysis results from different regions are separated and would not provide an overall impression of the whole corneal surface. The present study builds on earlier repeatability assessments and aims to concentrate on the repeatability of the Pentacam in eyes undergoing LASIK surgery.
A common feature of most of the current videokeratography systems is that they are viewer-centred and so their accuracy and reliability will be influenced by fixation lags and eye movements. Topography devices will reject large misalignments or compensate for them during data acquisition13, 23. However, smaller misalignments remain and may be unavoidable. Misalignments of corneal topography measurements can affect estimates of corneal biometric parameters such as corneal curvature, corneal asphericity and corneal thickness.
Overall, the Pentacam measurements in post-LASIK eyes have two possible sources of errors, systematic and random24, and it is difficult to separate their effects. Systematic errors include reduced accuracy in peripheral and posterior corneal regions, and optical distortion caused by aberrations in the Pentacam’s measuring lens, both leading to differences between successive topography measurements. On the other hand, random errors may be caused by an altered corneal refractive index, mistaken detection of stromal interface, variation in magnification ratio of the posterior cornea, stromal haze, change in transparency in the early postoperative cornea, and alterations in shape reconstruction algorithms25,26,27,28. These random errors may alter corneal shape measurements, causing further differences between successive maps and running risks of inappropriate retreatment decisions or misdiagnosis of early iatrogenic keratectasia after LASIK. In this study, the translational and rotational misalignments (x0, y0, z0, α, β, γ) between successive measurements are considered an important, albeit not the only, cause of random errors, and quantified herein when assessing the repeatability of topography maps.
In the post-LASIK stage, the surface analysis was more complex when compared with the more spherical corneas encountered in the pre-operation stage due to the central flattening caused by excimer ablation. The elevation differences (PreICP-RMS) between two succesive measurements increased significantly post-LASIK when compared with pre-operation. The result was similar to previous studies where the repeatability of the Pentacam decreased in eyes with corneal thinning and contour changes after refractive surgery29. However, the significant difference in elevation data should be considered alongside the non-significant differences observed in the corneal biometric parameters obtained before and after LASIK (Table 1).
LASIK corrects refractive errors by reshaping the anterior corneal surface. In the present study, the PreICP-RMS and PosICP-RMS for the anterior corneal surface were correlated with surgerical parameters in Pos1M and Pos3M, but not for the posterior surface (Table 5). The results agreed with the fact that changes in anterior corneal surface (direct surgery effects because of laser ablation) were greater than those in the posterior surface (indirect effects caused by surgical biomechanical effect).
The results further show that the correlations of OD with PreICP-RMS and PosICP-RMS were stronger than for RSB, MAD and SE. However, most correlations of PreICP-RMS and PosICP-RMS with OD, RSB and MAD became non-significant after correcting for the effects of SE. MAD, which is dependent on myopic diopter correction and optic zone diameter, is nomally restricted to be ≤130 μm when considering the safety of the surgery. Therefore, higher myopic diopter correction (or lower negative refractive error) was found to be correlated with smaller optic zone in this research (r = 0.688). It seems that the combined effect of refractive error correction and optical diameter had a greater influence on the repeatability of the Pentacam by affecting the optical quality of the postoperative corneal surface. As reported in a previous study30, smaller optical diameter and more myopic SE correction led to lower postoperative corneal optical quality, possibly reducing the repeatability of Pentacam post-operation. The correlation between RMS and surgerical parameters also decreased from Pos1M to Pos3M, possibly because of the effect of wound healing taking place during the follow-up period. Reports have also been published showing that loss of corneal transparency progressively decreased with time, resulting in improved accuracy of the corneal topography maps31. However, such a finding was not obvious in the current study and a longer follow-up period would be required to confirm it.
The ICP algorithm can provide reliable accuracy for topography matching32, and can quantify and correct for the effects of misalignments between successive maps. Elevation differences of corneal surface between successive measurements decreased significantly after ICP topography matching in the anterior (around 40%) and posterior (around 23%) corneal surfaces, especially in Pos1M and Pos3M. Although the elevation increased significantly post LASIK, the misalignment ratio between PreICP and PosICP remained similar for the anterior (around 0.40) and posterior surface (around 0.23) as shown in Table 2. This result confirmed that regular laser ablation did not increase the difficulty of apex detection, which could have led to increases in the weight ratio. As for the posterior surface, it is expected to be influenced by more error-inducing factors compared to the anterior surface, as discussed above, resulting in a lower misalignment ratio.
Although the difference from zero for several misalignment parameters were statistically significant, pre- and post-LASIK misalignment parameters shown in Table 4 were not large and may not be clinically relevent. The Overlap Area ratio of the corneal surface after topography matching were all above 0.975, and represented an acceptable repeatability of Pentacam both pre and post corneal refractive surgery. Rotational and translational misalignment parameters between successive measurements in different periods (Pre, Pos1M and Pos3M) were also not significant, while the overall CM increased significantly postoperatively. As CM was developed to combine the effects of individual misalignment components, it provided a more reliable assessment of the effects on reliability than considering individual misalignment components and whole data repeatability32.
The present study introduces a new approach to evaluating the repeatability of topography maps based on estimation and elimination of misalignment between successive maps using an ICP algorithm. The ICP algorithm has been a dominant method for registration of 3D free-form surfaces, and was introduced successfully to match topography maps in a rapid process (within 1 to 2 seconds)32,33,34.
The translational and rotational misalignments (x0, y0, z0, α, β, γ) of successive topography measurements were one cause of random errors. Quantified and isolated from random errors, the combined misalignment parameter combined the effects of all individual misalignment components and can be used to assess the effects of misalignment on the repeatability of corneal topography maps. The effect of misalignment on the total difference between successive measurements remained similar pre- and post-operatively. However, corneal refractive surgery decreased the repeatability of corneal topography measurements with higher myopic correction leading to lower repeatability, particularly for the anterior surface, which should be considered to improve reliability of post-surgery refractive assessment. Other factors influencing the repeatability of postoperative topography measurement include the optical diameter while wound healing may have an increasingly importance during the follow-up period of LASIK.
Methods
Study Participants
98 subjects (52 male and 46 female) aged between 17 and 43 years (mean age 23.39 ± 5.25 years) were recruited from myopic patients with spherical equivalent: ranging from −1.75 to −11.13 D (−5.56 ± 1.94 D) and who underwent Femtosecond laser-assisted LASIK treatment in the Refractive Surgery Department of the Eye Hospital, Wenzhou Medical University. All LASIK procedures were performed using the SCHWIND AMARIS platform (SCHWIND eye-tech-solutions, Kleinostheim, Germany). Corneal flaps were created with an LDV femtosecond laser (Ziemer Group, Port, Switzerland). Exclusion criteria included recent contact lens wear (soft contact lens within 2 weeks and rigid contact lens within 4 weeks), ocular disease, systemic disease, intraoperative or postoperative complications (e.g., free flap, reepithelialization) and retreatment. The study followed the tenets of the Declaration of Helsinki and was approved by the Scientific Committee of the Eye Hospital. Signed informed consent was obtained from the subjects after the procedures were explained to them. Patients were followed up for 3 months.
Data Acquisition
The study parameters included refractive error (RE), Kh and K v, Q30, CCT, and corneal elevation data of the anterior and posterior surfaces. RE was measured with a phoroptor (RT-2100, Nidek Inc, Gamagori, Japan)and converted to spherical equivalent, SE. Kh, K v, Q30, CCT and corneal elevation were provided by a Pentacam (OCULUS Optikgerate GmbH, Wetzlar, Germany) in different periods preoperative (Pre), postoperative 1 month (Pos1M) and 3 months (Pos3M). The Pentacam system was operated by a well-trained clinician (LFH) in a dim room in accordance with the manufacturer’s guidelines22, 32. Only data from the right eyes were collected and used in the analysis. Surgery parameters included optical diameter (OD), residual stromal bed thickness (RSB) and maximum ablation depth (MAD), and were recorded based on an operation plan and calculated using the ablation software of SCHWIND AMARIS.
Repeatability Analysis
Topography analysis was carried out using the Iterative Closest Point (ICP) method. Results included the corneal misalignment parameters (translational displacements: x0, y0 and z0, and rotational displacements: α, β and γ), the combined misalignment parameter (CM) and the root mean square (RMS) of the difference in elevation before (PreICP-RMS) and after (PosICP-RMS) the ICP topography matching between successive topography measurements, The results also included the area of overlap between successive maps calculated as described in a previous study32.
Corneal misalignment parameters take the form of rigid-body transformations, where α, β and γ are the spatial extrinsic rotational components around x, y and z axes, respectively, and x0, y0 and z0 represent the translational components along x, y and z axes. Since using six independent misalignment components makes it challenging to have an overall impression of correlation between misalignment and data repeatability, CM was developed to combine their individual effects on data repeatability32. RMS should be zero if the second successive measurements matched perfectly with the first, however, this is unlikely to occur in all cases. Misalignments can only explain part of the RMS between successive maps, and the misalignment ratio calculated in the form (1 - PosICP-RMS/PreICP-RMS) was used to describe the contribution made by misalignment to the overall difference between successive maps.
Statistical analysis
Analysis of variance (ANOVA) was carried out to compare the misalignments parameters, the inter-measurement difference of Kh, K v, Q30 and CCT in different periods (Pre, Pos1M and Pos3M). Commercial software SPSS 20.0 (Chicago, USA) was utilized for all analyses and a two-tailed probability of P < 0.05 was considered statistically significant. The relationship between surgery parameters, SE and the RMS (PreICP and PosICP) were determined by Pearson partial correlation analyses and the Spearman linear correlation factor.
References
Fatt, I. Physiology of the eye: An introduction to the vegetative functions. London: Butterworths, 1–42 (1978).
Klyce, S. D. Computer-assisted corneal topography. High-resolution graphic presentation and analysis of keratoscopy. Invest Ophthalmol Vis Sci 25, 1426–1435 (1984).
Alessio, G., Boscia, F., La Tegola, M. G. & Sborgia, C. Topography-driven excimer laser for the retreatment of decentralized myopic photorefractive keratectomy. Ophthalmology 108, 1695–1703, doi:S0161-6420(01)00706-0 [pii] (2001).
Schuster, A. K. et al. Intraocular lens calculation adjustment after laser refractive surgery using Scheimpflug imaging. J Cataract Refract Surg 42, 226–231, doi:10.1016/j.jcrs.2015.09.024 (2016).
Levy, D. et al. Videokeratographic anomalies in familial keratoconus. Ophthalmology 111, 867–874, doi:10.1016/j.ophtha.2003.12.024 S0161-6420(03)01731-7[pii] (2004).
Luz, A. et al. Enhanced Combined Tomography and Biomechanics Data for Distinguishing Forme Fruste Keratoconus. J Refract Surg 32, 479–494, doi:10.3928/1081597X-20160502-02 (2016).
Bhatoa, N. S., Hau, S. & Ehrlich, D. P. A comparison of a topography-based rigid gas permeable contact lens design with a conventionally fitted lens in patients with keratoconus. Cont Lens Anterior Eye 33, 128–135, doi:10.1016/j.clae.2009.11.004 (2010).
Weber, S. L., Ambrosio, R. Jr., Lipener, C., Coral-Ghanem, C. & Hofling-Lima, A. L. The use of ocular anatomical measurements using a rotating Scheimpflug camera to assist in the Esclera(R) scleral contact lens fitting process. Cont Lens Anterior Eye 39, 148–153, doi:10.1016/j.clae.2015.09.007 (2016).
Belin, M. W. & Khachikian, S. S. An introduction to understanding elevation-based topography: how elevation data are displayed - a review. Clin Experiment Ophthalmol 37, 14–29, doi:10.1111/j.1442-9071.2008.01821.x (2009).
Ciolino, J. B. & Belin, M. W. Changes in the posterior cornea after laser in situ keratomileusis and photorefractive keratectomy. J Cataract Refract Surg 32, 1426–1431, doi:10.1016/j.jcrs.2006.03.037 (2006).
Ha, B. J., Kim, S. W., Kim, S. W., Kim, E. K. & Kim, T. I. Pentacam and Orbscan II Measurements of Posterior Corneal Elevation Before and After Photorefractive Keratectomy. Journal of Refractive Surgery 25, 290–295 (2009).
Kawamorita, T. et al. Repeatability, reproducibility, and agreement characteristics of rotating Scheimpflug photography and scanning-slit corneal topography for corneal power measurement. J Cataract Refract Surg 35, 127–133, doi:10.1016/j.jcrs.2008.10.019 (2009).
Lackner, B., Schmidinger, G. & Skorpik, C. Validity and repeatability of anterior chamber depth measurements with Pentacam and Orbscan. Optom Vis Sci 82, 858–861 (2005).
Chen, D. & Lam, A. K. Intrasession and intersession repeatability of the Pentacam system on posterior corneal assessment in the normal human eye. J Cataract Refract Surg 33, 448–454, doi:10.1016/j.jcrs.2006.11.008 (2007).
Miranda, M. A., Radhakrishnan, H. & O’Donnell, C. Repeatability of corneal thickness measured using an Oculus Pentacam. Optom Vis Sci 86, 266–272, doi:10.1097/OPX.0b013e318196a737 (2009).
Fityo, S., Buhren, J., Shajari, M. & Kohnen, T. Keratometry versus total corneal refractive power: Analysis of measurement repeatability with 5 different devices in normal eyes with low astigmatism. J Cataract Refract Surg 42, 569–576, doi:10.1016/j.jcrs.2015.11.046 (2016).
Iskander, N. G., Peters, N. T., Penno, E. A. & Gimbel, H. V. Postoperative complications in laser in situ keratomileusis. Curr Opin Ophthalmol 11, 273–279 (2000).
Jin, H., Auffarth, G. U., Guo, H. & Zhao, P. Corneal power estimation for intraocular lens power calculation after corneal laser refractive surgery in Chinese eyes. J Cataract Refract Surg 38, 1749–1757, doi:10.1016/j.jcrs.2012.06.048 (2012).
Emara, B. et al. Correlation of intraocular pressure and central corneal thickness in normal myopic eyes and after laser in situ keratomileusis. J Cataract Refract Surg 24, 1320–1325 (1998).
Huang, J. et al. A Comparison between Scheimpflug imaging and optical coherence tomography in measuring corneal thickness. Ophthalmology 120, 1951–1958, doi:10.1016/j.ophtha.2013.02.022 (2013).
Guilbert, E., Saad, A., Grise-Dulac, A. & Gatinel, D. Corneal thickness, curvature, and elevation readings in normal corneas: combined Placido-Scheimpflug system versus combined Placido-scanning-slit system. J Cataract Refract Surg 38, 1198–1206, doi:10.1016/j.jcrs.2012.01.033 (2012).
Bao, F. et al. Evaluation of the shape symmetry of bilateral normal corneas in a Chinese population. PLoS One 8, e73412, doi:10.1371/journal.pone.0073412 (2013).
Buehl, W., Stojanac, D., Sacu, S., Drexler, W. & Findl, O. Comparison of three methods of measuring corneal thickness and anterior chamber depth. Am J Ophthalmol 141, 7–12, doi:10.1016/j.ajo.2005.08.048 (2006).
Bland, M. An Introduction to Medical Statistics. 3rd ed. Oxford. UK: Oxford University Press 2000, 268–275.
Iskander, N. G., Anderson Penno, E., Peters, N. T., Gimbel, H. V. & Ferensowicz, M. Accuracy of Orbscan pachymetry measurements and DHG ultrasound pachymetry in primary laser in situ keratomileusis and LASIK enhancement procedures. J Cataract Refract Surg 27, 681–685 (2001).
Nawa, Y., Masuda, K., Ueda, T., Hara, Y. & Uozato, H. Evaluation of apparent ectasia of the posterior surface of the cornea after keratorefractive surgery. J Cataract Refract Surg 31, 571–573, doi:10.1016/j.jcrs.2004.05.050 (2005).
Boscia, F., La Tegola, M. G., Alessio, G. & Sborgia, C. Accuracy of Orbscan optical pachymetry in corneas with haze. J Cataract Refract Surg 28, 253–258 (2002).
Lopez-Miguel, A., Nieto, J. C., Diez-Cuenca, M., Pinero, D. P. & Maldonado, M. J. Agreement of non-contact pachymetry after LASIK: comparison of combined scanning-slit/Placido disc topography and specular microscopy. Eye (Lond) 24, 1064–1070, doi:10.1038/eye.2009.233 (2010).
Xu, Z. et al. Reliability of Pentacam HR Thickness Maps of the Entire Cornea in Normal, Post-Laser In Situ Keratomileusis, and Keratoconus Eyes. Am J Ophthalmol 162, 74–82 e71, doi:10.1016/j.ajo.2015.11.008 (2016).
Pop, M. & Payette, Y. Risk factors for night vision complaints after LASIK for myopia. Ophthalmology 111, 3–10, doi:10.1016/j.ophtha.2003.09.022 (2004).
Prisant, O., Calderon, N., Chastang, P., Gatinel, D. & Hoang-Xuan, T. Reliability of pachymetric measurements using Orbscan after excimer refractive surgery. Ophthalmology 110, 511–515 (2003).
Bao, F. et al. Effect of Misalignment between Successive Corneal Videokeratography Maps on the Repeatability of Topography Data. PLoS One 10, e0139541 (2015).
Yang, C. & Gérard, M. Object modelling by registration of multiple range images. Image and Vision Computing 10, 145–155 (1992).
Paul, J. B. & Neil, D. M. Method for registration of 3-D shapes. IEEE Transactions on Pattern Analysis and Machine Intelligence 14, 239–256 (1992).
Acknowledgements
This study was supported by the Natural Science Foundation of Zhejiang Province (LY16H120005), Scientific Research Project of Zhejiang Provincial Department of Education (Y201534199), Projects of medical and health technology development program in ZheJiang Province (2016ZHB012), the Science Foundation of the Affiliated Eye Hospital of Wenzhou Medical University (YNZD201501, YNCX201405) and the National Natural Science Foundation of China (81300807, 81600712).
Author information
Authors and Affiliations
Contributions
X.B.Z. and W.H.Y., S.C., Y.P.Z.: analyzed data and drafted the manuscript. J.J.W. and B.G.: analyzed data and revised the draft. L.F.H., captured the elevation images of corneal surface and analyzed the data. F.J.B.: designed the experiment, built initial constructs, analyzed data, proposed the idea and supervised the project. Q.M.W. and A.E.: revised the draft, proposed the idea and supervised the project. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zheng, X., Yang, W., Huang, L. et al. Evaluating the repeatability of corneal elevation through calculating the misalignment between Successive topography measurements during the follow up of LASIK. Sci Rep 7, 3122 (2017). https://doi.org/10.1038/s41598-017-03223-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03223-9
This article is cited by
-
Repeatability of corneal elevation maps in keratoconus patients using the tomography matching method
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.