Abstract
Breast cancer incidence and survival is high in Southeast Asia. As such, many women diagnosed with breast cancer are at risk of dying of other causes. Given the increased risk of cardiotoxicity induced by breast cancer treatments, it is important to identify patients at high risk of cardiovascular disease (CVD) mortality. The aim of this study was to investigate if this risk varies by age and ethnicity. Patient details were obtained from 5,868 Chinese, Malay, and Indian women diagnosed with in situ or non-metastasized invasive breast cancer at the National University Hospital of Singapore and KK Women’s and Children’s Hospital in Singapore. Death causes were obtained from the National Registry of Births and Deaths. Flexible parametric survival models estimated CVD mortality rates and hazard ratios. During a median follow-up of six years, 1,010 deaths occurred of which 6.8% were due to CVD. CVD mortality rates of older women peaked within the first year following diagnosis and increased over time since diagnosis. Indian had more than double the risk of CVD mortality than Chinese, independent of age at diagnosis and stage. Taking ethnicity and age into account may promote CVD risk stratification and management in (Southeast Asian) women with breast cancer.
Similar content being viewed by others
Introduction
Breast cancer incidence is rising dramatically in Southeast Asia, which, in combination with improved survival rates due to earlier detection and improved treatments, leads to an increasing number of women living with or after breast cancer1, 2. Many of these women are at risk of dying of other causes than breast cancer3,4,5,6. Breast cancer patients treated with adjuvant treatments such as radiotherapy or chemotherapy may be at increased absolute risk of treatment-induced cardiac toxicity, and therefore, to develop CVD7,8,9,10. As such, CVD is now an important cause of death among women with breast cancer, with up to 10% of breast cancer patients dying of CVD4,5,6.
In the multi-ethnic population of Southeast Asia, comprising mainly of Chinese, Malay and Indian, there are ethnic differences in breast cancer survival11. Malay breast cancer patients have a higher risk of overall death following breast cancer compared to Chinese, regardless of age at diagnosis, tumor and treatment characteristics11. Furthermore, ethnic differences in severity of and death due to CVD is observed in high risk Southeast Asian patients, though not in breast cancer patients, with lowest severity of CVD in Chinese and highest CVD-specific mortality rates in Malay12, 13.
Given the increased risk of cardiac toxicity induced by breast cancer treatments, it is important to identify patients at high risk of CVD mortality. Taking the risk (factors) of CVD into account with breast cancer treatment decision will promote personalized CVD risk stratification and management of (Southeast Asian) breast cancer patients.
The objective of the present study was to investigate the risk of CVD mortality following breast cancer in Southeast Asia, and to assess if these risks vary by age at diagnosis and ethnicity.
Methods and Materials
Cohort study
This prospective cohort study was conducted within the context of two hospital-based breast cancer registries from the National University Hospital (NUH) in Singapore and KK Women’s and Children’s Hospital (KKH) in Singapore. All methods were carried out in accordance with the guidelines and regulations of NUH and KKH. The NUH received ethic approval from the National Healthcare Group Domain Specific Review Board and KKH received approval from SingHealth Centralized Institutional Review Board. The need for informed consent from all patients was waived by these ethics review boards.
The NUH breast cancer registry contains data of all 4,122 women diagnosed with breast cancer between 1990 and 2011. Details of the registry have been described elsewhere14. Data were collected retrospectively for 492 patients diagnosed between 1990 and 1995, and prospectively for 3,630 patients diagnosed after 1995. The KKH breast cancer registry contains prospectively collected data of all 2,192 women diagnosed with breast cancer between 2005 and 2015. Both registries from NUH and KKH include data on patient’s socio-demographic characteristics, tumor and treatment profile.
For the present study, breast cancer patients with distant metastases at diagnosis (n = 431) were excluded, leaving 5,868 women with in situ or non-metastasized invasive breast cancer. Ethnicity was categorized into four groups: Chinese, Malay, Indian and other (e.g. Eurasian, Caucasian). Other variables of interest included age at diagnosis, year of diagnosis, tumor stage at diagnosis according to the classification of malignant tumors (TNM)15, tumor differentiation (good, moderate, poor, unknown), estrogen receptor status (positive >1% of tumor cells expressing estrogen receptors, negative, unknown), breast cancer treatment including surgery (yes, no, unknown), chemotherapy (yes, no, unknown), radiotherapy (yes, no, unknown) and hormonal therapy (yes, no, unknown).
Outcomes
For the NUH breast cancer registry, information on vital status and cause of death was obtained from the National Registry of Births and Deaths in Singapore on April 30, 2015, and was complete for all 3,841 breast cancer patients from NUH. For the KKH breast cancer registry, vital status of each patient was known until last clinical follow-up visit, and cause of death was verified from the National Registry of Births and Deaths in Singapore for patients who did not show up at the follow-up visit and could not be contacted. The National Registry of Births and Deaths has certificates on causes of death issued by doctors or authorized medical practitioners within 24 hours after death. Causes of death were classified according to the International Classification of Diseases (ICD) versions 8, 9 or 10 codes, and regrouped into: death as a result of CVD (ICD8: 390 to 459; ICD9: 390 to 459; ICD10: 100 to 199), death as a result of breast cancer (ICD8: 174; ICD9: 174; ICD10: C50), and death as a result of all other cause (all ICD codes except those already listed).
Statistical analysis
Demographics, tumor characteristics, treatment details and survival time were described for the total population and for the total number of deaths, deaths from CVD, deaths from breast cancer and deaths from all other cause within 10 years of diagnosis. Time at risk for specific causes of death (i.e. CVD, breast cancer, all other cause) was calculated as the minimum of time between date of breast cancer diagnosis and date of death, end of study (April 30, 2015), last clinical follow-up visit, or ten years post diagnosis, whichever occurred first.
Flexible parametric survival models were used to estimate both mortality rates and hazard ratios (HRs) for death from CVD, death from breast cancer, and death from all other cause within 10 years after diagnosis, using restricted cubic spline functions16. First, we estimated unadjusted mortality rates for death from CVD, breast cancer and all other cause within 10 years after diagnosis for age at diagnosis in three categories (<50, 50–69, ≥70 years). This model used three internal knots in total: two internal knots for the association between age at diagnosis in categories and follow-up time, and one knot for the time varying effect of age. Mortality rates were reported per 1,000 person-years using days as underlying time.
Second, (crude) HRs with 95% confidence intervals (CI) were estimated as a measure of association between the main determinant ethnicity – Chinese, Malay, and Indian; other ethnicities were excluded due to the small number of patients with heterogeneous origins (n = 104) – and outcomes (i.e. death from CVD, breast cancer, all other cause). These HRs are similar to those estimated by the Cox’s proportional hazard models. Flexible parametric survival models, however, have the ability to estimate the baseline mortality rates allowing the HRs to change over time. Crude HRs for determinants other than ethnicity and age at diagnosis were estimated in a similar manner. Those that were statistically significant were included in the multivariable model. Due to having only 67 CVD-specific deaths, the maximum degrees of freedom used was limited to six for CVD-specific mortality. The following models were used for the analysis: (1) CVD-specific mortality model which has zero internal knots assuming proportional hazards over 10 years of follow-up and is adjusted for age at diagnosis (per 10 year increase) and stage (in situ to stage II, stage III or unknown, women with unknown stage showed similar mortality risks as those with stage III), (2) breast cancer-specific mortality model which has two internal knots and is adjusted for age at diagnosis (per 10 year increase), categorized year of diagnosis (1990–2005, 2006–2010, 2011–2015), stage (in situ to stage II, stage III or unknown), tumor differentiation grade, chemotherapy, radiotherapy, and hormonal therapy, and (3) the model for all other cause-specific mortality which has zero internal knots and is adjusted for age at diagnosis (per 10 year increase), categorized TNM stage (in situ to stage II, stage III or unknown), and radiotherapy.
Results
Of the 5,868 women with breast cancer in the study, median age at diagnosis was 52 years (interquartile range: 45–60) and median follow-up was six years (interquartile range: 3–10) (Table 1). Of these women, 79% (n = 4,663) were Chinese, 12% (n = 694) were Malay, 6% (n = 351) were Indian, and 3% (n = 160) were women with another ethnicity. The majority of women (86%, n = 5,024) were diagnosed with breast cancer after 1999. Thirteen percent of women (n = 764) were diagnosed with carcinoma in situ, 24% (n = 1,381) with stage I, 37% (n = 2,181) with stage II, 13% (n = 756) with stage III, and stage was unknown for 13% (n = 786).
In total, 1,010 deaths occurred within 10 years of follow-up of which 6.8% (n = 67) were due to CVD (Table 1). Of these, 24 deaths were due to acute myocardial infarction, 4 deaths were due to congestive heart failure, 16 deaths were due to acute ischemic heart disease, 3 deaths were due to coronary artery disease, 11 deaths were due to cerebrovascular death (anoxic brain damage), and 9 deaths were due to other heart disease problems (cardiorespiratory failure) (data not presented). The most common cause of death was breast cancer accounting for 76.6% (n = 774) of all deaths, and in 16.7% (n = 169), death was due to other causes than breast cancer or CVD. Of the 740 Chinese women with breast cancer who died, 6.8% (n = 50) died of CVD, 75.0% (n = 555) died of breast cancer, and 18.2% (n = 135) died of other causes. Of the 178 Malay women with breast cancer who died, 4.4% (n = 8) died of CVD, 86.0% (n = 153) died of breast cancer, and 9.6% (n = 47) died of other causes. Furthermore, of the 61 Indian women with breast cancer who died, 13.1% (n = 8) died of CVD, 77.0% (n = 47) died of breast cancer, and 9.9% (n = 6) died of other causes.
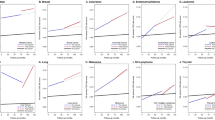
Among women over 70 years at breast cancer diagnosis, CVD mortality rates peaked in the first year after diagnosis followed by a decrease until approximately three years after breast cancer diagnosis (Fig. 1). Thereafter, CVD mortality rates rose until approximately 12 per 1,000 person-years after 10 years of follow-up. CVD mortality rates among women aged 50 to 69 years at breast cancer diagnosis gradually increased with follow-up until approximately 4 per 1,000 person-years after 10 years of follow-up. In women younger than 50 years, CVD mortality remained almost constant at less than 1 per 1,000 person years during the 10 years of follow-up. Breast cancer-specific mortality rates peaked at one to three years after diagnoses for all breast cancer patients. Women over 70 years had substantially higher breast cancer specific mortality rates within the first five years after diagnosis than younger women. After eight years since diagnosis, similar breast cancer-specific mortality rates (approximately 20 per 1,000 person-years) were seen in all age groups. Mortality rates from other causes were highest among women aged over 70 years, and showed an early peak within the first year after breast cancer diagnosis followed by a steady increase over time until approximately 25 per 1,000 person-years after ten years of follow-up. In the younger age groups, mortality rates from other causes remained stable over follow-up time at approximately five per 1,000 person-years for women aged between 50 and 69 years and less than one per 1,000 person-years for women younger than 50 years.
Estimated mortality rates within 10 years of diagnosis in Southeast Asian women with breast cancer diagnosed between 1990 and 2011 (mortality rates estimated from flexible parametric survival models with age as only covariate, allowing age effect to vary by time since diagnosis). Death due to (a) cardiovascular disease, (b) breast cancer, (c) all other cause.
The risk of death from CVD within 10 years of diagnosis in Indian women was more than double the risk of Chinese women (HR = 2.5, 95% CI = 1.2–5.2), independent of age at diagnosis and stage (Table 2). Furthermore, the risk of death from breast cancer in Malay women was almost double the risk of Chinese women (HR = 1.9, 95% CI = 1.6–2.3) independent of age at diagnosis, tumor stage, tumor differentiation grade, chemotherapy, radiotherapy, and hormonal therapy.
Discussion
Breast cancer survival is improving in Southeast Asia. As such, the number of breast cancer survivors at risk of dying of other causes is increasing. Given the increased risk of cardiac toxicity induced by breast cancer treatments, it is important to identify patients at high risk of CVD mortality.
The present study shows that the risk of CVD mortality following breast cancer in multi-ethnic Southeast Asia is generally low during the first decade after diagnosis. Breast cancer is still the main cause of death. The risk of CVD mortality is increased in women with higher age at breast cancer diagnosis and in Indian women.
Among women with a higher age at breast cancer diagnosis, CVD mortality rates peak within the first year following diagnosis and show an overall increase during the ten years of follow-up. Similar results have been reported among Caucasian women with breast cancer4. Our unadjusted survival analysis show that women who have been treated with chemotherapy or radiotherapy have a lower risk of dying of CVD than women who did not receive those therapies. Moreover, women with a positive estrogen receptor status have a higher risk of dying of CVD than women with a negative receptor status. A possible explanation is the phenomenon is that women with breast cancer who receive chemotherapy, radiotherapy, and/or have a negative estrogen receptor status have a higher TNM stage and therefore die more often due to breast cancer than due to CVD. Also, some selection may have taken place, as women who are at increased risk of CVD are less likely to be treated with cardiac toxic chemotherapy or (left-sided) radiotherapy. Furthermore, our study shows that Indian women have an increased risk of CVD mortality following breast cancer compared to Chinese women. Variation in the risk of CVD mortality by ethnicity in our population may be due to genetic differences and/or differences in lifestyle associated comorbidities like obesity and diabetes and dietary habits17, 18. Differences in the presence of CVD risk factors between Chinese, Malay and Indian in Southeast Asia have been reported17, 19,20,21,22. Indian women have the highest rate of central obesity and diabetes21, while the rate of obesity is highest among Malay followed by Indian and Chinese19, 20. These differences, however, are not fully explained by dietary intake23. Moreover, Indians have the highest level of lipoprotein a, which is a causal genetic risk factor for cardiovascular disease22.
In the current study, CVD mortality rates of women with breast cancer aged over 70 years were over 10 per 1,000 person-years shortly after diagnosis until 10 years after diagnosis, however, CVD mortality rates of women from the general population in Singapore aged over 70 years ranged from 19 per 1,000 person-years in 2005 to 17 per 1,000 person-years in 2015 (data not presented)24. Furthermore, in this study, CVD mortality rates of women with breast cancer aged 50 to 69 years were approximately 0.3 per 1,000 person-years throughout the 10 years follow-up while the CVD mortality rates of women from the general population in Singapore aged 50 to 69 years ranged from 1.4 per 1,000 person-years in 2005 to 0.9 per 1,000 person-years in 2015 (data not presented)24. These numbers show that mortality rates of CVD among women with breast cancer patients in Singapore are somewhat lower than that of women from the general population in Singapore.
In the present study, CVD mortality rates increase over time while breast cancer mortality rates decrease after three years since diagnosis. Colzani et al. found similar results among Caucasian women with breast cancer: CVD-specific mortality rates increase after three years since diagnoses in women aged over 55 years at diagnosis, while breast cancer-specific mortality rates decreased after four years since diagnosis among all ages4. These results are not surprising as age is a well-known important risk factor of CVD25, and the majority of deaths from breast cancer within the first four years following diagnosis in our prospective cohort were women diagnosed with more severe stages i.e. II and III.
We acknowledge that the present study has limitations. The follow-up time of our study population was relatively short, which explains (part of) the low absolute risk of CVD mortality. Previous research has shown, that the risk of CVD mortality increases up to and beyond 20 years after diagnosis4, 26, 27, as age is a well-known CVD risk factor28 and cardiac toxicity induced by radiotherapy manifest itself many years following treatment29, 30. Furthermore, misclassification of cause of death due to CVD could have occurred, especially in cases of sudden death from CVD outside a hospital, for example at home, were it is difficult to state the proper cause of death by doctors or authorized medical practitioners that are not familiar with this particular women.
In conclusion, the risk of CVD mortality is generally low in the first decade following breast cancer diagnosis in Southeast Asia. Women with higher age at breast cancer diagnosis and Indian women are at increased risk of CVD mortality following breast cancer. The notion that women who survive breast cancer will subsequently be at risk for CVD is important in their management and in addition, taking ethnic-specific risks and age into account, may promote optimal prevention of CVD in (Southeast Asian) women with breast cancer. Future research may assess factors, dependent or independent of breast cancer, explaining the variation in risk of CVD mortality according to ethnicity. Furthermore, breast cancer patients would benefit from a personalized CVD risk prediction short after breast cancer diagnosis so that treatment can be adjusted accordingly and CVD management can be initialized.
References
Lim, G. H., Chow, K. Y. & Lee, H. P. Singapore cancer trends in the last decade. Singapore Med. J. 53, 3–9; quiz 10 (2012).
Youlden, D. R., Cramb, S. M., Yip, C. H. & Baade, P. D. Incidence and mortality of female breast cancer in the Asia-Pacific region. Cancer. Biol. Med 11, 101–115, doi:10.7497/j.issn.2095-3941.2014.02.005 (2014).
Riihimaki, M., Thomsen, H., Brandt, A., Sundquist, J. & Hemminki, K. Death causes in breast cancer patients. Ann. Oncol. 23, 604–610, doi:10.1093/annonc/mdr160 (2012).
Colzani, E. et al. Prognosis of patients with breast cancer: causes of death and effects of time since diagnosis, age, and tumor characteristics. J. Clin. Oncol 29, 4014–4021, doi:10.1200/JCO.2010.32.6462 (2011).
Berkman, A. et al. Racial differences in breast cancer, cardiovascular disease, and all-cause mortality among women with ductal carcinoma in situ of the breast. Breast Cancer Res. Treat. 148, 407–413, doi:10.1007/s10549-014-3168-3 (2014).
Bradshaw, P. T. et al. Cardiovascular Disease Mortality Among Breast Cancer Survivors. Epidemiology (2015).
Bird, B. R. & Swain, S. M. Cardiac toxicity in breast cancer survivors: review of potential cardiac problems. Clin. Cancer Res 14, 14–24, doi:10.1158/1078-0432.CCR-07-1033 (2008).
Borger, J. H. et al. Cardiotoxic effects of tangential breast irradiation in early breast cancer patients: the role of irradiated heart volume. Int. J. Radiat. Oncol. Biol. Phys 69, 1131–1138, doi:10.1016/j.ijrobp.2007.04.042 (2007).
McGale, P. et al. Incidence of heart disease in 35,000 women treated with radiotherapy for breast cancer in Denmark and Sweden. Radiother. Oncol. 100, 167–175, doi:10.1016/j.radonc.2011.06.016 (2011).
Pinder, M. C., Duan, Z., Goodwin, J. S., Hortobagyi, G. N. & Giordano, S. H. Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J. Clin. Oncol. 25, 3808–3815, doi:10.1200/JCO.2006.10.4976 (2007).
Bhoo-Pathy, N. et al. Ethnic differences in survival after breast cancer in South East Asia. PLoS One 7, e30995, doi:10.1371/journal.pone.0030995 (2012).
de Carvalho, L. P. et al. Differences in late cardiovascular mortality following acute myocardial infarction in three major Asian ethnic groups. Eur. Heart J. Acute Cardiovasc. Care 3, 354–362, doi:10.1177/2048872614527007 (2014).
Gijsberts, C. M. et al. Inter-Ethnic Differences in Quantified Coronary Artery Disease Severity and All-Cause Mortality among Dutch and Singaporean Percutaneous Coronary Intervention Patients. PLoS One 10, e0131977, doi:10.1371/journal.pone.0131977 (2015).
Lim, S. E. et al. Clinical observations from a breast cancer registry in Asian women. World J. Surg. 31, 1387–1392, doi:10.1007/s00268-007-9086-3 (2007).
Edge, S. B., Byrd, D. R. & Compton, C. C. AJCC Cancer Staging Manual (ed 7) Springer. (New York, NY, 2010).
Royston, P. & Parmar, M. K. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat. Med. 21, 2175–2197, doi:10.1002/sim.1203 (2002).
Jacobson, T. A. Lipoprotein(a), cardiovascular disease, and contemporary management. Mayo Clin. Proc. 88, 1294–1311, doi:10.1016/j.mayocp.2013.09.003 (2013).
Sasayama, S. Heart disease in Asia. Circulation 118, 2669–2671, doi:10.1161/CIRCULATIONAHA.108.837054 (2008).
Pan, A., Malik, V. S. & Hu, F. B. Exporting diabetes mellitus to Asia: the impact of Western-style fast food. Circulation 126, 163–165, doi:10.1161/CIRCULATIONAHA.112.115923 (2012).
Deurenberg-Yap, M. et al. Can dietary factors explain differences in serum cholesterol profiles among different ethnic groups (Chinese, Malays and Indians) in Singapore? Asia Pac. J. Clin. Nutr. 10, 39–45, doi:10.1046/j.1440-6047.2001.00202.x (2001).
Hughes, K. et al. Cardiovascular diseases in Chinese, Malays, and Indians in Singapore. II. Differences in risk factor levels. J. Epidemiol. Community Health 44, 29–35, doi:10.1136/jech.44.1.29 (1990).
Hughes, K., Aw, T. C., Kuperan, P. & Choo, M. Central obesity, insulin resistance, syndrome X, lipoprotein(a), and cardiovascular risk in Indians, Malays, and Chinese in Singapore. J. Epidemiol. Community Health 51, 394–399, doi:10.1136/jech.51.4.394 (1997).
Mak, K. H. et al. Ethnic differences in acute myocardial infarction in Singapore. Eur. Heart J. 24, 151–160, doi:10.1016/S0195-668X(02)00423-2 (2003).
Institute for Health Metrics and Evaluation (IHME). GDB Compare Data. http://vizhub.healthdata.org/gbd-compare/ (2016).
D’Agostino, R. B. S. et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 117, 743–753, doi:10.1161/CIRCULATIONAHA.107.699579 (2008).
Darby, S. C., McGale, P., Taylor, C. W. & Peto, R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol. 6, 557–565, doi:10.1016/S1470-2045(05)70251-5 (2005).
EBCTCG (Early Breast Cancer Trialists’ Collaborative Group). et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet 383, 2127–2135, doi:10.1016/S0140-6736(14)60488-8 (2014).
Tsao, C. W. & Vasan, R. S. Cohort Profile: The Framingham Heart Study (FHS): overview of milestones in cardiovascular epidemiology. Int. J. Epidemiol. 44, 1800–1813, doi:10.1093/ije/dyv337 (2015).
Darby, S. C. et al. A dose-response relationship for the incidence of radiation-related heart disease. Int. J. Radiat. Oncol. Biol. Phys. 78, S49–S50, doi:10.1016/j.ijrobp.2010.07.151 (2010).
Cuomo, J. R., Sharma, G. K., Conger, P. D. & Weintraub, N. L. Novel concepts in radiation-induced cardiovascular disease. World J. Cardiol. 8, 504–519, doi:10.4330/wjc.v8.i9.504 (2016).
Acknowledgements
We thank Marleen Emaus for critically reviewing the manuscript.
Author information
Authors and Affiliations
Contributions
Data collection from the National University Hospital of Singapore was conducted by P.J.H., H.M.V. and M.H., who conceived and coordinated this registry. S.H.L. was involved in obtaining the data from the KK Women’s and Children’s Hospital. S.A.M.G., P.J.H., H.M.V. and M.H. designed the study. P.J.H. and S.A.M.G. performed the statistical data analysis. S.A.M.G., P.J.H., N.R. and H.M.V. wrote the manuscript. All authors were involved in data interpretation, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gernaat, S.A.M., Ho, P.J., Rijnberg, N. et al. Risk of death from cardiovascular disease following breast cancer in Southeast Asia: a prospective cohort study. Sci Rep 7, 1365 (2017). https://doi.org/10.1038/s41598-017-01540-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-01540-7
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.