Abstract
Antibiotic resistance, particularly to fluoroquinolones and macrolides, in the major foodborne pathogen Campylobacter is considered a serious threat to public health. Although ruminant animals serve as a significant reservoir for Campylobacter, limited information is available on antibiotic-resistant Campylobacter of bovine origin. Here, we analyzed the antimicrobial susceptibilities of 320 C. jejuni and 115 C. coli isolates obtained from feedlot cattle farms in multiple states in the U.S. The results indicate that fluoroquinolone resistance reached to 35.4% in C. jejuni and 74.4% in C. coli, which are significantly higher than those previously reported in the U.S. While all fluoroquinolone resistant (FQR) C. coli isolates examined in this study harbored the single Thr-86-Ile mutation in GyrA, FQR C. jejuni isolates had other mutations in GyrA in addition to the Thr-86-Ile change. Notably, most of the analyzed FQR C. coli isolates had similar PFGE (pulsed field gel electrophoresis) patterns and the same MLST (multilocus sequence typing) sequence type (ST-1068) regardless of their geographic sources and time of isolation, while the analyzed C. jejuni isolates were genetically diverse, suggesting that clonal expansion is involved in dissemination of FQR C. coli but not C. jejuni. These findings reveal the rising prevalence of FQR Campylobacter in the U.S. and provide novel information on the epidemiology of antibiotic-resistant Campylobacter in the ruminant reservoir.
Similar content being viewed by others
Introduction
Campylobacter is a leading cause of bacterial foodborne gastroenteritis worldwide and is a major public health problem1, 2. Although the majority of Campylobacter infections are self-limited and do not require antimicrobial treatment, antibiotics are indicated for severe and chronic conditions3. Clinical treatment of campylobacteriosis requires the use of fluoroquinolone (FQ) or macrolide antibiotics. However, antibiotic-resistant Campylobacter is becoming increasingly prevalent. Due to the rising resistance, especially to FQ, the Centers for Disease Control and Prevention (CDC) has recently identified drug-resistant Campylobacter as a serious antibiotic resistance threat in the United States4. The CDC reported that almost 25% of human Campylobacter isolates were resistant to ciprofloxacin in the USA4. Development and transmission of antibiotic resistant Campylobacter is complicated by the fact that Campylobacter is a zoonotic pathogen and is exposed to antibiotics used in both animal production and human medicine.
Contaminated poultry meat is frequently recognized as the major source for human infections5. However, ruminants also play a significant role in epidemiology of human Campylobacter infections and are increasingly reported as the implicated source6,7,8,9. Ruminant Campylobacter contributes to human disease via multiple transmission routes including direct contact (e.g. petting zoo and occupational exposure), consumption of unpasteurized milk (and associated dairy products), and environmental contamination (e.g., water and produce)10,11,12. Molecular typing methods, such as multilocus sequence typing (MLST) and pulsed field gel electrophoresis (PFGE), revealed that certain genotypes of C. jejuni from ruminants are indistinguishable from human isolates12,13,14, linking ruminant Campylobacter to human diseases. Raw milk is a well-recognized transmission route as a number of raw milk associated outbreaks of campylobacteriosis have been documented15,16,17,18. Ruminant Campylobacter may also contaminate water supplies via agricultural runoff. A waterborne outbreak associated with Campylobacter was reported to be the result of contamination of the town’s water supply with Campylobacter originating from a cattle farm in the vicinity11. Thus, control of Campylobacter in ruminants will have a direct impact on food safety and human health.
Despite the importance of ruminant Campylobacter in foodborne disease, few studies have been conducted to understand antibiotic-resistant Campylobacter from cattle. Earlier reports from the U.S. (including the Feedlot 1999 and Dairy 2002 NAHMS studies) and Canada indicated very low levels of FQ resistance (less than 5%) in Campylobacter isolates from cattle19,20,21,22. Bae et al.23 also reported a low level (ca. 5%) of resistance to ciprofloxacin in C. jejuni from different cattle production types in Western U.S., although C. coli isolates from the same study had much higher (ca. 45%) resistance rate to this drug during 2002–2003. Similarly, a study on Campylobacter from dairy cattle in the Midwest U.S. during mid-2000s indicated that less than 1% of isolates were resistant to ciprofloxacin24. However, a slaughterhouse survey25 conducted during late 2008 in the U.S. found that high percentage of both C. jejuni and C. coli (27.3% and 49.2%, respectively) from different types of cattle types (including both feedlot cattle and adult cows and bulls) were resistant to ciprofloxacin.
These observations point to a possible rising trend of FQ-resistance in the U.S. and highlight the need for conducting surveillance studies on a national scale to assess antibiotic resistance in ruminant Campylobacter. Although the National Antimicrobial Resistance Monitoring System (NARMS) operated by USDA monitors the occurrence of antimicrobial resistance in Campylobacter isolates from food animals at slaughter, the sampling and testing strategy does not include cattle and is limited to chicken carcass rinsates (http://www.ars.usda.gov/Main/docs.htm?docid=6750&page=2). To understand the ecology and facilitate control of antimicrobial resistant Campylobacter in the ruminant reservoir, we determined in this study the antimicrobial susceptibility of Campylobacter isolates derived from feedlot cattle operations in geographically diverse regions in the U.S.
Results
Prevalence of Campylobacter in feedlot cattle
The overall prevalence rate of Campylobacter in the feedlot cattle feces was 72.2% (2298/3184), and ranged between 69.2–78.2% among the different states from which the samples were derived. Of the Campylobacter isolates, 82.1% (1886/2298) were identified as C. jejuni, and 15.0% (344/2298) were determined to be C. coli by PCR (Fig. S1). The remaining 68 isolates (2.9%) were of different Campylobacter spp. than C. jejuni and C. coli and were not characterized further to species level (Table 1).
Antimicrobial susceptibility of the C. jejuni and C. coli isolates from feedlot cattle
Of the 320 representative cattle C. jejuni isolates selected across the 35 feedlots tested in this study, 281 (88.1%) were found to be resistant to tetracycline, 114 (35.6%) were resistant to ciprofloxacin, and 110 (34.3%) were resistant to nalidixic acid. Resistance to azithromycin, clindamycin, erythromycin, florfenicol, gentamicin and telithromycin was low (one isolate for each) (Table 2). Among the 115 representative cattle C. coli isolates tested, 86 (74.8%) were found to be resistant to tetracycline, 89 (77.4%) were resistant to ciprofloxacin, 95 (82.6%) were resistant to nalidixic acid, and 5 (4.3%) were resistant to florfenicol and clindamycin. None of the C. coli isolates were resistant to azithromycin, erythromycin, gentamicin or telithromycin (Table 2). The ciprofloxacin resistance in C. coli (77.4%) was significantly (P < 0.05) higher than in C. jejuni (35.6%), as was the resistance rate for nalidixic acid (82.6% vs. 34.3%), whereas resistance to tetracycline was comparable (74.8% vs. 88.1%) between C. coli and C. jejuni (P > 0.05), respectively (Table 2). The resistance rates of either C. jejuni or C. coli isolates for tetracycline, ciprofloxacin and nalidixic acid did not vary substantially among different states (Data not shown). These results indicated an overall high rate of FQ resistance in feedlot cattle Campylobacter isolates, especially in C. coli.
Multiple drug resistance in C. jejuni and C. coli from cattle was observed frequently. Of the 320 C. jejuni isolates tested, 114 (35.6%) were resistant to two or more antimicrobial agents, 100 (31.2%) were resistant to three or more antibiotics, 3 were resistant to four or more agents, 2 were resistant to five or more drugs, and 1 was resistant to seven antibiotics including azithromycin, ciprofloxacin, erythromycin, gentamicin, tetracycline, nalidixic acid and telithromycin (Table 3). None of the C. jejuni isolates were resistant to all nine drugs tested. Of the 115 C. coli isolates, 89 (77.3%) were resistant to two or more antimicrobial agents, 63 (54.7%) were resistant to three or more drugs, and 5 (4.3%) were resistant to five antibiotics (Table 3). None of the C. coli isolates were resistant to six or more antimicrobial agents included in the MIC test. Only one C. jejuni isolate was co-resistant to both ciprofloxacin and erythromycin, while none of the C. coli isolates displayed co-resistance to these two antibiotics (Table 3). The most common multidrug resistance pattern was to ciprofloxacin, nalidixic acid, and tetracycline, which was observed in ~30% of C. jejuni and 50% of C. coli isolates, respectively (Table 3).
Genetic diversity of FQR Campylobacter from cattle
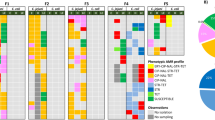
To determine if FQR Campylobacter isolates are genetically related, we analyzed the genetic diversity of representative isolates using PFGE and MLST. A total of 26 FQR C. coli isolates were randomly selected for this purpose. Based on the 90% similarity level, the 26 isolates were grouped into five separate clusters, with the vast majority of isolates (76.9%, 20/26) grouped in cluster I, two isolates in cluster II and IV and one isolate in each of the remaining two clusters (Fig. 1a). The first four clusters had closely related PFGE profiles; the only noticeable difference among the patterns was the presence of extra one or two bands in some isolates (Fig. 1a). The 26 C. coli isolates tested came from 15 different feedlot cattle farms in five different states that were sampled at different times. The 20 strains that grouped together in cluster I included those from 11 different farms in three different states, 10 from Colorado, 6 from Kansas, 4 from Texas while those in Cluster II were from 2 different farm in two states, the two isolates in Cluster IV came from the same farm in Missouri. MLST showed that the isolates grouped in cluster I, II, III and IV had the same sequence type (ST-1068), while the isolate in cluster V was ST-5446.
Dendrogram constructed using the PFGE patterns of KpnI digested FQR C. coli (Fig. 1a) and C. jejuni (Fig. 1b) isolates. Numbers of bootstraps represent similarity. Clusters are determined using a cut off of 90% similarity. Isolate names are listed on the right side of each dendrogram. Tx: Texas; Co: Colorado; IA: Iowa; Ks: Kansas; Mo: Missouri; Fc: Feces.
Additionally, 24 FQR C. jejuni isolates were examined for genetic diversity via PFGE. In contrast to the situation with C. coli, no predominant genotypes were observed among the C. jejuni isolates. There were a total of 17 different PFGE profiles using 90% similarity as the cut off (Fig. 1b). MLST analysis of 7 C. jejuni isolates (Ks-3-Fc-56, Co-4-Fc-1, Co-1-Fc-22, Ks-4-Fc-1, IA-5-Fc-63, IA-3-Fc-18, Mo-1-Fc-27) representative of different PFGE pattern showed 6 different sequence types (ST982, ST3855, ST219, ST45, ST6751, ST459, ST3855 respectively). The MLST result confirmed the genetic diversity of FQR C. jejuni isolates. All together the PFGE and MLST findings suggest that clonal expansion is not involved in dissemination of FQR C. jejuni on the cattle farms.
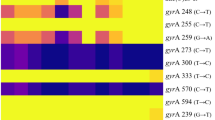
Antibiotic resistance mechanism of FQR Campylobacter
In Campylobacter, FQ resistance is conferred by point mutations in the gyrA gene in conjunction with the function of the CmeABC efflux pump26. To examine the mechanisms of FQ resistance, the quinolone resistance determining region (QRDR) in gyrA of 27 FQR C. coli and 27 FQR C. jejuni isolates were sequenced to determine the mutations associated with FQ resistance. These isolates were selected to represent all farms that were positive with FQR Campylobacter. All C. coli isolates harbored a single Thr-86-Ile mutation in GyrA without any other nucleotide changes in this region (Table 4). Among the 27 FQR C. jejuni isolates sequenced in this study, 10 isolates had the Thr-86-Ile point mutation only, 8 isolates carried the Thr-86-Ile mutation plus the Arg-285-Lys mutation or the Asn-203-Ser change, and 7 isolates carried theAsn-203-Ser and Arg-285-Lys mutations, one of which had an additional Ser-22-Gly change. Interestingly, 2 FQR C. jejuni isolates had no point mutations in QRDR. (Table 4, Table S1). Ser-22-Gly and Arg-285-Lys substitution have not been previously reported to be associated with FQ resistance in Campylobacter. However, Arg-285-Lys mutation was also found in ciprofloxacin susceptible isolates, indicating this point mutation alone would not confer FQ resistance.
Additionally, we analyzed the resistance determinant for tetracycline resistance using a tet(O)-specific PCR. Among the 20 tetracycline-resistant Campylobacter isolates examined in this study, all were positive with tet(O), indicating it is responsible for the resistance phenotype.
Discussion
Results from this study revealed high prevalence of FQR Campylobacter in feedlot cattle in the U.S. The resistance rate in C. coli is especially high, reaching to 77%. Such a high-level prevalence of FQ resistance in ruminants was not reported in earlier studies conducted in the U.S.19,20,21, although a recent study conducted in 200825 found that 27.3% C. jejuni and 49.2% C. coli from different types of cattle productions (including both feedlot cattle and adult cows) were resistant to ciprofloxacin. Our findings in this study showed an even higher frequency of resistance to ciprofloxacin (35.4% in C. jejuni and 77.3% in C. coli) and nalidixic acid (34.3% in C. jejuni and 82.6% in C. coli). All together, these observations clearly indicate a rising trend of FQR Campylobacter in ruminants in the U.S. The reason that FQ resistance was much more prevalent in C. coli than in C. jejuni is unknown, but it has been known that C. coli is more likely to acquire antibiotic resistance than C. jejuni 23, 27,28,29,30.
Campylobacter is highly mutable, and multiple independent studies including our work have demonstrated the rapid emergence of FQR mutants in animals originally infected with FQS C. jejuni and then treated with an FQ antimicrobial2, 31,32,33,34. FQR mutants spontaneously occur in Campylobacter populations and use of FQ antimicrobials selects and enriches these mutants. In Campylobacter, FQ-resistance is mainly mediated by point mutations in the QRDR of DNA gyrase (GyrA) in conjunction with the function of the multidrug efflux pump CmeABC2, 26, 35, 36. The most frequent mutation observed in FQR Campylobacter isolates is Thr-86-Ile, followed by Asp-90-Asn, Thr-86-Lys, Thr-86-Ala, Thr-86-Val, Asp-90-Tyr and Ala-70-Thr2, 37, 38. The Thr-86-Ile mutation confers a high level of FQ resistance (ciprofloxacin MIC ≥ 16 µl/ml) in Campylobacter, while other mutations are associated with a low to medium level of resistance (MIC = 1–8 µg/ml)2, 39, 40. Double mutations including Thr-86-Ile/Pro-104-Ser and Thr-86-Ile/Asp-90-Asn have also been linked to FQ resistance in Campylobacter 39.
Consistent with the previous findings discussed above, we found in this study that the FQR C. coli and C. jejuni isolates. However, we also identified three additional amino acid substitution in the C. jejuni isolates. One is Asn-203-Ser, which is known to confer FQ resistance along with Thr-86-Ile mutation27, 41. Another one is Arg-285-Lys, which alone may not confer FQ resistance because it was identified in susceptible strains. Six FQR contained both Asn-203-Ser and Arg-285-Lys, but no Thr-86-Ile (Table 4; Table S1). Whether the two mutations alone were responsible for the FQ resistance phenotype is unknown and needs further investigation. The third mutation is Ser-22-Gly, which has not been associated with FQ resistance in Campylobacter. Interestingly, two FQR C. jejuni isolates from the same farm did not show any mutations in QRDR of gyrA (Table 4), and what is responsible for their resistance to FQ is unknown and can’t be explained by mutations in gyrA. These findings indicate that the gyrA mutations in FQR C. jejuni isolates are more diverse than in FQR C. coli isolates.
FQ antibiotics are frequently used in veterinary medicine for the treatment and control of infectious diseases of pets and food-producing animals42. For example, enrofloxacin and danofloxacin are approved as an injectable solution (various dosage regimens) for use in the treatment and control of respiratory disease in cattle associated with Mannheimia haemolytica, Pasteurella multocida, Histophilus somni and Mycoplasma bovis in the United States and many other countries42. The initial approval of enrofloxacin by FDA was in 1998 and it was only for the treatment of bovine respiratory disease (BRD) in beef cattle. Subsequent approvals extended their use for BRD treatment in dairy replacement heifers of less than 20 months of age in 2008, and their metaphylactic use for control of BRD in beef and non-lactating dairy cattle at high risks of developing BRD in 2012. About 43% of the feedlots included in the Feedlot 2011 NAHMS study reported therapeutic use of FQs in approximately 42% of cattle with respiratory disease43. In the United States, the use of these drugs in cattle production is permitted only under a prescription from a veterinarian and their extralabel use in food producing animals is strictly prohibited. In this study, we showed a substantial increase in the prevalence of FQ resistance in Campylobacter isolates from cattle in the U.S., which coincides with the expanded use of FQ antibiotics in cattle production. However, it is still unknown if the on-farm use directly influences the development and dissemination of FQ-resistant Campylobacter and if the treatment regimen can be managed to reduce the development and prevalence of FQ-resistance.
Except for FQs and tetracycline, the Campylobacter isolates examined in this study are generally susceptible to other tested antimicrobials (Table 2). For example, the resistance to macrolide (erythromycin) was barely detected in both C. coli and C. jejuni. Tetracycline has been used for animal production for many years, and we found that tetracycline resistance is high in both C. jejuni (88.1%) and C. coli (74.8%), which is even higher than previously reported19, 20, 44. The predominant tetracycline resistance determinant in Campylobacter is tet (O), although a recent study reported that tet (A) also conferred resistant to tetracycline in Campylobacter 45. In this study, all examined tetracycline-resistant isolates harbored the tet(O) gene, consistent with previously reported findings.
PFGE and MLST are two commonly used genotyping methods for differentiation of Campylobacter isolates46,47,48. In this study, PFGE typing of 26 FQR C. coli and 24 FQR C. jejuni revealed that C. coli is more clonal than C. jejuni (Fig. 1), despite the fact that the C. coli isolates were from 15 feedlots in 5 different states. The majority of the PFGE-typed C. coli isolates were grouped into three clusters (I, II and IV) of high genetic similarity, which was confirmed by MLST to be a single ST (ST-1068), suggesting dissemination of a single clone on different cattle farms. This ST was observed in 83% (52/63) of the C. coli isolates of cattle origin in another report49, further indicating that it is highly prevalent in cattle. The presence of C. coli with identical genotype on multiple geographically distant farms implies the dissemination of a single strain from farm to farm, which could be a potential factor driving the increase in FQR prevalence in Campylobacter. Similar findings were reported in a previous study, in which multiple antibiotic resistant C. coli collected from different cattle farms and at different times had an indistinguishable PFGE pattern, in contrast to the genetic diverse of C. jejuni isolates50. The exact vehicles or mechanisms promoting clonal dissemination of C. coli in different cattle farms are unknown and need to be further investigated. For the C. jejuni isolates examined in this study, they are genetically diverse and it is unlikely that colonal expansion is involved in their dissemination.
In summary, we observed high prevalence of FQ-resistance in both C. jejuni and C. coli isolates derived from cattle in the U.S. The reason for this rising trend in FQ resistance is uncertain, but it is likely due to the hyper-mutable nature of Campylobacter and the selection from use of FQ antimicrobials in the control of respiratory diseases in cattle production. Additionally, clonal expansion, as reported in other studies51,52,53, may have also contributed to the increasing prevalence of FQR Campylobacter. Development of FQ resistance is known to affect the fitness of Campylobacter in chickens, resulting in persistence of FQR Campylobacter even in the absence of antibiotic selection pressure54.
Considering this possibility and the fact that FQs are currently used for cattle production, it is possible that the prevalence of FQR Campylobacter will continue to rise. Given that ruminant Campylobacter is a significant source of foodborne campylobacteriosis in humans, heightened efforts are needed to control the development and dissemination of FQR Campylobacter in cattle production.
Methods and Materials
Sample collection and bacterial isolation
A total of 3,184 cattle fecal samples were collected from 35 different feedlot cattle herds located in Iowa (n = 8), Texas (n = 8), Colorado (n = 8), Missouri (n = 3) and Kansas (n = 8) on two different occasions during December 2012 to March 2013. Collection of cattle fecal samples followed methods that have been described previously55. Cattle fecal samples were collected from the floor of animal pens and only freshly voided fecal pats were sampled. In other words, the sample was collected from a fecal pat only after a cow was observed defecating. This procedure allowed us to standardize environmental exposure time among fecal samples and estimate herd prevalence of Campylobacter without confining animals for collection of rectal samples. Freshly voided fecal pats were scraped with a sterile cotton tipped swab and the swab was immediately placed in 10 ml glass tubes containing Campylobacter Thioglycollate Broth (CAMPY-THIO). Vials were labeled and then immediately placed in an electric cooler set to 4 °C. All cattle fecal samples were shipped priority overnight to the testing laboratory. All samples were shipped, in insulated boxes packed with Ice-Brix® (Polar Tech Industries, Genoa, IL 60135). Only samples received by the laboratories within 24 hours of the date of collection were screened for Campylobacter. From the Campy-Thio containing the fecal samples, 1 ml was added into tubes containing 9 ml of Campylobacter enrichment broth (Mueller–Hinton [MH] medium supplemented with selective growth supplements [SR084E and SR117E; Oxoid]), and incubated at 42 °C for 48 h under microaerobic conditions (5% O2, 10% CO2, and 85% N2). From the enrichment culture, an inoculum of 100 µl was streaked onto MH agar containing the same selective supplements, which were further incubated for 48 h under the same conditions. A single Campylobacter-like colony from each sample was subcultured onto a MH agar plate and the pure cultures were stored in glycerol stocks at −80 °C until further use.
Campylobacter identification
PCR was used to detect and differentiate C. jejuni and C. coli. Two sets of previously published PCR primers were used56, 57. The first primer pair (CCCJ-F: 5′-AAT CTA ATG GCT TAA CCA TTA-3′; CCCJ-R: 5′-GTA ACT AGT TTA GTA TTC CGG-3′), targeting 16S rRNA, was designed to co-identify C. jejuni and C. coli 56. The second primer pair (mapA-F: 5′-GAG TGC TTG TGC AAC TAA AC-3′; mapA-R: 5′-ATA GCA TCT TGA GTT GCT CC-3′) was specific for C. jejuni only57. The primers were synthesized at the DNA facility in Iowa State University using the MerMade-192 synthesizer. PCR reactions were performed as described previously56, 57.
Antimicrobial susceptibility testing
In total, 320 C. jejuni (5 from each feedlot) and 115 C. coli (3 from each feedlot) isolates were randomly chosen and included in the susceptibility testing. The minimum inhibitory concentrations (MICs) of nine antibiotics were determined using a standard broth microdilution method as recommended by Clinical and Laboratory Standards Institute (CLSI) and National Antimicrobial Resistance Monitoring System for Enteric Bacteria (NARMS)58,59,60. Commercially available Sensititre Campylobacter plates (Trek Diagnostic Systems, Cleveland, Ohio) were used for antimicrobial susceptibility testing. The plates were read after incubated in a microaerobic environment for 24 h at 42 °C. The lowest antimicrobial concentration at which no bacterial growth developed was used as MIC value for each isolate. The antimicrobial resistance breakpoints were chosen according to the interpretive standards established by the CLSI for bacteria isolated from animals58,59,60. C. jejuni ATCC 33560 and C. coli ATCC 33559 were used as quality control strains for C. jejuni and C. coli, respectively.
PFGE and MLST typing of Campylobacter isolates
In total, 26 FQR C. jejuni and 24 FQR C. coli isolates were randomly chosen from different feedlots in different states. In this study, 15 feedlots were positive with FQR C. coli, and 17 feedlots were positive with FQR C. jejuni. We selected 1–2 isolates from each positive feedlot to represent all positive farms in all five states. PFGE analysis of the macrorestriction fragment patterns of genomic DNA using KpnI enzyme was performed on these isolates following the CDC’s standardized PulseNet protocol for Campylobacter with minor modifications47. Briefly, fresh cultures of Campylobacter were embedded in 1% Seakem Gold agarose (Fisher Scientific, Fair Lawn, NJ) and lysed with proteinase K for 1 h at 55 °C in a water bath shaker. The gel plugs were digested with KpnI for 4 h at 37 °C. Digested plugs were embedded into 1% agarose and separated by electrophoresis in 0.5 × TBE buffer (Promega) at 14 °C for 18 h using a Chef Mapper electrophoresis system (Bio-Rad, Hercules, CA). Gel was stained with ethidium bromide for 30 min and then photographed by UV transillumination (Alpha Innotech, Santa, Clara, CA). The PFGE patterns were analyzed by the GelCompare II v.6.5 software program (Applied Maths, Kortrijik, Belgium) using Dice similarity coefficient and unweighted-pair group method with arithmetic averages (UPGMA) with 0.5% optimization and 1.5% position tolerance. Lambda DNA ladder (Bio-Rad) was used as the molecular size marker.
To further confirm the genotype of those isolates, MLST, originally developed by Dingle et al.46, was carried out on FQR C. coli and C. jejuni isolates representative of different PFGE types. Seven housekeeping genes were amplified and sequenced using the primer sets recommended at the Campylobacter MLST website (http://pubmlst.org/campylobacter/), developed by Keith Jolley and Man-Suen Chan at the University of Oxford61. All PCR products were purified using the QIAquick® PCR purification kit (QIAGEN, Hilden, Germany) and then sequenced at the DNA Core Facility of Iowa State University using an Applied Biosystems 3730xl DNA Analyzer. Allelic numbers were assigned to the isolates by performing BLAST searches for the assembled sequences using the single-locus query function, whereas sequence types were assigned using the allelic profile query function in the MLST database. Sequences that were identical to existing alleles in the MLST database were assigned the corresponding allele numbers. Novel sequences were assigned new allele numbers and sequence types (STs) within the MLST database.
Antibiotic resistance mechanism determination
A total of 27 FQR C. coli and 27 FQR C. jejuni isolates were selected for determination of the point mutations in gyrA (Table S1). To amplify the QRDR region of gyrA by PCR, primers GyrAF1 (5′-CAACTGGTTCTAGCCTTTTG-3′) and GyrAR1 (5′-AATTTCACTCATAGCCTCACG-3′) were used for C. jejuni, while GyrAF2 (5′-TTATTTAGATTATTCTATGAGCGT-3′) and GyrAR2 (5′-CTTGAGTTCGATTACAACAC-3′) were used for C. coli. All PCR products were purified using the QIAquick® PCR purification kit (QIAGEN, Hilden, Germany) and then sequenced at the DNA Core Facility of Iowa State University using an Applied Biosystems 3730xl DNA Analyzer.
The presence of the tet(O) gene (the predominant determinant of tetracycline resistance in Campylobacter), was determined by PCR. For this purpose, primers tet(O)-F (5′-GGCGTTTTGTTTATGTGCG-3′) and tet(O)-R (5′-ATGGACAACCCGACAGAAGC-3′) were used to amplify a 559-bp region of the tet(O) gene as described elsewhere47.
Statistical analysis
To compare the prevalence of antimicrobial resistance between C. jejuni and C. coli, the statistical analyses were performed with GLIMMIX procedure in SAS 9.4 version (SAS Institute Inc., Cary, NC, USA) for binary distribution (yes/no response variable) with logit link function. Both states and farms were considered as random effects, the Campylobacter species (C. jejuni and C. coli) was the fixed effect, and three different models were fitted separately with three kinds of antibiotics (ciprofloxacin, nalidixic acid and tetracycline) as response variables. The significance level used here is 0.05.
References
Adak, G. K., Meakins, S. M., Yip, H., Lopman, B. A. & O’Brien, S. J. Disease risks from foods, England and Wales, 1996–2000. Emerging infectious diseases 11, 365–372, doi:10.3201/eid1103.040191 (2005).
Luo, N., Sahin, O., Lin, J., Michel, L. O. & Zhang, Q. In vivo selection of Campylobacter isolates with high levels of fluoroquinolone resistance associated with gyrA mutations and the function of the CmeABC efflux pump. Antimicrobial agents and chemotherapy 47, 390–394 (2003).
Nachamkin, I. Campylobacter infections. Current Opinion in Infectious Diseases 6, 72–76.
CDC. Antibiotic Resistance Threats in the United States. http://www.cdc.gov/drugresistance/threat-report-2013/ (2013).
Gormley, F. J. et al. A 17-year review of foodborne outbreaks: describing the continuing decline in England and Wales (1992–2008). Epidemiology and infection 139, 688–699, doi:10.1017/S0950268810001858 (2011).
Cha, W. Antimicrobial Susceptibility Profiles of Human Campylobacter jejuni Isolates and Association with Phylogenetic Lineages. Frontiers in microbiology 7, 589, doi:10.3389/fmicb.2016.00589 (2016).
Boysen, L. et al. Source attribution of human campylobacteriosis in Denmark. Epidemiology and infection 142, 1599–1608, doi:10.1017/S0950268813002719 (2014).
Davis, K. R. et al. Campylobacter jejuni Infections Associated with Raw Milk Consumption - Utah, 2014. MMWR. Morbidity and mortality weekly report 65, 301–305, doi:10.15585/mmwr.mm6512a1 (2016).
Davis, M. A. et al. Risk factors for campylobacteriosis in two washington state counties with high numbers of dairy farms. Journal of clinical microbiology 51, 3921–3927, doi:10.1128/JCM.01433-13 (2013).
Doyle, M. P. & Roman, D. J. Prevalence and survival of Campylobacter jejuni in unpasteurized milk. Applied and environmental microbiology 44, 1154–1158 (1982).
Clark, C. G. et al. Characterization of waterborne outbreak-associated Campylobacter jejuni, Walkerton, Ontario. Emerging infectious diseases 9, 1232–1241, doi:10.3201/eid0910.020584 (2003).
Stanley, K. & Jones, K. Cattle and sheep farms as reservoirs of Campylobacter. Journal of applied microbiology 94 Suppl, 104S–113S (2003).
Wilson, D. J. et al. Tracing the source of campylobacteriosis. PLoS genetics 4, e1000203, doi:10.1371/journal.pgen.1000203 (2008).
Fitzgerald, C., Stanley, K., Andrew, S. & Jones, K. Use of pulsed-field gel electrophoresis and flagellin gene typing in identifying clonal groups of Campylobacter jejuni and Campylobacter coli in farm and clinical environments. Applied and environmental microbiology 67, 1429–1436, doi:10.1128/AEM.67.4.1429-1436.2001 (2001).
Heuvelink, A. E. et al. Two outbreaks of campylobacteriosis associated with the consumption of raw cows’ milk. International journal of food microbiology 134, 70–74, doi:10.1016/j.ijfoodmicro.2008.12.026 (2009).
Newkirk, R., Hedberg, C. & Bender, J. Establishing a milkborne disease outbreak profile: potential food defense implications. Foodborne pathogens and disease 8, 433–437, doi:10.1089/fpd.2010.0731 (2011).
Lejeune, J. T. & Rajala-Schultz, P. J. Food safety: unpasteurized milk: a continued public health threat. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 48, 93–100, doi:10.1086/595007 (2009).
Headrick, M. L. et al. The epidemiology of raw milk-associated foodborne disease outbreaks reported in the United States, 1973 through 1992. American journal of public health 88, 1219–1221 (1998).
Englen, M. D., Fedorka-Cray, P. J., Ladely, S. R. & Dargatz, D. A. Antimicrobial resistance patterns of Campylobacter from feedlot cattle*. Journal of applied microbiology 99, 285–291, doi:10.1111/j.1365-2672.2005.02609.x (2005).
Englen, M. D., Hill, A. E., Dargatz, D. A., Ladely, S. R. & Fedorka-Cray, P. J. Prevalence and antimicrobial resistance of Campylobacter in US dairy cattle. Journal of applied microbiology 102, 1570–1577, doi:10.1111/j.1365-2672.2006.03189.x (2007).
Halbert, L. W. et al. Evaluation of antimicrobial susceptibility patterns in Campylobacter spp isolated from dairy cattle and farms managed organically and conventionally in the midwestern and northeastern United States. Journal of the American Veterinary Medical Association 228, 1074–1081, doi:10.2460/javma.228.7.1074 (2006).
Inglis, G. D. et al. Temporal prevalence of antimicrobial resistance in Campylobacter spp. from beef cattle in Alberta feedlots. Applied and environmental microbiology 72, 4088–4095, doi:10.1128/AEM.02830-05 (2006).
Bae, W. et al. Prevalence and antimicrobial resistance of thermophilic Campylobacter spp. from cattle farms in Washington State. Applied and environmental microbiology 71, 169–174, doi:10.1128/AEM.71.1.169-174.2005 (2005).
Sato, K., Bartlett, P. C., Kaneene, J. B. & Downes, F. P. Comparison of prevalence and antimicrobial susceptibilities of Campylobacter spp. isolates from organic and conventional dairy herds in Wisconsin. Applied and environmental microbiology 70, 1442–1447 (2004).
Sanad, Y. M. et al. Genotypic and phenotypic properties of cattle-associated Campylobacter and their implications to public health in the USA. PloS one 6, e25778, doi:10.1371/journal.pone.0025778 (2011).
Zhang, Q., Lin, J. & Pereira, S. Fluoroquinolone-resistant Campylobacter in animal reservoirs: dynamics of development, resistance mechanisms and ecological fitness. Animal health research reviews/Conference of Research Workers in Animal Diseases 4, 63–71 (2003).
Ge, B. et al. Antimicrobial-resistant Campylobacter species from retail raw meats. Applied and environmental microbiology 69, 3005–3007 (2003).
Gupta, A. et al. Antimicrobial resistance among Campylobacter strains, United States, 1997-2001. Emerging infectious diseases 10, 1102–1109, doi:10.3201/eid1006.030635 (2004).
Van Looveren, M. et al. Antimicrobial susceptibilities of Campylobacter strains isolated from food animals in Belgium. The Journal of antimicrobial chemotherapy 48, 235–240 (2001).
Luangtongkum, T. et al. Effect of conventional and organic production practices on the prevalence and antimicrobial resistance of Campylobacter spp. in poultry. Applied and environmental microbiology 72, 3600–3607, doi:10.1128/AEM.72.5.3600-3607.2006 (2006).
Farnell, M. B. et al. Campylobacter susceptibility to ciprofloxacin and corresponding fluoroquinolone concentrations within the gastrointestinal tracts of chickens. Journal of applied microbiology 99, 1043–1050, doi:10.1111/j.1365-2672.2005.02712.x (2005).
Griggs, D. J. et al. Incidence and mechanism of ciprofloxacin resistance in Campylobacter spp. isolated from commercial poultry flocks in the United Kingdom before, during, and after fluoroquinolone treatment. Antimicrobial agents and chemotherapy 49, 699–707, doi:10.1128/AAC.49.2.699-707.2005 (2005).
McDermott, P. F. et al. Ciprofloxacin resistance in Campylobacter jejuni evolves rapidly in chickens treated with fluoroquinolones. The Journal of infectious diseases 185, 837–840, doi:10.1086/339195 (2002).
van Boven, M., Veldman, K. T., de Jong, M. C. & Mevius, D. J. Rapid selection of quinolone resistance in Campylobacter jejuni but not in Escherichia coli in individually housed broilers. The Journal of antimicrobial chemotherapy 52, 719–723, doi:10.1093/jac/dkg402 (2003).
Ge, B., McDermott, P. F., White, D. G. & Meng, J. Role of efflux pumps and topoisomerase mutations in fluoroquinolone resistance in Campylobacter jejuni and Campylobacter coli. Antimicrobial agents and chemotherapy 49, 3347–3354, doi:10.1128/AAC.49.8.3347-3354.2005 (2005).
Yao, H. et al. Emergence of a Potent Multidrug Efflux Pump Variant That Enhances Campylobacter Resistance to Multiple Antibiotics. mBio 7, doi:10.1128/mBio.01543-16 (2016).
Engberg, J., Aarestrup, F. M., Taylor, D. E., Gerner-Smidt, P. & Nachamkin, I. Quinolone and macrolide resistance in Campylobacter jejuni and C. coli: resistance mechanisms and trends in human isolates. Emerging infectious diseases 7, 24–34, doi:10.3201/eid0701.700024 (2001).
Wang, Y., Huang, W. M. & Taylor, D. E. Cloning and nucleotide sequence of the Campylobacter jejuni gyrA gene and characterization of quinolone resistance mutations. Antimicrobial agents and chemotherapy 37, 457–463 (1993).
Payot, S. et al. Mechanisms of fluoroquinolone and macrolide resistance in Campylobacter spp. Microbes and infection/Institut Pasteur 8, 1967–1971, doi:10.1016/j.micinf.2005.12.032 (2006).
Yan, M., Sahin, O., Lin, J. & Zhang, Q. Role of the CmeABC efflux pump in the emergence of fluoroquinolone-resistant Campylobacter under selection pressure. The Journal of antimicrobial chemotherapy 58, 1154–1159, doi:10.1093/jac/dkl412 (2006).
Corcoran, D., Quinn, T., Cotter, L. & Fanning, S. Relative contribution of target gene mutation and efflux to varying quinolone resistance in Irish Campylobacter isolates. FEMS microbiology letters 253, 39–46, doi:10.1016/j.femsle.2005.09.019 (2005).
Giguere, S., Prescott, J. F., Baggot, J. D., Walker, R. D. and Dowling, P. M. Antimicrobial Therapy in Veterinary Medicine. John Wiley & Sons, Inc, Ames, IA (2013).
USDA. USDA Feedlot 2011 “Part IV: Health and Health Management on U.S. Feedlots with a Capacity of 1,000 or More Head. USDA-APHIS-VS-CEAH-NAHMS. Fort Collins, CO. #638.0913 (2015).
Wieczorek, K., Kania, I. & Osek, J. Prevalence and antimicrobial resistance of Campylobacter spp. isolated from poultry carcasses in Poland. Journal of food protection 76, 1451–1455, doi:10.4315/0362-028X.JFP-13-035 (2013).
Abdi-Hachesoo, B. et al. Tetracycline Resistance Genes in Campylobacter jejuni and C. coli Isolated From Poultry Carcasses. Jundishapur journal of microbiology 7, e12129, doi:10.5812/jjm.12129 (2014).
Dingle, K. E. et al. Multilocus sequence typing system for Campylobacter jejuni. Journal of clinical microbiology 39, 14–23, doi:10.1128/JCM.39.1.14-23.2001 (2001).
Sahin, O. et al. Emergence of a tetracycline-resistant Campylobacter jejuni clone associated with outbreaks of ovine abortion in the United States. Journal of clinical microbiology 46, 1663–1671, doi:10.1128/JCM.00031-08 (2008).
Taboada, E. N., Clark, C. G., Sproston, E. L. & Carrillo, C. D. Current methods for molecular typing of Campylobacter species. Journal of microbiological methods 95, 24–31, doi:10.1016/j.mimet.2013.07.007 (2013).
Miller, W. G. et al. Identification of host-associated alleles by multilocus sequence typing of Campylobacter coli strains from food animals. Microbiology 152, 245–255, doi:10.1099/mic.0.28348-0 (2006).
Bae, W. et al. Dissemination of antimicrobial resistant strains of Campylobacter coli and Campylobacter jejuni among cattle in Washington State and California. Veterinary microbiology 122, 306–315, doi:10.1016/j.vetmic.2007.01.020 (2007).
Kovac, J. et al. High genetic similarity of ciprofloxacin-resistant Campylobacter jejuni in central Europe. Frontiers in microbiology 6, 1169, doi:10.3389/fmicb.2015.01169 (2015).
Kittl, S., Heckel, G., Korczak, B. M. & Kuhnert, P. Source attribution of human Campylobacter isolates by MLST and fla-typing and association of genotypes with quinolone resistance. PloS one 8, e81796, doi:10.1371/journal.pone.0081796 (2013).
Wimalarathna, H. M. et al. Widespread acquisition of antimicrobial resistance among Campylobacter isolates from UK retail poultry and evidence for clonal expansion of resistant lineages. BMC microbiology 13, 160, doi:10.1186/1471-2180-13-160 (2013).
Luo, N. et al. Enhanced in vivo fitness of fluoroquinolone-resistant Campylobacter jejuni in the absence of antibiotic selection pressure. Proceedings of the National Academy of Sciences of the United States of America 102, 541–546, doi:10.1073/pnas.0408966102 (2005).
Carlson, J. C. et al. Efficacy of European starling control to reduce Salmonella enterica contamination in a concentrated animal feeding operation in the Texas panhandle. BMC veterinary research 7, 9, doi:10.1186/1746-6148-7-9 (2011).
Linton, D., Lawson, A. J., Owen, R. J. & Stanley, J. PCR detection, identification to species level, and fingerprinting of Campylobacter jejuni and Campylobacter coli direct from diarrheic samples. Journal of clinical microbiology 35, 2568–2572 (1997).
Linton, D., Owen, R. J. & Stanley, J. Rapid identification by PCR of the genus Campylobacter and of five Campylobacter species enteropathogenic for man and animals. Research in microbiology 147, 707–718 (1996).
Institute., C. a. L. S. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals; approved standards VET01-A4, 4rd ed. Wayne, PA, USA: CLSI (2013).
Ge, B., Wang, F., Sjolund-Karlsson, M. & McDermott, P. F. Antimicrobial resistance in campylobacter: susceptibility testing methods and resistance trends. Journal of microbiological methods 95, 57–67, doi:10.1016/j.mimet.2013.06.021 (2013).
Institute, C. a. L. S. Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria: Approved Guideline-second edition. CLSI Document M45-A2: Wayne, PA (2010).
Jolley, K. A., Chan, M. S. & Maiden, M. C. mlstdbNet - distributed multi-locus sequence typing (MLST) databases. BMC bioinformatics 5, 86, doi:10.1186/1471-2105-5-86 (2004).
Acknowledgements
We thank Kyle Anderegg, Brandi Dellore, and Angela Landorf for their assistance in the experiments conducted. This work was supported by USDA National Institute of Food and Agriculture grant no. 2012-67005-19614.
Author information
Authors and Affiliations
Contributions
Y.T. and Q.Z. designed research; N.P., O.S., J.L., J.C. collected and cultured samples, Y.T. and L.D. performed research; Y.T., O.S., Z.W. and L.D. analyzed data. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Tang, Y., Sahin, O., Pavlovic, N. et al. Rising fluoroquinolone resistance in Campylobacter isolated from feedlot cattle in the United States. Sci Rep 7, 494 (2017). https://doi.org/10.1038/s41598-017-00584-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-00584-z
This article is cited by
-
Zoonotic and antibiotic-resistant Campylobacter: a view through the One Health lens
One Health Advances (2023)
-
Mining therapeutic targets from the antibiotic-resistant Campylobacter coli and virtual screening of natural product inhibitors against its riboflavin synthase
Molecular Diversity (2023)
-
Comparisons of plasma and fecal pharmacokinetics of danofloxacin and enrofloxacin in healthy and Mannheimia haemolytica infected calves
Scientific Reports (2022)
-
Antibiotic resistance, molecular characterizations, and clinical manifestations of Campylobacteriosis at a military medical center in Hawaii from 2012–2016: a retrospective analysis
Scientific Reports (2018)
-
Genotypic diversity, antimicrobial resistance and biofilm-forming abilities of Campylobacter isolated from chicken in Central China
Gut Pathogens (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.