Abstract
Small cell lung cancer (SCLC), as a proportion, makes up only 15–17% of lung cancer cases. The development of treatments for SCLC has remained stagnant for decades, and SCLC is expected to persist as a threat to human health. To date, no publications based on large populations have been reported. We calculated survival changes in patients with SCLC during each decade between 1983 and 2012 to determine the roles of race, sex, age, and socioeconomic status (SES) on survival rates based on the Surveillance, Epidemiology, and End Results (SEER) registries. In total, 106,296 patients with SCLC were identified, with the overall incidence per 100,000 decreasing each decade from 9.6 to 7.8 to 5.8. The median survival for SCLC remained 7 months, and the 12-month relative survival rates (RSRs) remained relatively stable at 32.9%, 33.2% and 33.2% during each decade. The 5-year RSRs significantly improved from 4.9% to 5.9% to 6.4% during each decade, but remained extremely low. In addition, a narrowing of the survival gaps among SES groups and stable survival gaps between sexes were observed. Although the incidence of SCLC decreased during each decade, the overall survival remained relatively stable, highlighting the urgency of developing novel treatments and the importance of prevention and early detection.
Similar content being viewed by others
Introduction
Lung cancer is estimated to be the second most common cancer type and the leading cause of cancer-related death in both sexes, with an estimated 116,990 cases in males and 105,510 in females1. Small-cell lung cancer (SCLC), accounting for approximately 15% to 17% of all diagnosed lung cancers, is characterized by a high invasiveness, short doubling time, high growth fraction and ease of metastasis upon diagnosis2, 3. Classified as a neuroendocrine tumor despite its differences with non-small cell lung cancer (NSCLC), SCLC is distinctly different from extrapulmonary small cell carcinoma in disease progression, prognosis and etiology4.
Radiotherapy plus platinum-based chemotherapy has been the standard treatment for most SCLC cases for 30 years and has reached an efficiency plateau. Surgery is only an option for a small proportion of limited stage patients based on Veterans Administration Lung Study Group (VALSG) staging5,6,7,8. In addition and in sharp contrast to NSCLC, for which survival has improved remarkably in the past few decades due to the development of EGFR, ROS1, and ALK inhibitors among others, no major developments have been made in SCLC treatment, including targeted agents, such as EGFR-TKI, BCR-ABL TKIs, or mTOR inhibitors9,10,11. These factors have limited improvements of the currently dismal survival rates for SCLC. In addition, the average cost for SCLC treatment remains enormous, at 11,556 pounds, or 15,418 Euros, for limited disease and 12,482 Euros for extensive disease12, 13. More radical chemotherapy or maintenance of chemotherapy did not significantly improve patients’ survival8, 14,15,16,17. These trends have challenged healthcare legislators as the current treatment plateau has not been overcome by additional financial expenditures, especially given the already high financial burden of SCLC. In addition to the lack of treatment effectiveness, approximately 70% of SCLC diagnoses are already at the point of extensive disease, indicating that more emphasis should be placed on clinical awareness of screening and early detection18. Intuitively, SCLC survival is expected to remain constant, but no relevant large population-based publications have been reported. Previous publications on SCLC survival rates focused on specific patient populations at certain stages or patients receiving chemotherapy, prophylactic cranial irradiation and surgery19,20,21,22,23. This study, using period analyses, aimed to evaluate the survival changes in each decade from 1983 to 2012 on the basis of the Surveillance, Epidemiology, and End Results (SEER) database.
Additionally, racial and socioeconomic status (SES) disparities in the U.S. health care system are of great concern and have been shown to influence survival in many malignancies24, 25. Preliminary data have shown that SES can also affect survival for extensive stages of SCLC, indicating the need for amelioration in healthcare policies to balance this survival disparity26. This study determined the survival changes over three decades and clarified the roles of sex, age, race and SES on the survival of patients with SCLC based on the SEER database.
Results
Incidence of SCLC over three decades
To guarantee the comparability of incidence data over three decades by extracting data from the same registry sites, we extracted incidence data from the nine original registry sites in the SEER database. A total of 56,220 cases diagnosed with SCLC between 1983 and 2012 were identified. The overall incidence of SCLC per 100,000 decreased each decade over time to 9.6, 7.8 and 5.8, as illustrated in Fig. 1 and Supplementary Table S1. This trend of reduction in incidence can be seen in most age groups, with large decreases in some groups: from 24.4 to 17.4 to 11.5 in the 50–64 age group and from 48.7 to 43.0 to 33.1 in the 65–79 age group (Fig. 1a, Suppl. Table S1). However, incidence remained stable in the 0–34 and older than 80 age groups. Incidence was highest in the 65–79 age group in all three decades. The SCLC patient number decreased in most groups except for the over 80 group, in which the patient number kept increasing over time (Fig. 1b, Suppl. Table S1).
Summary incidences of patients diagnosed as having SCLC between 1983 and 2012 at the original nine SEER sites. Incidence (a) and number (b) of SCLC cases are shown by age group (total and ages 0–34, 35–49, 50–64, 65–79, and 80+ years) and calendar period. Incidence and number of SCLC cases are grouped by sex (c,d), SES (e,f), and race (g,h), respectively.
Incidence differences were observed between sexes, with a higher incidence per 100,000 in males (12.9 vs. 7.1 in 1983–1992, 9.2 vs. 6.8 in 1993–2002, and 6.4 vs. 5.4 in 2003–2012; Fig. 1c, Suppl. Table S1). More importantly, the incidence gaps between sexes kept shrinking due to the rapidly declining incidence in males and stable incidence in females. The patient number in both sexes became similar over the last two decades due to decreasing male cases and a stable number of female cases (Fig. 1d).
SCLC incidence by SES and by race
As illustrated in Fig. 1e,f and Supplementary Table S1, ever-decreasing incidence rates over the three decades were observed in all SES groups. The medium-poverty group (from 9.5 to 7.9 to 5.9) shared a similar incidence with the low-poverty group (from 9.7 to 7.8 to 5.8) each decade and had a higher incidence than the high-poverty group (from 7.3 to 6.4 to 4.7). The number of SCLC patients continuously decreased in the low-poverty and medium-poverty groups, whereas in the high-poverty group, it remained relatively stable (Fig. 1f).
The incidence per 100,000 patients in all racial groups decreased over the three decades, with Whites showing a higher SCLC incidence than Blacks or Others. The incidence gaps between Whites and Others kept narrowing each decade (from 5.1 to 4.1 to 3.1), whereas the incidence gaps between Whites and Blacks widened slightly each decade (Fig. 1g, Suppl. Table S1.) The number of White and Black SCLC patients decreased each decade; however, the number of patients in the Others group increased slightly (Fig. 1h).
Survival for SCLC patients over three decades
A total of 106,439 patients with SCLC between 1983 and 2012 at 18 registry sites were identified, with the five-year survival rate improving from 4.9% to 5.9% to 6.4% each decade (p < 0.0001). However, the median survival remained 7 months in each decade.
Relative survival rates (RSRs) in patients with SCLC remained relatively stable in the total population and in almost all age groups over the three decades (Table 1 and Fig. 2a). The 12-month RSRs remained relatively stable in the total population and all age groups across the three decades. However, a slight survival improvement could be seen in the 36-month RSRs, improving from 7.2% to 8.6% to 9.3% over the three decades, with a larger increase in the first two decades (p < 0.0001). More importantly, the survival improvement over the three decades was age-dependent, with a greater survival improvement in younger patient groups. The improvement in RSR over the three decades was followed up for 5 years. Significantly improved survival times over the three decades in the total population and in the 35–49, 50–64 and 65–79 age groups were also confirmed by Kaplan-Meier curves (p < 0.0001, Fig. 2b). Furthermore, the trends toward increased long-term survival and age-dependent survival improvement were also seen in the Kaplan-Meier curves.
As illustrated in Table 2 and Fig. 3, the 12-month RSRs in both sexes remained relatively stable over the three decades. However, slight improvements could be seen for both sexes in the 60-month RSRs, as well as in the 24- and 36-month RSRs (Table 2, Fig. 3, Suppl. Figure S1, Suppl. Table S2). A survival advantage in the 12-month RSRs was determined in females (37.2% vs. 29.8%, p < 0.0001), and the survival gap between sexes remained relatively stable each decade (36.6% vs. 30.2% in 1993–2002 and 36.4% vs. 30.1% in 2003–2012, p < 0.0001; Table 2, Fig. 3a). The survival advantage in females and stable survival gap could also be seen in the Kaplan-Meier survival analyses and 60-month RSRs, as well as in the 24- and 36-month RSRs (p < 0.0001) (Fig. 3b, Suppl. Table S2, Suppl. Figure S2 and Suppl. Figure S3).
In addition, survival superiority in females was more evident in some age groups, as illustrated in Table 2 and Fig. 3. Significantly higher 12-month RSRs in females were seen in patients aged 50–64 years in each decade (44.9% vs. 35.1% in 1983–1992, 45.7% vs. 35.6% in 1993–2002, 45.1% vs. 35.4% in 2003–2012; p < 0.0001 for each). In addition, the age-dependent survival difference between sexes was also observed in the 35–49 and 65–79 age groups. A similar trend in RSR differences between the sexes was noted in the 24- and 36-month RSRs (Suppl. Table S2 and Suppl. Figure S1). The significant age-dependent RSR differences between the sexes were confirmed by Kaplan-Meier curves in most age groups, except for the 0–34 year group (p = 0.0585 for group 0–34 years, p = 0.0025 for group 80+ years and p < 0.0001 for the rest, Fig. 3b).
Furthermore, age, SES, and sex were independent predictors for overall survival over the three decades according to Cox regression analyses (p < 0.001) (Suppl. Table S3). The hazard ratios of all of the variables remained stable in each decade and for the three decades combined.
Survival by race and SES
The 12-month RSRs remained relatively stable, whereas a slight improvement could be seen in the 36- and 60-month RSRs in all races and SES groups. Whites shared similar RSRs with Blacks in each decade (Fig. 4a, Table 3 and Suppl. Table S4). Kaplan-Meier survival analyses showed that the survival disparity between Whites and Blacks continued to diminish each decade with increasing p values from 0.0537 to 0.1279 to 0.4220 (Fig. 4c). After classifying all patients, including Hispanic or those with a non-Hispanic status, by racial records in the SEER database, Hispanic patients, as a major minority, shared similar survival with non-Hispanic patients in each decade and the three decades combined (Suppl. Figure S4). In terms of SES, the highest SES was found in the low-poverty group, with the lowest in the high-poverty group (Fig. 4b, Table 4, and Suppl. Table S5). In addition, statistically significant differences in survival among the three SES groups were found each decade (p < 0.0001 for each); more importantly, the survival disparities narrowed each decade (Fig. 4d). Interestingly, the percentage of low-poverty patients in the Whites group was dramatically higher than in the Blacks group (43.8% vs. 17.5%), but the percentage of medium-poverty individuals was higher in the Black group over the three decades (71.5% vs. 48.0%; Suppl. Figure S5; Suppl. Table S6). The variables race and SES were related, with Spearman rank correlation coefficients of 0.121 and p < 0.001. Indeed, the survival difference between Whites and Blacks reflected their different distribution in SES.
Discussion
Here, we demonstrated that the incidence of SCLC declined each decade in terms of the total patient population and each patient group stratified by age, sex, race or SES. Long-term survival improved slightly, especially in the first two decades, despite the relatively stable median survival time. Moreover, the survival gaps among races or SES groups diminished each decade.
The incidence and etiology of SCLC
The incidence of SCLC declined in the total population and most age groups, except for the 80+ age group, in which the incidence remained relatively stable. Risk factors for lung cancer mainly included smoking, air pollution, and exposure to carcinogenic chemicals, such as asbestos, arsenic, radon, and polycyclic aromatic hydrocarbons2, 10, 27. The lung cancer rates and trends reflected the trends of tobacco consumption28,29,30. In the United States, smoking rates and lung cancer occurrence declined markedly after increased public awareness of the harm of smoking following the United States Surgeon General’s Reports released in 1964 and deployment of comprehensive tobacco control programs31,32,33. Recent studies found that TP53, RB1, NOTCH, MYC and PI3K are aberrantly mutated in SCLC samples; however, well-established etiological factors for SCLC, like the EGFR-mutation in NSCLC, have not been identified34,35,36,37.
Current trends and challenges in SCLC survival
Although the long-term survival of patients with SCLC improved each decade, long-term survival remained at an extremely low level, indicating a pressing need for improvements in the of management of SCLC. In addition, despite the significant changes observed in survival time over the three decades, the absolute increments in each decade were marginal in both the total population and each patient group stratified. Several factors were responsible for the slight survival improvement over the three decades. First, unlike cases in NSCLC, attempts of using novel agents, including pravastatin and targeted therapy, for SCLC failed, and radiotherapy plus platinum-based chemotherapy with etoposide has been the standard care since the early 1980s, but an efficacy plateau has been reached5,6,7,8, 38,39,40. Earlier administration of radiotherapy can marginally improve overall survival41. Second, based on our data, most cases were diagnosed as distant cases, with 62%, 64% and 71% in this category in each decade, respectively, indicating the exigence of improving clinical awareness of early detection and detection techniques (Suppl. Table S7). Early screening by low-dose computed topography may help identify early stage lung cancer and thereby benefit patients; however, this screening has not been widely adapted42,43,44,45. Third, the development of targeted therapy and clinical staging was halted by a scarcity of well-elucidated driver mutations and pathological characteristics. In addition, EGFR-TKI,BCR-ABL TKIs, mTOR inhibitors and anti-angiogenesis treatments have not received approval for SCLC due to a lack of clinical efficiency9, 10. The slight improvement in long-term survival may be due to developments in second line chemotherapy and hospice care. Recently, preliminary data from clinical trials on CTLA4 and PD-1 inhibitors have demonstrated promising efficiency at treating SCLC, with durable and manageable AEs5. In addition, 22.5% of lung cancer cases fail to receive timely treatment, and great importance should therefore be attached to the timeliness of receiving treatment46.
Sexual disparities in SCLC
In sharp contrast to the markedly declined incidence trend in males, the incidence in females remained stable across the three decades. Males had more space to decline due to increased tobacco consumption, and females showed a weaker response to tobacco cessation programs47,48,49. Despite the stable 12-month RSRs, we observed a slightly improving long-term survival in both sexes, with survival superiority in females, indicating an intrinsic genomic differences between the sexes.
Racial disparities in SCLC
The incidence of SCLC in all races decreased each decade, and the incidence gap between the Black and Other groups continued to narrow over the three decades. As demonstrated by the Kaplan-Meier curves, no significant survival difference existed between Whites and Blacks, and the survival gap among them continued to narrowed in each decade. Furthermore, the outcomes for both African-Americans and non-African-Americans were similar when equivalent therapies were offered50. Interestingly, a higher proportion of White patients were classified as low-poverty compared to Black patients. Similarly, the narrowing survival disparities in both races and SES groups may have been due to differing SES distributions between Blacks and Whites since financially disadvantaged patients were believed to be less likely to receive medical care, ultimately leading to shorter survival. In addition, Hispanics, a major minority, showed similar survival with non-Hispanics in each decade and the three decades combined.
SCLC Disparities among the SES groups
There were differences in the incidence of SCLC among the various SES groups, with the highest incidence in the low- and medium-poverty groups. Lower incidence in the high-poverty group could be partly due to a lower consumption of cigarettes and living in less industrialized regions, keeping them away from air pollution. The survival differed among different SES groups, however, and the survival gaps among the various SES groups continued to narrow each decade (p < 0.0001 for each). This narrowing trend may be attributed to the following reasons: first, the development of health care systems narrows the survival disparities among different SES groups by covering more patients, and second, the standard first-line chemotherapy regimen and the radiotherapy, which are applicable to most SCLC cases, were financially available to most patients. However, the cost of SCLC treatment is considerable as was the financial heterogeneity inside patient groups, which may have led to the aforementioned survival disparity12. Therefore, healthcare regulations to compensate financially disadvantaged patients may help fill the gaps among SES groups.
In this study, we did not divide patients by stage because this was outside the scope of this study and the staging systems (both TNM and VALSG) have changed over time. In addition, the patient data from selected SEER registry sites only reflect the tendencies of selected areas, and therefore, the results and conclusions should be interpreted with caution when being applied to other areas. Furthermore, this study may be affected by bias and errors if there is any under-registration or misclassification in the SEER database51.
In general, this study demonstrated the declining incidence and relatively stable survival rates of SCLC. However, the medical burden brought on by SCLC remains significant, indicating the urgency not only for early detection and prevention but also for developing novel therapies. In addition, the survival disparities demonstrated in this study imply that there is heterogeneity in SCLC. This study may help in the design of better clinical trials by balancing these disparities and ultimately improving the clinical treatment of SCLC. Furthermore, the trends shown here highlight the need for developing novel agents by clarifying genetic patterns and may assist politicians in passing legislation to rectify disparities among SES groups.
Materials and Methods
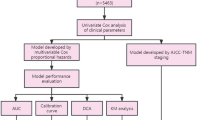
Data extraction from SEER database
All cases of patients diagnosed with SCLC between 1983 and 2012 were accessed from the SEER database, a database maintained by the National Cancer Institute, covering approximately 28% of the U.S. population52. In addition, incidence data and survival data were obtained from nine original registry sites and 18 registry sites, respectively. SEER*Stat version 8.3.2 software was used for all data collection.
Categorized SCLC cases across three decades
Patients were included on the basis of the SEER site recode using the International Classification of Diseases for Oncology, Third Edition (2008), Lung and Bronchus (C34.0–C34.9). We accessed only the cases diagnosed between 1983 and 2012. SCLC cases were histologically defined by the following International Classification of Diseases for Oncology, Third Edition, histology codes for malignant cases: 8041/2 (Small cell carcinoma in situ), 8041/3 (Small cell carcinoma, NOS), 8042/3 (Oat cell carcinoma), 8043/3 (Small cell carcinoma, fusiform cell), 8044/3 (Small cell carcinoma, intermediate cell), and 8045/3 (Combined small cell carcinoma). We excluded cases of SCLC that had been identified by an autopsy or a death certificate.
We analyzed incidence and survival data in each decade between 1983 and 2012. Furthermore, patient cases were classified by race, sex, age, and SES. We defined SES levels as published previously; briefly, SES levels, on the basis of the county poverty rate, were divided into three categories25. In addition, all patients included were classified as either Hispanic or non-Hispanic based on the racial record in the SEER database, and their survival was compared, as Hispanics are a major minority in U.S.
Incidence and survival trends
Incidence data were calculated per 100,000 persons and RSR was restricted to the deaths owing directly to SCLC25. The differences between Kaplan-Meier curves were evaluated by a two-tailed log-rank test.
Cox regression and Spearman rank correlation analyses
The Others group was excluded from Cox regression analysis due to disparities within the group. In addition, the original high-poverty group and medium-poverty group were merged as a novel “med-high-poverty group”. Ages were divided into five groups, as previously discussed. We performed Spearman rank correlation analyses because race and SES were not normally distributed. Stata MP 14 software (Stata Corp) was used for Cox regression analyses and Spearman rank correlation analyses. A two-tailed p value of <0.01 was considered statistically significant.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer Statistics, 2017. CA: a cancer journal for clinicians 67, 7–30, doi:10.3322/caac.21387 (2017).
Hamilton, G. & Rath, B. Smoking, inflammation and small cell lung cancer: recent developments. Wiener medizinische Wochenschrift 165, 379–386, doi:10.1007/s10354-015-0381-6 (2015).
Kahnert, K., Kauffmann-Guerrero, D. & Huber, R. M. SCLC-State of the Art and What Does the Future Have in Store? Clinical lung cancer, 10.1016/j.cllc.2016.05.014 (2016).
Dores, G. M., Qubaiah, O., Mody, A., Ghabach, B. & Devesa, S. S. A population-based study of incidence and patient survival of small cell carcinoma in the United States, 1992–2010. BMC cancer 15, 185, doi:10.1186/s12885-015-1188-y (2015).
Paglialunga, L., Salih, Z., Ricciuti, B. & Califano, R. Immune checkpoint blockade in small cell lung cancer: is there a light at the end of the tunnel? ESMO open 1, e000022, doi:10.1136/esmoopen-2015-000022 (2016).
Hensing, T., Chawla, A., Batra, R. & Salgia, R. A personalized treatment for lung cancer: molecular pathways, targeted therapies, and genomic characterization. Advances in experimental medicine and biology 799, 85–117, doi:10.1007/978-1-4614-8778-4_5 (2014).
Kalemkerian, G. P. Advances in pharmacotherapy of small cell lung cancer. Expert opinion on pharmacotherapy 15, 2385–2396, doi:10.1517/14656566.2014.957180 (2014).
Chute, J. P., Chen, T., Feigal, E., Simon, R. & Johnson, B. E. Twenty years of phase III trials for patients with extensive-stage small-cell lung cancer: perceptible progress. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 17, 1794–1801, doi:10.1200/JCO.1999.17.6.1794 (1999).
Mamdani, H., Induru, R. & Jalal, S. I. Novel therapies in small cell lung cancer. Translational lung cancer research 4, 533–544, doi:10.3978/j.issn.2218-6751.2015.07.20 (2015).
Stratigos, M., Matikas, A., Voutsina, A., Mavroudis, D. & Georgoulias, V. Targeting angiogenesis in small cell lung cancer. Translational lung cancer research 5, 389–400, doi:10.21037/tlcr.2016.08.04 (2016).
Thomas, A., Liu, S. V., Subramaniam, D. S. & Giaccone, G. Refining the treatment of NSCLC according to histological and molecular subtypes. Nature reviews. Clinical oncology 12, 511–526, doi:10.1038/nrclinonc.2015.90 (2015).
Oliver, E. et al. Treatment pathways, resource use and costs in the management of small cell lung cancer. Thorax 56, 785–790, doi:10.1136/thorax.56.10.785 (2001).
Corral, J. et al. Estimation of lung cancer diagnosis and treatment costs based on a patient-level analysis in Catalonia (Spain). BMC health services research 15, 70, doi:10.1186/s12913-015-0725-3 (2015).
Lally, B. E., Urbanic, J. J., Blackstock, A. W., Miller, A. A. & Perry, M. C. Small cell lung cancer: have we made any progress over the last 25 years? The oncologist 12, 1096–1104, doi:10.1634/theoncologist.12-9-1096 (2007).
Riess, J. W. & Lara, P. N. Jr. Left behind? Drug discovery in extensive-stage small-cell lung cancer. Clinical lung cancer 15, 93–95, doi:10.1016/j.cllc.2013.12.010 (2014).
Sculier, J. P. et al. Maintenance chemotherapy for small cell lung cancer: a critical review of the literature. Lung cancer 19, 141–151, doi:10.1016/S0169-5002(97)00084-6 (1998).
ECC 2015: First Targeted Treatment for Small Cell Lung Cancer Show Promise. http://www.ascopost.com/ViewNews.aspx?nid=33887.
Kalemkerian, G. P. et al. Small cell lung cancer. Journal of the National Comprehensive Cancer Network: JNCCN 11, 78–98, doi:10.6004/jnccn.2013.0011 (2013).
Kim, E. et al. Comparison of cisplatin/etoposide versus carboplatin/etoposide concurrent chemoradiation therapy for limited-stage small cell lung cancer (LS-SCLC) in the elderly population (age > 65 years) using national SEER-Medicare data. Practical radiation oncology, 10.1016/j.prro.2016.01.011 (2016).
Caprario, L. C., Kent, D. M. & Strauss, G. M. Effects of chemotherapy on survival of elderly patients with small-cell lung cancer: analysis of the SEER-medicare database. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 8, 1272–1281, doi:10.1097/JTO.0b013e3182a007ba (2013).
Eaton, B. R. et al. Effect of prophylactic cranial irradiation on survival in elderly patients with limited-stage small cell lung cancer. Cancer 119, 3753–3760, doi:10.1002/cncr.28267 (2013).
Yu, J. B., Decker, R. H., Detterbeck, F. C. & Wilson, L. D. Surveillance epidemiology and end results evaluation of the role of surgery for stage I small cell lung cancer. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 5, 215–219, doi:10.1097/JTO.0b013e3181cd3208 (2010).
Lally, B. E. et al. Trends in the outcomes for patients with limited stage small cell lung cancer: An analysis of the Surveillance, Epidemiology, and End Results database. Lung cancer 64, 226–231, doi:10.1016/j.lungcan.2008.08.010 (2009).
Wang, S. et al. Improved survival of patients with hepatocellular carcinoma and disparities by age, race, and socioeconomic status by decade, 1983–2012. Oncotarget 7, 59820–59833, doi:10.18632/oncotarget.10930 (2016).
Sun, H., Ma, H., Hong, G., Sun, H. & Wang, J. Survival improvement in patients with pancreatic cancer by decade: a period analysis of the SEER database, 1981–2010. Scientific reports 4, 6747, doi:10.1038/srep06747 (2014).
Ou, S. H., Ziogas, A. & Zell, J. A. Prognostic factors for survival in extensive stage small cell lung cancer (ED-SCLC): the importance of smoking history, socioeconomic and marital statuses, and ethnicity. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 4, 37–43, doi:10.1097/JTO.0b013e31819140fb (2009).
Hamra, G. B. et al. Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect 122, 906–911, doi:10.1289/ehp.1408092 (2014).
Bray, F. I. & Weiderpass, E. Lung cancer mortality trends in 36 European countries: secular trends and birth cohort patterns by sex and region 1970–2007. Int J Cancer 126, 1454–1466, doi:10.1002/ijc.24855 (2010).
Thun, M., Peto, R., Boreham, J. & Lopez, A. D. Stages of the cigarette epidemic on entering its second century. Tob Control 21, 96–101, doi:10.1136/tobaccocontrol-2011-050294 (2012).
Youlden, D. R., Cramb, S. M. & Baade, P. D. The International Epidemiology of Lung Cancer: geographical distribution and secular trends. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 3, 819–831, doi:10.1097/JTO.0b013e31818020eb (2008).
Jemal, A. et al. Annual report to the nation on the status of cancer, 1975–2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst 100, 1672–1694, doi:10.1093/jnci/djn389 (2008).
Centers for Disease, C. & Prevention. State-specific trends in lung cancer incidence and smoking–United States, 1999–2008. MMWR Morb Mortal Wkly Rep 60, 1243–1247 (2011).
Cummings, K. M. & Proctor, R. N. The changing public image of smoking in the United States: 1964–2014. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology 23, 32–36, doi:10.1158/1055-9965.EPI-13-0798 (2014).
Wojtalla, A. et al. Targeting the phosphoinositide 3-kinase p110-alpha isoform impairs cell proliferation, survival, and tumor growth in small cell lung cancer. Clinical cancer research: an official journal of the American Association for Cancer Research 19, 96–105, doi:10.1158/1078-0432.CCR-12-1138 (2013).
Kim, Y. H. et al. Combined microarray analysis of small cell lung cancer reveals altered apoptotic balance and distinct expression signatures of MYC family gene amplification. Oncogene 25, 130–138, doi:10.1038/sj.onc.1208997 (2006).
George, J. et al. Comprehensive genomic profiles of small cell lung cancer. Nature 524, 47–53, doi:10.1038/nature14664 (2015).
Carvajal, L. A. & Manfredi, J. J. Another fork in the road–life or death decisions by the tumour suppressor p53. EMBO reports 14, 414–421, doi:10.1038/embor.2013.25 (2013).
Rudin, C. M. et al. Phase II study of single-agent navitoclax (ABT-263) and biomarker correlates in patients with relapsed small cell lung cancer. Clinical cancer research: an official journal of the American Association for Cancer Research 18, 3163–3169, doi:10.1158/1078-0432.CCR-11-3090 (2012).
Han, J. Y. et al. A phase 2 study of irinotecan, cisplatin, and simvastatin for untreated extensive-disease small cell lung cancer. Cancer 117, 2178–2185, doi:10.1002/cncr.25790 (2011).
Seckl, M. J. et al. Multicenter, Phase III, Randomized, Double-Blind, Placebo-Controlled Trial of Pravastatin Added to First-Line Standard Chemotherapy in Small-Cell Lung Cancer (LUNGSTAR). Journal of clinical oncology: official journal of the American Society of Clinical Oncology, JCO2016697391, 10.1200/JCO.2016.69.7391 (2017).
De Ruysscher, D. et al. Impact of thoracic radiotherapy timing in limited-stage small-cell lung cancer: usefulness of the individual patient data meta-analysis. Annals of oncology: official journal of the European Society for Medical Oncology 27, 1818–1828, doi:10.1093/annonc/mdw263 (2016).
Roberts, H. C. et al. Lung cancer screening with low-dose computed tomography: Canadian experience. Canadian Association of Radiologists journal=Journal l’Association canadienne des radiologistes 58, 225–235 (2007).
Eberth, J. M. et al. Lung cancer screening using low-dose CT: the current national landscape. Lung cancer 85, 379–384, doi:10.1016/j.lungcan.2014.07.002 (2014).
Jacobs, C. D. & Jafari, M. E. Early Results of Lung Cancer Screening and Radiation Dose Assessment by Low-dose CT at a Community Hospital. Clinical lung cancer. doi:10.1016/j.cllc.2017.01.011 (2017).
Sagawa, M. et al. Efficacy of low-dose computed tomography screening for lung cancer: the current state of evidence of mortality reduction. Surgery today. doi:10.1007/s00595-016-1438-x (2016).
Nadpara, P., Madhavan, S. S. & Tworek, C. Guideline-concordant timely lung cancer care and prognosis among elderly patients in the United States: A population-based study. Cancer epidemiology 39, 1136–1144, doi:10.1016/j.canep.2015.06.005 (2015).
Jarvis, M. J., Cohen, J. E., Delnevo, C. D. & Giovino, G. A. Dispelling myths about gender differences in smoking cessation: population data from the USA, Canada and Britain. Tob Control 22, 356–360, doi:10.1136/tobaccocontrol-2011-050279 (2013).
Perkins, K. A. Smoking cessation in women. Special considerations. CNS Drugs 15, 391–411, doi:10.2165/00023210-200115050-00005 (2001).
Jamal, A. et al. Current Cigarette Smoking Among Adults - United States, 2005-2015. MMWR Morb Mortal Wkly Rep 65, 1205–1211, doi:10.15585/mmwr.mm6544a2 (2016).
Blackstock, A. W. et al. Similar outcomes between African American and non-African American patients with extensive-stage small-cell lung carcinoma: report from the Cancer and Leukemia Group B. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 24, 407–412, doi:10.1200/JCO.2005.02.1436 (2006).
Krieger, N. et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? the Public Health Disparities Geocoding Project. Am J Epidemiol 156, 471–482, doi:10.1093/aje/kwf068 (2002).
Warren, J. L., Klabunde, C. N., Schrag, D., Bach, P. B. & Riley, G. F. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Medical care 40, IV-3–18, doi:10.1097/01.MLR.0000020942.47004.03 (2002).
Acknowledgements
This research was supported by the National Natural Science Foundation of China (81500030, 81560403) and the Natural Science Foundation of Guangdong Province (2016A030313272, 2016A030313277).
Author information
Authors and Affiliations
Contributions
Research design: H.S. and H.M. Data collection and drafting: H.M., J.T., S.W. and T.S. Statistical analysis: H.M., J.T., and S.W. Manuscript polishing: H.S., X.Z. (Zhibin Cheng) and Z.C. Building figures: T.S., H.M., J.L., J.T. and H.S. (Hongliu Sun) and X.Z. (Xiuling Zhou). Manuscript editing: S.W., J.T., C.Z. and H.Z. Manuscript revision: J.T., S.W., H.M. and H.S.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, S., Tang, J., Sun, T. et al. Survival changes in patients with small cell lung cancer and disparities between different sexes, socioeconomic statuses and ages. Sci Rep 7, 1339 (2017). https://doi.org/10.1038/s41598-017-01571-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-01571-0
This article is cited by
-
C-Myc protein expression indicates unfavorable clinical outcome in surgically resected small cell lung cancer
World Journal of Surgical Oncology (2024)
-
Pamiparib as consolidation treatment after concurrent chemoradiotherapy of limited-stage small cell lung cancer: a single-arm, open-label phase 2 trial
Radiation Oncology (2024)
-
Efficacy and safety of thoracic radiotherapy in extensive-stage small-cell lung cancer patients receiving first-line immunotherapy plus chemotherapy: a propensity score matched multicentre retrospective analysis
Radiation Oncology (2024)
-
Phase 1 study of pembrolizumab plus chemotherapy in Japanese patients with extensive-stage small-cell lung cancer
Investigational New Drugs (2024)
-
Comparison of efficacy and safety between PD-1 inhibitors and PD-L1 inhibitors plus platinum-etoposide as first-line treatment for extensive-stage small-cell lung cancer: a multicenter, real-world analysis
BMC Cancer (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.