Abstract
Dengue, a mosquito-transmitted viral disease, has posed a public health challenge to Singaporean residents over the years. In 2020, Singapore experienced an unprecedented dengue outbreak. We collected a dataset of geographical dengue clusters reported by the National Environment Agency (NEA) from 15 February to 9 July in 2020, covering the nationwide lockdown associated with Covid-19 during the period from 7 April to 1 June. NEA regularly updates the dengue clusters during which an infected person may be tagged to one cluster based on the most probable infection location (residential apartment or workplace address), which is further matched to fine-grained spatial units with an average coverage of about 1.35 km2. Such dengue cluster dataset helps not only reveal the dengue transmission patterns, but also reflect the effects of lockdown on dengue spreading dynamics. The resulting data records are released in simple formats for easy access to facilitate studies on dengue epidemics.
Measurement(s) | dengue infection locations |
Technology Type(s) | NEA’s disclosured report |
Factor Type(s) | Singapore’s dengue in in 2020 |
Similar content being viewed by others
Background & Summary
Dengue, a mosquito-borne viral infection transmitted to humans by Aedes aegypti (https://www.who.int/health-topics/dengue-and-severe-dengue), is prevalent in tropics and subtropics1. The dengue virus (DENV) is grouped into four closely related, but antigenically distinct and genetically diverse serotypes (DENV 1–4)2. Limited understanding of the immunological interactions among serotypes has hampered the development of effective vaccines3. Scientists estimate that dengue causes a worldwide symptomatic disease in 60 to 100 million population each year with 14 to 20 thousand annual deaths4,5.
As a city-state located in the tropics, Singapore’s climate and the highly urbanized environment make it ideal for the breeding of Aedes mosquitoes and transmission of dengue6,7,8. Dengue has been an endemic disease of Singapore and posing a public health challenge to the residents9,10,11. In 2020, Singapore had been facing the worst dengue outbreak. The cumulative number of dengue cases stood at more than 32000 as of 19 Oct 2020 (https://www.nea.gov.sg/dengue-zika/dengue/dengue-cases), which was the worst toll since 2013 when a total of 22,170 cases were reported (https://www.moh.gov.sg/docs/librariesprovider5/resources-statistics/reports/vector-borne–zoonotic-diseases.pdf). What makes the case of that year’s dengue spreading even more special is that the spike in early May coincided with Singapore’s COVID-19 lockdown period, named “circuit breaker (CB)”, from 7 April to 1 June. Before the lockdown, non-essential workers were no longer allowed to go to work on 27 March (https://www.gov.sg/article/covid-19-circuit-breaker-closure-of-workplace-premises). This nationwide lockdown was tightened from 7 April to 4 May when all business, social, or activity that cannot be conducted through telecommuting were suspended, and only essential services (e.g., supermarkets) remained open with minimum staff on premises. The lockdown was later extended to 1 June when limited additional economical activities were allowed (https://sso.agc.gov.sg/SL-Supp/S254-2020/Published/20200407?DocDate=20200407). The reopening process went through two different stages by the day of 9 July, 2020, where workplaces with safe management measures were reopened on 2 June (https://www.gov.sg/article/ending-circuit-breaker-phased-approach-to-resuming-activities-safely) and social gatherings of up to five people are allowed since June 19 (https://www.channelnewsasia.com/news/singapore/covid-19-phase-2-of-reopening-to-start-from-jun-19-social-12835758). Scientists argue that a factor that may have contributed to worsening the dengue outbreak that year was the lockdown measures: when more people were staying at home all the time, there may be more residential mosquito breeding and more opportunities for “blood meals” (https://www.channelnewsasia.com/news/singapore/mosquito-singapore-dengue-clusters-weekly-historical-high-12831856; https://edition.cnn.com/2020/07/03/asia/singapore-dengue-intl-hnk/index.html).
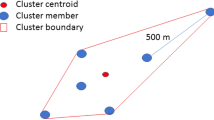
An open dengue dataset that covers the lockdown period may help facilitate exploring how the lockdown measures have affected the dengue outbreak. We collected the weekly dengue clusters from 15 February to 9 July in Singapore, which covers the whole nationwide lockdown period. A dengue cluster is formed and dynamically updated by NEA when two or more cases have onset within 14 days and are located within 150 m of each other based on the apartment block or the workplace address. To facilitate utilizing the dataset, we map the location record in the dengue clusters into the smallest spatial unit of Singapore, named the subzone (https://data.gov.sg/dataset/master-plan-2014-subzone-boundary-no-sea?resource_id=c30bfcc0-7e23-4959-b4d9-c5da5e00af54). Specifically, the Urban Redevelopment Authority (URA) of Singapore divides Singapore into 323 subzones, where each of them is typically centred around a focal point such as a neighbourhood centre or a commercial centre. Singapore covers a total area of 781.9 km2 and owns 5.7 million residents, with a high average population density at 7866 per km2 (https://www.citypopulation.de/php/singapore-admin.php). Except for those subzones with a population density lower than 10 per km2, the mean coverage of each of the other subzones is only about 1.35 km2. We map the dengue cases that are involved in the dengue clusters into the corresponding subzones.
After the map matching, each data record in the published dataset denotes an infection location (apartment block or workplace address) for a given week. A record contains record ID, latitude, longitude, date, cases, cluster label and the subzone ID. The date denotes the end of the week when the cluster was reported. The subzone ID is labelled by the shapefile that is described in the Methods section. With this dataset, both the spatial and temporal information of dengue transmission localities reported from 15 February to 9 July are recorded. This detailed record of an unprecedented dengue outbreak in Singapore before, during and after an unprecedented nationwide lockdown would be of high values to studies on risk estimation and system dynamics of dengue transmission, as well as the effects of lockdown on disease spreading and control.
Methods
Original data sources
The main data source is the dengue cluster records. Information of dengue clusters with infection locations comes from NEA (https://www.nea.gov.sg/dengue-zika/dengue/dengue-clusters). As aforementioned, a dengue cluster is formed by NEA when two or more cases have onset within 14 days and are located within 150 m of each other based the reported infection location. Here a location refers to the street address of an infected person’s workplace or homeplace down to the apartment block level. Such dengue cluster data is collected once or twice a week and each location is further labelled with the corresponding latitude and longitude by SGCharts (http://outbreak.sgcharts.com/data). The timestamp of the reported dengue clusters in the original data is recorded as the end date of the week within which the dengue case was reported. Note that the imported dengue cases are not included in the records as such cases are not disclosed by NEA.
Another open data source is the data that defines the subzone boundaries. The indictive polygon of the subzone boundary is defined by a shapefile, which is a data format widely used in the geographic information system (GIS). It can be downloaded from the online open data platform of Singapore (https://data.gov.sg/dataset/master-plan-2014-subzone-boundary-no-sea?resource_id=c30bfcc0-7e23-4959-b4d9-c5da5e00af54). For convenient usage, the shapefile data that defined the subzone boundary is also disclosed at figshare12. In the shapefile, each subzone boundary is defined by a polygon with a subzone ID.
Mapping locations to subzones
We utilize the ArcGIS Desktop platform with the ArcMap (version 10.4.1) module and the embedded ArcToolbox to match each location in the original dengue cluster data to the corresponding subzone. The downloaded shapefile that defines the subzone boundary is first added to ArcMap. The original location involved in the dengue clusters is stored in a comma-separated value (CSV) file, which contains the “latitude” and “longitude” of the reported infected location (apartment block or workplace address). The CSV file is then added to ArcMap, and the latitude and longitude are together displayed by choosing the “Geographic Coordinate Systems” as “WGS_1984”. After loading the CSV file, the data in the CSV file is uploaded into a software embedded table in the ArcMap. Before matching these locations to subzones, the embedded table should be converted to a shapefile by utilizing the toolbox of “ConversionTool- > To Shapefile”. Then we load the converted.shp file, which is opened as a table. The.shp file that defines the subzone boundary is then added to ArcMap. By using the “Spatial Join” toolbox to the two added layers, locations labelled with latitude and longitude are mapped to the corresponding subzones. With such map matching, the cumulative number of locations that are involved in the dengue clusters in each subzone during the period from 15 February to 9 July can be calculated. The geographical distribution of the mapping results is shown in Figs. 1 and 2.
Data Records
The dataset is released as a CSV file, which can be openly downloaded13. The total time period that the dataset covers is from 15 February to 9 July in 2020. It contains a total of 16116 records. The data file is named “dengue outbreak_Singapore_2020.csv”, where each item (row) contains a few elements as follows:
-
record ID: the data record id.
-
latitude: numerical value for the latitude of the location.
-
longitude: numerical value for the longitude of the location.
-
date: the end date of the week when the location was reported to be enrolled in the dengue cluster by NEA. For example, “20200228” denotes the week from 22 February to 28 February in 2020.
-
case number: number of reported dengue cases with onset in last 2 weeks at this location. New cases at this location for the corresponding week could be calculated by comparing the cases with those in the last week.
-
cluster label: numerical label of a cluster for the given week.
-
subzone ID: the ID of the subzone in which the workplace or homeplace of the case is located. Note that the subzone ID is defined by the shapefile that can be downloaded12. Each subzone is a spatial polygon as shown in Fig. 1.
The following Table 1 gives an example of the data items.
Technical Validation
Dengue infection locations in subzones over weeks
All dengue clusters are recorded in 21 weeks from 15 February to 9 July, which covers the nationwide lockdown period from 7 April to 1 June. The dataset of these 21 weeks is thus classified into three parts, namely before lockdown (BL), CB, and after lockdown (AL) respectively.
For each week, we first rank the subzones in a descending order in terms of the number of locations inside the subzone in that week. Then we count the number of top-ranked subzones with cumulatively no fewer than a certain percentage of all the locations. The results are shown in Fig. 3. As can be observed, when the percentage is set to be 100%, meaning that all locations are taken into account, there was a significant increase in the subzone number starting in the second half of May. This indicates that the dengue transmission locations were dispersed to more subzones which were originally free of dengue clusters. It is interesting to observe that this dispersion started before lockdown officially came to an end. The reasons leading to it may need some further investigation.
Further observations show that, when the cumulative percentage is respectively set as 30%, 50%, and 70%, the corresponding subzone numbers remain relatively stable at low values. It means that, for most of time, a small number of subzones (fewer than 30 subzones before 19 June) contained no fewer than 70% of all the dengue infection locations. Even when the percentage value is set to be 90%, though the subzone number started to increase in May, it kept as being less than 85 in all weeks. Only when the percentage is set as 100%, a significantly larger number of subzones are enrolled starting in May. These newly enrolled subzones, combined together, contain no more than 10% of all the dengue infection locations. Take a specific week from 16 May to 22 May as an example, 90% of all locations were reported in 48 subzones, while the other 10% of locations are scattered in 31 subzones. Note that in the last two weeks of May, the number of the enrolled subzones increased while the number of reported infection locations still remained largely stable. When it came to June and July of 2020, however, the number of enrolled subzones further increased, accompanied with a significant increase in the number of infecting locations.
Infection location number changes in subzones during lockdown
By looking into the time series of location number in each subzone, some details of the location number changes in the three periods (BL, CB, and AL respectively) could be observed. Specifically, given a subzone z, the average location number, loci, j, in each period is calculated as
where i is the subzone ID of the location record in the dataset and j is the end date of the week in the data record. nBL, nCB, and nAL are respectively the number of weeks for each period (BL, CB, and AL). Looking into the time series, two different types of changes can be observed in different subzones, which are respectively defined as follows.
-
CASE 1: the number of location number, which are involved in the dengue clusters, increased during the nationwide lockdown and it subsequently decreased after the lockdown.
-
CASE 2: the location number sharply decreased during the lockdown and rose back after the lockdown.
We have that \({A}_{z}^{BL} < {A}_{z}^{CB} > {A}_{z}^{AL}\) for CASE 1 and \({A}_{z}^{BL} > {A}_{z}^{CB} < {A}_{z}^{AL}\) for CASE 2.
The time series of these two special cases may help anchor which areas in Singapore have been potentially influenced by the lockdown in terms of the reported location. The subzones for the two different cases are shown in Fig. 4. The corresponding geographical locations of these subzones for CASE 1 and CASE 2 are illustrated in Fig. 5.
Usage Notes
The data are useful for investigating the spatial and temporal dengue risk at a fine-grained spatial resolution. An important note is that the dataset contains only the dengue cases that are involved in the dengue clusters. There are sporadic cases that are not part of clusters, and NEA presumes that such cases may acquire the disease elsewhere outside their home or workplace. Such sporadic cases are not involved in our dataset. Researchers who intend to model the dengue case variation may need to keep this fact in mind while using this data set. The dengue cluster data set may also be integrated with other datasets, such as the rainfall, temperature, and vegetation index data, etc., for estimating the dengue transmission risks.
The time period of this dataset covers the national lockdown period from April 7 to June 1 and involves seven weeks before the lockdown and six weeks after the lockdown as well. The commuting patterns started to change when lockdown preparation started on 27 March 2020 and experienced some drastic changes during the lockdown period before going through two different stages of reopening. As previous investigations have certified, human mobility is one of the main factors affecting the spatial transmission of dengue. Thus, this dataset may also contribute to helping assess the effects of human mobility on the spatial and temporal transmission of dengue in the highly urbanized city-state of Singapore.
An important factor that may need to be taken into account when using this data set to investigate the mobility effects on dengue transmission is the changes in population immunity: the main serotype of dengue virus in year 2020 was the DENV-3, whereas in the past three decades, the main serotype of dengue in Singapore had steadily been the DENV-1 or DENV-2. Another factor that needs to be considered is the resurgence of the mosquito population during this period of time. NEA reported observing a five-fold increase in the incidents of mosquito larvae in homes and common corridors in residential areas during the two-month circuit breaker period compared to those in two months prior.
Code availability
Matlab codes for data analysis of calculating the dengue locations in subzones over weeks are available at the figshare repository14.
References
Van Panhuis, W. G. et al. Region-wide synchrony and traveling waves of dengue across eight countries in southeast asia. PNAS 112, 13069–13074 (2015).
Guzman, M. G. & Harris, E. Dengue. The Lancet 385, 453–465 (2015).
Stoddard, S. T. et al. House-to-house human movement drives dengue virus transmission. PNAS 110, 994–999 (2013).
Messina, J. P. et al. The current and future global distribution and population at risk of dengue. Nature Microbiology 4, 1508–1515 (2019).
Bhatt, S. et al. The global distribution and burden of dengue. Nature 496, 504–507 (2013).
Ong, J. et al. A novel entomological index, aedes aegypti breeding percentage, reveals the geographical spread of the dengue vector in singapore and serves as a spatial risk indicator for dengue. Parasites & vectors 12, 17 (2019).
Ooi, E. E., Goh, K. T. & Gubler, D. J. Dengue prevention and 35 years of vector control in singapore. Emerg Infect Dis. 12, 887 (2006).
Salje, H. et al. Revealing the microscale spatial signature of dengue transmission and immunity in an urban population. PNAS 109, 9535–9538 (2012).
Lee, K. S. et al. Dengue virus surveillance for early warning, singapore. Emerg Infect Dis. 16(5), 847 (2010).
Goh, K. Changing epidemiology of dengue in singapore. The Lancet 346, 1098 (1995).
Ooi, E. E., Hart, T. J., Tan, H. C. & Chan, S. H. Dengue seroepidemiology in singapore. The Lancet 357, 685–686 (2001).
Huang, L. P. shapefile for subzones of Singapore, Figshare, https://doi.org/10.6084/m9.figshare.19800040.v1 (2022).
Huang, L. P. Geographical clusters of dengue outbreak in Singapore during the COVID-19 nationwide lockdown of 2020, Figshare, https://doi.org/10.6084/m9.figshare.20417658.v1 (2022).
Huang, L. P. code for dengue outbreak in Singapore, Figshare, https://doi.org/10.6084/m9.figshare.19322213.v1 (2022).
Acknowledgements
This work was partially supported by National Research Foundation (NRF), Singapore, under Virtual Singapore-Phase II programme, contact no. NRF2017VSG-AT3DCM001-045, and the National Natural Science Foundation of China under 61902145.
Author information
Authors and Affiliations
Contributions
Liping Huang contributed to data acquisition, data processing and report writing. Gaoxi Xiao contributed to methodology development, data processing, and report writing and revision. Hechang Chen contributed to data acquisition and data processing. All the other authors contributed to methodology refinement and report revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, L., Xiao, G., Chen, H. et al. Geographical clusters of dengue outbreak in Singapore during the Covid-19 nationwide lockdown of 2020. Sci Data 9, 547 (2022). https://doi.org/10.1038/s41597-022-01666-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41597-022-01666-y