Abstract
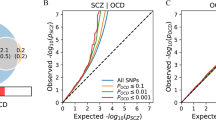
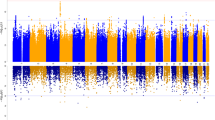
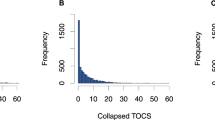
Obsessive–compulsive disorder (OCD) affects 1–2% of the population, and, as with other complex neuropsychiatric disorders, it is thought that rare variation contributes to its genetic risk. In this study, we performed exome sequencing in the largest OCD cohort to date (1,313 total cases, consisting of 587 trios, 41 quartets and 644 singletons of affected individuals) and describe contributions to disease risk from rare damaging coding variants. In case–control analyses (n = 1,263/11,580), the most significant single-gene result was observed in SLITRK5 (odds ratio (OR) = 8.8, 95% confidence interval 3.4–22.5, P = 2.3 × 10−6). Across the exome, there was an excess of loss of function (LoF) variation specifically within genes that are LoF-intolerant (OR = 1.33, P = 0.01). In an analysis of trios, we observed an excess of de novo missense predicted damaging variants relative to controls (OR = 1.22, P = 0.02), alongside an excess of de novo LoF mutations in LoF-intolerant genes (OR = 2.55, P = 7.33 × 10−3). These data support a contribution of rare coding variants to OCD genetic risk.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Gene-based collapsing analysis summary statistics are provided in Supplementary Tables 4 and 5. DNMs detected across the 587 OCD trios and 41 quartets are provided in Supplementary Tables 8 and 9, respectively. Summary statistics from extTADA analysis (including LoF counts per gene in 476 OCD cases versus 1,761 healthy controls) are provided in Supplementary Table 16. Clinical data for cases and healthy family members sequenced as part of this study are available on dbGaP (https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs000903.v1.p1).
Code availability
Extraction of sample-level coverage information and extraction of QC-passing genotypes was done using ATAV (https://github.com/igm-team/atav). Manipulation of PLINK files and subsetting according to genotype missingness were done using PLINK version 1.90_3.38 (https://www.cog-genomics.org/plink2/). Kinship analysis was performed using KING version 1.4 (http://people.virginia.edu/~wc9c/KING/). PCA was performed using FLASHPCA version 2.0 (https://github.com/gabraham/flashpca) in gene-based collapsing analysis and EIGENSOFT version 6.1.4 (https://data.broadinstitute.org/alkesgroup/EIGENSOFT/) in LoF rate comparisons. Calculation of trio-based coverage was done using mosdepth version 0.2.4 (https://github.com/brentp/mosdepth) and bedtools version 2.25.0 (https://github.com/arq5x/bedtools2/releases). Full analysis code written specifically for the analysis described in this manuscript is available in the Supplementary Software Appendix and is also available in a public repository (https://github.com/Halvee/OCD_WES_analysis_full_NatureNeuro2020).
References
Nestadt, G., Grados, M. & Samuels, J. F. Genetics of obsessive–compulsive disorder. Psychiatr. Clin. North Am. 33, 141–158 (2010).
Polderman, T. J. et al. Meta-analysis of the heritability of human traits based on fifty years of twin studies. Nat. Genet. 47, 702–709 (2015).
Stewart, S. E. et al. Genome-wide association study of obsessive–compulsive disorder. Mol. Psychiatry 18, 788–798 (2013).
Mattheisen, M. et al. Genome-wide association study in obsessive–compulsive disorder: results from the OCGAS. Mol. Psychiatry 20, 337–344 (2015).
International Obsessive Compulsive Disorder Foundation Genetics Collaborative (IOCDF-GC) & OCD Collaborative Genetics Association Studies (OCGAS). Revealing the complex genetic architecture of obsessive-compulsive disorder using meta-analysis. Mol. Psychiatry 23, 1181–1188 (2018).
Kendall, K.M. et al. Association of rare copy number variants with risk of depression. JAMA Psychiatry 76, 818–825 (2019).
Cappi, C. et al. De novo damaging DNA coding mutations are associated with obsessive–compulsive disorder and overlap with Tourette’s disorder and autism. Biol. Psychiatry 87, 1035–1044 (2020).
Wang, S. et al. De novo sequence and copy number variants are strongly associated with Tourette disorder and implicate cell polarity in pathogenesis. Cell Rep. 24, 3441–3454 (2018).
Willsey, A. J. et al. De novo coding variants are strongly associated with Tourette disorder. Neuron 94, 486–499 (2017).
Iossifov, I. et al. The contribution of de novo coding mutations to autism spectrum disorder. Nature 515, 216–221 (2014).
Adzhubei, I. A. et al. A method and server for predicting damaging missense mutations. Nat. Methods 7, 248–249 (2010).
Samocha, K. E. et al. Regional missense constraint improves variant deleteriousness prediction. Preprint at bioRxiv https://doi.org/10.1101/148353 (2017).
Havrilla, J. M., Pedersen, B. S., Layer, R. M. & Quinlan, A. R. A map of constrained coding regions in the human genome. Nat. Genet. 51, 88–95 (2019).
Traynelis, J. et al. Optimizing genomic medicine in epilepsy through a gene-customized approach to missense variant interpretation. Genome Res. 27, 1715–1729 (2017).
Karczewski, K. J. et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581, 434–443 (2020).
Satterstrom, F. K. et al. Large-scale exome sequencing study implicates both developmental and functional changes in the neurobiology of autism. Cell 180, 568–584 (2020).
Robinson, J. T. et al. Integrative Genomics Viewer. Nat. Biotechnol. 29, 24–26 (2011).
Epi, K. C. et al. De novo mutations in epileptic encephalopathies. Nature 501, 217–221 (2013).
Samocha, K. E. et al. A framework for the interpretation of de novo mutation in human disease. Nat. Genet. 46, 944–950 (2014).
Coe, B. P. et al. Neurodevelopmental disease genes implicated by de novo mutation and copy number variation morbidity. Nat. Genet. 51, 106–116 (2019).
Deciphering Developmental Disorders, S. Prevalence and architecture of de novo mutations in developmental disorders. Nature 542, 433–438 (2017).
Nguyen, H. T. et al. Integrated Bayesian analysis of rare exonic variants to identify risk genes for schizophrenia and neurodevelopmental disorders. Genome Med. 9, 114 (2017).
Howrigan, D. P. et al. Exome sequencing in schizophrenia-affected parent–offspring trios reveals risk conferred by protein-coding de novo mutations. Nat. Neurosci. 23, 185–193 (2020).
Rees, E. et al. De novo mutations identified by exome sequencing implicate rare missense variants in SLC6A1 in schizophrenia. Nat. Neurosci. 23, 179–184 (2020).
Takahashi, H. et al. Selective control of inhibitory synapse development by Slitrk3-PTPδ trans-synaptic interaction. Nat. Neurosci. 15, 389–398 (2012).
Um, J. W. & Ko, J. LAR-RPTPs: synaptic adhesion molecules that shape synapse development. Trends Cell Biol. 23, 465–475 (2013).
Um, J. W. et al. Structural basis for LAR-RPTP/Slitrk complex-mediated synaptic adhesion. Nat. Commun. 5, 5423 (2014).
Yim, Y. S. et al. Slitrks control excitatory and inhibitory synapse formation with LAR receptor protein tyrosine phosphatases. Proc. Natl Acad. Sci. USA 110, 4057–4062 (2013).
Han, K. A., Jeon, S., Um, J. W. & Ko, J. Emergent synapse organizers: LAR-RPTPs and their companions. Int. Rev. Cell Mol. Biol. 324, 39–65 (2016).
Shmelkov, S. V. et al. Slitrk5 deficiency impairs corticostriatal circuitry and leads to obsessive–compulsive-like behaviors in mice. Nat. Med. 16, 598–602 (2010).
Song, M. et al. Rare synaptogenesis-impairing mutations in SLITRK5 are associated with obsessive compulsive disorder. PLoS ONE 12, e0169994 (2017).
Singh, T. et al. Exome sequencing identifies rare coding variants in 10 genes which confer substantial risk for schizophrenia. Preprint at medRxiv https://doi.org/10.1101/2020.09.18.20192815 (2020).
Guo, H. et al. Genome sequencing identifies multiple deleterious variants in autism patients with more severe phenotypes. Genet. Med. 21, 1611–1620 (2019).
Sugathan, A. et al. CHD8 regulates neurodevelopmental pathways associated with autism spectrum disorder in neural progenitors. Proc. Natl Acad. Sci. USA 111, E4468–E4477 (2014).
Nestadt, G. et al. Obsessive–compulsive disorder: subclassification based on co-morbidity. Psychol. Med. 39, 1491–1501 (2009).
Wang, Y. et al. Gender differences in genetic linkage and association on 11p15 in obsessive–compulsive disorder families. Am. J. Med. Genet. B Neuropsychiatr. Genet. 150B, 33–40 (2009).
Khramtsova, E. A. et al. Sex differences in the genetic architecture of obsessive–compulsive disorder. Am. J. Med. Genet. B Neuropsychiatr. Genet. 180, 351–364 (2019).
Guze, S. B. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV). Am. J. Psychiatry 152, 1228–1228 (1995).
Mannuzza, S., Fyer, A. J., Klein, D. F. & Endicott, J. Schedule for Affective Disorders and Schizophrenia–Lifetime Version modified for the study of anxiety disorders (SADS-LA): rationale and conceptual development. J. Psychiatr. Res 20, 317–325 (1986).
Glasofer, D., Brown, A. J., & Riegel, M. Structured Clinical Interview for DSM-IV (SCID). (Springer, 2015).
Raghavan, N. S. et al. Whole-exome sequencing in 20,197 persons for rare variants in Alzheimer’s disease. Ann. Clin. Transl. Neurol. 5, 832–842 (2018).
Chang, C. C. et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience 4, 7 (2015).
Abraham, G., Qiu, Y. & Inouye, M. FlashPCA2: principal component analysis of Biobank-scale genotype datasets. Bioinformatics 33, 2776–2778 (2017).
Povysil, G. et al. Assessing the role of rare genetic variation in patients with heart failure. JAMA Cardiol. 6, 379–386 (2021).
Agresti, A. A survey of exact inference for contingency tables. Stat. Sci. 7, 131–153 (1992).
Cirulli, E. T. et al. Exome sequencing in amyotrophic lateral sclerosis identifies risk genes and pathways. Science 347, 1436–1441 (2015).
Rees, E. et al. Analysis of intellectual disability copy number variants for association with schizophrenia. Nat. Genet. 49, 1167–1173 (2017).
Marshall, C. R. et al. Contribution of copy number variants to schizophrenia from a genome-wide study of 41,321 subjects. Nat. Genet. 49, 27–35 (2017).
Price, A. L. et al. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 38, 904–909 (2006).
Ruden, D. et al. Using Drosophila melanogaster as a model for genotoxic chemical mutational studies with a new program, SnpSift. Front. Genet. 3, 35 (2012).
Liu, X., Jian, X. & Boerwinkle, E. dbNSFP: a lightweight database of human nonsynonymous SNPs and their functional predictions. Hum. Mutat. 32, 894–899 (2011).
Liu, X., Jian, X. & Boerwinkle, E. dbNSFP v2.0: a database of human non-synonymous SNVs and their functional predictions and annotations. Hum. Mutat. 34, E2393–E2402 (2013).
Ware, J. S., Samocha, K. E., Homsy, J. & Daly, M. J. Interpreting de novo variation in human disease using denovolyzeR. Curr. Protoc. Hum. Genet. 87, 7.25.1–7.25.15 (2015).
Acknowledgements
We are grateful to the research participants, as this study would not have been possible without their participation. This work was supported by the following National Institutes of Health grants: ‘Identifying de novo mutations causing OCD in trios by whole exome sequencing’ (MH099216—D.B.G. and G.N.); ‘Identification of rare variants of OCD’ (MH097971—D.B.G.; MH097993—G.N.). Data acquisition was made possible by the OCD Collaborative Genetics Association Study, funded by the following National Institute of Mental Health grants: MH071507 (D.G.), MH079489 (A.J.F.), MH079487 (J.M.), MH079494 (J.A.K.) and MH 071507 (G.N.).
Author information
Authors and Affiliations
Contributions
D.B.G. and G.N. conceived of and obtained funding for the research, and D.B.G. designed the experiments. J.F.S., J.K., D.G., A.J.F., B.D.G., J.T.M., O.J.B., J.A.K., M.A.R., M.A.G., P.S.N., Y.W., F.S.G. and B.M. collected samples, prepared samples for analysis or were involved in clinical evaluation. IGM staff members performed all experiments, and M.H. executed data analyses, with critical help provided by T.D.P. D.B.G., G.N., B.M., T.D.P., A.W.Z. and F.S.G. provided analysis suggestions. M.H. and D.B.G. performed the primary writing of the manuscript, with input from G.N., B.M., F.S.G., A.W.Z. and J.F.S. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
D.B.G. reports equity holdings in precision medicine companies and consultancy payments from Gilead Sciences, AstraZeneca and GoldFinch Bio. All other authors declare no competing financial interests.
Additional information
Peer review information Nature Neuroscience thanks Ditte Demontis and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–16.
Supplementary Tables
Supplementary Tables 1–16.
Supplementary Software Appendix 1
Supplementary Software
Rights and permissions
About this article
Cite this article
Halvorsen, M., Samuels, J., Wang, Y. et al. Exome sequencing in obsessive–compulsive disorder reveals a burden of rare damaging coding variants. Nat Neurosci 24, 1071–1076 (2021). https://doi.org/10.1038/s41593-021-00876-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41593-021-00876-8
This article is cited by
-
Dimensional and transdiagnostic phenotypes in psychiatric genome-wide association studies
Molecular Psychiatry (2023)
-
Comparison of three bioinformatics tools in the detection of ASD candidate variants from whole exome sequencing data
Scientific Reports (2023)
-
Rare X-linked variants carry predominantly male risk in autism, Tourette syndrome, and ADHD
Nature Communications (2023)
-
The prefrontal cortex and OCD
Neuropsychopharmacology (2022)
-
Whole exome sequencing in dense families suggests genetic pleiotropy amongst Mendelian and complex neuropsychiatric syndromes
Scientific Reports (2022)