Abstract
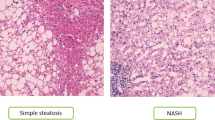
To test the hypothesis that the gut microbiota of individuals with nonalcoholic fatty liver disease (NAFLD) produce enough ethanol to be a driving force in the development and progression of this complex disease, we performed one prospective clinical study and one intervention study. Ethanol was measured while fasting and 120 min after a mixed meal test (MMT) in 146 individuals. In a subset of 37 individuals and in an external validation cohort, ethanol was measured in portal vein blood. In an intervention study, ten individuals with NAFLD and ten overweight but otherwise healthy controls were infused with a selective alcohol dehydrogenase (ADH) inhibitor before an MMT. When compared to fasted peripheral blood, median portal vein ethanol concentrations were 187 (interquartile range (IQR), 17–516) times higher and increased with disease progression from 2.1 mM in individuals without steatosis to 8.0 mM in NAFL 21.0 mM in nonalcoholic steatohepatitis. Inhibition of ADH induced a 15-fold (IQR,1.6- to 20-fold) increase in peripheral blood ethanol concentrations in individuals with NAFLD, although this effect was abolished after antibiotic treatment. Specifically, Lactobacillaceae correlated with postprandial peripheral ethanol concentrations (Spearman’s rho, 0.42; P < 10−5) in the prospective study. Our data show that the first-pass effect obscures the levels of endogenous ethanol production, suggesting that microbial ethanol could be considered in the pathogenesis of this highly prevalent liver disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Fecal metagenomics and liver transcriptomics data have been deposited in the European Nucleotide Archive (ENA; PRJEB47902) and European Genome-Phenome Archive (EGAS00001005704), respectively. A comprehensive data analysis report can be found at https://amcmc.github.io/BARIA_ETHANASH/.Source data which are provided with this paper.
References
Zhu, L. et al. Characterization of gut microbiomes in nonalcoholic steatohepatitis (NASH) patients: a connection between endogenous alcohol and NASH. Hepatology 57, 601–609 (2013).
Yuan, J. et al. Fatty liver disease caused by high-alcohol-producing Klebsiella pneumoniae. Cell Metab. 30, 675–688 (2019).
Younossi, Z. et al. Global perspectives on non-alcoholic fatty liver disease and non-alcoholic steatohepatitis. Hepatology https://doi.org/10.1002/hep.30251 (2018).
Farrell, G. C. & Larter, C. Z. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology 43, S99–S112 (2006).
Sym, W. K., Teaberry, V., Choi, S. S. & Diehl, A. M. Similarities and differences in the pathogenesis of alcoholic and nonalcoholic steatohepatitis. Semin Liver Dis. 29, 200–210 (2009).
Diehl, A. M. & Day, C. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis. N. Engl. J. Med. 377, 2063–2072 (2017).
Thursz, M. et al. EASL clinical practice guidelines: management of alcohol-related liver disease. J. Hepatol. 69, 154–181 (2018).
Engstler, A. J. et al. Insulin resistance alters hepatic ethanol metabolism: studies in mice and children with non-alcoholic fatty liver disease. Gut 65, 1–8 (2015).
Cope, K., Risby, T. & Diehl, A. M. Increased gastrointestinal ethanol production in obese mice: implications for fatty liver disease pathogenesis. Gastroenterology 119, 1340–1347 (2000).
de Medeiros, I. C. & de Lima, J. G. Is nonalcoholic fatty liver disease an endogenous alcoholic fatty liver disease?—A mechanistic hypothesis. Med. Hypotheses 85, 148–152 (2015).
Simic, M., Ajdukovic, N., Veselinovic, I., Mitrovic, M. & Djurendic-Brenesel, M. Endogenous ethanol production in patients with diabetes mellitus as a medicolegal problem. Forensic Sci. Int. 216, 97–100 (2012).
Jeon, S. & Carr, R. Alcohol effects on hepatic lipid metabolism. J. Lipid Res. 61, 470–479 (2020).
Cederbaum, A. I. Alcohol metabolism. Clin. Liver Dis. 16, 667 (2012).
Wilson, D. F. & Matschinsky, F. M. Ethanol metabolism: the good, the bad, and the ugly. Med. Hypotheses 140, 109638 (2020).
van Olden, C. et al. A systems biology approach to understand gut microbiota and host metabolism in morbid obesity: design of the BARIA Longitudinal Cohort Study. Journal of Internal Medicine joim.13157 https://doi.org/10.1111/joim.13157 (2020).
Nascimbeni, F. et al. Clinical validation of the FLIP algorithm and the SAF score in patients with non-alcoholic fatty liver disease. J. Hepatol. https://doi.org/10.1016/j.jhep.2019.12.008 (2020).
Mardinoglu, A. et al. An integrated understanding of the rapid metabolic benefits of a carbohydrate-restricted diet on hepatic steatosis in humans. Cell Metab. 27, 1547–1558 (2018).
Francque, S. M. et al. A randomized, controlled trial of the Pan-PPAR agonist lanifibranor in NASH. N. Engl. J. Med. 385, 1547–1558 (2021).
Elshaghabee, F. et al. Ethanol production by selected intestinal microorganisms and lactic acid bacteria growing under different nutritional conditions. Front. Microbiol. 7, 47 (2016).
Pyo, J. H. et al. Proton pump inhibitors use and the risk of fatty liver disease: a nationwide cohort study. J. Gastroenterol. Hepatol. 36, 1235–1243 (2021).
Krautkramer, K. A., Fan, J. & Bäckhed, F. Gut microbial metabolites as multi-kingdom intermediates. Nat. Rev. Microbiol. 19, 77–94 (2020).
Fell, J. C. & Scherer, M. Estimation of the potential effectiveness of lowering the blood alcohol concentration (BAC) limit for driving from 0.08 to 0.05 grams per deciliter in the United States. Alcohol. Clin. Exp. Res. 41, 2128–2139 (2017).
Nosova, T. et al. Aldehyde dehydrogenase activity and acetate production by aerobic bacteria representing the normal flora of human large intestine. Alcohol Alcohol. 31, 555–564 (1996).
Frantz, J. C. & McCallum, R. E. Growth yields and fermentation balance of Bacteroides fragilis cultured in glucose-enriched medium. J. Bacteriol. 137, 1263–1270 (1979).
Amaretti, A. et al. Kinetics and metabolism of Bifidobacterium adolescentis MB 239 growing on glucose, galactose, lactose, and galactooligosaccharides. Appl. Environ. Microbiol. 73, 3637–3644 (2007).
Weimer, P. J. & Zeikus, J. G. Fermentation of cellulose and cellobiose by Clostridium thermocellum in the absence and presence of Methanobacterium thermoautotrophicum. Appl. Environ. Microbiol. 33, 289–297 (1977).
del Chierico, F. et al. Gut microbiota profiling of pediatric nonalcoholic fatty liver disease and obese patients unveiled by an integrated meta-omics-based approach. Hepatology 65, 451–464 (2017).
Deschasaux, M. et al. Depicting the composition of gut microbiota in a population with varied ethnic origins but shared geography. Nat. Med. 24, 1526–1531 (2018).
He, Y. et al. Regional variation limits applications of healthy gut microbiome reference ranges and disease models. Nat. Med. 24, 1532–1535 (2018).
Fuchs, H. F. et al. Benefits of bariatric surgery do not reach obese men. J. Laparoendosc. Adv. Surg. Tech. A 25, 196–201 (2015).
Seitz, H. K. et al. Alcoholic liver disease. Nat. Rev. Dis. Prim. 4, 16 (2018).
Meijnikman, A. S. et al. Distinct differences in gut microbial composition and functional potential from lean to morbidly obese subjects. J. Intern. Med. https://doi.org/10.1111/joim.13137 (2020).
Kleiner, D. E. et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology https://doi.org/10.1002/hep.20701 (2005).
Bedosa, P. & FLIP Pathology Consortium Utility and appropriateness of the fatty liver inhibition of progression (FLIP) algorithm and steatosis, activity, and fibrosis (SAF) score in the evaluation of biopsies of nonalcoholic fatty liver disease.Hepatology 60, 565–575 (2014).
Costea, P. I. et al. Towards standards for human fecal sample processing in metagenomic studies. Nat. Biotechnol. https://doi.org/10.1038/nbt.3960 (2017).
Karlsson, F. H., Nookaew, I. & Nielsen, J. Metagenomic data utilization and analysis (MEDUSA) and construction of a global gut microbial gene catalogue. PLoS Comput. Biol. 10, e1003706 (2014).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. Methods https://doi.org/10.1038/nmeth.1923 (2012).
Chamberlain, S. A. & Szöcs, E. taxize: taxonomic search and retrieval in R. F1000Res 2, 191 (2013).
Soverini, M. et al. HumanMycobiomeScan: a new bioinformatics tool for the characterization of the fungal fraction in metagenomic samples. BMC Genomics 20, 496 (2019).
Edgar, R. C. Search and clustering orders of magnitude faster than BLAST. Bioinformatics 26, 2460–2461 (2010).
Edgar, R. C. UNOISE2: improved error-correction for Illumina 16S and ITS amplicon sequencing. Preprint at bioRxiv 081257 https://doi.org/10.1101/081257 (2016).
Wang, Q., Garrity, G. M., Tiedje, J. M. & Cole, J. R. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl. Environ. Microbiol. 73, 5261–5267 (2007).
Quast, C. et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 41, D590–D596 (2013).
Bolger, A. M., Lohse, M. & Usadel, B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30, 2114–2120 (2014).
Bray, N. L., Pimentel, H., Melsted, P. & Pachter, L. Near-optimal probabilistic RNA-seq quantification. Nat. Biotechnol. 34, 525–527 (2016).
R Core Team. R: A Language and Environment for Statistical Computing. (R Foundation for Statistical Computing, 2013).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Oksanen, J. et al. Package ‘vegan’. Community Ecology Package. (2019).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. Roy. Stat. Soc. B 57, 289–300 (1995).
Acknowledgements
M.N. is supported by a ZONMW VICI grant 2020 (number 09150182010020). H.H. is supported by a Senior Fellowship of the Dutch Diabetes Research Foundation (2019.82.004). A.S.M. is supported by a Lilly/EFSD grant for Young Investigators. O.A. and V.T. are appointed on a NNF GUTMMM grant 2016 NNF15OC0016798 (to M.N., T.W.S. and F.B.). The study reported here was additionally supported by Le Ducq consortium grant 17CVD01 to F.B. and M.N. M.N, H.H. and A.K.G. are supported by a Dutch Heart Foundation CVON IN CONTROL-2 consortium grant. S.F. has a senior clinical research mandate from the Fund for Scientific Research (FWO) Flanders (1802154N). A.G.H. is supported by the Amsterdam UMC Fellowship, two TKI-PPP grants from Health~Holland and the Gilead Research Scholar grant.
Author information
Authors and Affiliations
Contributions
A.S., M.N., A.K., FB. and V.G. conceived and designed the studies. A.S.M., H.H., M.D., O.A., S.B., M.L.D.B. and J.V. managed the clinical studies and collection of stool samples and clinical data. M.K. was responsible for the study medication. A.S.M., O.A., A.G.H. and M.T. were responsible for the inclusion of participants. E.D., J.W., A.V., C.D.B., L.V. and S.F. delivered the samples of the validation cohort. M.D., V.T., F.B., T.S. and J.N. oversaw the processing of the data. M.D., A.K. and A.S.M. analyzed the data. A.S.M., M.D., H.H., U.B., A.K. and M.N. wrote the manuscript, with input from all the authors.
Corresponding author
Ethics declarations
Competing interests
M.N. is on the scientific board of Caelus Pharmaceuticals, Netherlands. F.B. is on the scientific board of Metabogen AB, Sweden. However, none of these are directly relevant for the current paper. S.F. has acted as advisor and/or lecturer for Roche, Gilead, Abbvie, Bayer, BMS, MSD, Janssen, Actelion, Astellas, Genfit, Inventiva, Intercept, Genentech, Galmed, Promethera, Coherus and NGM Bio. However, none of these are directly relevant for the current paper. A.G.H. has consulted for Novo Nordisk, Gilead, Amgen, Echosens and Julius Clinical. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Jasmohan Bajaj and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Jennifer Sargent, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Portal ethanol concentrations linked to NAFLD disease markers in two independent cohorts.
Portal ethanol concentrations linked to histological scores for NAFLD (a–d). Portal vein ethanol in individuals with NAFL and NASH compared to those without steatosis (e). Ethanol concentrations between different SAF-Activity scores (f) and Nonalcoholic Fatty Liver Disease Activity Scores (g). Box plots feature the median (center line), upper and lower quartiles (box limits), 1.5× the interquartile range (whiskers), points outside of boxplot range are outliers. Significant differences were determined by two-tailed Mann–Whitney test (****P < 0.0001;***P < 0.001; **P < 0.01; *P < 0.05).
Extended Data Fig. 2 Peripheral ethanol concentrations linked to NAFLD disease markers in fasted and post prandial state.
Peripheral ethanol concentrations in relation with histological scores for NAFLD (a–d). Ethanol concentrations in individuals with NAFL and NASH compared to those without steatosis (e). Peripheral ethanol concentrations between different SAF-Activity scores (f) and Nonalcoholic Fatty Liver Disease Activity Scores (g). Box plots feature the median (center line), upper and lower quartiles (box limits), 1.5× the interquartile range (whiskers), points outside of boxplot range are outliers. Significant differences were determined by two-tailed Mann–Whitney test (****P < 0.0001;***P < 0.001; **P < 0.01; *P < 0.05).
Extended Data Fig. 3 Correlations between portal, fasted and post-prandial peripheral ethanol levels and insulin levels.
Spearman’s Rho correlations are given, and lines represent an overall linear fit, with grey areas the standard error with a 0.95 confidence interval.
Extended Data Fig. 4 Correlations between portal and peripheral ethanol levels.
Correlations between portal and fasting peripheral ethanol (a) and post prandial peripheral ethanol (b) concentrations. Correlation strength was tested with Spearman’s rank correlation. Colored lines represent a linear fit for each of the NAFLD classes while black represents the overall fit.
Extended Data Fig. 5 MA plots of liver gene expression in association with NAFLD and ethanol concentrations.
MA plots for fasted peripheral (a), post prandial peripheral (b) and portal (c) ethanol concentrations, between No Steatosis and NAFL (d) and NASH (e). Significant differentially abundant genes are highlighted in blue. NADH2A and CYB2E1 specifically are highlighted in red.
Extended Data Fig. 6 Small intestinal Streptococcus abundance associates with NAFLD and ethanol concentrations.
Relative abundance is increased in NAFL and NASH (a) and correlates with fasted (b) and post-prandial (c) peripheral and portal (d) ethanol concentrations. Difference in abundance was tested with two-tailed Mann–Whitney test Line represents a linear fit with grey areas the standard error with a 0.95 confidence interval. Spearman’s Rho correlation coefficients are shown. Box plots feature the median (center line), upper and lower quartiles (box limits), 1.5× the interquartile range (whiskers), points outside of boxplot range are outliers.
Extended Data Fig. 7 Prospective cohort microbiome alpha diversity analysis.
Shannon’s diversity Index with NAFLD classes (a) shown with violin plots, portal ethanol concentrations (b), fasted peripheral ethanol concentrations (c), post prandial ethanol concentrations (d). Differences in alpha diversity between NAFLD classes were determined by Kruskal-Wallis test. Correlations were tested using spearman’s rank correlation.
Extended Data Fig. 8 Prospective cohort microbiome beta diversity analysis.
NAFLD classes (a), portal ethanol concentrations (b), fasted peripheral ethanol concentrations (c), post prandial ethanol concentrations (d). Bray-Curtis was used as a distance metrics and dissimilarity was tested using permanova using 1000 permutations.
Extended Data Fig. 9 Prospective cohort microbiome associations.
S. cerevisiae abundance associations with NAFLD classes (a), portal ethanol concentrations (b), fasted peripheral ethanol concentrations (c), post prandial ethanol concentrations (d). Significant differences in abundance were determined by two-tailed Mann–Whitney test (*P < 0.05). Correlations were tested using spearman’s rank correlation.
Extended Data Fig. 10 Microbiome characteristics of the intervention study.
Alpha- diversity in NASH (a), PCoA of Bray-Curtis dissimilarity between NAFLD class (b), PCoA of Bray Curtis dissimilarity with rate of ethanol accumulation after 4-methylpyrazole infusion (c), Volcano plot with differential taxa abundance analysis (d). Alpha diversity metrics was compared using a two-tailed Mann–Whitney test. Box plots feature the median (center line), upper and lower quartiles (box limits), 1.5× the interquartile range (whiskers), points outside of boxplot range are outliers. Beta diversity was tested using permanova using 1000 permutations. Differential taxa abundance was tested using deSeq2 and observed p values were Benjamini & Hochberg corrected.
Supplementary information
Supplementary Tables
Supplementary Table 1. Patient characteristics table portal subcohort. Supplementary Table 2. Patient characteristics table portal validation cohort. Supplementary Table 3. Differential expression and gene set enrichment analysis results. Supplementary Table 4. Correlation analysis between ethanol concentrations and fecal microbiome. Supplementary Table 5. Correlation analysis between KEGG orthologous functions and ethanol levels. Supplementary Table 6 DESeq2 analyses of gut microbiome in the intervention study.
Source data
Source Data Fig. 1
Source data for Fig. 1
Source Data Fig. 2
Source data for Fig. 2
Source Data Extended Data Fig. 1
Source data for Extended Data Fig. 1
Source Data Extended Data Fig. 2
Source data for Extended Data Fig. 2
Source Data Extended Data Fig. 3
Source data for Extended Fig. 3
Source Data Extended Data Fig. 4
Source data for Extended Data Fig. 4
Source Data Extended Data Fig. 5
Source data for Extended Data Fig. 5
Source Data Extended Data Fig. 6
Source data for Extended Data Fig. 6
Source Data Extended Data Fig. 7
Source data for Extended Data Fig. 7
Source Data Extended Data Fig. 8
Source data for Extended Data Fig. 8
Source Data Extended Data Fig. 9
Source data for Extended Data Fig. 9
Source Data Extended Data Fig. 10
Source data for Extended Data Fig. 10
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Meijnikman, A.S., Davids, M., Herrema, H. et al. Microbiome-derived ethanol in nonalcoholic fatty liver disease. Nat Med 28, 2100–2106 (2022). https://doi.org/10.1038/s41591-022-02016-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-022-02016-6
This article is cited by
-
Gut and bladder fermentation syndromes: a narrative review
BMC Medicine (2024)
-
What are the common downstream molecular events between alcoholic and nonalcoholic fatty liver?
Lipids in Health and Disease (2024)
-
Integration of polygenic and gut metagenomic risk prediction for common diseases
Nature Aging (2024)
-
Cryptogenic non-cirrhotic HCC: Clinical, prognostic and immunologic aspects of an emerging HCC etiology
Scientific Reports (2024)
-
Non-alcoholic fatty liver disease in patients with morbid obesity: the gut microbiota axis as a potential pathophysiology mechanism
Journal of Gastroenterology (2024)