Abstract
High tumor expression of epidermal growth factor-like domain 7 (EGFL7) has been associated with a poor prognosis in colorectal cancer. The aim of the current study was to investigate the possible prognostic impact of circulating EGFL7 (cir-EGFL7), combined with single nucleotide polymorphism (SNP) analyses, in patients with metastatic colorectal cancer (mCRC) treated with first line chemotherapy and bevacizumab. A total of 88 patients were included. Serum was collected prior to treatment initiation, at first evaluation after 3 weeks, and at progression. Cir-EGFL7 was analysed by the enzyme-linked immunosorbent assay (ELISA) technique. The SNPs were analysed by real-time qPCR based on DNA from whole blood. Endpoints were response rate (RR), progression free survival (PFS), and overall survival (OS). Cir-EGFL7 decreases after administration of chemotherapy plus bevacizumab. Baseline levels of cir-EGFL7 were significantly related to PFS and OS, p = 0.0431 and p = 0.0017, respectively, with increasing cir-EGFL7 levels associated with a worse prognosis. Circulating EGFL7 was not associated with RR. The SNP analyses revealed a significant relationship between rs1051851 and OS, p = 0.030. This study demonstrates that cir-EGFL7 changes during treatment with chemotherapy plus bevacizumab and that baseline levels and genetic variations may influence the overall prognosis of patients with mCRC. The findings call for further validation.
Similar content being viewed by others
Introduction
Patients diagnosed with metastatic colorectal cancer (mCRC) have a poor prognosis. Recent years, however, have witnessed an increase in median overall survival (OS) beyond two years as recently demonstrated in the TRIBE study1. This may, among other reasons, be attributable to individualized treatment strategies aiming at optimal benefit of all available treatment modalities in every line of treatment. Despite the recent increase in OS, the benefit from first line treatment alone has not changed over the same period calling for increased focus on upfront treatment strategies.
Targeting angiogenesis has been a standard treatment modality in mCRC over a decade and new anti-angiogenic drugs are approved every year. While the understanding of the molecular sub-classification of colorectal cancer (CRC) is improving, the field of anti-angiogenic treatments is still characterized by the lack of validated biomarkers.
In contrast to normal blood vessels, the endothelial cells (ECs) of tumor associated blood vessels are highly active and contribute to the shedding of cell components into the circulation, including pro-angiogenic factors2. This could reflect tumor load in general and may change during the course of treatment. We have previously shown that changes in the levels of EC specific microRNA-126 (miRNA-126) during treatment may be predictive as to benefit of first line chemotherapy and bevacizumab in patients with mCRC3. MicroRNA-126 is transcribed from the epidermal growth factor-like domain 7 (EGFL7) gene4, and the EGFL7 protein is secreted by activated ECs, a process almost non-existing in normal quiescent blood vessels5,6,7,8. In the extracellular matrix, EGFL7 supports EC adhesion and migration7, 9, protects the ECs from apoptosis10, and is important for tube formation7 and guiding of endothelial sprouts9. Recent studies have suggested a relationship between efficacy of first line treatment and tumor expression of EGFL711, 12, but the role of circulating EGFL7 (cir-EGFL7) in this context has so far not been explored. The possible influence of variations in the EGFL7 gene also calls for elucidation.
The aim of the current study was to investigate the possible prognostic impact of cir-EGFL7, combined with single nucleotide polymorphism (SNP) analyses, in patients with mCRC treated with first line chemotherapy and bevacizumab.
Results
Patient characteristics
The main patient characteristics of the included 88 patients are summarised in Table 1. At the time of cir-EGFL7 analysis, i.e. at a median follow-up of 28.9 months, the median progression free survival (PFS) was 7.6 months (95% confidence interval (CI): 7.0–9.2 months), whereas the median OS was 20.9 months (95% CI: 18.4–23.8).
Circulating epidermal growth factor-like domain 7
Treatment with chemotherapy plus bevacizumab resulted in a significant reduction in the cir-EGFL7 levels. The median concentration at baseline was 269 ng/ml (95% CI: 170–396), at the first assessment after three weeks it was 171 ng/ml (95% CI: 118–212), and later on changes were rather modest up to the progression level of 130 ng/ml (95% CI: 101–182), p = 0.003. Dividing the patients into three groups (tertiles) according to baseline levels revealed that decreasing cir-EGFL7 during treatment was primarily a characteristic of the patients with high baseline levels (Fig. 1). Baseline cir-EGFL7 was significantly lower in patients who had undergone primary tumor resection 136 ng/ml (95% CI: 86–227) compared to those with the primary tumor in situ 504 ng/ml (95% CI: 203–872), p = 0.0001. The same applies to patients with a rectal cancer compared to colon cancer (p = 0.0108), and the 15 patients that underwent R0 resection after treatment initiation compared to those who did not (p = 0.0114, Supplementary Table 1). Cir-EGFL7 was not related to RAS/RAF status (p = 0.56, Supplementary Table 1). Addressing liver limited disease only, the potential candidates for R0 resection showed a similar association with a median EGFL7 of 117 ng/ml (95% CI: 68–227) in patients who underwent resection later compared to 400 ng/ml (95% CI: 159–872) in those remaining unresectable, p = 0.014.
Median circulating epidermal growth factor-like domain 7 (cir-EGFL7) according to baseline levels (lowest third, intermediate third, and highest third) at baseline, first evaluation, and progression. Horizontal lines mark the respective upper and lower limits of the 95% confidence intervals (CI). The upper limit (2003 ng/ml) of the 95% CI for the high cir-EGFL7 levels at baseline is censored for graphical reasons, but not from the analyses. The broken time line between first evaluation and progression indicates that this time period varies between the patients. The differences between the medians for the low, intermediate, and high groups were significant at baseline and at first evaluation but not at time of progression (p < 0.05).
Neither the baseline level of cir-EGFL7 nor its dynamics during treatment was related to treatment response (Supplementary Table 2). When grouped according to level, baseline cir-EGFL7 demonstrated a non-significant relationship with PFS in the log rank test as illustrated in Fig. 2a, whereas the Cox regression analysis indicated a significantly worse PFS of patients with a high baseline level (Table 2).
Impaired OS was demonstrated of patients with high baseline cir-EGFL7 (Fig. 2b); an association that remained significant after a multiple Cox regression analysis, hazard ratio 2.0331 (95% CI: 1.0077–4.1019), p = 0.0476 (Table 3).
Epidermal growth factor-like domain 7 single nucleotide polymorphisms
The distribution of genotypes in the five analyzed SNPs followed the Hardy-Weinberg equilibrium (Supplementary Table 3). There were no significant relationships between genotype distributions and cir-EGFL7 (Supplementary Table 4).
The response rate of patients harboring the CT genotype of the rs4880118 SNP was significantly higher than the patients with the CC genotype, 10/13 = 77% and 31/70 = 44%, p = 0.038. This relationship, however, did not translate into a significant difference in PFS (Table 4).
The genotype distribution in the rs1051851 SNP demonstrated a significant relationship with OS (p = 0.03) (Table 4).
Discussion
Recent studies have indicated that high tumor expression levels of EGFL7 may be associated with poor prognosis in several different malignancies12,13,14,15,16. Furthermore, we have previously shown a relationship between high expression levels of EGFL7 in CRC tissue and reduced response rate (RR) in the metastatic setting11, 12, and antibodies targeting EGFL7 have demonstrated efficacy in early phases of clinical testing17. In order to further characterize the clinical value of EGFL7 it is necessary to address it in the circulation and investigate how this pro-angiogenic protein is influenced by disease and treatment.
The present study demonstrated a relationship between high levels of cir-EGFL7 at baseline and poor PFS and OS for patients with mCRC treated with first line chemotherapy and bevacizumab. To the best of our knowledge the study by Fan et al. is the only previous study in which EGFL7 has been analysed in blood samples from patients with CRC13. They demonstrated an elevated median EGFL7 concentration in serum from patients with different cancers, among these 64 patients with CRC, compared to a reference cohort of healthy donors. The possible association with clinical outcome was not addressed in their study. A publication from 2015 by Liu et al. demonstrated significantly higher serum levels of EGFL7 in patients with hepatocellular carcinomas compared to healthy donors18. Both studies thus demonstrated elevated cir-EGFL7 in the presence of cancer. The results of the present study are in line with previous tissue-based studies, emphasizing the prognostic disadvantage of high EGFL7 levels, while simultaneously demonstrating this relationship to be accessible through the analysis of blood samples. This approach holds important advantages compared to tissue analysis, including easier sampling and the avoidance of tumor heterogeneity. In regard to the survival analyses, one may argue that the censoring of PFS data from 15 out of 88 patients is problematic. However, since the censored patients are expected to be at lower risk of progression (limited disease and resected) than the remaining patients in the analyses, and given the fact that the majority of the censored patients are from the low (N = 8) and middle (N = 5) EGFL7 groups (baseline), the true difference in PFS based on EGFL7 base-line levels is likely to be bigger19 than the one illustrated in the present analyses.
Given this association with PFS and OS, and the similar findings in other malignancies, the lack of relationship with treatment efficacy seems rather surprising. This is especially the case considering our previous studies demonstrating a relationship between RR and EGFL7 tumor tissue expression levels11, 12. In addition to multiple methodological differences (formalin fixed paraffin embedded tissue versus serum, immunohistochemistry versus enzyme-linked immunosorbent assay (ELISA), subjective/semi-quantitative versus quantitative assessment, etc.) the angiogenic activity assessed by EGFL7 in situ may simply provide a better estimate of tumor responsiveness. Such a composite tumor estimate provides both quantitative information about the blood vessel area and functional input as to the multiple angiogenic processes modulated by EGFL7, e.g. blood vessel maturity that may be linked to chemotherapy uptake20. In contrast, cir-EGFL7 is more likely to reflect the overall state of activated tumor angiogenesis from the entire tumor burden in the patient. Upon treatment initiation, which especially targets immature blood vessels, this burden, and its ability to secrete EGFL7, decreases without necessarily providing specific information as to the delivery/vulnerability of the individual tumors in the patient. Upon treatment resistance, these patients may experience tumor regrowth to a larger extent (multiple sites), which may explain the association with OS (intrinsic treatment resistance).
A number of clinical observations from the present study deserve to be discussed in further detail.
First of all it was interesting, that baseline cir-EGFL7 levels of potentially resectable patients were guiding as to later resectability. Patients who underwent resection later during their treatment course presented with significantly lower baseline values compared to the patients that was not resected. In support of this observation are the results presented by Shen et al. in a study, where EGFL7 was analyzed in serum from 112 patients with pancreatic cancer21. In this study EGFL7 was lower in resectable patients compared to the non-resectable and in patients who underwent resection EGFL7 dropped significantly postoperatively. These observations, of course, needs to be investigated in suitable settings, but the similarities between the results supports their plausibility and the idea of a molecular biomarker instrumental in the upfront selection of patients for intensive treatment is of high clinical relevance.
A second observation concerns tumor load in general. It appears that the initial tumor burden seems to influence the steady state levels of cir-EGFL7, i.e. primary tumor resected or not. Patients with the primary tumor in situ presented with significantly higher levels of cir-EGFL7 (approximately 4 fold) than those who had previously undergone tumor resection. This corresponds rather well with basic angiogenic knowledge stating that tumor associated ECs are highly activated, leaky, and release high levels of pro-angiogenic proteins such as EGFL72 as compared to the remaining vascular network, where EGFL7 expression is rather limited in the quiescent ECs5.
The third point to be highlighted is in regard to the dynamics of cir-EGFL7. Overall, cir-EGFL7 dropped after initiation of therapy but was maintained at low levels during treatment until progression, suggesting that the acquired treatment resistance to some extent may be EGFL7 independent. This scenario is similar to what has previously been shown for vascular endothelial growth factor A (VEGF-A) during bevacizumab treatment22. This specific observation may be highly relevant considering the future possibility of adding anti-EGFL7 antibodies to the treatment regimens, as such a step needs to be guided by the fluctuation of relevant biomarkers, such as cir-EGFL7.
Turning to the genomics, the EGFL7 associated SNPs analyzed in the present study did not demonstrate any evidence of functionality in regard to cir-EGFL7 levels. The rs4880118 SNP demonstrated a significant relationship with RR, but this difference was not translated to a difference in PFS and hence, the clinical importance of this observation is uncertain. A significant difference in OS was observed when addressing the rs1051851 SNP. However, based on the genotypes it was not clear whether the A- or G-allele determined the survival advantage. These results call for further assessment and validation in larger cohorts in order to determine the potential clinical impact. In 2013, Li et al. presented an abstract at the ASCO Annual Meeting (J Clin Oncol 31, 2013 (suppl; abstr 3565)) arguing for a relationship between the EGFL7 rs1051851 SNP and RR from a pooled cohort of 455 patients with mCRC treated with first line FOLFIRI and bevacizumab, but the original article containing these observations does not seem to have been published, yet. The lack of obvious relationships between the investigated SNPs and treatment outcome was the main reason for not exploring possible associations with underlying haplotypes in the EGFL7 gene.
In reference to previously published data on this cohort12 we found no relationship between tumor expression of EGFL7 and the present cir-EGFL7 data. These comparisons across data furthermore indicate that tumors from patients with the rs9411215 GG genotype presented with a lower EGFL7 tumor expression but this is based on a rather small subsample (N = 40).
In conclusion, this exploratory investigation demonstrates that cir-EGFL7 decreases after the first administration of chemotherapy plus bevacizumab, and how that the baseline level of this angiogenic parameter is of prognostic importance in patients with mCRC. These findings along with the possible influence of the rs1051851 SNP on OS call for further validation.
Methods
Reporting in this study is in accordance with the REMARK23 and BRISQUE24 criteria. The analysing of angiogenesis related SNPs and proteins was pre-specified in the study protocol.
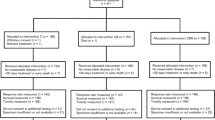
Study population
This study prospectively included 88 patients between March 2010 and October 2013 with histologically verified mCRC deemed unresectable at baseline, measurable disease according to the Response Evaluation Criteria In Solid Tumours (RECIST 1.1)25, and planned for first line chemotherapy combined with bevacizumab. Patients having completed adjuvant chemotherapy more than 6 months before enrolment were accepted. All patients were older than 18 years and presented with normal hepatic, renal, and bone marrow function. Previous malignancies diagnosed within 5 years (except non-melanoma skin cancer and carcinoma in situ of the cervical uterus) were exclusion criteria. All data were recorded according to good clinical practice. The study was approved by the Regional Scientific Ethical Committee (S-20100005) of Southern Denmark and the Danish Data Protection Agency and all methods were performed in accordance with relevant guidelines and regulations. Written informed consent was obtained from all patients enrolled in the study.
Treatment and evaluation
Treatment consisted of capecitabine 1000 mg/m2 twice daily on days 1 through 14 (28 doses) in a 21-day cycle, and oxaliplatin 130 mg/m2 as a 2-hour intravenous infusion on day 1. Bevacizumab was given as an infusion (7.5 mg/kg) on day 1 of each treatment cycle. Treatment continued until disease progression or unacceptable toxicity, but treatment-free intervals were accepted after six cycles, if requested by the patient. Response evaluation was based on clinical and radiologic examination using CT scans of the chest and abdomen every 9 weeks and assessed according to the RECIST 1.1 criteria25. Responding patients were classified as having complete response (CR) or partial response (PR), while non-responding patients were classified as stable disease (SD) or progressive disease (PD).
Sampling
Sampling of peripheral blood was carried out at baseline before treatment initiation (serum and whole blood) and then 3-weekly at each clinical evaluation (serum) until progression. To improve comparability, three samples were chosen for the present study (baseline, first clinical evaluation, and progression). The first two were available for analysis from all 88 patients and the sample at progression from 74 patients (84%).
Venous blood, drawn from the antecubital area and collected in 6 ml dry glass, was left for a minimum of 30 min. for a clot to form, spun down for 10 min. at 2500 g, and serum was transferred to Greiner tubes (SIGMA-ALDRICH, USA) and frozen at −80 °C. Blood intended for SNP analyses was collected in 3 ml EDTA tubes and frozen immediately at −80 °C. The median storage time from sampling to analysis was 2.4 years. Samples were transported on ice from storage to analysis.
Protein analyses
A sandwich enzyme-linked immunosorbent assay (Cloud-Clone Corp., SEL643Hu, Houston, TX, USA) was used to quantify EGFL7 in serum. Analysis was performed according to the manufacturer’s protocol. In brief, 100 µl of standard or sample was added to each well of a 96-well strip plate, pre-coated with an antibody specific to EGFL7, and incubated for 2 hours at 37 °C. Aspiration was followed by addition of detection reagent A, incubation for one hour at 37 °C, aspiration and three times washing. This step was repeated for detection reagent B with 30 minutes of incubation and five washes. Then substrate solution was added, incubated for 15 minutes at 37 °C, followed by addition of stopping solution and read at 450 nm. Concentrations of EGFL7 were assessed through comparisons with the standard curve and multiplied with the initial dilution factor (4 fold). Samples with concentrations above the standard curve were diluted further (and multiplied accordingly).
All samples were assayed in duplicate and the average was used for comparison with clinical data. The total in-house analytical coefficients of variation (CV) at two levels were 19.2% (high) and 23.4% (low). This is considered acceptable in reference to a study population (interpatient) CV of 95%. All protein concentrations are expressed in ng/ml.
EGFL7 genotyping
We decided to analyse SNPs in the EGFL7 gene region in order to test for possible functional influence on EGFL7 protein levels and for possible associations with clinical outcome. The selection of SNPs was based on a tagging SNP strategy aiming for a broad coverage of the EGFL7 gene region, while simultaneously ensuring a sufficient frequency of the rare allele in the selected SNPs. Based on this, five SNPs were chosen for analyses (Supplementary Fig. 1).
Germline DNA was isolated from whole blood by the Maxwell® method according to the user manual (Promega Corporation, WI, USA) (http://www.promega.com/tbs/tm284/tm284.pdf). Genotyping was performed by PCR analysis using the ABI PRISM 7900 HT fast real-time PCR system (Applied Biosystem, Foster City, CA, USA). Commercial assays functionally tested and validated (LifeTechnologies, Carlsbad, CA, USA) were used. Assay numbers are listed in Supplementary Figure 1. The analysis was performed as previously described26. Genotyping was not possible in two patients due to an insufficient amount of DNA. All other samples met the quality value threshold of 98%. Blood samples blinded to patient outcome were successfully processed and analysed at the same institution (Vejle Hospital, Denmark).
Statistics
We report median values with a 95% confidence interval (CI). The Wilcoxon rank sum test was used for comparison of median values. Fisher’s exact test was used for comparison between categorical parameters, while chi-square statistics were used to test for Hardy-Weinberg equilibrium. Survival functions were estimated by log rank tests and illustrated by the Kaplan-Meier method. Simple Cox regression analysis was used to estimate the hazard ratio of individual potential prognostic variables, and variables with p-values below 0.1 were included in multiple Cox regression analyses. Progression free survival was defined as the time from start of treatment until the first documented tumor progression or death from any cause. The PFS data were censored in 15 cases due to liver resection (N = 14) and radio frequency ablation (N = 1) for liver metastases. Data were censored from the day of the intervention, meaning that these patients contributed with “time” until their respective dates of intervention and the interventions did not count as an “event” in the Cox regression analyses. Overall survival was defined as the time from start of treatment until death of any cause. Adjustment for multiple comparisons was not made. All patients were successfully followed until progression. A two-sided 0.05 significance level was used in all statistical tests. Statistical calculations were carried out using the NCSS statistical software (NCSS Statistical Software, Kaysville, UT 84037, USA, version 2007). P values < 0.05 were considered significant, and all tests were two-sided.
References
Loupakis, F. et al. Initial therapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer. N Engl J Med 371, 1609–1618, doi:10.1056/NEJMoa1403108 (2014).
Nikolic, I. et al. EGFL7 ligates alphavbeta3 integrin to enhance vessel formation. Blood 121, 3041–3050, doi:10.1182/blood-2011-11-394882 (2013).
Hansen, T. F., Carlsen, A. L., Heegaard, N. H., Sorensen, F. B. & Jakobsen, A. Changes in circulating microRNA-126 during treatment with chemotherapy and bevacizumab predicts treatment response in patients with metastatic colorectal cancer. Br J Cancer 112, 624–629, doi:10.1038/bjc.2014.652 (2015).
Meister, J. & Schmidt, M. H. miR-126 and miR-126*: new players in cancer. Scientific World Journal 10, 2090–2100, doi:10.1100/tsw.2010.198 (2010).
Campagnolo, L. et al. EGFL7 is a chemoattractant for endothelial cells and is up-regulated in angiogenesis and arterial injury. Am J Pathol 167, 275–284, doi:10.1016/S0002-9440(10)62972-0 (2005).
Fitch, M. J., Campagnolo, L., Kuhnert, F. & Stuhlmann, H. Egfl7, a novel epidermal growth factor-domain gene expressed in endothelial cells. Dev Dyn 230, 316–324, doi:10.1002/dvdy.20063 (2004).
Parker, L. H. et al. The endothelial-cell-derived secreted factor Egfl7 regulates vascular tube formation. Nature 428, 754–758, doi:10.1038/nature02416 (2004).
Soncin, F. et al. VE-statin, an endothelial repressor of smooth muscle cell migration. EMBO J 22, 5700–5711, doi:10.1093/emboj/cdg549 (2003).
Schmidt, M. et al. EGFL7 regulates the collective migration of endothelial cells by restricting their spatial distribution. Development 134, 2913–2923, doi:10.1242/dev.002576 (2007).
Xu, D., Perez, R. E., Ekekezie, I. I., Navarro, A. & Truog, W. E. Epidermal growth factor-like domain 7 protects endothelial cells from hyperoxia-induced cell death. Am J Physiol Lung Cell Mol Physiol 294, 17–23, doi:10.1152/ajplung.00178.2007 (2008).
Hansen, T. F. et al. MicroRNA-126 and epidermal growth factor-like domain 7-an angiogenic couple of importance in metastatic colorectal cancer. Results from the Nordic ACT trial. Br J Cancer 109, 1243–1251, doi:10.1038/bjc.2013.448 (2013).
Hansen, T. F., Nielsen, B. S., Sorensen, F. B., Johnsson, A. & Jakobsen, A. Epidermal growth factor-like domain 7 predicts response to first-line chemotherapy and bevacizumab in patients with metastatic colorectal cancer. Mol Cancer Ther 13, 2238–2245, doi:10.1158/1535-7163.MCT-14-0131 (2014).
Fan, C. et al. The expression of Egfl7 in human normal tissues and epithelial tumors. Int J Biol Markers 28, 71–83, doi:10.5301/JBM.2013.10568 (2013).
Li, J. J., Yang, X. M., Wang, S. H. & Tang, Q. L. Prognostic role of epidermal growth factor-like domain 7 protein xpression in laryngeal squamous cell carcinoma. J Laryngol Otol 125, 1152–1157, doi:10.1017/S0022215111002441 (2011).
Oh, J. et al. High expression of epidermal growth factor-like domain 7 is correlated with poor differentiation and poor prognosis in patients with epithelial ovarian cancer. J Gynecol Oncol 25, 334–341, doi:10.3802/jgo.2014.25.4.334 (2014).
Zhou, L. et al. Prognostic significance of epidermal growth factor-like domain 7 in pancreatic cancer. Hepatobiliary Pancreat Dis Int 13, 523–528, doi:10.1016/S1499-3872(14)60272-1 (2014).
Johnson, L. et al. Anti-EGFL7 antibodies enhance stress-induced endothelial cell death and anti-VEGF efficacy. J Clin Invest 123, 3997–4009, doi:10.1172/JCI67892 (2013).
Liu, X. J. et al. Multivariate analysis of molecular markers in peripheral blood associated with recurrence and metastasis of hepatocellular carcinoma. Genet Mol Res 14, 1502–1507, doi:10.4238/2015.February.20.5 (2015).
Campigotto, F. & Weller, E. Impact of informative censoring on the Kaplan-Meier estimate of progression-free survival in phase II clinical trials. J Clin Oncol 32, 3068–3074, doi:10.1200/JCO.2014.55.6340 (2014).
Jain, R. K. Normalizing tumor microenvironment to treat cancer: bench to bedside to biomarkers. J Clin Oncol 31, 2205–2218, doi:10.1200/JCO.2012.46.3653 (2013).
Shen, X. et al. Epidermal growth factor-like domain 7 promotes cell invasion and angiogenesis in pancreatic carcinoma. Biomed Pharmacother 77, 167–175, doi:10.1016/j.biopha.2015.12.009 (2016).
Loupakis, F. et al. Pharmacodynamic and pharmacogenetic angiogenesis-related markers of first-line FOLFOXIRI plus bevacizumab schedule in metastatic colorectal cancer. Br J Cancer 104, 1262–1269, doi:10.1038/bjc.2011.85 (2011).
McShane, L. M. et al. REporting recommendations for tumour MARKer prognostic studies (REMARK). Br J Cancer 93, 387–391, doi:10.1038/sj.bjc.6602678 (2005).
Moore, H. M. et al. Biospecimen reporting for improved study quality (BRISQ). Cancer Cytopathol 119, 92–101, doi:10.1002/cncy.v119.2 (2011).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45, 228–247, doi:10.1016/j.ejca.2008.10.026 (2009).
Hansen, T. F. et al. The predictive value of single nucleotide polymorphisms in the VEGF system to the efficacy of first-line treatment with bevacizumab plus chemotherapy in patients with metastatic colorectal cancer: Results from the Nordic ACT trial. Int J Colorectal Dis 27, 715–720, doi:10.1007/s00384-011-1382-6 (2012).
Acknowledgements
We are very thankful for the technical assistance provided by Camilla Davidsen and Lone Frischknecht and for the linguistic editing provided by Karin Larsen. This study was supported by The Cancer Foundation, The Danish Council for Independent Research, and the Regional Strategic Council for Research in the Region of Southern Denmark, none of which had any influence on any part of the study.
Author information
Authors and Affiliations
Contributions
T.F.H., F.B.S., and A.J. conceived and designed the experiments. T.F.H. performed statistical analyses of the data and wrote the manuscript. R.F.A. performed the genotype analyses and D.A.O. performed the protein analyses. F.B.S. revised all histological samples to ensure diagnoses and eligibility. A.J. supervised the project. All authors discussed the results, commented, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hansen, T.F., Andersen, R.F., Olsen, D.A. et al. Prognostic importance of circulating epidermal growth factor-like domain 7 in patients with metastatic colorectal cancer treated with chemotherapy and bevacizumab. Sci Rep 7, 2388 (2017). https://doi.org/10.1038/s41598-017-02538-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-02538-x
This article is cited by
-
Low EGFL7 expression is associated with high lymph node spread and invasion of lymphatic vessels in colorectal cancer
Scientific Reports (2023)
-
Serum epidermal growth factor-like domain 7 serves as a novel diagnostic marker for early hepatocellular carcinoma
BMC Cancer (2021)
-
EGFL7 as a novel therapeutic candidate regulates cell invasion and anoikis in colorectal cancer through PI3K/AKT signaling pathway
International Journal of Clinical Oncology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.