Abstract
Although targeting oxidative phosphorylation (OXPHOS) is a rational anticancer strategy, clinical benefit with OXPHOS inhibitors has yet to be achieved. Here we advanced IACS-010759, a highly potent and selective small-molecule complex I inhibitor, into two dose-escalation phase I trials in patients with relapsed/refractory acute myeloid leukemia (NCT02882321, n = 17) and advanced solid tumors (NCT03291938, n = 23). The primary endpoints were safety, tolerability, maximum tolerated dose and recommended phase 2 dose (RP2D) of IACS-010759. The PK, PD, and preliminary antitumor activities of IACS-010759 in patients were also evaluated as secondary endpoints in both clinical trials. IACS-010759 had a narrow therapeutic index with emergent dose-limiting toxicities, including elevated blood lactate and neurotoxicity, which obstructed efforts to maintain target exposure. Consequently no RP2D was established, only modest target inhibition and limited antitumor activity were observed at tolerated doses, and both trials were discontinued. Reverse translational studies in mice demonstrated that IACS-010759 induced behavioral and physiological changes indicative of peripheral neuropathy, which were minimized with the coadministration of a histone deacetylase 6 inhibitor. Additional studies are needed to elucidate the association between OXPHOS inhibition and neurotoxicity, and caution is warranted in the continued development of complex I inhibitors as antitumor agents.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Requests for access to patient-level data from these trials should be made to the corresponding authors. For each request, an independent review panel at MD Anderson Cancer Center will convene within 30 days of the request and decide whether the data will be provided; the data will then be available for up to 12 months. Source data are available for Figs. 2, 3a–d, 3f–k, 4, and Extended Data Figs. 1–8, 9a, 9c-f, 9h, 10. Source data are provided with this paper.
References
Baccelli, I. et al. Mubritinib targets the electron transport chain Complex I and reveals the landscape of OXPHOS dependency in acute myeloid leukemia. Cancer Cell 36, 84–99 (2019).
Schockel, L. et al. Targeting mitochondrial complex I using BAY 87-2243 reduces melanoma tumor growth. Cancer Metab. 3, 11 (2015).
Andrzejewski, S., Siegel, P. M. & St-Pierre, J. Metabolic profiles associated with metformin efficacy in cancer. Front. Endocrinol. (Lausanne) 9, 372 (2018).
Kuramoto, K. et al. Development of a potent and orally active activator of adenosine monophosphate-activated protein kinase (AMPK), ASP4132, as a clinical candidate for the treatment of human cancer. Bioorg. Med. Chem. 28, 115307 (2020).
Xu, Y., Xue, D., Bankhead, A. 3rd & Neamati, N. Why all the fuss about oxidative phosphorylation (OXPHOS)? J. Med. Chem. 63, 14276–14307 (2020).
Rha, S. Y. et al. Phase I study of IM156, a novel potent biguanide oxidative phosphorylation (OXPHOS) inhibitor, in patients with advanced solid tumors. J. Clin. Oncol. 38, 3590–3590 (2020).
Sullivan, L. B. et al. Supporting aspartate biosynthesis is an essential function of respiration in proliferating Cells. Cell 162, 552–563 (2015).
Kuntz, E. M. et al. Targeting mitochondrial oxidative phosphorylation eradicates therapy-resistant chronic myeloid leukemia stem cells. Nat. Med. 23, 1234–1240 (2017).
Stuani, L. et al. Mitochondrial metabolism supports resistance to IDH mutant inhibitors in acute myeloid leukemia. J. Exp. Med. 218, e20200924 (2021).
Dykens, J. A. et al. Biguanide-induced mitochondrial dysfunction yields increased lactate production and cytotoxicity of aerobically-poised HepG2 cells and human hepatocytes in vitro. Toxicol. Appl. Pharmacol. 233, 203–210 (2008).
Bridges, H. R., Jones, A. J., Pollak, M. N. & Hirst, J. Effects of metformin and other biguanides on oxidative phosphorylation in mitochondria. Biochem. J. 462, 475–487 (2014).
Janku, F. et al. First-in-human study of IM156, a novel potent biguanide oxidative phosphorylation (OXPHOS) inhibitor, in patients with advanced solid tumors. Invest. New Drugs https://doi.org/10.1007/s10637-022-01277-9 (2022).
Sanchez, M., Gastaldi, L., Remedi, M., Caceres, A. & Landa, C. Rotenone-induced toxicity is mediated by Rho-GTPases in hippocampal neurons. Toxicol. Sci. 104, 352–361 (2008).
Betarbet, R. et al. Chronic systemic pesticide exposure reproduces features of Parkinson’s disease. Nat. Neurosci. 3, 1301–1306 (2000).
Trotta, A. P. et al. Disruption of mitochondrial electron transport chain function potentiates the pro-apoptotic effects of MAPK inhibition. J. Biol. Chem. 292, 11727–11739 (2017).
Janku, F. et al. First-in-human evaluation of the novel mitochondrial complex I inhibitor ASP4132 for treatment of cancer. Invest. New Drugs 39, 1348–1356 (2021).
Molina, J. R. et al. An inhibitor of oxidative phosphorylation exploits cancer vulnerability. Nat. Med. 24, 1036–1046 (2018).
Chung, I. et al. Cork-in-bottle mechanism of inhibitor binding to mammalian complex I. Sci. Adv. 7, eabg4000 (2021).
Samudio, I. et al. Pharmacologic inhibition of fatty acid oxidation sensitizes human leukemia cells to apoptosis induction. J. Clin. Invest. 120, 142–156 (2010).
Lagadinou, E. D. et al. BCL-2 inhibition targets oxidative phosphorylation and selectively eradicates quiescent human leukemia stem cells. Cell Stem Cell 12, 329–341 (2013).
Boultwood, J. et al. Amplification of mitochondrial DNA in acute myeloid leukaemia. Br. J. Haematol. 95, 426–431 (1996).
Lissanu Deribe, Y. et al. Mutations in the SWI/SNF complex induce a targetable dependence on oxidative phosphorylation in lung cancer. Nat. Med. 24, 1047–1057 (2018).
Piel, S., Ehinger, J. K., Elmer, E. & Hansson, M. J. Metformin induces lactate production in peripheral blood mononuclear cells and platelets through specific mitochondrial complex I inhibition. Acta Physiol. (Oxf.) 213, 171–180 (2015).
Bando, K. et al. Comparison of potential risks of lactic acidosis induction by biguanides in rats. Regul. Toxicol. Pharm. 58, 155–160 (2010).
Dohner, H. et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129, 424–447 (2017).
Nishino, M., Jagannathan, J. P., Ramaiya, N. H. & Van den Abbeele, A. D. Revised RECIST guideline version 1.1: what oncologists want to know and what radiologists need to know. Am. J. Roentgenol. 195, 281–289 (2010).
Saito, K. et al. Exogenous mitochondrial transfer and endogenous mitochondrial fission facilitate AML resistance to OxPhos inhibition. Blood Adv. 5, 4233–4255 (2021).
Deuis, J. R., Dvorakova, L. S. & Vetter, I. Methods used to evaluate pain behaviors in rodents. Front. Mol. Neurosci. 10, 284 (2017).
Curzon P, Zhang M, Radek RJ, et al. The Behavioral Assessment of Sensorimotor Processes in the Mouse: Acoustic Startle, Sensory Gating, Locomotor Activity, Rotarod, and Beam Walking. In: Buccafusco JJ, editor. Methods of Behavior Analysis in Neuroscience. 2nd edition. Boca Raton (FL): CRC Press/Taylor & Francis; 2009. Chapter 8.
Bennett, G. J., Doyle, T. & Salvemini, D. Mitotoxicity in distal symmetrical sensory peripheral neuropathies. Nat. Rev. Neurol. 10, 326–336 (2014).
Ma, J., Kavelaars, A., Dougherty, P. M. & Heijnen, C. J. Beyond symptomatic relief for chemotherapy-induced peripheral neuropathy: targeting the source. Cancer 124, 2289–2298 (2018).
Kiryu-Seo, S. & Kiyama, H. Mitochondrial behavior during axon regeneration/degeneration in vivo. Neurosci. Res. 139, 42–47 (2019).
Krukowski, K. et al. HDAC6 inhibition effectively reverses chemotherapy-induced peripheral neuropathy. Pain 158, 1126–1137 (2017).
Zhang, J., Ma, J., Trinh, R. T., Heijnen, C. J. & Kavelaars, A. An HDAC6 inhibitor reverses chemotherapy-induced mechanical hypersensitivity via an IL-10 and macrophage dependent pathway. Brain Behav. Immun. 100, 287–296 (2022).
Kirkpatrick, D. L. & Powis, G. Clinically evaluated cancer drugs inhibiting redox signaling. Antioxid. Redox Signal. 26, 262–273 (2017).
Jha, M. K., Lee, I. K. & Suk, K. Metabolic reprogramming by the pyruvate dehydrogenase kinase-lactic acid axis: linking metabolism and diverse neuropathophysiologies. Neurosci. Biobehav. Rev. 68, 1–19 (2016).
Krukowski, K., Nijboer, C. H., Huo, X., Kavelaars, A. & Heijnen, C. J. Prevention of chemotherapy-induced peripheral neuropathy by the small-molecule inhibitor pifithrin-mu. Pain 156, 2184–2192 (2015).
Flatters, S. J. L. & Bennett, G. J. Studies of peripheral sensory nerves in paclitaxel-induced painful peripheral neuropathy: evidence for mitochondrial dysfunction. Pain 122, 245–257 (2006).
Maj, M. A., Ma, J., Krukowski, K. N., Kavelaars, A. & Heijnen, C. J. Inhibition of mitochondrial p53 accumulation by PFT-mu prevents cisplatin-induced peripheral neuropathy. Front. Mol. Neurosci. 10, 108 (2017).
Xiao, W. H. & Bennett, G. J. Effects of mitochondrial poisons on the neuropathic pain produced by the chemotherapeutic agents, paclitaxel and oxaliplatin. Pain 153, 704–709 (2012).
Zheng, H., Xiao, W. H. & Bennett, G. J. Mitotoxicity and bortezomib-induced chronic painful peripheral neuropathy. Exp. Neurol. 238, 225–234 (2012).
Hirst, J. Mitochondrial complex I. Annu. Rev. Biochem. 82, 551–575 (2013).
Schapira, A. H. Complex I: inhibitors, inhibition and neurodegeneration. Exp. Neurol. 224, 331–335 (2010).
Chinnery PF. Primary Mitochondrial Disorders Overview. 2000 Jun 8 [Updated 2021 Jul 29]. In: Adam MP, Everman DB, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2022.
Stine, Z. E., Schug, Z. T., Salvino, J. M. & Dang, C. V. Targeting cancer metabolism in the era of precision oncology. Nat. Rev. Drug Discov. 21, 141–162 (2022).
Koopman, W. J., Distelmaier, F., Smeitink, J. A. & Willems, P. H. OXPHOS mutations and neurodegeneration. EMBO J. 32, 9–29 (2013).
Stephenson, Z. A. et al. Identification of a novel toxicophore in anti-cancer chemotherapeutics that targets mitochondrial respiratory complex I. eLife 9, e55845 (2020).
El-Hattab, A. W. & Scaglia, F. Mitochondrial cardiomyopathies. Front. Cardiovasc. Med. 3, 25 (2016).
Finsterer, J. & Kothari, S. Cardiac manifestations of primary mitochondrial disorders. Int. J. Cardiol. 177, 754–763 (2014).
Gillies, R. J., Robey, I. & Gatenby, R. A. Causes and consequences of increased glucose metabolism of cancers. J. Nucl. Med. 49, 24S–42S Suppl. 2 (2008).
Jha, M. K. et al. Metabolic connection of inflammatory pain: pivotal role of a pyruvate dehydrogenase kinase-pyruvate dehydrogenase-lactic acid axis. J. Neurosci. 35, 14353–14369 (2015).
Durante, M. et al. Adenosine A3 agonists reverse neuropathic pain via T cell-mediated production of IL-10. J. Clin. Invest. 131, e139299 (2021).
Ruzhansky, K. M. & Brannagan, T. H. 3rd Neuromuscular complications of hematopoietic stem cell transplantation. Muscle Nerve 52, 480–487 (2015).
Sakellari, I. et al. Neurological adverse events post allogeneic hematopoietic cell transplantation: major determinants of morbidity and mortality. J. Neurol. 266, 1960–1972 (2019).
Koeppen, S., Thirugnanasambanthan, A. & Koldehoff, M. Neuromuscular complications after hematopoietic stem cell transplantation. Support Care Cancer 22, 2337–2341 (2014).
Dowling, M. R. et al. Neurologic complications after allogeneic hematopoietic stem cell transplantation: risk factors and impact. Bone Marrow Transpl. 53, 199–206 (2018).
Siegal, D. et al. Central nervous system complications after allogeneic hematopoietic stem cell transplantation: incidence, manifestations, and clinical significance. Biol. Blood Marrow Transpl. 13, 1369–1379 (2007).
Rooney, J. P. et al. PCR based determination of mitochondrial DNA copy number in multiple species. Methods Mol. Biol. 1241, 23–38 (2015).
Lodi, A. et al. Combinatorial treatment with natural compounds in prostate cancer inhibits prostate tumor growth and leads to key modulations of cancer cell metabolism. NPJ Precis. Oncol. 1, 18 (2017).
Stanford, S. M. et al. The low molecular weight protein tyrosine phosphatase promotes adipogenesis and subcutaneous adipocyte hypertrophy. J. Cell. Physiol. 236, 6630–6642 (2021).
Wishart, D. S. et al. HMDB: the Human Metabolome Database. Nucleic Acids Res. 35, D521–D526 (2007).
Okuda, S. et al. KEGG Atlas mapping for global analysis of metabolic pathways. Nucleic Acids Res. 36, W423–W426 (2008).
Chao, H. P. et al. Systematic evaluation of RNA-Seq preparation protocol performance. BMC Genomics 20, 571 (2019).
Patro, R., Duggal, G., Love, M. I., Irizarry, R. A. & Kingsford, C. Salmon provides fast and bias-aware quantification of transcript expression. Nat. Methods 14, 417–419 (2017).
Robinson, M. D. & Oshlack, A. A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biol. 11, R25 (2010).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Series B Stat. Methodol. 57, 289–300 (1995).
Kolde, R. & Vilo, J. GOsummaries: an R package for visual functional annotation of experimental data. F1000Res 4, 574 (2015).
Wang, B., Cunningham, J. M. & Yang, X. H. Seq2pathway: an R/Bioconductor package for pathway analysis of next-generation sequencing data. Bioinformatics 31, 3043–3045 (2015).
Chaplan, S. R., Bach, F. W., Pogrel, J. W., Chung, J. M. & Yaksh, T. L. Quantitative assessment of tactile allodynia in the rat paw. J. Neurosci. Methods 53, 55–63 (1994).
Singhmar, P. et al. The fibroblast-derived protein PI16 controls neuropathic pain. Proc. Natl Acad. Sci. USA 117, 5463–5471 (2020).
Ma, J. et al. Cell-specific role of histone deacetylase 6 in chemotherapy-induced mechanical allodynia and loss of intraepidermal nerve fibers. Pain 160, 2877–2890 (2019).
Laumet, G. et al. Interleukin-10 resolves pain hypersensitivity induced by cisplatin by reversing sensory neuron hyperexcitability. Pain 161, 2344–2352 (2020).
Mao-Ying, Q. L. et al. The anti-diabetic drug metformin protects against chemotherapy-induced peripheral neuropathy in a mouse model. PLoS ONE 9, e100701 (2014).
Acknowledgements
We thank S. Hammonds Nelson for providing help with clinical data verification. This research is in part supported by the MD Anderson Cancer Center Leukemia (NIH no. SPORE P50 CA100632 (M.K.), NIH no. R01 CA206210 (M.K. and S.T.), NIH no. R01 CA227064 (A.K. and C.J.H.), CPRIT no. RP180309 (M.K.), NIH Clinical Translational Science Award no. 1UL1TR003167 (D.D.K.), MD Anderson Cancer Center support grant no. P30 CA016672, the Sheikh Ahmed Bin Zayed Al Nahyan Center for Pancreatic Cancer Grant and the Leukemia & Lymphoma Society through its Therapy Acceleration Program and by the MD Anderson Moon Shots program. The CPRIT Core is supported by CPRIT Core Facility Support Grants (nos. RP120348 and RP170002).
Author information
Authors and Affiliations
Contributions
Clinical studies were designed and initiated by T.A.Y., N.D., F.M.-B., C.K.-M., C.P.V., T.P.H., P.J., J. R. Marszalek and M.K. Collection and analysis of clinical data were conducted by T.A.Y., N.D., F.M.-B., C.K.-M., C.P.V., T.P.H., P.J., J. R. Marszalek, M.K., C.S., M.B.B., E.E.D., S.F., D.S.H., D.D.K., S.A.P.-P., J.R., V.S., S.P. and A.M.T. Several patients were recruited by N.P., F.R., M.Y., E.J.J., M.O., K.S., P.B., N.B. and H.M.K. PK analyses and related figures were generated by S. Gera, J. R. Marszalek and Q.A.X. PD analyses in AML blasts and related figures were generated by S.T., M.M., M.E.C., Q.Z., J.H. and A.L. Transcriptomic analyses, data analyses and related figures and tables were generated by C.P.V., C.A.B., Y.L. and Z.J. Preclinical studies and related figures were generated by C.J.H., A.K., J.Z., J.P.G., M.E., D.F. and J. R. Molina. The manuscript was written by T.A.Y., N.D., F.M.B., C.P.V., T.H., P.J., J. R. Marszalek, M.K. and S. Gao. All authors reviewed the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
T.A.Y. is the Medical Director of the Institute for Applied Cancer Science (M.D Anderson Cancer Center), which has a commercial interest in DDR and other inhibitors (no. IACS30380/ART0380 was licensed to Artios). T.A.Y.’s research has been supported by Acrivon, Artios, AstraZeneca, Bayer, Beigene, BioNTech, Blueprint, BMS, Clovis, Constellation, Cyteir, Eli Lilly, EMD Serono, Forbius, F-Star, GlaxoSmithKline, Genentech, Haihe, ImmuneSensor, Ionis, Ipsen, Jounce, Karyopharm, KSQ, Kyowa, Merck, Mirati, Novartis, Pfizer, Ribon Therapeutics, Regeneron, Repare, Rubius, Sanofi, Scholar Rock, Seattle Genetics, Tesaro, Vivace and Zenith; he has consulted for AbbVie, AstraZeneca, Acrivon, Adagene, Almac, Aduro, Amphista, Artios, Athena, Atrin, Avoro, Axiom, Baptist Health Systems, Bayer, Beigene, Boxer, Bristol-Myers Squibb, C4 Therapeutics, Calithera, Cancer Research UK, Clovis, Cybrexa, Diffusion, EMD Serono, F-Star, Genmab, Glenmark, GLG, Globe Life Sciences, GSK, Guidepoint, Idience, Ignyta, I-Mab, ImmuneSensor, Institut Gustave Roussy, Intellisphere, Jansen, Kyn, MEI pharma, Mereo, Merck, Natera, Nexys, Novocure, OHSU, OncoSec, Ono Pharma, Pegascy, PER, Pfizer, Piper-Sandler, Prolynx, Repare, resTORbio, Roche, Schrodinger, Theragnostics, Varian, Versant, Vibliome, Xinthera, Zai Labs and ZielBio; he is a stockholder in Seagen. N.D. has received research funding from Daiichi Sankyo, Bristol-Myers Squibb, Pfizer, Gilead, Sevier, Genentech, Astellas, Daiichi Sankyo, Abbvie, Hanmi, Trovagene, FATE therapeutics, Amgen, Novimmune, Glycomimetics, Trillium and ImmunoGen and has served in a consulting or advisory role for Daiichi Sankyo, Bristol-Myers Squibb, Arog, Pfizer, Novartis, Jazz, Celgene, AbbVie, Astellas, Genentech, Immunogen, Servier, Syndax, Trillium, Gilead, Amgen, Shattuck labs and Agios. M.K. has received research funding from AbbVie, Genentech, F. Hoffman La Roche, Eli Lilly, Cellectis, Calithera, Ablynx, Stemline Therapeutics, Agios, Ascentage, AstraZeneca, Rafael Pharmaceutical, Sanofi and Forty-Seven and has served in a consulting or advisory role for AbbVie, Genentech, F. Hoffman La Roche, Stemline Therapeutics, Amgen, Forty-Seven, Kisoji and Janssen. N.P. serves on the Board of Directors for the following: Dan’s House of Hope; Consulting: AbbVie, Aptitude Health, Astellas Pharma US, Inc., Blueprint Medicines, Bristol-Myers Squibb, Celgene Corp, Cimeio Therapeutics AG, ClearView Healthcare Partners, CTI BioPharma, Dava Oncology, Immunogen, Incyte, Intellisphere, LLC., Novartis AG, Novartis Pharmaceuticals Corp, OncLive (Owned by Intellisphere, LLC), Patient Power, PharmaEssentia, Protagonist Therapeutics, Sanofi-aventis, Stemline Therapeutics, Inc. and Total CME; financial relationships (for example, Stock, Royalty, Gift, Employment or Business Ownership): Karger Publishers; Scientific/Advisory Committee Member: Cancer.Net, CareDx, CTI BioPharma, EUSA Pharma, Inc., Novartis Pharmaceuticals Corp, Pacylex, PharmaEssentia; Speaker/Preceptorship: AbbVie, Aplastic Anemia & MDS International Foundation, Curio Science LLC, Dava Oncology, Imedex, Magdalen Medical Publishing, Medscape, Neopharm, PeerView Institute for Medical Education, Physician Education Resource (PER), Physicians Education Resource (PER), Postgraduate Institute for Medicine, Stemline Therapeutics, Inc. F.M.-B. consults for AbbVie, Aduro BioTech Inc., Alkermes, AstraZeneca, Daiichi Sankyo Co. Ltd., DebioPharm, Ecor1 Capital, eFFECTOR Therapeutics, F. Hoffman La Roche Ltd., GT Apeiron, Genentech Inc., Harbinger Health, IBM Watson, Infinity Pharmaceuticals, Jackson Laboratory, Kolon Life Science, Lengo Therapeutics, Menarini Group, OrigiMed, PACT Pharma, Parexel International, Pfizer Inc., Protai Bio Ltd, Samsung Bioepis, Seattle Genetics Inc., Tallac Therapeutics, Tyra Biosciences, Xencor and Zymeworks; serves on the advisory committee for Black Diamond, Biovica, Eisai, FogPharma, Immunomedics, Inflection Biosciences, Karyopharm Therapeutics, Loxo Oncology, Mersana Therapeutics, OnCusp Therapeutics, Puma Biotechnology Inc., Seattle Genetics, Sanofi, Silverback Therapeutics, Spectrum Pharmaceuticals and Zentalis; and has received honoraria from Chugai Biopharmaceuticals; leads clinical trials that are funded or sponsored by Aileron Therapeutics, Inc., AstraZeneca, Bayer Healthcare Pharmaceutical, Calithera Biosciences, Inc., Curis Inc., CytomX Therapeutics Inc., Daiichi Sankyo Co. Ltd., Debiopharm International, eFFECTOR Therapeutics, Genentech Inc., Guardant Health Inc., Klus Pharma, Takeda Pharmaceutical, Novartis, Puma Biotechnology Inc. and Taiho Pharmaceutical Co. P.B. recieves research funding from Incyte, BMS, CTI BioPharma, Constellation (now Morphosys), Kartos, Blueprint Medicines, Cogent Biosciences, Ionis, Pfizer, Astellas, NS Pharma and Promedior, and honoraria from Incyte, BMS, CTI BioPharma, Sierra Oncology (now GSK), Blueprint Medicines, Cogent Biosciences, Abbvie, Karyopharm, Pharma Essentia, Novartis, Constellation (now Morphosys) and Kartos. A.M.T. is funded by OBI Pharma, Agenus, Parker Institute for Cancer Immunotherapy, Tvardi Therapeutics, Tempus, IMMATICS; Consulting or Advisory Roles: Vincerx, Diaccurate, BrYet, NEX-I, Macrogenics and BioEclipse. J.R. serves on the advisory board of Peptomyc, Kelun Pharmaceuticals/Klus Pharma, Ellipses Pharma, Molecular Partners and IONCTURA; receives research funding from Blueprint Medicines, Black Diamond Therapeutics, Merck Sharp & Dohme, Hummingbird, Yingli, Vall d’Hebron Institute of Oncology/Cancer Core Europe; receives clinical research support from Novartis, Spectrum Pharmaceuticals, Symphogen, BioAlta, Pfizer, GenMab, CytomX, Kelun-Biotech, Takeda-Millenium, GalxoSmithKline, Taiho, Roche Pharmaceuticals, Hummingbird, Yingli, Bycicle Therapeutics, Merus, Curis, Bayer, AadiBioscience, Nuvation, ForeBio, BioMed Valley Discoveries, Loxo Oncology, Hutchinson MediPharma, Cellestia, Deciphera, Ideaya, Amgen, Tango Therapeutics and Mirati Linnaeus Therapeutics; and receives travel support from the European Society for Medical Oncology. IACS-010759 was developed by scientists at MD Anderson. If this drug becomes FDA approved and commercially available, MD Anderson will profit from its sale. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Chi Dang, Daniel Pollyea, Juliane Gust and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editors: Saheli Sadanand and Joao Monteiro, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Effect of IACS-010759 on venous lactate and blood pH.
a–d, Relationship between venous lactate and IACS-010759 concentrations in AML (a) cohort 1, (b) cohort 2, (c) cohort 3, and (d) cohort 4. Dotted line indicates 8 nM of plasma IACS-010759. e-h, Relationship between blood pH and plasma IACS-010759 concentrations in AML (e) cohort 1, (f) cohort 2, (g) cohort 3, and (h) cohort 4. Dotted line indicates 8 nM of plasma IACS-010759. i-m, Relationship between venous lactate and IACS-010759 concentrations in Solid Tumor (i) cohort 1, (j) cohort 2, (k) cohort 3, (l) cohort 4, and (m) cohort 5. Dotted line indicates 8 nM of plasma IACS-010759. n-r, Relationship between blood pH and plasma IACS-010759 concentrations in Solid Tumor (n) cohort 1, (o) cohort 2, (p) cohort 3, (q) cohort 4, and (r) cohort 5. Dotted line indicates 8 nM of plasma IACS-010759.
Extended Data Fig. 2 Treatment-induced peripheral neuropathy.
a, b, (a) Ultrastructural examination and (b) electronic microscopy analysis of a biopsy collected from the left superficial peroneal upper leg nerve root of a Cohort 4 patient from the Solid Tumor trial. The patient developed Grade 3-4 peripheral neuropathy while on a treatment regimen of 2.5 mg of IACS-010759 daily during the induction phase (Day 1–7), and 2.5 mg bi-weekly during the maintenance phase. Images indicate severe vacuolar changes in myelin sheath with axonal degenerative changes and atrophy.
Extended Data Fig. 3 Pharmacokinetics of IACS-010759 in AML and Solid Tumor cohorts.
Dosing regimens are detailed in Fig. 1, Supplementary Table 1. a, b, Plasma IACS-010759 concentrations over time in (a) AML Cohort 1 (blue) and Cohort 2 (red); (b) AML Cohort 3 (green) and 4 (purple). c, d, Plasma IACS-010759 concentrations (nM) over time in Solid Tumor (c) Cohort 1 (blue), Cohort 2 (red), and Cohort 3 (green); (d) Cohort 4 (purple), Cohort 5 (orange), and Cohort 6 (black). Each dot represents the mean plasma IACS-010759 concentration at one collection point for one patient.
Extended Data Fig. 4 Plasma IACS-010759 concentrations in individual patients.
Dosing regimens are detailed in Fig. 1, Supplementary Table 1. a, b, Plasma IACS-010759 concentrations AML patients in (a) Cohort 1 (red) and Cohort 2 (blue), which each received QD dosing, as well as in (b) Cohort 3 (red) and Cohort 4 (blue), which each received an induction and maintenance phase. c-e, Plasma IACS-010759 concentrations in Solid Tumor (c) Cohorts 1 (blue) and 5 (orange), (d) Cohorts 2 (purple) and 4 (red), (e) Cohort 3, and (f) Cohort 6. All cohorts received induction and maintenance phases.
Extended Data Fig. 5 Correlations between plasma IACS-010759 concentration and baseline oxygen consumption rate (OCR) from AML blasts.
Baseline OCR has been normalized to cell number. Closed circles are predose and open circles indicate post dose values. Blue indicates pre-dose (C1D1). Red indicates after one week of QD dosing (C1D7 - Cohorts 3, 4; C1D14 - Cohorts 1, 2). Black closed circles are other timepoints collected during cycle 1. Correlations analyzed by a two-tailed Pearson’s correlation coefficient test; p < 0.05. Each symbol represents the mean +/− 95% confidence interval derived from technical replicates. a, n = 3 at C1D8(6), C1D10; n = 5 at C1D1, C1D1(6) C1D8, and C1D14; n = 6 at all other times. b, n = 5 at C1D8, C1D8(6), C1D22(6), C1D28, C1D28(6); n = 6 at all other times. c, n = 6. d, n = 2 at C1D9, C1D14(6), C1D25(6), C1D28, C1D28(6); n = 3 at C1D8, C1D8(6), C1D14, C1D17, C1D17(6); n = 4 at C1D2, C1D10; n = 5 at C1D1, C1D1(6). e, n = 5 at C1D10; n = 6 at all other times. f, n = 4 at C1D8(6); n = 6 at all other times. g, n = 4 at C1D1(4); n = 5 at C1D1; n = 6 at all other times. h, n = 6. i, n = 2 at C1D7(4); n = 3 at C1D7, C1D15, C1D15(4), n = 6 at C1D1, C1D1(4). j–k, n = 6. l, n = 3 at C1D1, C1D1(4); n = 4 C1D7, C1D7(4); n = 6 at all other times.
Extended Data Fig. 6 Correlations between plasma IACS-010759 concentration and maximal oxygen consumption rate (OCR) from AML blasts.
Maximal OCR has been normalized to cell number. Closed circles are predose and open circles are post dose values. Blue indicates pre-dose (C1D1). Red indicates after one week of QD dosing (C1D7 - Cohorts 3, 4; C1D14 - Cohorts 1, 2). Black closed circles are other timepoints collected during cycle 1. Correlations analyzed by a two-tailed Pearson’s correlation coefficient test; p < 0.05. Each symbol represents the mean +/− 95% confidence interval derived from technical replicates. a, n = 3 at C1D8(6), C1D10; n = 4 at C1D1, C1D2, C1D8; n = 5 at C1D1(6), C1D14, C1D14(6), n = 6 at all other times. b, n = 4 at C1D28, C1D28(6); n = 5 at C1D8, C1D8(6), C1C14, C1C14(6), C1D22(6); n = 6 at all other times. c, n = 6. d, n = 1 at C1D17; n = 2 at C1D9, C1D14, C1D14(6), C1D25(6), C1D28, C1D28(6); n = 3 at C1D8, C1D8(6), C1D17(6); n = 4 at C1D2, C1D10; n = 5 at C1D1, C1D1(6). e, n = 4 at C1D10; n = 6 at all other times. f, n = 4 at C1D8(6); n = 5 at all other times. g, n = 4 at C1D1(4), C1D15; n = 5 at C1D1, C1D15(4), C1D21, n = 6 at C1D7, C1D7(4). H, n = 5 at C1D15, C1D15(4); n = 6 at all other times. i, n = 2 at C1D7(4), C1D15; n = 3 at C1D7, C1D15(4); n = 6 at C1D1, C1D1(4). j, n = 5 at C1D1, C1D1(4), C1D21, unscheduled collection time point; n = 6 at all other times. k, n = 3 at C1D15, C1D15(4); n = 6 at all other times. l, n = 2 at C1D1; n = 3 at C1D1(4); n = 4 at C1D7, C1D7(4); n = 5 at C1D21; n = 6 at C1D15, C1D15(4), end of study.
Extended Data Fig. 7 Evidence of target inhibition in AML blasts.
a-e, Effect of IACS-010759 on levels of (a) NAD+, (b) nicotinamide, (c) tryptophan, (d) glutamine, or (e) alanine in AML blasts from Patients 16, 17, and 19 from AML Cohort 4. Y-axis shows metabolite levels relative to pre-dose levels. N = 4, n = 7, or n = 5 biologically independent samples for Patients 16, 17, or 19 respectively. Differences from pre-trial levels analyzed by a simple linear regression. g-f, Effect of IACS-010759 exposure on NMP, NDP, and NTP levels in AML blasts from (f) Patient 19 and (g) Patient 16 from AML Cohort 4. Y-axis shows nucleotide levels respective to pre-dose levels. N = 4 biologically independent samples. Differences from pre-trial levels analyzed by a simple linear regression.
Extended Data Fig. 8 Drug-induced effects on gene expression in AML blasts.
a, Gene Ontology enrichment analysis on RNA-sequencing (RNA-seq) results from AML blasts collected from Patients 16, 17, and 19 of AML Cohort 4 at several pre- and post-dose timepoints across Cycle 1. b, Pathway analysis ranking deregulated biological pathways upon IACS-010759 treatment from patients described in (a).
Extended Data Fig. 9 IACS-010759 elevates plasma lactate as well as induces behavioral and physiological changes indicative of peripheral neuropathy in preclinical models.
a, Effect of escalating doses of IACS-010759 or vehicle on plasma lactate in NSG and B6 mice. n = 4 or n = 5 biologically independent samples from vehicle-treated mice or all other groups, respectively. Data analyzed by two-tailed unpaired Student’s T-test; n.s. = non-significant. Mean ± SE shown. b, Schematic of the Conditioned Place Preference (CPP) Test. c, Spontaneous pain assessed with a CPP test (b) after the last dose of IACS-010759 (n = 6) or vehicle (n = 6). Data analyzed by two-sided unpaired Student’s T-test. Mean ± SE shown. d, Sensorimotor function of mice in (c) assessed with a beam walk test. n = 12 biologically independent samples. Data analyzed with a two-way ANOVA with Tukey’s multiple comparison test. Mean ± SE shown. e, Oxygen consumption rate (OCR) in the dorsal root ganglion (DRG) from mice in (c) measured under basal conditions (Basal) and after addition of oligomycin (ATP, H + leak), FCCP (Max), or actinomycin + rotenone (spare capacity).; n = 8, n = 4, or n = 8 biologically independent mice for 0 (vehicle), 0.3, or 1 mg/kg IACS-010759, respectively. Data analyzed by two-way ANOVA with Dunnett’s Multiple comparison test. Mean ± SE shown. f, Density of intraepidermal nerve fibers (IENF) from mice in (b) assessed by quantifying PGP9.5 and nerve fibers crossing into the hind paw epidermis per length (mm) of the basement membrane. n = 12, n = 8, or n = 8 biologically independent samples for vehicle, 1 mg/kg, or 5 mg/kg IACS-010759, respectively. Data analyzed by one-way ANOVA followed by Dunnett’s multiple comparison test. Mean ± SE shown. g, Immunohistochemistry (IHC) analysis of DRG ATF3 expression (pink) in of mice treated with vehicle, or 1 mg/kg or 5 mg/kg IACS-010759. Positive control = spare nerve injury (SNI) with ATF3 staining. Scale bar = 167.2 µm. Independently repeated three times with similar results. (h) (top) Representative transmission electron microscopy cross sections of the sciatic nerve from mice in (c) after the last dose of vehicle or IACS-010759. Scale bar=2 µm. (bottom) Effects of 5 mg/kg IACS-010759 (n = 131 axons/4 mice) or vehicle (n = 205 axons/4 mice) on myelin. Differences from vehicle group analyzed by a two-tailed Fisher’s exact test; ***p = 0.0003, **p = 0.0031, *p = 0.0447.
Extended Data Fig. 10 Co-administration of an HDAC inhibitor mitigates the behavioral symptoms of IACS-010759-induced peripheral neuropathy.
a, Spontaneous pain assessed with a Conditioned Place Preference test (Extended Data Fig. 9b) after the last dose of IACS-010759 or vehicle +/− ACY-1215. n = 11, n = 8, or n = 12 biologically independent mice for vehicle, vehicle + ACY-1215, or 1 mg/kg IACS-010759 + vehicle/ACY-1215, respectively. Data were analyzed by a two-way ANOVA. Mean ± SE shown. b, Sensorimotor function of mice in (a) was assessed with a beam walk test after the last dose of IACS-010759 or vehicle +/− ACY-1215. Data represent time to cross the beam. n = 8 or n = 12 biologically independent mice for vehicle + ACY-1215 or all other groups, respectively. Data analyzed by two-way ANOVA with Tukey’s Multiple comparison test. Mean ± SE shown. (c) (left) Representative transmission electron microscopy cross sections of the sciatic nerve from mice in (a) after the last dose of vehicle (top), IACS-010759 (center), or IACS-010759 + ACY-1215 (bottom). Scale bar=2 µm. (Right) Comparison of effects induced by vehicle (n = 184 axons/4 mice), 0.3 mg/kg IACS-010759 (n = 233 axons/4 mice), 1 mg/kg IACS 010759 (n = 158 axons/4 mice), 1 mg/kg IACS-010759 + ACY1215 (n = 201 axons/4 mice), or ACY-1215 (n = 255 axons/4 mice) on myelin. Analysis by two-tailed Fisher’s exact test; **p = 0.0016 vs vehicle; ##p = 0.0041 vs 1 mg/kg IACS-010759.
Supplementary information
Supplementary Information
Supplementary Tables 1–17, Fig. 1, and thee AML Trial protocol and Solid Tumor trial protocol.
Source data
Source Data Fig. 2
Raw data for statistical analyses.
Source Data Fig. 3
Raw data for statistical analyses.
Source Data Fig. 4
Raw data for statistical analyses.
Source Data Extended Data Fig. 1
Raw data for statistical analyses.
Source Data Extended Data Fig. 3
Raw data for statistical analyses.
Source Data Extended Data Fig. 4
Raw data for statistical analyses.
Source Data Extended Data Fig. 5
Raw data for statistical analyses.
Source Data Extended Data Fig. 6
Raw data for statistical analyses.
Source Data Extended Data Fig. 7
Raw data for statistical analyses.
Source Data Extended Data Fig. 8
Raw data for statistical analyses.
Source Data Extended Data Fig. 9
Raw data for statistical analyses.
Source Data Extended Data Fig. 10
Raw data for statistical analyses.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yap, T.A., Daver, N., Mahendra, M. et al. Complex I inhibitor of oxidative phosphorylation in advanced solid tumors and acute myeloid leukemia: phase I trials. Nat Med 29, 115–126 (2023). https://doi.org/10.1038/s41591-022-02103-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-022-02103-8
This article is cited by
-
Deoxycytidine kinase inactivation enhances gemcitabine resistance and sensitizes mitochondrial metabolism interference in pancreatic cancer
Cell Death & Disease (2024)
-
Metabolic alterations in hereditary and sporadic renal cell carcinoma
Nature Reviews Nephrology (2024)
-
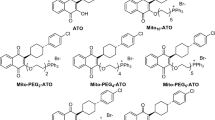
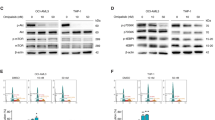
Antitumour effect of the mitochondrial complex III inhibitor Atovaquone in combination with anti-PD-L1 therapy in mouse cancer models
Cell Death & Disease (2024)
-
Chronic lymphocytic leukemia patient-derived xenografts recapitulate clonal evolution to Richter transformation
Leukemia (2024)
-
UCP2 and pancreatic cancer: conscious uncoupling for therapeutic effect
Cancer and Metastasis Reviews (2024)