Abstract
Gout is caused by hyperuricemia, with alcohol consumption being an established risk factor. Alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) are crucial enzymes for alcohol metabolism. We recently performed a genome-wide association study of gout and a subsequent fine-mapping study which identified rs671 of ALDH2 as a gout locus. However, the association between gout and common variants of ADH1B has hitherto remained unreported, prompting us to investigate the association between gout and common dysfunctional variants of ADH1B (rs1229984) and ALDH2 (rs671). We used 1,048 clinically defined gout cases and 1,334 controls of Japanese male. The “His carrier” (His/His or His/Arg) of rs1229984 (His48Arg) of ADH1B significantly increased gout risk (P = 4.3 × 10−4, odds ratio = 1.76), as did the “non-Lys carrier (Glu/Glu)” of rs671 (Glu504Lys) of ALDH2. Furthermore, common variants of ADH1B and ALDH2 are independently associated with gout. Our findings likewise suggest that genotyping these variants can be useful for the evaluation of gout risk.
Similar content being viewed by others
Introduction
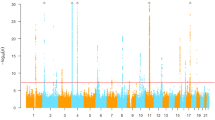
Gout is an increasingly common disease resulting from hyperuricemia, which causes acute arthritis. Several genes have been reported to be associated with gout1,2,3,4,5. Some urate transporter genes, such as ABCG2 6,7,8, SLC2A9 3, 4, SLC17A1 3, 9 and SLC22A12 10, have major effects on the progression of gout/hyperuricemia. Certain environmental factors appear also to be risk factors for gout/hyperuricemia, of which alcohol consumption is one of the best known. Ethanol is oxidized to acetaldehyde by alcohol dehydrogenase (ADH), and acetaldehyde is further metabolized to acetate by aldehyde dehydrogenase (ALDH)11. These processes crucially depend on ADH1B and ALDH2, respectively (Fig. 1). We recently performed a genome-wide association study (GWAS) of gout4 followed by a fine-mapping study12 that identified rs671 (Glu504Lys) of ALDH2 as a gout locus12. On the other hand, to our knowledge, the association between gout and common variants of ADH1B has not hitherto been reported. Additionally, there are no association analysis reports between gout and common variants of ADH1B and ALDH2 that include adjustment for alcohol consumption. We therefore performed an association analysis between gout and a common dysfunctional variant of ADH1B, rs1229984 (His48Arg). We further investigated the effects of alcohol consumption on the association between gout and common variants of ADH1B and ALDH2.
Ethanol oxidization by ADH and ALDH. Ethanol is oxidized to acetaldehyde by alcohol dehydrogenase (ADH), and acetaldehyde is further metabolized to acetate by aldehyde dehydrogenase (ALDH). These oxidization activities largely depend on ADH1B and ALDH2, respectively. The enzymatic activities of ADH1B and ALDH2 depend on common dysfunctional variants, rs1229984 (His48Arg) and rs671 (Glu504Lys) in East Asians, respectively. The A/A (His/His) or A/G (His/Arg) genotype of rs1229984 has been reported to produce 40-fold faster ethanol oxidation by ADH1B than the G/G (Arg/Arg) genotype. Individuals with heterozygotes (Lys/Glu) of rs671 have only 6.25% of the enzyme activity of those with normal ALDH2 (Glu/Glu), and those with homozygotes (Lys/Lys) show almost no activity. Therefore, the Lys carrier of ALDH2 metabolizes acetaldehyde more slowly than the non-Lys carrier, resulting in acetaldehyde accumulation.
Results
Association analysis between gout and common variants of ADH1B and ALDH2
We performed genotyping of rs1229984 (His48Arg) of ADH1B using 1,048 clinically defined gout cases and 1,334 controls of Japanese male (Table 1). The results are shown in Table 2 and Supplementary Table S1. The call rate for rs1229984 was 98.4%: this variant in the control group was in Hardy-Weinberg equilibrium (P > 0.05). The common dysfunctional variant of ADH1B, rs1229984, showed a significant association with gout for each allele model (P = 0.037; odds ratio [OR] = 1.16; 95% confidence interval [CI]: 1.01–1.34; Table 2). As shown in Supplementary Table S1, A/G (His/Arg) and A/A (His/His) genotypes significantly increase the risk of gout (P = 0.020 and 7.3 × 10−3; OR = 1.69 and 1.80, respectively) as compared with the G/G (Arg/Arg) genotype; however, there is no significant difference in effect sizes on gout between A/G (His/Arg) and A/A (His/His) genotypes (P = 0.51), and the OR is close to 1.00 (OR = 0.94; 95% CI: 0.79–1.12). Based on these results and enzyme activity13,14,15, we also performed an association analysis in the “His carrier (His/His or His/Arg)” (high tolerance for alcohol) vs. “non-His carrier (Arg/Arg)” (low tolerance for alcohol) model. Our results showed that the presence of “His carrier” significantly increased the risk of gout (P = 4.3 × 10−4; OR = 1.76; 95% CI: 1.15–2.69; Table 3). In addition, although not significant, the “A” allele (His) of ADH1B tended to increase alcohol consumption in controls (P = 0.14; 149.0 g/week for G/G, 155.7 g/week for A/G and 194.5 g/week for A/A; Supplementary Table S2). We further performed a logistic regression analysis that included alcohol consumption in the model using the classification of drinker or non-drinker. rs1229984 of ADH1B showed a significant association with gout, even after adjustment for alcohol consumption (P = 6.1 × 10−3; OR = 1.83; 95% CI: 1.19–2.81; Supplementary Table S3). Moreover, this association was also significant in the analysis conducted in drinkers only (P = 0.013) and the OR was similar to that in the analysis conducted in all participants (OR = 1.77; 95% CI: 1.13–2.78; Table 3); however, it proved not significant in the analysis conducted in non-drinkers only (P = 0.24; OR = 2.48; 95% CI: 0.55–11.2; Table 3), although the direction of OR is the same as that seen in the analysis conducted in all participants and in drinkers only; however, the sample size of non-drinkers is relatively small.
We have previously demonstrated an association between rs671 (Glu504Lys) of ALDH2 and gout12 as also shown in Table 2. In addition, as shown in Supplementary Table S1, A/G (Lys/Glu) and A/A (Lys/Lys) genotypes of ALDH2 significantly decrease the risk of gout (P = 3.8 × 10−19 and 4.8 × 10−7; OR = 0.45 and 0.41, respectively) as compared with the G/G (Glu/Glu) genotype; however, there is no significant difference in effect sizes on gout between A/G (Lys/Glu) and A/A (Lys/Lys) genotypes (P = 0.71), and the OR is close to 1.00 (OR = 1.09; 95% CI: 0.75–1.62). Based on these results and enzyme activity16, the “non-Lys carrier (Glu/Glu)” (high tolerance for alcohol) vs. “Lys carrier (Lys/Glu or Lys/Lys)” (low tolerance for alcohol) model was used for the following analysis. We also performed a multivariate logistic regression analysis that included alcohol consumption in the model because ALDH2 genotypes were significantly associated with the proportion of non-drinkers (P = 2.5 × 10−83; 93.5% for A/A, 32.2% for A/G and 6.3% for G/G: Supplementary Table S2) and alcohol consumption in controls (P = 2.0 × 10−51; 0.68 g/week for A/A, 91.2 g/week for A/G and 231.0 g/week for G/G: Supplementary Table S2). The association between gout and rs671 of ALDH2 remained significant even after adjustment for alcohol consumption (P = 4.3 × 10−12; OR = 1.92; 95% CI: 1.60–2.31: Supplementary Table S3). Contrary to the result for ADH1B, this association was still significant in the analysis conducted in both non-drinkers only and drinkers only, and the direction of OR and the effect size were similar to those obtained in the analysis conducted in all participants (P = 0.021 and 7.2 × 10−11; OR = 1.93 and 1.92; 95% CI: 1.12–3.33 and 1.58–2.34, respectively: Table 3).
Gout risk due to combination of the ADH1B and ALDH2 genotypes
Next, we investigated the combined effects on gout of the common variants of ADH1B (rs1229984) and ALDH2 (rs671). Based on enzyme activity13,14,15, the “His carrier (His+)” vs. “non-His carrier (His−)” model was selected for the association analysis between gout and rs1229984 (His48Arg) of ADH1B. Regarding the association analysis between gout and rs671 (Glu504Lys) of ALDH2, we adopted the “non-Lys carrier (Lys−)” vs. “Lys carrier (Lys+)” model as described in our previous paper12. Individuals whose combination of rs1229984 and rs671 is “His−/Lys+”, “His−/Lys−” or “His+/Lys+” were subject to a significantly lower risk of gout (P = 3.0 × 10−3, 2.9 × 10−3 and 8.7 × 10−22, respectively) than the other group (“His +/Lys−”), as shown in Table 4. Furthermore, although the 95% CIs overlap each other, the OR of “His−/Lys+” (OR = 0.36; 95% CI: 0.18–0.71) is lower than those of “His−/Lys−” and “His+/Lys+” (OR = 0.44 and 0.42; 95% CI: 0.25–0.75 and 0.36–0.51, respectively).
Discussion
ADH1B and ALDH2 are crucial enzymes for alcohol metabolism, and it is already established that individual differences in these two enzymes’ activities are caused by common variants13. The functionally important variants for ADH1B are rs1229984 (His48Arg) and rs2066702 (Arg370Cys)17,18,19. The allele frequencies of rs1229984 and rs2066702 of ADH1B differ among populations, according to the results of a previous paper13 and ISGR’s 1000 Genomes Phase 320. rs1229984 is polymorphic in Europeans and East Asians, including Japanese, while it is monomorphic in Africans. On the other hand, rs2066702 is monomorphic in Europeans and East Asians but polymorphic in Africans. In this study, therefore, we genotyped rs1229984 with Japanese participants. Because the A/A (His/His) or A/G (His/Arg) genotype of rs1229984 has been reported to produce 40-fold faster ethanol oxidation than the G/G (Arg/Arg) genotype13,14,15, in the present study, we investigated not only the genotype model but also the “His carrier” vs. “non-His carrier” model for the analysis of rs1229984. Regarding the analysis of ALDH2, rs671 (Glu504Lys) is a noted functional variant16, 21. The Lys allele of rs671 is common in East Asians, but quite rare in Europeans and Africans20, 22. Individuals with heterozygotes (Lys/Glu) of rs671 have only 6.25% of the enzyme activity of those with normal ALDH2 (Glu/Glu), and those with homozygotes (Lys/Lys) show almost no activity16. We therefore adopted the “non-Lys carrier” vs. “Lys carrier” model for rs671 in the present study.
No reports on the association between gout and common variants of ADH1B have been published, although Yokoyama et al. recently reported that a common dysfunctional variant of ADH1B, rs1229984, is associated with serum uric acid (SUA) levels in male Japanese alcoholics23. In this study, for the first time, we revealed a significant association between a common dysfunctional variant of ADH1B (rs1229984) and gout (Table 2 and Supplementary Table S1).
We previously reported the association between gout and rs671 of ALDH2 12. Other Japanese24 and Chinese25 studies have also indicated this association. However, in these studies12, 24, 25, alcohol consumption was not taken into consideration, even though rs671 is associated with alcohol consumption (Supplementary Table S2). Thus, we first investigated the association between gout and rs671 of ALDH2 including alcohol consumption in the model. The common dysfunctional variant of ALDH2, rs671, also showed a significant association with gout, even after adjustment for alcohol consumption (Supplementary Table S3) and even in non-drinkers or in drinkers (Table 3). On the other hand, although the association between gout and rs1229984 of ADH1B was still significant even after adjustment for alcohol consumption (Supplementary Table S3) and in drinkers (Table 3), this association was not significant in non-drinkers (Table 3). Because the sample size of non-drinkers was relatively small, further studies are necessary to clarify the effects of alcohol consumption on the association between gout and common variants of ADH1B and ALDH2.
It appears that alcohol intake elevates SUA level by increasing urate production26, 27 and decreasing renal urate excretion28. Ethanol is oxidized to acetate mainly by ADH1B and ALDH2 (Fig. 1). When acetate is further metabolized to acetyl-coenzyme A, adenosine triphosphate (ATP) hydrolyzes to adenosine monophosphate (AMP), which is ultimately metabolized to urate. Thus, alcohol consumption could increase urate by enhancing hydrolysis from ATP to AMP27. Furthermore, the “His+/Lys−” genotype combination causes faster ethanol and acetaldehyde elimination and may accelerate the increase in ATP degradation, which further elevates SUA23. This may be one of the reasons why “His+/Lys−” tends to have a stronger effect on gout than other genotype combinations, in spite of the 95% CIs overlapping each other (Table 4). It is also well known that alcohol consumption can increase lactate29 which is exchanged for urate via urate transporter 1 (URAT1/SLC22A12) in the human kidney30. Therefore, alcohol consumption could also increase the SUA level by enhancing the renal urate reabsorption via URAT1. Taking into consideration the factors mentioned above, alcohol consumption could increase the risk of gout susceptibility resulting from hyperuricemia. ADH1B and ALDH2 enzyme activities, which depend on the common variants, affect alcohol consumption behavior, and the genotyping of ADH1B and ALDH2 variants can be a surrogate for alcohol consumption in the estimation of risks for several diseases, including esophageal cancer, which were demonstrated by Mendelian randomization approaches31, 32. Thus, we initially assumed that the associations between gout and common variants of ADH1B and ALDH2 would be accounted for by alcohol consumption. Contrary to this expectation, these associations were still significant even after adjustment for alcohol consumption (Supplementary Table S3), which indicates that common variants of ADH1B and ALDH2 can be associated with gout susceptibility through not only alcohol consumption but also other factors and/or mechanisms. However, the association of ADH1B was not significant in non-drinkers (Table 3). This study had several limitations in that we were able to use only the frequency data, not the quantity data, on alcohol consumption by gout cases. Similarly, the adjustment for alcohol consumption might not be sufficient because these alcohol-drinking data were self-reported, and it is difficult to obtain data on lifetime alcohol consumption. A further problem is that adjustment of the association between these genetic variants and gout for alcohol consumption could also lead to collider bias. It is similar that the adjustment for cigarettes smoked per day does not entirely mediate the relationship between genetic variants and lung cancer: this is most likely due to the fact that daily cigarette consumption does not accurately capture total tobacco exposure33. Therefore, from the point of view of alcohol consumption, further studies are necessary to be able to elucidate the association between gout and common variants of ADH1B and ALDH2.
In summary, our data show that common variants of ADH1B (rs1229984) and ALDH2 (rs671) are independently associated with gout, which indicates that the genotyping of rs1229984 and rs671 can be useful for the evaluation of gout risk.
Methods
Study participants
This study was approved by the institutions’ Ethical Committees (National Defense Medical College and Nagoya University). All procedures were performed in accordance with the Declaration of Helsinki, with written informed consent obtained from each subject. In this study, all the participants were Japanese males: the frequency of Japanese female gout patients is extremely low, at about only 1% of the entire population of gout patients that we analyzed. The gout cases comprised 1,048 patients assigned from Japanese male outpatients at the gout clinics of Kyoto Industrial Health Association (Kyoto, Japan) or Ryougoku East Gate Clinic (Tokyo, Japan). All patients were clinically diagnosed with primary gout according to the criteria established by the American College of Rheumatology34. Patients with inherited metabolic disorders, including Lesch–Nyhan syndrome, were excluded. For the control group, 1,334 Japanese males with SUA levels of ≤7.0 mg/dl and without a history of gout were recruited from the participants in the Shizuoka area in the Japan Multi-Institutional Collaborative Cohort Study (J-MICC Study)35, 36. Participants who consumed alcohol at least once a month were classified as drinkers. In the controls, the information on alcohol consumption was collected at the point of recruitment into the study. Meanwhile, in the gout cases, we used information on alcohol consumption at the point of gout onset. There is detailed information on alcohol consumption for the controls: we show and analyze the amount of alcohol consumption data for each genotype (Supplementary Table S2). On the other hand, the information on alcohol consumption in gout cases was limited to whether the subject is a drinker or non-drinker. Thus, in this study, the adjustment for alcohol consumption was performed using the classification of drinker or non-drinker. The details on the participants in this study are shown in Table 1.
Genetic analysis
Genomic DNA was extracted from whole peripheral blood cells37. Genotyping of rs1229984 of ADH1B was performed using the TaqMan method (Thermo Fisher Scientific, Waltham, MA, USA) employing a LightCycler 480 (Roche Diagnostics, Mannheim, Germany)37 with minor modifications. The custom TaqMan assay probe was designed as follows: VIC- CTGTAGGAATCTGTCACACAG and FAM- TGTAGGAATCTGTCGCACAG. Genotyping data on rs671 of ALDH2 was obtained from our previous study12.
Statistical analyses
R-3.1.1 (http://www.r-project.org/) software was used for all calculations in the statistical analysis38. The association analyses were examined using Fisher’s exact test, Cochran-Armitage test, linear regression analysis and logistic regression analysis. All P values were two-tailed and P values of <0.05 were regarded as statistically significant.
References
Matsuo, H. et al. Common defects of ABCG2, a high-capacity urate exporter, cause gout: a function-based genetic analysis in a Japanese population. Sci Transl Med 1, 5ra11–5ra11, doi:10.1126/scitranslmed.3000237 (2009).
Woodward, O. M. et al. Identification of a urate transporter, ABCG2, with a common functional polymorphism causing gout. Proc Natl Acad Sci USA 106, 10338–42, doi:10.1073/pnas.0901249106 (2009).
Phipps-Green, A. J. et al. Twenty-eight loci that influence serum urate levels: analysis of association with gout. Ann Rheum Dis 75, 124–30, doi:10.1136/annrheumdis-2014-205877 (2016).
Matsuo, H. et al. Genome-wide association study of clinically defined gout identifies multiple risk loci and its association with clinical subtypes. Ann Rheum Dis 75, 652–9, doi:10.1136/annrheumdis-2014-206191 (2016).
Li, C. et al. Genome-wide association analysis identifies three new risk loci for gout arthritis in Han Chinese. Nat Commun 6, 7041, doi:10.1038/ncomms8041 (2015).
Matsuo, H. et al. Common dysfunctional variants in ABCG2 are a major cause of early-onset gout. Sci Rep 3, 2014, doi:10.1038/srep02014 (2013).
Matsuo, H. et al. ABCG2 dysfunction causes hyperuricemia due to both renal urate underexcretion and renal urate overload. Sci Rep 4, 3755, doi:10.1038/srep03755 (2014).
Nakayama, A. et al. Common dysfunctional variants of ABCG2 have stronger impact on hyperuricemia progression than typical environmental risk factors. Sci Rep 4, 5227, doi:10.1038/srep05227 (2014).
Chiba, T. et al. NPT1/SLC17A1 is a renal urate exporter in humans and its common gain-of-function variant decreases the risk of renal underexcretion gout. Arthritis Rheumatol 67, 281–7, doi:10.1002/art.38884 (2015).
Sakiyama, M. et al. The effects of URAT1/SLC22A12 nonfunctional variants, R90H and W258X, on serum uric acid levels and gout/hyperuricemia progression. Sci Rep 6, 20148, doi:10.1038/srep20148 (2016).
Takeuchi, F. et al. Confirmation of ALDH2 as a major locus of drinking behavior and of its variants regulating multiple metabolic phenotypes in a Japanese population. Circ J 75, 911–918, doi:10.1253/circj.CJ-10-0774 (2011).
Sakiyama, M. et al. Identification of rs671, a common variant of ALDH2, as a gout susceptibility locus. Sci Rep 6, 25360, doi:10.1038/srep25360 (2016).
Bosron, W. F. & Li, T. K. Genetic polymorphism of human liver alcohol and aldehyde dehydrogenases, and their relationship to alcohol metabolism and alcoholism. Hepatology 6, 502–10, doi:10.1002/hep.1840060330 (1986).
Hashibe, M. et al. Evidence for an important role of alcohol- and aldehyde-metabolizing genes in cancers of the upper aerodigestive tract. Cancer Epidemiol Biomarkers Prev 15, 696–703, doi:10.1158/1055-9965.EPI-05-0710 (2006).
Tanaka, F. et al. Strong interaction between the effects of alcohol consumption and smoking on oesophageal squamous cell carcinoma among individuals with ADH1B and/or ALDH2 risk alleles. Gut 59, 1457–64, doi:10.1136/gut.2009.205724 (2010).
Matsuo, K. et al. Alcohol dehydrogenase 2 His47Arg polymorphism influences drinking habit independently of aldehyde dehydrogenase 2 Glu487Lys polymorphism: analysis of 2,299 Japanese subjects. Cancer Epidemiol Biomarkers Prev 15, 1009–13, doi:10.1158/1055-9965.EPI-05-0911 (2006).
Jornvall, H., Hempel, J., Vallee, B. L., Bosron, W. F. & Li, T. K. Human liver alcohol dehydrogenase: amino acid substitution in the beta 2 beta 2 Oriental isozyme explains functional properties, establishes an active site structure, and parallels mutational exchanges in the yeast enzyme. Proc Natl Acad Sci USA 81, 3024–8, doi:10.1073/pnas.81.10.3024 (1984).
Yoshida, A., Impraim, C. C. & Huang, I. Y. Enzymatic and structural differences between usual and atypical human liver alcohol dehydrogenases. J Biol Chem 256, 12430–6 (1981).
Burnell, J. C. et al. The human beta 3 alcohol dehydrogenase subunit differs from beta 1 by a Cys for Arg-369 substitution which decreases NAD(H) binding. Biochem Biophys Res Commun 146, 1227–33, doi:10.1016/0006-291X(87)90779-0 (1987).
1000 Genomes Project Consortium. et al. A map of human genome variation from population-scale sequencing. Nature 467, 1061–73, doi:10.1038/nature09534 (2010).
Yoshida, A., Huang, I. Y. & Ikawa, M. Molecular abnormality of an inactive aldehyde dehydrogenase variant commonly found in Orientals. Proc Natl Acad Sci USA 81, 258–61, doi:10.1073/pnas.81.1.258 (1984).
Goedde, H. W. et al. Distribution of ADH2 and ALDH2 genotypes in different populations. Hum Genet 88, 344–6, doi:10.1007/BF00197271 (1992).
Yokoyama, A. et al. Alcohol dehydrogenase-1B (rs1229984) and aldehyde dehydrogenase-2 (rs671) genotypes and alcoholic ketosis are associated with the serum uric acid level in Japanese alcoholic men. Alcohol Alcohol 51, 268–74, doi:10.1093/alcalc/agv123 (2016).
Yamanaka, H. et al. Analysis of the genotypes for aldehyde dehydrogenase 2 in Japanese patients with primary gout. Adv Exp Med Biol 370, 53–6, doi:10.1007/978-1-4615-2584-4 (1994).
Wang, C. et al. The polymorphisms of aldehyde dehydrogenase 2 gene are associated with gout disease in male Han Chinese. Gout and Hyperuricemia 3, 40–45 (2016).
Faller, J. & Fox, I. H. Ethanol-induced hyperuricemia: evidence for increased urate production by activation of adenine nucleotide turnover. N Engl J Med 307, 1598–602, doi:10.1056/NEJM198212233072602 (1982).
Puig, J. G. & Fox, I. H. Ethanol-induced activation of adenine nucleotide turnover. Evidence for a role of acetate. J Clin Invest 74, 936–41, doi:10.1172/JCI111512 (1984).
Lieber, C. S., Jones, D. P., Losowsky, M. S. & Davidson, C. S. Interrelation of uric acid and ethanol metabolism in man. J Clin Invest 41, 1863–70, doi:10.1172/JCI104643 (1962).
Taniguchi, A. & Kamatani, N. Control of renal uric acid excretion and gout. Curr Opin Rheumatol 20, 192–7, doi:10.1097/BOR.0b013e3282f33f87 (2008).
Enomoto, A. et al. Molecular identification of a renal urate anion exchanger that regulates blood urate levels. Nature 417, 447–52, doi:10.1038/nature742 (2002).
Holmes, M. V. et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 349, g4164–g4164, doi:10.1136/bmj.g4164 (2014).
Lewis, S. J. & Smith, G. D. Alcohol, ALDH2, and esophageal cancer: a meta-analysis which illustrates the potentials and limitations of a Mendelian randomization approach. Cancer Epidemiol Biomarkers Prev 14, 1967–71, doi:10.1158/1055-9965.EPI-05-0196 (2005).
VanderWeele, T. J., Tchetgen Tchetgen, E. J., Cornelis, M. & Kraft, P. Methodological challenges in mendelian randomization. Epidemiology 25, 427–35, doi:10.1097/EDE.0000000000000081 (2014).
Wallace, S. L. et al. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum 20, 895–900, doi:10.1002/(ISSN)1529-0131 (1977).
Hamajima, N., J-MICC Study Group. The Japan Multi-Institutional Collaborative Cohort Study (J-MICC Study) to detect gene-environment interactions for cancer. Asian Pac J Cancer Prev 8, 317–23 (2007).
Asai, Y. et al. Baseline data of Shizuoka area in the Japan Multi-Institutional Collaborative Cohort Study (J-MICC Study). Nagoya J Med Sci 71, 137–44 (2009).
Sakiyama, M. et al. Common variant of leucine-rich repeat-containing 16A (LRRC16A) gene is associated with gout susceptibility. Hum Cell 27, 1–4, doi:10.1007/s13577-013-0081-8 (2014).
R Core Team R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/ (2014).
Acknowledgements
We would like to thank all the participants for their generous involvement in this study. Our sincere gratitude also goes to the members of the Japan Multi-Institutional Collaborative Cohort Study (J-MICC Study) Shizuoka Field for supporting the study. We are indebted to K. Gotanda, Y. Morimoto, M. Miyazawa, Y. Kawamura, T. Chiba, H. Inoue, M. Komatsu, R. Sugiyama and T. Nakamura at National Defense Medical College for genetic analysis and helpful discussions, and to A. Tokumasu and K. Ooyama at Ryougoku East Gate Clinic and K. Wakai and N. Hamajima at Nagoya University for sample collection. This study was supported by grants from the Ministry of Education, Culture, Sports, Science and Technology (MEXT) of Japan including the MEXT Kakenhi (Grant numbers 25293145 and 15K15227), the Ministry of Health, Labour and Welfare of Japan, the Ministry of Defense of Japan, the Japan Society for the Promotion of Science, the Kawano Masanori Memorial Foundation for Promotion of Pediatrics, and the Gout Research Foundation of Japan. The study was also supported by a JSPS Kakenhi Grant (Grant number 16H06277) and Grants-in-Aid for Scientific Research on Priority Areas (Grant number 17015018) and Innovative Areas (Grant numbers 221S0001 and 221S0002) from the Japanese Ministry of Education, Culture, Sports, Science, and Technology.
Author information
Authors and Affiliations
Contributions
M.S. and H.M. conceived and designed this study. M.N., S.K., T.S. and H.O. collected samples and analyzed the clinical data. M.S., H.M., A.A., S.S., T.H., M.K. and A.N. performed genetic analyses. M.S., H.M. and H.N. performed statistical analyses. Y.S., K.I. and N.S. provided intellectual input and assisted with the preparation of the manuscript. M.S. and H.M. wrote the manuscript. M.S. and H.M. contributed equally to this work.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakiyama, M., Matsuo, H., Akashi, A. et al. Independent effects of ADH1B and ALDH2 common dysfunctional variants on gout risk. Sci Rep 7, 2500 (2017). https://doi.org/10.1038/s41598-017-02528-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-02528-z
This article is cited by
-
Interaction of genetic variation at ADH1B and MLXIPL with alcohol consumption for elevated serum urate level and gout among people of European ethnicity
Arthritis Research & Therapy (2024)
-
Identification of CDC42BPG as a novel susceptibility locus for hyperuricemia in a Japanese population
Molecular Genetics and Genomics (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.