Abstract
The purpose of this meta-analysis was to compare the efficacy and safety of regional anesthesia to manage chronic postsurgery pain. A systematic search of PubMed, EmBase, and the Cochrane Central Register of Controlled Trials was performed to identify randomized controlled trials that focused on chronic pain frequency, analgesic consumption, and adverse effects under different surgical categories. We collected 21 trials assessing 1,980 patients for our meta-analysis. The summary of relative risks (RRs) and standard mean differences (SMDs) were calculated to measure the treatment effect of regional anesthesia. Results indicated that regional anesthesia significantly reduced the frequency of postsurgery pain (RR, 0.69; 95% confidence interval [CI], 0.56–0.85; p < 0.001). The results showed significant differences in overall patient satisfaction between applications with and without regional anesthesia (SMD, 1.95; 95%CI, 0.83–3.06; p = 0.001); however in other results, there were no significant differences between the two groups. Subgroup analysis suggested that regional anesthesia treatment might differ according to country. In conclusion, our study indicated that regional anesthesia was effective and safe in reducing the frequency of postsurgery pain and improved overall patient satisfaction; however, studies on the long-term efficacy and safety of regional anesthesia are still required to further confirm these findings.
Similar content being viewed by others
Introduction
Postsurgery pain is a major medial challenge for patients and clinical staff and results in physical discomfort, psychological harm, and hormonal disturbances1. The major causes for postsurgery pain are tissue injury, residual pneumoperitoneum, and phrenic neuropraxia2. The incidence of acute neuropathic pain in patients within days after surgery ranged from 1.0 to 3.0%, and acute postsurgery neuropathic pain persisting for ≥3.0 months was regarded as chronic3, 4. Patients undergoing various surgical procedures and those receiving adequate postsurgery analgesia should have a lower result on the visual analog scale (VAS) and better endocrine response, which, in turn, could accelerate wound recovery5. Further, postsurgery regional analgesia is widely used for pain control. It improves analgesic efficacy and reduces the need for opioids for pulmonary and gastrointestinal dysfunction and, thus, their side effects5,6,7.
Opioids are most commonly used to manage postsurgery pain, but are frequently associated with adverse effects, such as respiratory depression, drug addiction, and nausea and vomiting8,9,10; therefore, an additional effective analgesic approach must be found. Regional analgesia has been clearly shown to be effective in reducing postsurgery pain, and has been associated with less adverse effects than opioids11,12,13,14. In addition, regional anesthesia, such as epidurals, are used in procedures involving specific wound entry sites. Because of the advances in regional analgesia, it has been recommended as an alternative to opioids for controlling postsurgery pain. Previous meta-analyses studies evaluated the effects of regional analgesia on specific surgical sites15,16,17; however, comprehensive evaluation of the effects in preventing chronic postsurgery pain over that of traditional analgesics remains controversial.
Regional analgesia is effective in pain management and reduces the consumption of opioids, but a clear comparison of the differences in long-term pain control between regional and traditional analgesics is needed. Hence, in this study, we evaluated the efficacy and safety of regional analgesia in preventing postsurgery chronic pain. In addition, we compared the treatment effects of regional analgesia among patients after surgery who had different baseline characteristics.
Results
Literature search
The study retrieved 598 articles from PubMed, 942 from EmBase, and 263 from the Cochrane Library database and 1,036 articles were identified after removing the duplicates. Of these, 995 articles were excluded because of irrelevance after scanning the titles and abstracts. Additional full-text articles were reviewed and 20 more studies were excluded. Finally, 21 trials assessing 1,980 patients were collected for our systematic review18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38. The search process was showed in flow chart (Fig. 1).
Study characteristics
The surgical type, including general, orthopedic, gynecological, and thoracotomy, were analyzed. Regional anesthesia methods included epidural, wound infusion, topical application, plexus blocks, spinal blocks, peritoneal instillation, and paravertebral blocks. The major effects measured were pain frequency, analgesia consumption, pain scale, and adverse effects. The follow-up duration ranged from 3.0 months to 4.7 y. According to Jadad scores, all studies were within the range of 1 to 4, so the overall quality of the included studies was not ideal (Table 1).
Analysis results
The results reported that postsurgery pain frequency was significantly reduced in the 19 patients who underwent major surgery with regional anesthesia (RR, 0.69; 95%CI, 0.56–0.85; p < 0.001; Fig. 2); however, moderate heterogeneity was observed among the included studies (I2, 50.1%, p = 0.007). A sensitivity analysis showed that the results were not affected after sequentially excluding each trial. Subgroup analysis of pain frequency showed no significant differences between regional and traditional anesthesia in the trials conducted in Europe, sample size >100, and at surgery sites other than thoracotomy or laparotomy. In addition, RRR showed a statistically significant different effect of regional and traditional anesthesia on pain frequency in trials conducted in Europe when compared to trials conducted in other countries (Table 2).
In addition, other bivariate outcomes (Fig. 3) from aggravating factors causing pain, such as carrying heavy objects (RR, 0.47; 95%CI, 0.21–1.07; p = 0.072), coughing (RR, 0.98; 95%CI, 0.69–1.41; p = 0.932), emotional stress (RR, 0.44; 95%CI, 0.08–2.27; p = 0.325), sitting up from a prone position (RR, 1.31; 95%CI, 0.81–2.12; p = 0.265), taking a deep breath (RR, 0.58; 95%CI, 0.10–3.33; p = 0.544), touching the wound (RR, 1.03; 95%CI, 0.52–2.06; p = 0.924), and walking (RR, 1.19; 95%CI, 0.68–2.06; p = 0.542), showed no significant differences between the regional and no anesthesia groups. The above results were based mainly on the 2004 Katz study18 in which there was no statistical difference in the number of patients who needed analgesics regardless of whether regional anesthesia was used (RR, 0.42; 95%CI, 0.15–1.14; p = 0.090).
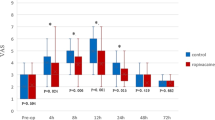
The overall satisfaction of the continuous variable outcomes (Fig. 4) showed significant differences between the groups (SMD, 1.95; 95%CI, 0.83–3.06; p = 0.001). Other outcomes, such as analgesic consumption (SMD, −1.89; 95%CI, −4.92–1.14; p = 0.221), current pain intensity based on the McGill index (SMD, −0.34; 95%CI, −0.71–0.03; p = 0.076), number of words chosen (SMD, −0.09; 95%CI, −0.45–0.28; p = 0.649), pain rating index (SMD, 0.07; 95%CI, −0.26–0.39; p = 0.692), mental health inventory-18 (SMD, −0.14; 95%CI, −0.55–0.28; p = 0.519), pain disability index (SMD, −0.05; 95%CI, −0.46–0.37; p = 0.830), VAS (SMD, −0.44; 95%CI, −1.03–0.14; p = 0.140), worst pain since discharge (SMD, −0.37; 95%CI, −0.79–0.04; p = 0.080), and functional activity score (SMD, −0.34; 95%CI, −1.25–0.57; p = 0.462), showed no significant differences between the regional and no anesthesia groups.
A review of the funnel plots could not rule out the potential for publication bias of pain frequency (Fig. 5). Although the Begg’s test showed no evidence of publication bias for pain frequency (P = 0.401), a significant publication bias was detected using the Egger’s test (P = 0.004). The conclusions were not changed after adjustment for publication bias using the trim and fill method39.
Discussion
Our meta-analysis was based on 21 RCTs, which included regional anesthesia for the prevention of chronic pain after major surgery. This large quantitative study included 1,980 patients with a broad range of populations. We found that regional anesthesia could significantly reduce postsurgery pain frequency and improve overall patient satisfaction. Subgroup analysis showed significant differences between regional and traditional anesthesia and was country specific. Regional anesthesia technology has been used extensively for multimodal anesthesia since it was developed; however, large numbers of studies supported the limitations on its effects and complications; therefore, researchers have begun to question the superiority of regional anesthesia on postsurgery pain. Epidural anesthesia has had an ideal postsurgery analgesic effect with less impacts on respiratory and gastrointestinal functions; however, during major surgeries, especially during joint replacement surgery, routine anticoagulants are used to prevent lower limb venous thrombosis, which would significantly increase the risk of iatrogenic epidural bleeding and limits epidural anesthesia application in major orthopedic surgeries. Others techniques, such as local nerve blocks, were widely accepted in surgeries and could reduce the amount of analgesic drugs with fewer complications; however, its area of action is less compared to that of epidural anesthesia and was frequently used in only minor orthopedic surgeries. In addition, the duration of this technique is relatively short, and whether it extends the blockade time or increases the frequency to improve the analgesic effect still needs further research. Local infiltration anesthesia blocks opioid receptors in the inflamed tissues to increase the overall effect of anesthesia; however, this method is used more in minor surgeries, such as breast surgery and hernia repair, and, at times, in major orthopedic surgeries as an additional and important component of multimodal anesthesia, but whether local infiltration anesthesia significantly prevents postsurgery pain must still be confirmed. Although regional anesthesia as part of multimodal anesthesia is gradually being accepted by researchers, controversies exist in clinical practice. Our study systematically analyzed whether the combined application of regional anesthesia could improve postsurgery pain, and the results indicated that regional anesthesia has significant advantages in postsurgery pain frequency and overall satisfaction; however, there was insufficient data for robust conclusions based on other study results.
Most of our secondary findings were in agreement with the trial conducted in Canada18, which comprised 83 patients who underwent major gynecological surgery by laparotomy. The results showed that although patients who received epidural analgesia had fewer disabilities 3.0 weeks after surgery, there was no significant impact on chronic pain frequency, which might have been because of their baseline and postsurgery measurements, such as psychological, emotional, and physical variables. Senturk et al.24, in their clinically, randomized, prospective study, suggested that patients who received thoracic epidural analgesia before the initiation of surgery showed no acute and long-term thoracotomy pain. In contrast, Shahin et al.27 indicated that intraperitoneal instillation decreased the incidence and scores of postcesarean pain after the parietal peritoneum was sutured. Strazisar et al.33 illustrated that wound infusion with a regional anesthetic reduced acute and chronic pain and opioid consumption, and also resulted in less postsurgery sedation and the need for antiemetics. Most of the trials showed no significant differences in chronic pain frequency, which might have been because of the trial design with acute pain control as the primary endpoint and the relatively small sample sizes, which did not allow the adequate statistical ability to detect potential clinical differences; therefore, large-scale RCTs should be conducted to verify the treatment effects on chronic pain.
Significant differences between Europe and other countries were observed for the effect of regional analgesia on chronic pain frequency. These results were somewhat surprising and the reasons remain unclear, but it is possible that the surgery sites and dosage of analgesics might play an important role in this difference. Most trials conducted in Europe included patients who underwent major surgeries, which might have required multimodal anesthesia to alleviate acute and chronic pain. The results of our data varied from that of other studies. Although fewer trials provided data about the pain scale, analgesia consumption, and adverse events, variable conclusions were reached.
Conclusions
Regional analgesia significantly reduced the incidence in patients of chronic postsurgery pain at different surgery sites compared to that with traditional analgesia, but the analgesic efficacy of regional analgesia might not be similar in studies conducted in different countries. Future trials that focus on the long-term efficacy of regional analgesia in specific populations, including the characteristics of patients, are warranted.
Study Limitations
Our meta-analysis had several limitations. First, the results were based on other studies, but not at the individual level. Second, there was relatively high heterogeneity in our analysis; therefore, the random-effects model was used to take possible heterogeneity into consideration. In addition, subgroup analyses were conducted based on the publication year, country, sample size, surgical sites, and follow-up duration to further explore the source of heterogeneity; however, unexplained heterogeneity also persisted, which might have been from the varying use of combined analgesia, different disease status, and surgical approaches. Third, the results of the data on most of the outcomes were too small to reach robust conclusions. Finally, the quality and reliability of our results might be limited by the quality of the underlying data. In the future, it is highly recommended that unified results for assessing the criteria are found, especially in small-sample studies.
Materials and Methods
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement40.
Search strategy and study selection
We conducted a literature search of PubMed, EmBase, and the Cochrane Central Register of Controlled Trials databases for articles published up to July 2016 using the following core search terms: “Anesthesia”, “Anesthetics”, “Analgesia”, “regional”, “local”, “Pain”, and “Postoperative”. The potential eligible studies with the titles and abstracts were reviewed to identify additional candidate studies, the reference lists of the included studies, and reviews.
Two authors independently extracted data from the literature search using a standardized approach. In the case of inconsistencies between these two authors, a consensus was reached by group discussion. The inclusion criteria were as follows: 1. randomized controlled trial studies; 2. studies focused on prevention and treatment of chronic postsurgery pain under different surgical categories; 3. study reports at least one outcome, such as pain frequency, pain scale, analgesic consumption, and adverse events; 4. studies published in English; and 5. a follow-up >30 d. The exclusion criteria were reviews, editorials, non-human studies, letters, and conference papers without sufficient data.
Data collection and quality assessment
Two reviewers independently extracted data, and the disagreements were resolved by consensus with a third-party investigator. The following items were extracted from the included articles: author, country, sample size, patient status, regional technique, outcomes, and follow-up duration. A quality assessment was independently performed by two authors using an established tool, the Jadad scale, in the following five domains: randomization (1 or 0), concealment of treatment allocation (1 or 0), blinding (1 or 0), completeness of follow-up (1 or 0), and the use of intention-to-treat analysis (1 or 0)41. The studies were scored based on these results, which were then used to assess the methodological quality of clinical trials.
Statistical analyses
A random-effects model was used to pool continuous data because of the high clinical heterogeneity among the studies and the results are presented as the standardized mean difference (SMD) and 95% confidence interval (CI) using the inverse variance method. Dichotomous data and results were summarized using risk ratio (RR) and 95% CIs using the Mantel-Haenszel method42, 43. Heterogeneity among studies was investigated using Q statistics, and P < 0.10 indicated significant heterogeneity44, 45. Subgroup analyses were conducted to assess the pain frequency on the basis of publication year, country, sample size, surgical sites, and follow-up duration. The relative risk ratios (RRRs) and the corresponding 95% CIs for pain frequency were estimated based on the publication year, country, sample size, surgical sites, and follow-up duration46. A sensitivity analysis was performed by removing each individual trial to evaluate the influence of each included study47. Egger48 and Begg’s49 tests were conducted and funnel plots created to check for any potential publication bias. All tests were two tailed, and p < 0.05 was considered statistically significant. We analyzed the data using STATA ver. 12.0 (StataCorp LLC, College Station, TX, USA).
References
Cassady, J. F. Jr., Lederhaas, G., Cancel, D. D., Cummings, R. J. & Loveless, E. A. A randomized comparison of the effects of continuous thoracic epidural analgesia and intravenous patient-controlled analgesia after posterior spinal fusion in adolescents. Reg Anesth Pain Med 25, 246–253 (2000).
Wills, V. L. & Hunt, D. R. Pain after laparoscopic cholecystectomy. Br J Surg 87, 273–284 (2000).
Akkaya, T. & Ozkan, D. Chronic post-surgical pain. Agri 21, 1–9 (2009).
Hayes, C., Browne, S., Lantry, G. & Burstal, R. Neuropathic pain in the acute pain service: A prospective study. Acute Pain 4, 45–8 (2002).
Block, B. M. et al. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA 290, 2455–2463 (2003).
Fotiadis, R. J., Badvie, S., Weston, M. D. & Allen-Mersh, T. G. Epidural analgesia in gastrointestinal surgery. Br J Surg 91, 828–841 (2004).
Shapiro, A. et al. A comparison of three techniques for acute postoperative pain control following major abdominal surgery. J Clin Anesth 15, 345–350 (2003).
Sanders, M. et al. New Formulation of Sustained Release Naloxone Can Reverse Opioid Induced Constipation Without Compromising the Desired Opioid Effects. Pain Med 16, 1540–1550 (2015).
Jamal, M. M., Adams, A. B., Jansen, J. P. & Webster, L. R. A randomized, placebo-controlled trial of lubiprostone for opioid-induced constipation in chronic noncancer pain. Am J Gastroenterol 110, 725–732 (2015).
Takigawa, C. et al. Breakthrough pain management using fentanyl buccal tablet (FBT) in combination with around-the-clock (ATC) opioids based on the efficacy and safety of FBT, and its relationship with ATC opioids: results from an open-label, multi-center study in Japanese cancer patients with detailed evaluation. Jpn J Clin Oncol 45, 67–74 (2015).
De Pinto, M. et al. Regional anesthesia for management of acute pain in the intensive care unit. Int J Crit Illn Inj Sci 5, 138–143 (2015).
Gadsden, J. & Warlick, A. Regional anesthesia for the trauma patient: improving patient outcomes. Local Reg Anesth 8, 45–55 (2015).
Bauer, M. C., Pogatzki-Zahn, E. M. & Zahn, P. K. Regional analgesia techniques for total knee replacement. Curr Opin Anaesthesiol 27, 501–506 (2014).
Humble, S. R., Dalton, A. J. & Li, L. A systematic review of therapeutic interventions to reduce acute and chronic post-surgical pain after amputation, thoracotomy or mastectomy. Eur J Pain 19, 451–465 (2015).
Bamigboye, A. A. & Hofmeyr, G. J. Local anaesthetic wound infiltration and abdominal nerves block during caesarean section for postoperative pain relief. Cochrane Database Syst Rev, CD006954 (2009).
Shanthanna, H., Singh, B. & Guyatt, G. A systematic review and meta-analysis of caudal block as compared to noncaudal regional techniques for inguinal surgeries in children. Biomed Res Int 2014, 890626 (2014).
Atchabahian, A., Schwartz, G., Hall, C. B., Lajam, C. M. & Andreae, M. H. Regional analgesia for improvement of long-term functional outcome after elective large joint replacement. Cochrane Database Syst Rev, CD010278 (2015).
Katz, J. & Cohen, L. Preventive analgesia is associated with reduced pain disability 3 weeks but not 6 months after major gynecologic surgery by laparotomy. Anesthesiology 101, 169–174 (2004).
Lavand’homme, P., De Kock, M. & Waterloos, H. Intraoperative epidural analgesia combined with ketamine provides effective preventive analgesia in patients undergoing major digestive surgery. Anesthesiology 103, 813–820 (2005).
Lavand’homme, P. M., Roelants, F., Waterloos, H. & De Kock, M. F. Postoperative analgesic effects of continuous wound infiltration with diclofenac after elective cesarean delivery. Anesthesiology 106, 1220–1225 (2007).
Karanikolas, M. et al. Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: a prospective, randomized, clinical trial. Anesthesiology 114, 1144–1154 (2011).
Singh, K., Phillips, F. M., Kuo, E. & Campbell, M. A prospective, randomized, double-blind study of the efficacy of postoperative continuous local anesthetic infusion at the iliac crest bone graft site after posterior spinal arthrodesis: a minimum of 4-year follow-up. Spine (Phila Pa 1976) 32, 2790–2796 (2007).
Fassoulaki, A., Triga, A., Melemeni, A. & Sarantopoulos, C. Multimodal analgesia with gabapentin and local anesthetics prevents acute and chronic pain after breast surgery for cancer. Anesth Analg 101, 1427–1432 (2005).
Senturk, M. et al. The effects of three different analgesia techniques on long-term postthoracotomy pain. Anesth Analg 94, 11–15 (2002).
Bain, G. I., Rudkin, G., Comley, A. S., Heptinstall, R. J. & Chittleborough, M. Digitally assisted acromioplasty: the effect of interscalene block on this new surgical technique. Arthroscopy 17, 44–49 (2001).
Burney, R. E., Prabhu, M. A., Greenfield, M. L., Shanks, A. & O’Reilly, M. Comparison of spinal vs general anesthesia via laryngeal mask airway in inguinal hernia repair. Arch Surg 139, 183–187 (2004).
Shahin, A. Y. & Osman, A. M. Intraperitoneal lidocaine instillation and postcesarean pain after parietal peritoneal closure: a randomized double blind placebo-controlled trial. Clin J Pain 26, 121–127 (2010).
Bell, R. F., Sivertsen, A., Mowinkel, P. & Vindenes, H. A bilateral clinical model for the study of acute and chronic pain after breast-reduction surgery. Acta Anaesthesiol Scand 45, 576–582 (2001).
Kairaluoma, P. M., Bachmann, M. S., Rosenberg, P. H. & Pere, P. J. Preincisional paravertebral block reduces the prevalence of chronic pain after breast surgery. Anesth Analg 103, 703–708 (2006).
Ju, H., Feng, Y., Yang, B. X. & Wang, J. Comparison of epidural analgesia and intercostal nerve cryoanalgesia for post-thoracotomy pain control. Eur J Pain 12, 378–384 (2008).
Paxton, L. D., Huss, B. K., Loughlin, V. & Mirakhur, R. K. Intra-vas deferens bupivacaine for prevention of acute pain and chronic discomfort after vasectomy. Br J Anaesth 74, 612–613 (1995).
Grosen, K. et al. Perioperative gabapentin for the prevention of persistent pain after thoracotomy: a randomized controlled trial. Eur J Cardiothorac Surg 46, 76–85 (2014).
Strazisar, B., Besic, N. & Ahcan, U. Does a continuous local anaesthetic pain treatment after immediate tissue expander reconstruction in breast carcinoma patients more efficiently reduce acute postoperative pain–a prospective randomised study. World J Surg Oncol 12, 16 (2014).
Kurmann, A. et al. Effect of intraoperative infiltration with local anesthesia on the development of chronic pain after inguinal hernia repair: a randomized, triple-blinded, placebo-controlled trial. Surgery 157, 144–154 (2015).
Chiu, M. et al. Reducing persistent postoperative pain and disability 1 year after breast cancer surgery: a randomized, controlled trial comparing thoracic paravertebral block to local anesthetic infiltration. Ann Surg Oncol 21, 795–801 (2014).
Suppa, E., Valente, A., Catarci, S., Zanfini, B. A. & Draisci, G. A study of low-dose S-ketamine infusion as “preventive” pain treatment for cesarean section with spinal anesthesia: benefits and side effects. Minerva Anestesiol 78, 774–781 (2012).
Ilfeld, B. M. et al. Persistent postmastectomy pain and pain-related physical and emotional functioning with and without a continuous paravertebral nerve block: a prospective 1-year follow-up assessment of a randomized, triple-masked, placebo-controlled study. Ann Surg Oncol 22, 2017–2025 (2015).
Zoric, L. et al. Single-shot intraoperative local anaesthetic infiltration does not reduce morphine consumption after total hip arthroplasty: a double-blinded placebo-controlled randomized study. Br J Anaesth 112, 722–728 (2014).
Duvall, S. & Tweedie, R. A nonparametric “trim and fill” method for assessing publication bias in meta-analysis. J Am Stat Assoc 95, 89–98 (2000).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6, e1000097 (2009).
Jadad, A. R. et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17, 1–12 (1996).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin Trials 7, 177–188 (1986).
Ades, A. E., Lu, G. & Higgins, J. P. The interpretation of random-effects meta-analysis in decision models. Med Decis Making 25, 646–654 (2005).
Deeks, J. J., Higgins, J. P. T. & Altman, D. G. Analyzing data and undertaking meta-analyses. In: Higgins, J., Green, S., eds Cochrane Handbook for Systematic Reviews of Interventions 5.0.1. Oxford, UK: The Cochrane Collaboration: chap 9 (2008).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Altman, D. G. & Bland, J. M. Interaction revisited: the difference between two estimates. BMJ 326, 219 (2003).
Tobias, A. Assessing the influence of a single study in meta-analysis. Stata Tech Bull 47 (1999).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 (1997).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–1101 (1994).
Author information
Authors and Affiliations
Contributions
Jun Zhou and Hongtao Chen contributed to conception and design of the study; Jun Zhou, Youling Fan, Jiying Zhong, Xianjie Wen, and Hongtao Chen contributed to acquisition, analysis, and interpretation of data; Jun Zhou, Youling Fan, Jiying Zhong, Xianjie Wen, and Hongtao Chen were involved in drafting or critical revision of the manuscript. All the authors approved the final version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, J., Fan, Y., Zhong, J. et al. Efficacy and safety of multimodal analgesic techniques for preventing chronic postsurgery pain under different surgical categories: a meta-analysis. Sci Rep 7, 678 (2017). https://doi.org/10.1038/s41598-017-00813-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-00813-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.