Abstractpost
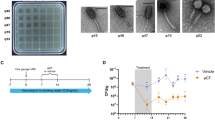
An 81-year-old immunocompetent patient with bronchiectasis and refractory Mycobacterium abscessus lung disease was treated for 6 months with a three-phage cocktail active against the strain. In this case study of phage to lower infectious burden, intravenous administration was safe and reduced the M. abscessus sputum load tenfold within one month. However, after two months, M. abscessus counts increased as the patient mounted a robust IgM- and IgG-mediated neutralizing antibody response to the phages, which was associated with limited therapeutic efficacy.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The GD82, GD01A and GD01B sequence data are available under accession nos. JADWXT000000000, CP035923 and CP035924, respectively. All phage information can be found at https://phagesdb.org/. Sequence information for Muddy, BPs and ZoeJ is available under accession nos. KF024728, EU568876 and KJ510412, respectively. ELISA raw data are available in the supplementary Excel file ‘Raw Data Fig2ab’.
References
Johansen, M. D., Herrmann, J.-L. & Kremer, L. Non-tuberculous mycobacteria and the rise of Mycobacterium abscessus. Nat. Rev. Microbiol. 18, 392–407 (2020).
Griffith, D. E. et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir. Crit. Care Med. 175, 367–416 (2007).
Choi, H. et al. Clinical characteristics and treatment outcomes of patients with macrolide-resistant Mycobacterium massiliense lung disease. Antimicrob. Agents Chemother. 61, e02189-16 (2017).
Choi, H. et al. Clinical characteristics and treatment outcomes of patients with acquired macrolide-resistant Mycobacterium abscessus lung disease. Antimicrob. Agents Chemother. 61, e01146-17 (2017).
Kortright, K. E., Chan, B. K., Koff, J. L. & Turner, P. E. Phage therapy: a renewed approach to combat antibiotic-resistant bacteria. Cell Host Microbe 25, 219–232 (2019).
Salmond, G. P. C. & Fineran, P. C. A century of the phage: past, present and future. Nat. Rev. Microbiol. 13, 777–786 (2015).
Dedrick, R. M. et al. Engineered bacteriophages for treatment of a patient with a disseminated drug-resistant Mycobacterium abscessus. Nat. Med. 25, 730–733 (2019).
Jerne, N. K. & Avegno, P. The development of the phage-inactivating properties of serum during the course of specific immunization of an animal: reversible and irreversible inactivation. J. Immunol. 76, 200–208 (1956).
Roach, D. R. et al. Synergy between the host immune system and bacteriophage is essential for successful phage therapy against an acute respiratory pathogen. Cell Host Microbe 22, 38–47.e4 (2017).
Hodyra-Stefaniak, K. et al. Mammalian host-versus-phage immune response determines phage fate in vivo. Sci. Rep. 5, 14802 (2015).
Górski, A. et al. Phage as a modulator of immune responses: practical implications for phage therapy. Adv. Virus Res. 83, 41–71 (2012).
Aslam, S. et al. Lessons learned from the first 10 consecutive cases of intravenous bacteriophage therapy to treat multidrug-resistant bacterial infections at a single center in the United States. Open Forum Infect. Dis. 7, ofaa389 (2020).
Łusiak-Szelachowska, M. et al. Phage neutralization by sera of patients receiving phage therapy. Viral Immunol. 27, 295–304 (2014).
Kamme, C. Antibodies against staphylococcal bacteriophages in human sera. I. Assay of antibodies in healthy individuals and in patients with staphylococcal infections. Acta Pathol. Microbiol. Scand. B Microbiol. Immunol. 81, 741–748 (1973).
Aslam, S. et al. Early clinical experience of bacteriophage therapy in 3 lung transplant recipients. Am. J. Transplant. 19, 2631–2639 (2019).
Schooley, R. T. et al. Development and use of personalized bacteriophage-based therapeutic cocktails to treat a patient with a disseminated resistant Acinetobacter baumannii infection. Antimicrob. Agents Chemother. 61, e00954-17 (2017).
Jault, P. et al. Efficacy and tolerability of a cocktail of bacteriophages to treat burn wounds infected by Pseudomonas aeruginosa (PhagoBurn): a randomised, controlled, double-blind phase 1/2 trial. Lancet Infect. Dis. 19, 35–45 (2019).
El Haddad, L., Harb, C. P., Gebara, M. A., Stibich, M. A. & Chemaly, R. F. A systematic and critical review of bacteriophage therapy against multidrug-resistant ESKAPE organisms in humans. Clin. Infect. Dis. 69, 167–178 (2019).
Hatfull, G. F. Actinobacteriophages: genomics, dynamics, and applications. Annu. Rev. Virol. 7, 37–61 (2020).
Dedrick, R. M. et al. Mycobacterium abscessus strain morphotype determines phage susceptibility, the repertoire of therapeutically useful phages, and phage resistance. MBio 12, e03431-20 (2021).
Jacobs-Sera, D. et al. On the nature of mycobacteriophage diversity and host preference. Virology 434, 187–201 (2012).
Dedrick, R. M. et al. Mycobacteriophage ZoeJ: a broad host-range close relative of mycobacteriophage TM4. Tuberculosis (Edinb.) 115, 14–23 (2019).
Hatfull, G. F. & Sarkis, G. J. DNA sequence, structure and gene expression of mycobacteriophage L5: a phage system for mycobacterial genetics. Mol. Microbiol. 7, 395–405 (1993).
Acknowledgements
We thank D. Jacobs-Sera and H. G. Aull for the phage cocktail preparation, R. Garlena and D. Russell at the University of Pittsburgh for DNA sequencing and analysis and M. Ramsay, C. Lippincott, J. Zenilman, K. Dooley and E. Ignatius at Johns Hopkins University School of Medicine for their clinical discussions regarding the care of this patient. This work was funded by a Cystic Fibrosis Foundation grant no. HATFUL19GO, a National Institutes of Health (NIH) grant no. GM131729, a Howard Hughes Medical Institute grant no. GT12053 and by the Fowler Fund for Phage Research to G.F.H. as well as grants from the National Heart, Lung, and Blood Institute/NIH (no. K08 HL139994) and the Burroughs Wellcome Fund Career Award for Medical Scientists to K.A.C. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript. We thank R. Schooley, E. Rubin and B. Bishai for comments on the manuscript.
Author information
Authors and Affiliations
Contributions
R.M.D., K.G.F., A.B-T. and B.E.S. contributed to data collection, analysis, interpretation and writing. J.A.N. prepared the regulatory approvals, contributed to data collection and analysis and edited the manuscript. A.E.W. and A.S.O. contributed to data collection and analysis and edited the manuscript. C.T.L. contributed to data analysis and interpretation and edited the manuscript. L.C.R. and N.M.P. provided reagents, technical support and edited the manuscript. G.F.H. conceived the study and contributed to the study design, data interpretation and writing. K.A.C. conceived the study, contributed to the study design, data interpretation, writing and regulatory approvals.
Corresponding authors
Ethics declarations
Competing interests
J.A.N. has received consulting fees from AstraZeneca. G.F.H. is a compensated consultant for Janssen. K.A.C. has received consulting fees from Insmed, Hillrom and Merck. The other authors declare no competing interests.
Additional information
Peer review information Nature Medicine thanks Nina Chanishvili, Laurent Kremer and Jeremy Barr for their contribution to the peer review of this work. Alison Farrell was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Determination of MAC sputum counts.
Quantitative MAC counts in expectorated sputum (log CFU mL−1) pre- and post-treatment. The observed decline in MAC treatment during phage therapy is likely attributable to the addition of anti-MAC antibiotics, azithromycin and ethambutol, to the multidrug regimen. MAC colony morphology appeared smooth and opaque.
Extended Data Fig. 2 Chest CT scans during therapy.
Non-contrast high resolution chest CT scans were performed immediately prior to phage treatment, and repeated after phage treatment initiation at two- and six-months. The majority of chronic airway changes such as bronchiectasis and bronchial wall thickening (white arrows) were stable throughout phage therapy. However, there was slightly increased cavitation in the right upper lobe (black arrows) noted at two months post-phage treatment, and interval development of peripheral left lower lobe consolidations and right lower lobe nodularity (black arrow heads) at six months post-phage treatment.
Extended Data Fig. 3 Antibiotic susceptibility of M. abscessus isolates.
Antibiotic minimum inhibitory concentration (MIC) determinations (in μg/mL) active against M. abscessus GD82 were determined pre-phage therapy initiation and monthly during phage therapy using a standard antibiotic panel for rapidly growing mycobacteria (Sensititre RAPMYCOTM).
Extended Data Fig. 4 Analysis of phage resistance in vitro.
a, 1 ml of 2 ×108 CFU GD82 was mixed with 2 ×109 PFU of each phage used in the cocktail or with all three phages, and incubated at 37 °C with shaking. After 48 hours, 0.1 ml of the mix was spread on solid media and incubated for 5 days at 37 °C. b, Four surviving colonies of each phage challenge were grown and retested for phage sensitivity by spotting 10-fold serial dilutions of phages as indicated. GD82-M_RM2 and GD82-Z_RM2 could not be propagated and were not tested further. BPsΔ33HTH_HRM10 RMs were not tested.
Extended Data Fig. 5 Clinical indicators during phage treatment.
Safety assessments during phage treatment included regular monitoring of complete blood counts with differential, comprehensive metabolic panels, and inflammatory markers. During six-months of intravenous phage treatment there were no clinically significant differences observed in a, white blood cell (WBC) total counts and differentials, b, hemoglobin and platelets, c, liver function (alanine transaminase, ALT; aspartate transaminase, AST; and total bilirubin) or kidney function (creatinine), and d, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
Supplementary information
Supplementary Information
Supplementary Results and References and Supplementary Figs. 1–5.
Supplementary Data 1
Raw data for the ELISA analyses.
Rights and permissions
About this article
Cite this article
Dedrick, R.M., Freeman, K.G., Nguyen, J.A. et al. Potent antibody-mediated neutralization limits bacteriophage treatment of a pulmonary Mycobacterium abscessus infection. Nat Med 27, 1357–1361 (2021). https://doi.org/10.1038/s41591-021-01403-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-021-01403-9
This article is cited by
-
Characterization, antibacterial, and cytotoxic activities of silver nanoparticles using the whole biofilm layer as a macromolecule in biosynthesis
Scientific Reports (2024)
-
Phage-specific immunity impairs efficacy of bacteriophage targeting Vancomycin Resistant Enterococcus in a murine model
Nature Communications (2024)
-
Mycobacterial nucleoid-associated protein Lsr2 is required for productive mycobacteriophage infection
Nature Microbiology (2023)
-
Understanding the mechanisms and translational implications of the microbiome for cancer therapy innovation
Nature Cancer (2023)
-
Mycobacterium abscessus VapC5 toxin potentiates evasion of antibiotic killing by ribosome overproduction and activation of multiple resistance pathways
Nature Communications (2023)