Abstract
Severe hyperlactatemia (SH)/lactic acidosis (LA) after laparoscopic resection of pheochromocytoma is an infrequently reported complication. The study aims to investigate the incidence of this complication and to determine the clinical risk factors. Patients who underwent laparoscopic resection for pheochromocytoma between 2011 and 2014 at Peking Union Medical College Hospital were enrolled. LA was defined as pH < 7.35, bicarbonate <20 mmol/L, and serum lactate ≥5 mmol/L; SH as lactate ≥5 mmol/L; and moderate hyperlactatemia (MH) as lactate 2.5–5.0 mmol/L without evidence of acidosis (pH > 7.35 and/or bicarbonate >20 mmol/L). Data concerning patient demographics, clinical history, and laboratory results were collected and statistical analyses were performed. Out of 145 patients, 59 (40.7%) developed post-operative hyperlactatemia. The incidences of MH and SH/LA were 25.5% and 15.2%, respectively. Multivariate analysis demonstrated that body mass index (BMI) (odds ratio [OR], 1.204; 95% confidence interval [CI], 1.016–1.426), 24-hour urine epinephrine concentration (OR, 1.012; 95% CI, 1.002–1.022), and tumor size (OR, 1.571; 95% CI, 1.102–2.240) were independent predictors of post-operative SH/LA. The data show that post-operative SH/LA is not a rare complication after pheochromocytoma resection and may be closely associated with higher BMI, larger tumor size, and higher levels of urine epinephrine.
Similar content being viewed by others
Introduction
Pheochromocytoma is a rare, catecholamine-producing neuroendocrine tumor originating from chromaffin cells of the adrenal medulla1. Cardinal manifestations of pheochromocytoma include episodic hypertension, headaches, sweating, and palpitations1. Although laparoscopic resection has become the first-line curative treatment for pheochromocytoma2, it is likely to induce wide fluctuations of circulating catecholamines intra-operatively. Excessive secretion of catecholamines may consequently augment glycolytic flux and decrease tissue perfusion, both of which have the capacity to boost lactate accumulation3.
Hyperlactatemia occurs when lactate generation exceeds lactate consumption. If not effectively controlled, moderate hyperlactatemia (MH) can progress to severe hyperlactatemia (SH) or even lactic acidosis (LA). LA, as a predictor of poor clinical outcome, may decrease myocardial contractility and cardiac output, can make the myocardium susceptible to cardiac arrhythmias, and can render the cardiovascular system insensitive to the effect of catecholamines4. In fact, previous studies have reported a myriad of cases of SH/LA in patients with pheochromocytoma5,6,7. However, owing to the rarity of pheochromocytoma, few studies have focused on the clinical factors resulting in post-operative SH/LA in patients who have undergone laparoscopic adrenalectomy.
The aim of this study was to evaluate the incidence of post-operative SH/LA and the clinical risk factors predisposing patients undergoing laparoscopic resection of pheochromocytoma to SH/LA.
Results
Of a total of 145 patients, post-operative MH occurred in 37 and SH/LA in 22. The clinical and biochemical characteristics of patients with normolactatemia, MH, and SH/LA are shown in Tables 1–4. Pre-operatively, subjects in the group with SH/LA had larger tumors but a lower incidence of comorbid diabetes mellitus than those in the group with normolactatemia. However, there were no statistical differences in primary and secondary diabetes mellitus among the three groups. The SH/LA group had a greater proportion of epinephrine-secreting tumors than the normolactatemia group (Table 1). There were no statistical differences for pre-operative parameters among the three groups (Table 2). Intra-operatively, patients in the normolactatemia group experienced lower maximum heart rate and shorter anesthetic time than those in the MH groups, while the SH/LA group had a longer operative time than the normolactatemia group (Table 3). Post-operatively, subjects in the group with SH/LA had a longer mechanical ventilation time, greater maximum heart rate, and longer length of hospitalization than those in the normolactatemia group. The plasma lactate levels in the normolactatemia group were significantly lower than those of the MH and SH/LA groups (Table 4). In the multivariate analysis, body mass index (BMI), 24-hour urine epinephrine, and tumor size were independent predictors of post-operative SH/LA, with an odds ratio of 1.204 (95% confidence interval [CI], 1.016–1.426); 1.012 (95% CI, 1.002–1.022) and 1.571 (95% CI, 1.102–2.240), respectively (Table 5).
Discussion
Hyperlactatemia is a frequent complication of laparoscopic resection of pheochromocytoma (40.7%); SH/LA is also relatively common (15.2%). According to the results, patients with post-operative SH/LA are likely to experience a longer post-operative hospitalization, a higher post-operative maximum heart rate, and a longer duration of mechanical ventilation than those with normolactatemia. Our data demonstrate that patients with higher urine epinephrine levels, larger tumor size, and higher BMI are predisposed to post-operative SH/LA which potentially requires intensive care for management of elevated serum lactate.
Normally, there is a balance between lactate production and consumption. This can be reflected by the redox-coupled interconversion of pyruvate and lactate. Physiologically, the blood lactate-to-pyruvate ratio is 10:1, but it rises as the ratio of NADH concentration to NAD+ concentration (redox state) increases. Most pyruvate is generated by anaerobic glycolysis. Therefore, anaerobic glycolysis is the most common cause of hyperlactatemia or even lactic acidosis. However, aerobic glycolysis, stimulated glycolysis that depends on factors other than tissue hypoxia, also prompts lactate generation8. From the point of bioenergetics, generation of lactate ions by way of glycolysis is coupled with the production of an equivalent number of protons from the hydrolysis of the produced ATP8. In addition to glycolysis, the more efficient but slower ATP-producing process used by many cells is oxidative phosphorylation. In short, glucose plays a major role in lactate production, and any disorders correlated with hyperglycemia are likely to facilitate lactate production.
Catecholamines exert their effects via adrenoceptors in the majority of patients with pheochromocytoma1. In the human body, epinephrine and norepinephrine have overlapping but distinct effects on α- and β-adrenoceptors. At low doses, epinephrine acts predominantly on the peripheral β 1- and β 2- adrenoceptors. However, with increasing doses of epinephrine, the α 1-adrenoceptor-mediated vasoconstrictor effect predominates. Norepinephrine acts predominantly on α-adrenoceptors to induce peripheral vasoconstriction, and has almost no effect on β-adrenoceptors. In addition, the metabolic effects of epinephrine are much stronger than those of norepinephrine9. According to the catecholamine effect, several mechanisms are adopted to explain the increase in blood lactate concentrations. The first is the metabolic effect of catecholamines. Not only do catecholamines have the ability to stimulate α 2-adrenoceptors to inhibit insulin secretion10, they are also able to augment peripheral insulin resistance primarily through β-adrenoceptor agonism11. This phenomenon has been well documented in previous studies; insulin sensitivity improves after tumor resection in subjects with pheochromocytoma12, 13. Furthermore, catecholamines boost glycogenolysis and gluconeogenesis through β-adrenoceptor activation14, 15. Additionally, the stimulatory effect of epinephrine on glucagon secretion further augments these processes. The second is the vasoconstrictor effect of catecholamines, which may give rise to tissue anoxia, resulting in anaerobic metabolism and lactate overproduction in peripheral tissues.
In the present study, we found that urine epinephrine, but not norepinephrine, was a predictor of post-operative SH/LA in patients who had undergone laparoscopic adrenalectomy. This is consistent with previous studies. Administration of epinephrine has long been shown to result in a dose-dependent increase in lactate levels16, 17. In addition, previous clinical studies have demonstrated that extrinsic infusion of epinephrine induced elevation of plasma lactate levels, whereas extrinsic norepinephrine infusion had no effect18. The release of blood lactate was shown to be highest after tumor removal5. Furthermore, correlation of intra-operative lactate with urine epinephrine but not with norepinephrine has previously been demonstrated5. Hence, the metabolic effect of epinephrine may play a more important role in SH/LA after tumor resection. However, the exact mechanism behind the increase in lactic acid remains unclear in the present study. Indeed, lactate levels follow many more metabolic processes that are not related to tissue hypoxia. The lactate-to-pyruvate ratio might be helpful to distinguish the potential underlying mechanisms.
This study also suggests that tumor size is an independent predictor of post-operative SH/LA. Researchers have indicated that larger tumors possibly exert greater endocrine activity because tumor size is proportional to the urine catecholamine level19, 20. In this study, tumor size was correlated with 24-hour urine epinephrine level, consistent with previous studies. Furthermore, previous studies have shown that patients with larger tumors are not only more susceptible to hypertensive episodes intra-operatively due to massive catecholamine release, but are also likely to demand a higher dose of catecholamine infusion to maintain hemodynamic stability19. Therefore, tumor size, correlated with endocrine activity, has a substantial impact on lactate production.
Another finding of the study was that higher BMI independently predicted post-operative SH/LA. Other researchers have linked obesity to metabolic disorders21. Increased levels of circulating fatty acids, released by adipocytes in patients with obesity, impair muscular glucose uptake and utilization, leading to many of the metabolic changes observed22. Furthermore, tumor necrosis factor-α, generated by adipocytes, also impairs insulin action23, 24. In addition, a positive correlation was found between BMI and operative time, post-operative complications, and hospital stay in patients undergoing laparoscopic adrenalectomy25. The longer duration of operation may promote catecholamine release due to prolonged stimulation of the tumor. Thus, obesity, together with epinephrine, may facilitate lactate production by boosting glycometabolism.
Increased lactate levels usually reflect increased morbidity in patients undergoing cardiac surgery, in septic patients, or in patients after resuscitation26, 27. Furthermore, various studies have suggested that any increase in arterial lactate level is a strong and independent risk factor for death28,29,30. Thus, lactic acidosis has a high prognostic value. In the present study, patients with SH/LA had a longer duration of mechanical ventilation and post-operative hospitalization, reflecting more severe disease progression.
Unexpectedly, the incidence of diabetes mellitus in the SH/LA group was lower than that in the normolactatemia group. Diabetes mellitus is one of the metabolic complications of pheochromocytoma. Catecholamines are able to mobilise fuel in human body to meet the energy requirements, thus playing an vital role in carbohydrate metabolism. Twenty-five patients (17.2%) in the present study with pheochromocytoma concurrently had diabetes mellitus. However, the urine hormone levels in our study showed no difference between the three groups, which indicated that the incidence of diabetes mellitus secondary to pheochromocytoma was not statistically different between the three groups. Consequently, we divided diabetes mellitus into primary and secondary diabetes mellitus and that found neither made a difference among the three groups. Thus, secondary diabetes mellitus may be a confounder, impacting the result of Chi Square test.
The strength of this study is the high number of cases, given the low frequency of pheochromocytoma. There have been previous reports on the occurrence of SH/LA in this condition, but these are mainly case reports6, 31. Moreover, a multivariate analysis of risk factors has not been reported as yet. Although Suzuki et al. found that urine epinephrine level showed a moderate correlation with intra-operative peak plasma lactate level5, the logistic regression method used in that study did not meet the statistical conditions due to the limited sample size. Furthermore, besides urine epinephrine, the present study also found that BMI and tumor size were independent predictors of elevation of plasma lactate levels. This information is helpful for clinicians to evaluate and manage SH/LA more effectively.
The study presents several significant clinical findings. First, SH/LA was shown, for the first time, to be a relatively common complication after laparoscopic resection of pheochromocytoma; this warrants attention. Second, excessive catecholamine secretion as a result of pheochromocytoma resection may induce SH/LA, and the effect of epinephrine might be stronger than that of norepinephrine. Consequently, it is meaningful to monitor the real-time trends of blood lactate and catecholamine levels peri-operatively, especially for subjects with epinephrine-secreting tumors. Intensive care management of patients with elevated lactate may be required. Third, higher BMI and larger tumor size may exacerbate lactate generation. Thus, patients with two or three of the independent risk factors may be more susceptible to post-operative SH/LA. Clinicians should be aware of this in order to make appropriate preparations to avoid the complication.
Despite the limitations inherent in this single-center retrospective review, we found a relatively high incidence of post-operative SH/LA (15.2%). A multi-center prospective study may be desirable to further verify our conclusion. Unfortunately, the availability of peri-operative data, especially the post-operative lactate level, was limited because of the study’s design. Thus, it would be useful to monitor the post-operative lactate variation trend in a future study.
Conclusions
In conclusion, post-operative SH/LA was a relatively frequent complication (15.2%) of laparoscopic resection for pheochromocytoma. A higher 24-hour urine epinephrine level, larger tumor size, and higher BMI were independent predictors of post-operative SH/LA.
Methods
Study population
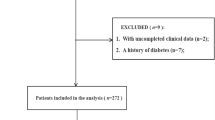
We retrospectively enrolled 145 patients (>16 years old) who underwent laparoscopic resection for pheochromocytoma in our centre between March 2011 and June 2014. Those with an associated paraganglioma and those who experienced conversion were excluded from the analysis. Ethical approval (Ethical Committee No. S-K124) was provided by the Institutional Research and Ethics Committee of the Peking Union Medical College Hospital Beijing, China (Chairperson Prof Long-cheng Li). This committee waived the need for informed consent from all eligible patients.
Laboratory and clinical parameters
In our centre, the blood lactate reference range was 0–2.5 mmol/L. MH was defined as serum lactate of 2.5–5.0 mmol/L without evidence of acidosis (pH > 7.35 and/or bicarbonate >20 mmol/L). LA was defined as pH < 7.35, bicarbonate <20 mmol/L and serum lactate ≥5 mmol/L. SH was defined as lactate ≥5 mmol/L. According to lactate level and acid-base status, patients were divided into three groups: the normolactatemia group, MH group, and SH/LA group. The first two groups were combined while performing univariate and multivariate analysis for predictors of post-operative SH/LA. Arterial blood samples were taken for measurement of lactate, performed using an arterial blood gas analyzer. Two blood samples were taken as soon as possible after the operation was finished. In our center, radial artery puncture is routinely performed before surgery to monitor intra- and post-operative invasive arterial blood pressure in patients with pheochromocytomata; this offers convenience for blood sampling. We used an arterial blood collection syringe (22 G × 1″BD Preset EclipseTM) produced by Becton, Dickinson and Company to take blood samples from the radial artery intra- and post-operatively. The post-anesthesia care unit is equipped with an ABL800 FLEX blood gas analyzer from Radiometer Medical. All blood samples underwent arterial blood analysis within 30–60 seconds of being obtained.
Variables comprised patient demographics, clinical history, laboratory data, and intra-operative details. Demographic data included age, sex, BMI, American Society of Anesthesiologists (ASA) classification, family history, clinical symptoms, and coexistent disease. Pre-operative laboratory analysis included serum hemoglobin and 24-hour urine catecholamine concentrations. Clinical data included duration and dose of alpha-blockade, kinds of pre-operative antihypertensive medications, tumor size, tumor location, length of intensive care unit stay, duration of mechanical ventilation, and length of post-operative hospitalization. Operative details included pre-operative mean arterial blood pressure measurement, pre-operative heart rate, maximum and minimum intra-operative systolic blood pressure measurements, maximum and minimum intra-operative heart rate, propofol dose, vasopressor and vasodilator usage, total volume of fluids administered, type of fluid infused, surgical approach, pneumoperitoneum pressure, volume of urine output, volume of blood loss, and anesthetic and operative durations.
Statistical analysis
Continuous data were classified as being normally distributed or not by Q-Q plot. The mean ± standard deviation, median (25th percentile, 75th percentile), and n (%) were used to express normally distributed continuous data, non-normally distributed continuous data, and categorical data, respectively. All parameters were labelled in Tables 1–4 according to their data type. Overall differences between the three groups were evaluated using one-way ANOVA (normally distributed continuous data), Kruskal-Wallis test (non-normally distributed continuous data) and Chi square test (categorical data). For parameters with an overall p value < 0.05, post-hoc analysis followed the Bonferroni method (normally distributed continuous data) and the Nemenyi test (non-normally distributed continuous data), and partitions of the Chi square method (categorical variables) were performed for all pairwise multiple comparisons. Using multivariate logistic regression, we determined factors associated with post-operative SH/LA. And variables with a p value < 0.10 on univariate analysis were entered into a multivariate logistic regression analysis. Statistical significance was defined as p < 0.05. SPSS version 19.0 (IBM, SPSS, Inc.) was used to perform all statistical analyses.
References
Pacak, K. Preoperative management of the pheochromocytoma patient. J Clin Endocrinol Metab 92, 4069–4079 (2007).
McCallum, R. W. & Connell, J. M. Laparoscopic adrenalectomy. Clin Endocrinol (Oxf) 55, 435–436 (2001).
Levy, B., Desebbe, O., Montemont, C. & Gibot, S. Increased aerobic glycolysis through beta2 stimulation is a common mechanism involved in lactate formation during shock states. Shock 30, 417–421 (2008).
Kraut, J. A. & Madias, N. E. Treatment of acute metabolic acidosis: a pathophysiologic approach. Nat Rev Nephrol 8, 589–601 (2012).
Suzuki, K., Tanaka, S., Uchida, T., Nakazawa, K. & Makita, K. Catecholamine release induces elevation in plasma lactate levels in patients undergoing adrenalectomy for pheochromocytoma. J Clin Anesth 26, 616–622 (2014).
Madias, N. E., Goorno, W. E. & Herson, S. Severe lactic acidosis as a presenting feature of pheochromocytoma. Am J Kidney Dis 10, 250–253 (1987).
Fujii, M., Kawabata, Y., Hayashi, T., Nishimae, H. & Masuko, S. Hyperlactemia during undiagnosed pheochromocytoma resection under laparoscopy. Masui 61, 197–199 (2012).
Kraut, J. A. & Madias, N. E. Lactic acidosis. New Engl J Med 371, 2309–2319 (2014).
Ensinger, H. & Georgieff, M. Is sepsis and septic shock due to a global oxygen insufficiency? A review in 2 parts. 2: Sepsis and lactate. Anasthesiologie Intensivmedizin Notfallmedizin Schmerztherapie 31, 205–215 (1996).
Yamaguchi, N. Sympathoadrenal system in neuroendocrine control of glucose: mechanisms involved in the liver, pancreas, and adrenal gland under hemorrhagic and hypoglycemic stress. Can J Physiol Pharmacol 70, 167–206 (1992).
Deibert, D. C. & DeFronzo, R. A. Epinephrine-induced insulin resistance in man. J Clin Invest 65, 717–721 (1980).
Bluher, M., Windgassen, M. & Paschke, R. Improvement of insulin sensitivity after adrenalectomy in patients with pheochromocytoma. Diabetes Care 23, 1591–1592 (2000).
Wiesner, T. D., Bluher, M., Windgassen, M. & Paschke, R. Improvement of insulin sensitivity after adrenalectomy in patients with pheochromocytoma. J Clin Endocrinol Metab 88, 3632–3636 (2003).
Sherwin, R. S. & Sacca, L. Effect of epinephrine on glucose metabolism in humans: contribution of the liver. Am J Physiol 247, E157–E165 (1984).
Steiner, K. E., Stevenson, R. W., Green, D. R. & Cherrington, A. D. Mechanism of epinephrine’s glycogenolytic effect in isolated canine hepatocytes. Metabolism 34, 1020–1023 (1985).
Griffith, F. R. Jr., Lockwood, J. E. & Loomis, T. A. The effect of intra-arterially injected adrenalin on blood flow, sugar retention and lactate output of the leg tissues of anesthetized cats. Am J Physiol 146, 677–688 (1946).
Griffith, F. R. Jr. et al. The effect of intravenous adrenalin on blood flow, sugar retention, lactate output and respiratory metabolism of peripheral (leg) tissues in the anesthetized cat. Am J Physiol 149, 64–76 (1947).
Levy, B., Perez, P., Perny, J., Thivilier, C. & Gerard, A. Comparison of norepinephrine-dobutamine to epinephrine for hemodynamics, lactate metabolism, and organ function variables in cardiogenic shock. A prospective, randomized pilot study. Crit Care Med 39, 450–455 (2011).
Namekawa, T. et al. Clinical predictors of prolonged postresection hypotension after laparoscopic adrenalectomy for pheochromocytoma. Surgery 159, 763–770 (2016).
Bruynzeel, H. et al. Risk Factors for hemodynamic instability during surgery for pheochromocytoma. J Clin Endocrinol Metab 95, 678–685 (2010).
Eckel, R. H., Grundy, S. M. & Zimmet, P. Z. The metabolic syndrome. Lancet 365, 1415–1428 (2005).
Boden, G., Chen, X., Ruiz, J., White, J. V. & Rossetti, L. Mechanisms of fatty acid-induced inhibition of glucose uptake. J Clin Invest 93, 2438–2446 (1994).
Donnelly, R. & Qu, X. Mechanisms of insulin resistance and new pharmacological approaches to metabolism and diabetic complications. Clin Exp Pharmacol Physiol 25, 79–87 (1998).
Hasin, Y., Kneen, M. M., Craik, D. J. & Nayler, W. G. Relationship between ATP resynthesis and calcium accumulation in the reperfused rat heart. Clin Exp Pharmacol Physiol 19, 79–87 (1992).
Erbil, Y. et al. The effect of retroperitoneal fat mass on surgical outcomes in patients performing laparoscopic adrenalectomy: the effect of fat tissue in adrenalectomy. Surg Innov 17, 114–119 (2010).
Demers, P., Elkouri, S., Martineau, R., Couturier, A. & Cartier, R. Outcome with high blood lactate levels during cardiopulmonary bypass in adult cardiac operation. Ann Thorac Surg 70, 2082–2086 (2000).
Casserly, B. et al. Lactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign database. Crit Care Med 43, 567–573 (2015).
Shapiro, N. I. et al. Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med 45, 524–528 (2005).
Vanni, S. et al. Prognostic value of plasma lactate levels among patients with acute pulmonary embolism: the thrombo-embolism lactate outcome study. Ann Emerg Med 61, 330–338 (2013).
van Beest, P. A. et al. Cumulative lactate and hospital mortality in ICU patients. Ann Intensive Care 3, 6 (2013).
Zaludik, J., Schuitemaker, F., DeWaal, R., Veldjuijzen, B. & Van der Meer, N. Severe lactate acidosis and cardiogenic shock: a rare manifestation of a phaeochromocytoma. Anaesth Intensive Care 38, 593–594 (2010).
Acknowledgements
We acknowledge Yue Qiu and Min Wei (Department of Anesthesiology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100730, P. R. China) for their assistance in the implementation of the study.
Author information
Authors and Affiliations
Contributions
S.W., W.C., and Y.H. designed the study protocol and wrote the manuscript. L.X. and L.S. participated in the study design and revised the manuscript. A.Z. collected the data and performed statistical analysis. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Wu, S., Chen, W., Shen, L. et al. Risk factors of post-operative severe hyperlactatemia and lactic acidosis following laparoscopic resection for pheochromocytoma. Sci Rep 7, 403 (2017). https://doi.org/10.1038/s41598-017-00467-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-00467-3
This article is cited by
-
Pre- versus post-operative untargeted plasma nuclear magnetic resonance spectroscopy metabolomics of pheochromocytoma and paraganglioma
Endocrine (2022)
-
Perioperative Aspekte in der Behandlung Katecholamin-produzierender Tumoren
Journal für Klinische Endokrinologie und Stoffwechsel (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.