Abstract
Autonomic regulation of blood pressure and cardiac rhythm progressively declines with increasing age. Impaired cardiovascular control promotes a variety of age-related cardio-vascular conditions. This study aims to provide a database of high-resolution biological signals to describe the effect of healthy aging on cardiovascular regulation. Electrocardiogram and continuous non-invasive blood pressure signals were recorded simultaneously at rest in 1,121 healthy volunteers. With this database, we provide raw signals as well as basic demographic information such as gender and body mass index. To demonstrate validity of the acquired data, we present the well-known decline of heart rate variability with increasing age in this database.
Measurement(s) | Cardiovascular autonomic function |
Technology Type(s) | Physiological signals |
Sample Characteristic - Organism | Homo sapiens |
Similar content being viewed by others
Background & Summary
As the elderly population has a high prevalence of cardiovascular diseases, representing the globally leading cause of death, it is essential to detect bodily changes that adumbrate cardiovascular impairments1. In addition, impairment of autonomic regulation of the cardiovascular system seems to accelerate the decline of cognitive performance and promotes the risk to develop age-related diseases2,3.
It is well established that arterial and ventricular stiffening, reduction of myocardial contractility, or degeneration of organ innervation impair cardiovascular function in an aged population and promote sustained hypertension, thrombosis, and atherosclerosis4. Recent scientific studies have suggested that an elevation of blood pressure and signs of thrombosis in midlife increase the risk to develop Alzheimer’s disease or other dementias in later life5,6.
A decreased sensitivity of vagal reflexes such as respiratory sinus arrhythmia leads to elevated heart rates and diminished heart rate variability in elderly participants7,8,9. The feedback loop decelerating heart rate due to increasing blood pressure, i.e. baroreflex function, is progressively diminished with increasing age. Structural changes such as the loss of sinoatrial pacemaker cells and left ventricular hypertrophy as well as functional changes of receptors initiating autonomic reflexes (e.g. baroreceptors) contribute to an altered cardiovascular regulation related to aging10,11.
Lower levels of vagally modulated HRV have been associated with increased cardiovascular morbidity and mortality in the elderly12. Hillebrand et al. reported that healthy participants with diminished resting heart rate variability (HRV) have a 32–45% increased risk to suffer from a first cardiovascular event13. Resting heart rate and HRV were demonstrated to predict cardiovascular disease as well as cardiac and overall mortality14.
In this study, we enrolled healthy volunteers between 2010 to 2020. Participants were recruited from the local community as well as employees of the University Hospital. We recorded electrocardiograms and continuous noninvasive blood pressure at carefully controlled resting state conditions in our laboratory with a constant well-defined room temperature and humidity, a defined illumination level and without any environmental noise. Available data might be used to describe the influence of aging on cardiovascular autonomic regulation to better understand mechanisms of healthy aging in contrast to pathological changes.
Methods
Participants
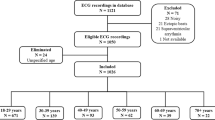
Resting state physiological recordings of 1,121 healthy volunteers were obtained. Exclusion criteria were any medical conditions, illegal drugs or medication potentially influencing cardiovascular function. Thorough physical examination, resting electrocardiography (ECG) and routine laboratory parameters (electrolytes, basic metabolic panel, and blood count) had to be without any pathological finding (results are not part of the database). Demographic information is depicted in Table 1.
Human subjects
The study was approved by the ethics committee of the Friedrich-Schiller-Universität Jena. All research was performed in accordance with relevant guidelines and regulations. Informed written consent and consent for anonymous data sharing were obtained from all participants.
Procedures
All measurements were recorded at the Department of Psychosomatic Medicine and Psychotherapy at Jena University Hospital.
ECG
An ECG (lead II) was recorded at 1000 Hz either by an MP150 (ECG100C, BIOPAC systems inc., Golata, CA, USA) or Task Force Monitor system (CNSystems Medizintechnik GmbH, Graz, AUT). Pre-gelled Ag/AgCl electrodes (BlueSensor VL, Ambu GmbH, Bad Nauheim, GER) were attached according to an Einthoven triangle (Fig. 1). ECG and continuous blood pressure were digitalized synchronously by the analog-to-digital converter incorporated in the main system (MP150 or Task Force Monitor).
Cardiovascular recordings using system 1 - the Task Force Monitor (CNSystems), or system 2 – the CNAP 500 (CNSystems) combined with an MP150 acquisition unit (BIOPAC Systems Inc.). Top left: In System 1, four electrodes have been attached at the right arm (red), the left arm (yellow), the left abdomen (green), and the right abdomen (black). Two ECG channels have been recorded between the electrodes red and yellow (lead I), and between red and green (lead II). Pressure cuffs have been attached around the left arm as well as left middle and index finger. Top right: Two ECG leads were sampled synchronously at 1000 Hz and the continuous blood pressure signal at 100 Hz. Bottom left: In System 2, three electrodes have been attached below the centre of the right clavicle (white), at the left lower thorax (7th intracoastal space at midclavicular line) (red), and at the sternum (black). One ECG channel has been recorded between the electrodes red and white (lead II). Pressure cuffs were attached around the left arm as well as left middle and index finger. Bottom right: The ECG was sampled synchronously at 1000 Hz and the continuous blood pressure signal at 100 Hz. Pictures from www.cnsystems.com and www.biopac.com adapted with permission.
Blood pressure
Continuous blood pressure was recorded non-invasively using the vascular unloading technique15. In short, a cuff around the finger is controlled to maintain constant pressure, while blood volume is recorded via photoplethysmography. With non-varying cuff pressure, the acquired blood volume is proportional to blood pressure in the arteries of the finger. The recorded signal is calibrated by an oscillometric measurement of the brachial blood pressure once during initialization of the system (measurement accuracy ± 3 mmHg). The Task Force Monitor is equipped with a module for continuous blood pressure measurement. The MP150 system digitizes the signal acquired by a separate monitor CNAP 500 (CNSystems Medizintechnik GmbH, Graz, AUT). The sampling frequency was 100 Hz for both systems.
Missing data
During some recordings, the system measured brachial blood pressure again for re-calibration. This led to loss of continuous NIBP signal over a short time span. Missing data points have been set to NaN. When demographic data was missing, respective cells were filled with NaN.
Parameters
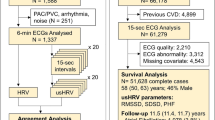
To demonstrate plausibility of collected data, we investigated a number of fundamental heart rate variability indices and their dependence on age. Therefore, heart beats were extracted and analyzed using the freely available PhysioNet Cardiovascular Signal Toolbox implemented in MATLAB (R2019a, The Mathworks, Natick, MA, USA). As exemplification, standard deviation of heart beat intervals (SDNN), root mean squared difference of successive heart beat intervals (RMSSD), and deceleration capacity (DC) was assessed using the PhysioNet Cardiovascular Signal Toolbox16. For pre-processing of heart beat interval time series, we used an adaptive filter algorithm that is also available online17. Outliers in age bins were excluded when exceeding three times the median absolute deviation18.
Measurement protocol
Measurements were performed in our autonomic laboratory that was temperature controlled at 22 °C. During recordings, the environment was quiet and fully shaded. The illumination level was kept constant via an indirect light source. The recording session started with an interview of the participant. Then, the purpose and design of the study was explained. All study volunteers gave his or her written consent to participate. Weight was measured using a person scale (SECA GmbH & Co. KG., Hamburg, GER) and height using a stadiometer (Harpenden, Holtain Ltd., Crosswell, UK).
After participants lied down comfortably on the examination tilt table, electrodes and pressure cuffs were placed. For the resting state recording, participants were instructed to avoid movement, yawning or coughing.
The instructor waited a few minutes for the participant to calm down and checked the quality of the acquired signals. In case of insufficient signal quality, electrodes and cuffs were re-arranged. Otherwise, the recording was started. The length of the recording was 8 to 35 minutes and was supervised by the instructor.
Data Records
Data are available at PhysioNet19,20. Each recording is stored as a data file with signals of ECG and blood pressure. Blood pressure values were spline-interpolated and resampled to 1000 Hz. Additional information can be found in subject-info.csv that is included in the repository.
Data anonymization
Data was anonymized using the free open-source Data Anonymization Tool ARX21. To assure that none of our participants can be identified based on demographic information, we generalized individual age to age groups. The applied a k = 2 anonymity condition and an average re-identification risk of 5%22,23. Files were pseudonymized to numbers 0001–1121 after random ordering.
Recorded data of each participant are stored in a data file (.dat) with raw signals of ECG and blood pressure. Amplitudes are included as a sequence of unsigned 16-bit integers for each signal. An associated header file is an ASCII text file storing meta information on this recording. The first line gives file name, number of signals, sampling frequency and number of samples separated by spaces (e.g., first line in 0023.hae: ‘0023 2 1000 1226975’). Each of the following lines include information regarding one signal, namely, file name, defined bit resolution, bit gain, baseline in brackets followed by a slash, units, bit resolution followed by a zero, first bit, checksum followed by a zero and signal name (e.g., second line in 0023.hae: ‘0023.dat 16 10688.4581(−12269)/mV 16 0 −13073 17059 0 ECG’). There is a script to convert wfdb files to mat format (and reverse) in the Waveform Database Software Package for MATLAB (wfdb2mat.m) available at PhysioNet24.
The table subjects.tsv gives basic demographic information i.e., age bin, gender and body mass index as well as length of recording in minutes and recording device.
Technical Validation
To explore validity of recorded data, the sample was divided into age bins of ten years (see Fig. 2). We estimated standard deviation of heart beat intervals (SDNN) and root mean square of successive differences between heart beat intervals (RMSSD), and deceleration capacity of heart beat intervals. Global heart rate variability as indicated by SDNN seems to decline progressively with advancing age (Fig. 2). DC and RMSSD suggested that short-term modulation of heart rate decreases until about 50 years of age in a linear matter. At a higher age both parameters remain nearly constant.
Code availability
For the technical validation, we used code that is publicly available without restrictions (see methods section). In detail following functions/scripts were used:
jqrs.m - QRS detector based on the Pan-Tompkins method (www.physionet.org/content/pcst)
ada_f.m – adaptive filtering of heart beat time series (www.tocsy.pik-potsdam.de/ada.php)
runrmssd.m – RMSSD estimation (www.physionet.org/content/pcst)
prsa.m – deceleration capacity estimation (www.physionet.org/content/pcst)
wfdb2mat.m – convertion of waveform database format to MATLAB file (www.physionet.org/content/wfdb-matlab/0.10.0/mcode/wfdb2mat.m).
References
Mendis, S., Puska, P. & Norrving, B. Global atlas on cardiovascular disease prevention and control. World Heal. Organ. 2–14 (2011).
Snyder, H. M. et al. Vascular contributions to cognitive impairment and dementia including Alzheimer’s disease. Alzheimer’s Dement. 11, 710–717 (2015).
Baumgart, M. et al. Summary of the evidence on modifiable risk factors for cognitive decline and dementia: A population-based perspective. Alzheimer’s Dement. 11, 718–726 (2015).
Dai, X. et al. Cardiovascular physiology in the older adults. J. Geriatr. Cardiol. 12, 196–201 (2015).
Mahinrad, S. et al. Cumulative blood pressure exposure during young adulthood and mobility and cognitive function in midlife. Circulation 712–724 https://doi.org/10.1161/CIRCULATIONAHA.119.042502 (2020).
Liang, Y. et al. Cardiovascular health metrics from mid- To late-life and risk of dementia: A population-based cohort study in Finland. PLoS Med. 17, 1–18 (2020).
Laitinen, T., Niskanen, L., Geelen, G., Länsimies, E. & Hartikainen, J. Age dependency of cardiovascular autonomic responses to head-up tilt in healthy subjects. J. Appl. Physiol. https://doi.org/10.1152/japplphysiol.00444.2003 (2004).
Boettger, M. K. et al. Influence of Age on Linear and Nonlinear Measures of Autonomic Cardiovascular Modulation. Ann. Noninvasive Electrocardiol. 15, 165–174 (2010).
Voss, A., Schroeder, R., Heitmann, A., Peters, A. & Perz, S. Short-Term Heart Rate Variability — Influence of Gender and Age in Healthy Subjects. 1–33, https://doi.org/10.1371/journal.pone.0118308 (2015).
Gribbin, B., Pickering, T. G., Sleight, P. & Peto, R. Effect of age and high blood pressure on baroreflex sensitivity in man. Circ. Res. https://doi.org/10.1161/01.RES.29.4.424 (1971).
Fukusaki, C., Kawakubo, K. & Yamamoto, Y. Assessment of the primary effect of aging on heart rate variability in humans. Clin. Auton. Res. https://doi.org/10.1007/BF02278016 (2000).
Tsuji, H. et al. Impact of Reduced Heart Rate Variability on Risk for Cardiac Events. Circulation 94, 2850–2855 (1996).
Hillebrand, S. et al. Heart rate variability and first cardiovascular event in populations without known cardiovascular disease: Meta-analysis and dose-response meta-regression. Europace 15, 742–749 (2013).
Jensen, M. T., Suadicani, P., Hein, H. O. & Gyntelberg, F. Elevated resting heart rate, physical fitness and all-cause mortality: A 16-year follow-up in the Copenhagen Male Study. Heart 99, 882–887 (2013).
Fortin, J. et al. Continuous non-invasive blood pressure monitoring using concentrically interlocking control loops. Comput. Biol. Med. 36, 941–57 (2006).
Vest, A. N. et al. An Open Source Benchmarked Toolbox for Cardiovascular Waveform and Interval Analysis. Physiol. Meas. 39, 105004 (2018).
Wessel, N. et al. Nonlinear analysis of complex phenomena in cardiological data. Herzschrittmachertherapie und Elektrophysiologie 11, 159–173 (2000).
Leys, C., Ley, C., Klein, O., Bernard, P. & Licata, L. Detecting outliers: Do not use standard deviation around the mean, use absolute deviation around the median. J. Exp. Soc. Psychol. 49, 764–766 (2013).
Goldberger, A. et al. PhysioBank, PhysioToolkit, and PhysioNet: Components of a new research resource for complex physiologic signals. Circ. 101, e215–e220 (2000).
Schumann, A. & Bär, K.-J. Autonomic Aging: A dataset to quantify changes of cardiovascular autonomic function during healthy aging. PhysioNet https://doi.org/10.13026/2hsy-t491 (2021).
Prasser, F., Eicher, J., Spengler, H., Bild, R. & Kuhn, K. A. Flexible data anonymization using ARX—Current status and challenges ahead. Softw. - Pract. Exp. 50, 1277–1304 (2020).
Sweeney, L. k-Anonymity: A Model for Protecting Privacy. Int. J. Uncertainty, Fuzziness Knowledge-based Syst. 10, 557–570 (2002).
Dankar, F. K., El Emam, K., Neisa, A. & Roffey, T. Estimating the re-identification risk of clinical data sets. BMC Med. Inform. Decis. Mak. 12, 1–15 (2012).
Silva, I., Moody, B. & Moody, G. B. An Open-source Toolbox for Analysing and Processing PhysioNet Databases in MATLAB and Octave. PhysioNet https://doi.org/10.13026/6zcz-e163 (2021).
Acknowledgements
A.S. is supported by the German Research Foundation (SCHU 3432/2-1; www.dfg.de) and the Interdisciplinary Center for Clinical Research Jena (MSP05-2019; www.uniklinikum-jena.de/izkf). K.B. is supported by the German Research Foundation (BA 3848/9-1; www.dfg.de). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
A.S. performed data analysis and wrote the manuscript. K.B. conceived the study, prepared and critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
All contributors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schumann, A., Bär, KJ. Autonomic aging – A dataset to quantify changes of cardiovascular autonomic function during healthy aging. Sci Data 9, 95 (2022). https://doi.org/10.1038/s41597-022-01202-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41597-022-01202-y
This article is cited by
-
An extensive quantitative analysis of the effects of errors in beat-to-beat intervals on all commonly used HRV parameters
Scientific Reports (2024)
-
Revisiting nonlinearity of heart rate variability in healthy aging
Scientific Reports (2023)